Introduction
Iron deficiency, defined as the absence of iron stored in the reticuloendothelial system, is the most common nutritional disorder, affecting 30–70% of the population of less developed countries but less than 20% of the population in the industrialized world. It is particularly prevalent in women of childbearing age and in children. If iron intake does not provide sufficient iron to maintain adequate production of red blood cells (RBCs), iron deficiency leads to iron deficiency anemia (IDA). IDA is the most common anemia syndrome encountered in clinical medicine. In a recent review of healthy individuals in the US military, IDA had an incidence of 3.4 per 10,000 patient-years in men but 29.5 per 10,000 patient-years in women.
Cause
Iron deficiency can develop primarily from insufficient intake in growing children and in pregnant women, who have increased iron requirements as part of normal development. However, in most cases it develops as a result of blood loss, since the majority of the body's iron is present in RBCs in the form of the oxygen-carrying protein hemoglobin. The most common reason for iron deficiency due to blood loss is menstruation. In adult men, iron deficiency is almost always due to abnormal loss of blood, particularly in the gastrointestinal tract. In patients with iron deficiency, persistence of circumstances where iron utilization (due to growth or blood loss) exceeds iron intake, leads to the development of IDA.
Symptoms and signs
Other than pica, there are no specific signs or symptoms of IDA, and the signs and symptoms below can be seen in anemia of any type. Patients with IDA due to blood loss may have signs or symptoms from the disease causing blood loss.
| •. | Pallor | ||||
| •. | Easy fatigue | ||||
| •. | Shortness of breath with exertion | ||||
| •. | Pica, which is compulsive eating of substances without nutritional value. The most frequent substance eaten is ice; other common forms involve corn starch, cardboard, or dirt. | ||||
Tests
The purpose of testing in evaluating patients with potential IDA is to demonstrate the absence of storage iron in the reticuloendothelial symptom.
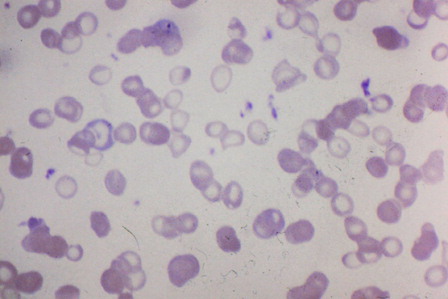
Microcytic/hypochromic RBCs: RBCs which are small (low mean corpuscular volume) and have an increased pale area in the center (low mean corpuscular hemoglobin concentration) are typical in iron deficiency.
Figure 1. Peripheral blood smear from a patient with IDA. Characteristic microcytic/hypochromic red cells noted in the center of the field.
Serum ferritin: Serum ferritin concentration is a marker of iron stores. A decreased serum ferritin is diagnostic of iron deficiency, but is seen in only 50% of cases. Ferritin may be falsely elevated by inflammation.
Serum iron and transferrin: Iron deficiency decreases serum iron and increases serum transferrin, producing a low ratio of iron to transferrin (‘transferrin saturation’). A transferrin saturation less than 10% is strongly suggestive of iron deficiency, but inflammation depresses both iron and transferrin and may make these tests difficult to interpret. Total iron binding capacity is another way to measure transferrin.
Serum-soluble transferrin receptor (sTfR): sTfR is increased in iron deficiency. It is usually expressed as a ratio with ferritin.
Bone marrow iron stain: Absence of iron on a bone marrow specimen is the ‘gold standard’ for diagnosis of iron deficiency, but requires an invasive procedure.
Differential diagnosis: The anemia of chronic disease (ACD), also called the anemia of inflammation, is often confused with IDA since both are associated with a low serum iron concentration, and approximately 20% of ACD patients have slightly microcytic RBCs. However, serum ferritin concentration in ACD is in the mid-normal to elevated range. Thalassemia or hemoglobinopathy trait syndromes are sometimes mistaken for iron deficiency since they are associated with microcytic RBCs. However, biochemical iron studies (serum iron, transferrin, ferritin) are normal in hemoglobinpathy and thalassemia.
Testing strategy: The sequence in which particular tests are used depends on the patient population. In healthy outpatients without chronic underlying disease, either serum ferritin alone or the combination of serum iron and transferrin is probably adequate to diagnose IDA. In patients with significant concurrent illness, serum iron, transferrin, and ferritin should all be ordered to simultaneously address the possibility of ACD. sTfR testing should be reserved for cases which are unclear. Bone marrow examination should be reserved for rare circumstances where IDA is suspected and cannot be ruled out by other means.
Treatment options
There are two goals of treatment: replacement of iron stores with correction of anemia; and identification/correction of the source of blood loss, if any.
| •. | Oral iron compounds: There are a variety of iron preparations, both liquid and tablet/capsule, which are safe, effective, and relatively inexpensive. However, they may produce constipation and/or stomach discomfort. | ||||
| •. | Intravenous iron replacement: Patients who do not respond to oral iron or cannot tolerate it can be treated with intravenous iron preparations. These are more expensive than oral agents, and have some risk of allergy-like reactions, although these are uncommon and manageable. | ||||
| •. | Treatment of IDA should continue until the anemia is corrected and iron stores are normal. | ||||
| •. | Evaluation for site of blood loss: All adult men and post-menopausal women should have evaluation of the gastrointestinal tract, looking for a cause of blood loss. This is probably not necessary in healthy women of childbearing age unless there is a reason on history or physical examination to suspect blood loss from a source other than menses or the patient fails to respond to iron. | ||||
| •. | Other reasons for blood loss: Other reasons for blood loss indicated by the patient's history and physical examination should be investigated if present. | ||||
Outlook
The outlook for patients with IDA is typically favorable but depends on the cause of blood loss. For patients with IDA due to gastrointestinal blood loss, for example, the outlook is determined by the nature of the underlying disease.
Additional resources (websites)
Iron Disorders Institute: http://www.irondisorders.org/iron-deficiency-anemia
U.S. Centers for Disease Control: http://www.cdc.gov/nutrition/everyone/basics/vitamins/iron.html
Mayo Clinic: http://www.mayoclinic.com/health/iron-deficiency-anemia/DS00323