Abstract
Objective and importance
Introduction of high-dose chemotherapy and the novel agents including bortezomib, Lenalidomide, and Thalidomide has provided a significant progress in the treatment of multiple myeloma (MM) with an increase in median overall survival up to 6–8 years. However, the advances in myeloma treatment comes at a price with new spectrum of treatment-related infectious complications which should be taken into consideration while treating these patients.
Clinical presentation
We report here two patients with Ig G λ MM presenting with intracerebral mass lesions in the abscence of constitutional symptoms that would suggest an infectious etiology. Both patients had severe hypogammaglobulinemia and lymphopenia, which was attributed to treatment regimens including bortezomib.
Intervention
The surgical intervention-revealed abscess in both cases caused by Nocardia cyriacigeorgica, a relatively new pathogen which rarely causes infections in humans and also an unexpected pathogen in myeloma patients.
Conclusion
Although every aspect of immune system is known to be affected in MM, humoral immune deficiency is the hallmark of the inherent immune defect in this disease. Introduction of the novel agents, bortezomib in particular seems to have changed the characteristics of the immune dysfunction and the spectrum of the opportunistic infections by causing qualitative and quantitative changes in cellular immunity. The new spectrum of infectious agents might not be limited to hepatitis B and herpes zoster. Monitoring lymphopenia and administration of prophylactic antimicrobial agents accordingly could be considered in patients treated with bortezomib.
Introduction
Involvement of the central nervous system in patients with multiple myeloma (MM) is very rare consisting of 1% of the patients. Parenchymal brain lesions without bone and dural involvement is even rarer.Citation1 Despite the rarity of intracranial mass lesions in patients with MM, their presence suggests plasmacytomas.Citation2,Citation3 Brain abscess is also a rare phenomenon in myeloma patients.Citation4–Citation7 Here we present two patients who developed intracranial mass lesions during their anti-myeloma treatment which came out to be abscess caused by a very rare pathogen; Nocardia cyriacigeorgica. MM is associated with severe immunodeficiency, humoral in particular, causing a variety of gram positive bacterial infections; Streptococcus pneumoniae and Haemophilus influenzae being the leading pathogens. However, Nocardia infections are not among the spectrum of bacterial infections we expect to see in MM patients.Citation8,Citation9 Here we report two MM patients with brain abscess caused by Nocardia species who are the first two cases in the literature to best of our knowledge. The possible causes of changing spectrum of infections in myeloma patients will also be discussed in this consise review.
Case 1
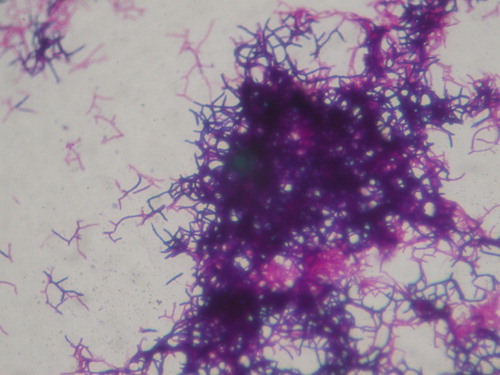
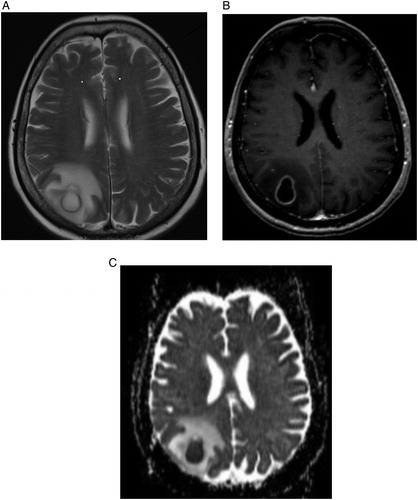
A 61-year-old woman was diagnosed with MM Ig G λ in November 2006. She received six cycles of vincristine, adriamisin, and dexamethasone (VAD) with minimal response. She consequently received thalidomide. She was consolidated with high-dose melphalan and autologous stem cell transplantation (ASCT) in September 2007, after achieving partial response with Thalidomide. She achieved complete remission (CR) after ASCT and remained so, until January 2012. She received three cycles of cyclofosfamide, bortezomib and dexamethasone (Cy-Bor-Dex) after the relapse of her MM, with the intention to proceed with a second ASCT. After the third cycle of Cy-Bor-Dex she developed an epileptic seizure. Her physical examination was unremarkable and she was afebrile and without any systemic symptoms then. Blood counts, serum chemistries, and viscosity tests were all within normal limits, except a very low level of absolute lymphocyte count of 885/μl. Her Ig G level was also very low with 531 mg/dl. Her Ig M and A levels were within normal limits. Diffusion magnetic resonance imaging (MRI) revealed a ring enhancing right posterior parietal mass lesion with prominent edema, showing diffusion restriction, suggesting an abscess (). Although discriminating abscess from neoplastic lesions can be challenging in these patients, the pattern with the restriction in diffusion-weighted imaging suggested an infectious etiology. She was operated on and found to have an abscess which was surgically removed. Colonies of Nocardia sp grew in the culture (). A molecular diagnostic method using 16S ribosomal ribonucleic acid (rRNA) gene sequencing, revealed 99.9% homology with N. cyriacigeorgica. The isolate showed susceptibility to amikacin, imipenem, meropenem, trimethoprim-sulfamethoxazole (TMP-SMX) and was resistant to ciprofloxacin and levofloxacin and showed intermediate susceptibility to amoxicillin-clavulanic acid. She received a 6-week course of meropenem intravenously and her treatment was continued with oral amoxacillin/clavulanic acid for another 6 weeks. As she was an ASCT candidate, TMP-SMX was avoided considering the myelosuppressive effect in the pre-engraftment period. She showed clinical improvement, with complete resolution of the lesions with the follow-up MRI at the 6th week of antibiotic therapy. After the first month of ASCT, amoxicillin-clavulanic acid was switched to oral TMP-SMX and was administered for an additional 6 months. She received a second ASCT after completing her antibiotic treatment and is in CR 6 months status post the second ASCT with an oligoclonal Ig A κ monoclonal band on her immunofixation.
Figure 1. T2-weighted (A) and post-contrast T1-weighted (B) brain MR images in the axial plane shows a right parietal mass lesion, with ring enhancement and peripheral edema. Apparent diffusion coefficient map (C) generated from diffusion-weighted study performed at the same anatomic level depicts diffusion restriction, reflecting the highly viscous content, consistent with abscess.
Case 2
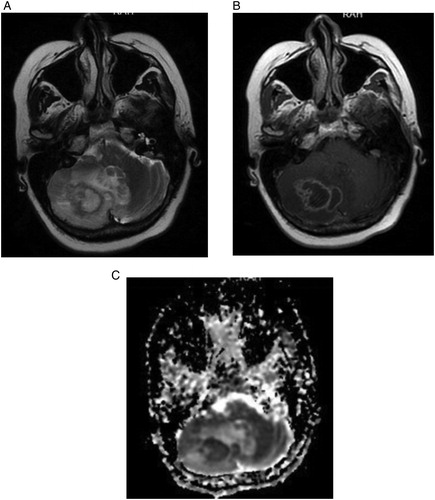
The second patient was a 60-year-old woman, diagnosed with MM immunoglobulin G λ in December 2011. Her medical history revealed breast cancer that was treated with breast-conserving surgery and tamoxifen in 2011 and remained in remission so far. Her MM was unresponsive to VAD and Cy-Bor-Dex was started. Her physical examination was unremarkable otherwise, when she developed signs of cerebellar dysfunction that included dysarthria, and gait disturbance after the fourth cycle of Cy-Bor-Dex. She denied headaches, recent fevers, or respiratory symptoms. Blood counts, serum chemistries, and viscosity tests were all within normal limits except a very low level of absolute lymphocyte count of 40/μl and an extremely low level of Ig G of 252 mg/dl. Ig A and M levels were within normal limits then. Contrast enhanced brain MRI revealed multiple peripherally enhancing mass lesions in the right cerebellum and left parietal lobe. The lesion in right cerebellum was about 3 cm and had prominent mass effect. On diffusion-weighted imaging, the lesion showed restriction consistent with an abscess (). As there was a risk of herniation, an emergent operation was performed and the mass lesion was removed with its wall. The sample was unfortunately not cultured during operation. However as the frosen pathology of the specimen revealed inflammatory process consistent with abscess, an immediate spinal tap was performed after the operation with the aim of culturing the cerebrospinal fluid (CSF). Biochemical analysis of the CSF showed the levels of glucose as 64 mg/dl, protein 192 mg/dl, chlor 126 mmol/l, and Na 140 meq/l. Nocardia was isolated in CSF cultures and identification of N. cyriacigeorgica was performed with 16S rRNA sequencing. According to disk diffusion antimicrobial susceptibility test results, it was found to be susceptible to amikacin, imipenem, meropenem, and TMP-SMX, and resistant to ciprofloxacin and levofloxacin. İmipenem/cilastatin was administered parenterally for 6 weeks and TMP-SMX was commenced with the plan of contining up to 6–12 months. She is well and free of myeloma treatment 6 months after the opertaion and still on TMP-SMX treatment. Interestingly, she also is in CR and has an Ig A λ monoclonal protien that we beleive is oligoclonal reconstitution.
Figure 3. T2-weighted (A) and postcontrast T1-weighted (B) brain MR images in the axial plane shows a right cerebellar mass lesion, with peripheral enhancement and accompanying edema causing mild midline shift. Apparent diffusion coefficient map (C) generated from diffusion-weighted study performed at the same anatomic level depicts diffusion restriction, enabling the diagnosis of an abscess.
Discussion
The presented two female patients with severe lymphopenia have some common features with the same M protein and have a brain abscess in the abscence of systemic symptoms after being treated with bortezomib. Nocardial brain abscess are reported to be more common in females in the immunocompromised population while more common in males in the immunocompetent patients in an extensive review of 120 patients with Nocardial brain abscess.Citation10 Patients with Ig G M protein are also known to have an increased risk of infection which also is associated with defective antibody response to antigenic stimuli and defective antibody formation in response to pneumococcal vaccine.Citation8 Systemic steroids on the other hand seems to have masked the symptoms including fever, by supressing the systemic inflammatory response in the presented cases.
MM is known with severe and global immunodeficiency though humoral immunity is involved in particular.Citation11 There have been a significant improvement in response rates and survival of the patients with the introduction of high-dose melphalan with ASCT and the novel agents in the management of MM.Citation12 However, this increased survival which almost turns MM to a chronic disease, comes at a price. These novel agents might contribute to the inherent immunodeficiency of MM and increase the risk of infection and change the spectrum of infections.Citation10,Citation12 Bortezomib in particular, has been showed to be associated with impaired T cell function due to inhibition of nuclear factor-κB and lead to increased risk and rate of several infections including herpes zoster (HZ) and hepatitis B in MM patients.Citation11,Citation13–Citation18
Immunocompromised patients are at increased risk of developing brain abscess.Citation19–Citation21 T-cell and macrophage dysfunction of various causes account for the brain abscess originating from atypic mycobacteria, Aspergillus, and Nocardia species.Citation20,Citation22 Despite the severe immunodeficiency and increased risk of infection in myeloma patients, brain abscess is extremely rare. A PubMed search revealed only four cases of brain abscess in MM patients.Citation4–Citation7 The pathogens were Chaetomium atrobrunnea, Listeria monocytogenes, Corynebacterium, and Aspergillus species in these reports.
Nocardia infections are opportunistic infections occurring in patients with impaired cellular immunity and are extremely rare in MM patients.Citation23 The presented two cases suggest that some new pathogens such as Nocardia species can also be added to the changing spectrum of infections in MM patients. Profound lymphopenia and very low Ig G levels are the common aspects of the presented cases and seems to have a role in the development of brain abscess. As it is well known to cause profound lymphopenia,Citation14 we believe that bortezomib accounts for the severe lymphopenia in the presented cases.
Antimicrobial prophylaxis has also changed in MM with the introduction of novel agents. Acyclovir is added to the treatment protocols to prevent HZ infections in MM patients who are treated with bortezomib.Citation24 Similar prophylaxis might as well be considered in patients at risk for hepatitis B reactivation or some other opportunistic infections.Citation15,Citation18 However, it should be noted that Nocardia infections might develop while under TMP/SMX prophylaxis.Citation25
In conclusion, bortezomib is associated with impaired cellular immunity and lymphopenia and might cause a probensity to Nocardia infections in MM patients. Neurological symptoms should be rigorously evaluated in patients receiving bortezomib and brain abscess should be considered in the differential diagnosis of intracranial mass lesions neurosurgeons should have a high index of suspicion and send samples from the resection material for cultures.
References
- Gozzetti A, Cerase A, Lotti F, Rossi D, Palumbo A, Petrucci MD, et al. Extramedullary intracranial localization of multiple myeloma and treatment with novel agents: a retrospective survey of 50 patients. Cancer 2012;118:1574–84.
- Cerase A, Tarantino A, Gozzetti A. Intracranial involvement in plasmacytomas and multiple myeloma: a pictorial essay. Neuroradiology 2008;50(8):665–74.
- Patriarca F, Zaja F, Silvestri F. Meningeal and cerebral involvement in multiple myeloma patients. Ann Hematol. 2001;80(12):758–62.
- Guppy KH, Thomas C, Thomas K, Anderson D. Cerebral fungal infections in the immunocompromised host: a literature review and a new pathogen – Chaetomium atrobrunneum: case report. Neurosurgery 1998;43(6):1463–9.
- Nishimoto T, Monden S, Watanabe K. A case of brain abscess associated with asymptomatic multiple myeloma. No Shinkei Geka. 2003;31(12):1303–7.
- Al-Khatti AA, Al-Tawfiq JA. Listeria monocytogenes brain abscess in a patient with multiple myeloma. J Infect Dev Ctries. 2010;4(12):849–51.
- Prabhakaran S, Gutin PH, Holodny A, Raizer JJ. Isolated primary intracerebral mycetoma: presenting as a mass lesion in a patient with prostate cancer and multiple myeloma. J Neurooncol. 2005;71(1):49–52.
- Kalambokis GN, Christou L, Tsianos EV. Multiple myeloma presenting with an acute bacterial infection. Int J Lab Hematol. 2009;31(4):375–83.
- Pratt G, Goodyear O, Moss P. Immunodeficiency and immunotherapy in multiple myeloma. Br J Haematol. 2007;138(5):563–79.
- Mamelak AN, Obana WG, Flaherty JF, Rosenblum ML. Nocardial brain abscess: treatment strategies and factors influencing outcome. Neurosurgery 1994;35(4):622–31.
- Nucci M, Anaissie E. Infections in patients with multiple myeloma in the era of high-dose therapy and novel agents. Clin Infect Dis. 2009;49(8):1211–25.
- Zangari M, van Rhee F, Anaissie E. Eight-year median survival in multiple myeloma after total therapy 2: roles of thalidomide and consolidation chemotherapy in the context of total therapy 1. Br J Haematol. 2008;141(4):433–44.
- Kim SJ, Kim K, Kim BS, Korean Multiple Myeloma Working Party. Bortezomib and the increased incidence of herpes zoster in patients with multiple myeloma. Clin Lymphoma Myeloma. 2008;8(4):237–40.
- Jung SH, Bae SY, Ahn JS. Lymphocytopenia is associated with an increased risk of severe infections in patients with multiple myeloma treated with bortezomib-based regimens. Int J Hematol. 2013;97(3):382–87.
- Basler M, Lauer C, Beck U, Groettrup M. The proteasome inhibitor bortezomib enhances the susceptibility to viral infection. J Immunol. 2009;183(10):6145–50.
- Mya DH, Han ST, Linn YC, Hwang WY, Goh YT, Tan DC. Risk of hepatitis B reactivation and the role of novel agents and stem-cell transplantation in multiple myeloma patients with hepatitis B virus (HBV) infection. Ann Oncol. 2012;23(2):421–6.
- Beysel S, Yeğin ZA, Yağci M. Bortezomib-associated late hepatitis B reactivation in a case of multiple myeloma. Turk J Gastroenterol. 2010;21(2):197–8.
- Piro E, Kropp M, Cantaffa R, Lamberti AG, Carillio G, Molica S. Visceral leishmaniasis infection in a refractory multiple myeloma patient treated with bortezomib. Ann Hematol. 2012;91(11):1827–8.
- Lakhmi V, Umabala P, Anuradha K. Microbiological spectrum of brain abscess at a tertiay care hospital in South India: 24-year data and review. Pathol Res Int. 2011;16:1–12.
- El-Herte R, Kanj SS, Araj GF, Chami H, Gharzuddine W. First report of Nocardia asiatica presenting as an anterior mediastinal mass in a patient with myasthenia gravis: a case report and review of the literature. Case Report in İnfectious Dieaes. 2012;16:1–4.
- Moon JH, Cho WS, Kang HS, Kim JE. Nocardia brain abscess in a liver transplant recipient. J Korean Neurosurg Soc. 2011;50(4):396–98.
- Alp E, Yıldız O, Aygen B, Sümerkan B, Sarı I, Koç K, et al. Disseminated nocardiosis due to unusual species: two case report. Scand J Infect Dis. 2006;38(6–7):545–8.
- Kageyama A, Yazawa K, Ishikawa J, Hotta K, Nishimura K, Mikami Y. Nocardial infections in Japan from 1992 to 2001, including the first report of infection by Nocardia transvalensis. Eur J Epidemiol. 2004;19(4):383–9.
- Vickrey E, Allen S, Mehta J, Singhal S. Acyclovir to prevent reactivation of varicella zoster virus (herpes zoster) in multiple myeloma patients receiving bortezomib therapy. Cancer 2009;115(1):229–32.
- Barnaud G, Deschamps C, Manceron V. Brain abscess caused by Nocardia cyriacigeorgica in a patient with human immunodeficiency virus infection. J Clin Microbiol. 2005;43(9):4895–7.