Abstract
Objective: Agranulocytosis is a rare but fatal condition. The majority of cases are associated with drugs. However, in‐patient incidences and the relationship between clinical outcomes and bone marrow characteristics have not been established.
Methods: We conducted a retrospective study in a university hospital. A total of 38 in‐patients diagnosed with agranulocytosis were analyzed.
Results: The average incidence of agranulocytosis in Songklanagarind Hospital between 1993 and 2007 was 0·98 cases per 10 000 admissions per year. Antimicrobial agents were the most common etiology (63% of patients) and antithyroid agents were the second most common (13·6%). Two patterns of bone marrow were noted: type I was characterized by a left‐shifted granulopoiesis and type II was recognized as having hypocellular bone marrow with markedly reduced granulocyte precursors. A significantly higher mortality was associated with type II.
Conclusion: Antimicrobial agents are the most common cause and the rare granulocyte precursors in bone marrow are associated with higher mortality rates.
Introduction
Agranulocytosis is a rare but life‐threatening disorder defined as an absolute neutrophil count less than 0·5×109/l.Citation1 Reports on case fatality rates were 5–16%.Citation2–Citation5More than 70% of cases are associated with drugs.Citation6 However, very little data is available concerning clinical and hematologic features of this condition. Our study aims to provide an incidence rate, a list of causative drugs, and a relationship between bone marrow characteristics and clinical outcomes of patients diagnosed with drug‐induced agranulocytosis in a university hospital in Southern Thailand.
Methods
Between 1993 and 2007, medical records of 38 patients in Songklanagarind Hospital who were diagnosed with drug‐induced agranulocytosis, were reviewed for demographic data, associated drugs, clinical features, hematologic profiles, microbiological data, bone marrow findings, and outcomes. The incidence rates were calculated by using the total admissions per year as a population at risk.
Agranulocytosis was defined as a condition in which an absolute neutrophil count less than 0·5×109/l with a history of current exposure to drug in which normalcy is regained after withdrawal of the suspected drug.Citation7 The exclusion criteria were: (1) cases possibly related to chemotherapy, radiotherapy or immunosuppressive therapy; and (2) disorders with affecting other cell lines, e.g., aplastic anemia.
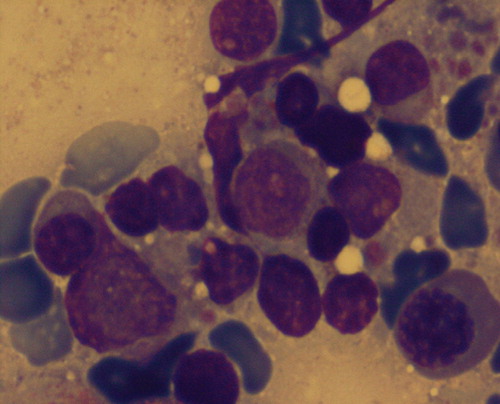
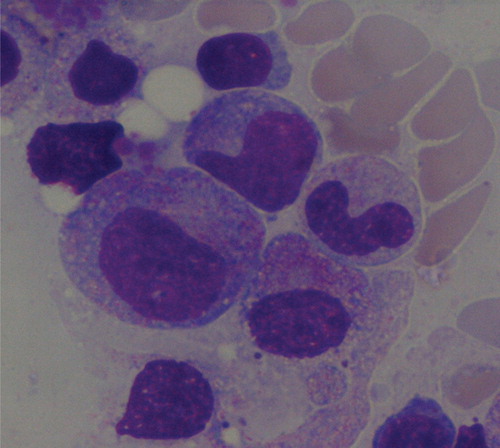
Two patterns of bone marrow findings were defined: type I was characterized by left‐shifted granulopoiesis with few or no mature forms of granulocytes beyond myelocytes () and type II was recognized as hypocellular marrow with markedly reduced granulocyte precursors ().Citation8
Figure 1. Type I agranulocytosis revealed prominent promyelocytes and metamyelocytes but rare mature forms (×1000).
All data were double entry into Epidata and analyzed by R program version 2.9.0 with Epicalc packages. Student’s t‐test and Ranksum test were used to test differences of continuous variables and Fisher’s exact test was used for categorical variables. Statistic significance was defined as P<0·05.
Results
An average incidence of agranulocytosis in Songklanagarind Hospital between 1993 and 2007 was 0·98 case per 10 000 admissions (). Among 38 patients with drug‐induced agranulocytosis, 21 (51%) were male and 17 (44·7%) were female. No patients suffered from more than one episode of agranulocytosis. The mean age±SD was 40·7±18·1 years (range 13–85 years). Four HIV‐infected patients were recognized and bone marrow confirmations were done in all of them.
Table 1. Incidences of agranulocytosis during 1993–2007
The implicated drugs are listed in . Antimicrobial agents were the most common in 63% of patients in which 15·9% were derived from trimethoprim‐sulfamethoxazole, 13·6% from ceftazidime and 11·3% from cloxacillin. Other antimicrobial agents causing this condition were cefazolin, cefoxitin, cefuroxime, cefotaxime, chloramphenicol, penicillin, rifampicin, and acyclovir. Antithyroid agents were responsible in 13·6% of cases with methimazole being more common than propylthiouracil.
Table 2. Drugs associated with agranulocytosis in 38 cases
The median duration of drug administration before the diagnosis of agranulocytosis was 15·5 days (range 2–90 days). Ten patients took drugs for less than 7 days, while five patients were exposed for more than 42 days.
All patients became ill with high‐grade fever at the time of diagnosis. Eight patients (21·3%) were presented with diarrhea. Skin and soft tissue infections were detected in five patients (13·1%). Sore throat and urinary tract infection were diagnosed in three patients each while two patients suffered from community‐acquired pneumonia and two from infective endocarditis. Pyogenic liver abscess, acute cholangitis and infected peritoneal dialysis were recognized in three patients.
The organisms were isolated from primary sites of infection during neutropenia period in eight patients (21·1%): Pseudomonas aeruginosa (3 cases), Klebsiella pneumoniae (2 cases), Escherichia coli (1 case), Mycobacterium tuberculosis (1 case) and Acinetobacter baumanii (1 case). Blood cultures were positive in 10 patients (26·3%): Escherichia coli (3 cases), Streptococcus spp. (2 cases), Pseudomonas aeruginosa (2 cases), Burkholderia pseudomallei (2 cases), Klebsiella pneumoniae (1 case) and Staphylococcus spp. (1 case).
Bone marrow examinations were done in 19 patients because one patient died before a bone marrow study was done, eight had rapid improvement of neutropenia after stopping their drug intake, and others refused this procedure. A comparison between the two patterns of bone marrow and clinical characteristics is shown in . The mortality rate was significantly higher in type II agranulocytosis.
Table 3. Comparison between two types of bone marrow and clinical characteristics
Discussion
This study provided an incidence rate based on total admissions per year and etiologies of non‐chemotherapy drug‐induced agranulocytosis in a single university hospital in Southern Thailand. In addition, the bone marrow characterized by rare granulocyte precursors was associated with significantly lower circulating white blood cells and a higher mortality rate than in bone marrow characterized by the appearance of left‐shifted granulopoiesis.
From several epidemiological studies and case reports, the risks of agranulocytosis for individual drugs, or a few drugs were explored. Our study provided a list of suspected drugs, which are used commonly in daily practice, related to the serious reaction. However, the reported causative drugs were only possibly related to agranulocytosis. Because of the paucity of cases and the confounding from multiple concomitant drugs, it was not feasible to conduct a study that demonstrated results with strong statistical power. Therefore, we tried to confirm the diagnosis with bone marrow examination, which revealed two characteristics of this condition relating to white cell count and mortality rate. In addition, the in‐hospital incidence of agranulocytosis should make physicians more alert than the population‐based incidence.
Several studies showed that annual community‐acquired incidences were 0·5–9·2 per million inhabitants.Citation9–Citation12 In 1999, the population‐based case‐control study showed the overall incidence of 0·8 per million per year in Bangkok, Thailand.Citation13 The incidences in other studies increased with age and were higher in womenCitation10,Citation14 but our study revealed a slight male predominance and a median age of only 40·7 years. The most common causative drugs in this study were antimicrobial agents and the second were antithyroid drugs. Unlike other population‐based studies, the strongest association appeared to be antithyroid drugs.Citation11,Citation13,Citation15 In this hospital‐based setting, the possibility could not be excluded that mild cases could have recovered without hospitalization.
The appearances of bone marrow findings type I and II may be result from two explanations: (1) the immunological processes – type I is related to complement‐mediated intravascular granulocyte destruction and related marrow hyperplasia, and type II is associated with direct toxic suppression of granulopoietic precursor proliferation; and (2) the stage of the disease at which bone marrow testing is performed.Citation8
Although almost all drugs have been reported at least once in the etiology, in our study a limited number of drugs are responsible for the etiology. Therefore, awareness by physicians and patients, especially in the first few months of certain medicines being prescribed, could reduce mortality. Moreover, appropriate management including empirical broad‐spectrum antibiotic therapy and hematopoietic cell growth factor could reduce mortality.Citation16
In the era of increased life expectancy and the emergence of new causative drugs, agranulocytosis, a potentially life‐threatening potential adverse event, should be of concern. Therefore, individual risk factors such as genetic polymorphisms, human compatibility antigens or clinical predictors, especially in commonly used drugs, could be quantified to avoid serious, non‐dose‐dependent and idiosyncratic reactions.
Conclusion
Agranulocytosis is a life‐threatening blood disorder. Physician awareness and prompt treatment could reduce the percentage of case fatality. This study showed that an average incidence of agranulocytosis was 0·98 cases per 10 000 admissions per year. The most common drugs responsible for this condition were antimicrobial agents. Two types of bone marrow characteristics were associated with mortality rates.
Ethical approval
This study was approved by the Ethics Committee of Prince of Songkla University.
Conflict of interest
None disclosed.
References
- Pisciotta AV. Drug-induced agranulocytosis. Peripheral destruction of polymorphonuclear leukocytes and their marrow precursors. Blood Rev 1990;4:226–37.
- Andres E, Kurtz JE, Maloisel F. Nonchemotherapy drug-induced agranulocytosis: experience of the Strasbourg teaching hospital (1985–2000) and review of the literature. Clin Lab Haematol 2002;24:99–106.
- Julia A, Olona M, Bueno J, Revilla E, Rossello J, Petit J, et al.. Drug-induced agranulocytosis: prognostic factors in a series of 168 episodes. Br J Haematol 1991;79:366–71.
- Andres E, Kurtz JE, Perrin AE, Dufour P, Schlienger JL, Maloisel F. Haematopoietic growth factor in antithyroid-drug-induced agranulocytosis. QJM 2001;94:423–8.
- Andres E, Kurtz JE, Martin-Hunyadi C, Kaltenbach G, Alt M, Weber JC, et al.. Nonchemotherapy drug-induced agranulocytosis in elderly patients: the effects of granulocyte colony-stimulating factor. Am J Med 2002;112:460–4.
- Kaufman DW, Kelly JP, Jurgelon JM, Anderson T, Issaragrisil S, Wiholm BE, et al.. Drugs in the aetiology of agranulocytosis and aplastic anaemia. Eur J Haematol Suppl 1996;60:23–30.
- Andres E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. Idiosyncratic drug-induced agranulocytosis: update of an old disorder. Eur J Intern Med 2006;17:529–35.
- Lekhakula A, Swasdikul D. Drug-induced agranulocytosis: experience in two university hospitals. J Med Assoc Thai 1991;74:121–30.
- Kaufman DW, Kelly JP, Issaragrisil S, Laporte JR, Anderson T, Levy M, et al.. Relative incidence of agranulocytosis and aplastic anemia. Am J Hematol 2006;81:65–7.
- Theophile H, Begaud B, Martin K, Laporte JR, Capella D. Incidence of agranulocytosis in Southwest France. Eur J Epidemiol 2004;19:563–5.
- Ibanez L, Vidal X, Ballarin E, Laporte JR. Population-based drug-induced agranulocytosis. Arch Intern Med 2005;165:869–74.
- Hamerschlak N, Maluf E, Pasquini R, Eluf-Neto J, Moreira FR, Cavalcanti AB, et al.. Incidence of aplastic anemia and agranulocytosis in Latin America – the LATIN study. Sao Paulo Med J 2005;123:101–4.
- Shapiro S, Issaragrisil S, Kaufman DW, Anderson T, Chansung K, Thamprasit T, et al.. Agranulocytosis in Bangkok, Thailand: a predominantly drug-induced disease with an unusually low incidence. Aplastic Anemia Study Group. Am J Trop Med Hyg 1999;60:573–7.
- van Staa TP, Boulton F, Cooper C, Hagenbeek A, Inskip H, Leufkens HG. Neutropenia and agranulocytosis in England and Wales: incidence and risk factors. Am J Hematol 2003;72:248–54.
- Rawson NS, Harding SR, Malcolm E, Lueck L. Hospitalizations for aplastic anemia and agranulocytosis in Saskatchewan: incidence and associations with antecedent prescription drug use. J Clin Epidemiol 1998;51:1343–55.
- Andersohn F, Konzen C, Garbe E. Systematic review: agranulocytosis induced by nonchemotherapy drugs. Ann Intern Med 2007;146:657–65.