?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
The vast majority of acute diarrheal diseases are self-limiting and do not require treatment on a regular basis. Empirical antibiotics should only be used to treat dysenteric and invasive bacterial diarrhea. Antibiotic misuse in the treatment of acute diarrhea is widespread in clinical practice worldwide. Hence, the purpose of this study was to examine the pattern of antibiotic use for the acute diarrheal diseases at Hiwot Fana Specialized University Hospital, Harar, Ethiopia.
Methods
A retrospective, institution-based cross-sectional study was conducted to investigate the antibiotic utilization pattern for the treatment of acute diarrheal diseases from September 1 to September 30, 2022. Data were obtained retrospectively from patient cards treated for diarrheal disorders from August 1, 2021 to August 31, 2022, using standardized questionnaires, and the analysis was performed using IBM SPSS Statistics version 27.
Results
Among 332 patients in present study, 271 (81.63%) of them received nine different types of antibiotics, with the most commonly prescribed drugs were Cotrimoxazole (30.26%), Ciprofloxacin (19.19%), and Azithromycin (17.71%). Based on the presence of blood in the stools, 14.76% of the cases were invasive bacterial in nature. Antibiotics were prescribed about 2.55 times more frequently to patients under the age of 12 than to subjects 65 and older (AOR 2.55, 95% CI 1.45–3.87). Patients who received three or more medications were 2.77 times more likely to be prescribed antibiotics (AOR 2.77, 95% CI 1.84–7.56). For every unit increase in the number of drugs prescribed, the odds of prescribing antibiotics increased by 2.44 units (COR 2.44; 95% CI 2.06–4.32).
Conclusions
The current study found that antibiotics were overused in both adults and children with acute diarrheal diseases at Hiwot Fana Specialized University Hospital. The number of antibiotics prescribed was significantly associated with the patient’s age and the number of medications prescribed. To reduce antibiotic overuse, health professionals have to follow the national standard treatment guidelines.
Background
Antibiotics are medicines that are currently used worldwide to treat bacterial infections in both humans and animals [Citation1, Citation2]. They work by killing the bacteria or making it difficult for bacteria to proliferate and flourish [Citation3, Citation4]. A new antibiotic is brought onto the market frequently, leaving doctors little time to thoroughly familiarize themselves with the new medications while also allowing microbes plenty of opportunities to evolve various forms of resistance to secure their survival [Citation5]. Antibiotics can be lifesaving in the treatment of bacterial infections and are the most commonly prescribed drugs among all medications. Their indiscriminate use increases the risk of antibiotic resistance, necessitating more cautious prescribing for the treatment of bacterial infections [Citation6–Citation8].
Antibiotics agent misuse raises therapy costs, adverse drug reactions (ADRs), and patient mortality [Citation9]. Inappropriate antibiotic use is defined as using antibiotics in a way that minimizes the therapeutic effects while increasing toxicity and resistance development. In Ethiopia, there is evidence of antibiotic misuse by healthcare providers, unskilled practitioners, and drug consumers. These, together with the rapid spread of resistant bacteria and insufficient surveillance, will exacerbate the problem [Citation10, Citation11]. Several studies have found various types of antibiotic misuse in hospital settings in both developing and developed countries, which raises the costs of treating bacterial infections and increases antibiotic resistance [Citation12–Citation16].
Diarrhea is regarded the passing of three or more loose or liquid stools per day. The passing of formed stools on a regular basis is not diarrhea, nor is the passing of loose, “pasty” stools by breastfed babies [Citation17]. There are three distinct clinical kinds of diarrhea: acute bloody diarrhea, commonly known as dysentery; acute watery diarrhea, which lasts several hours or days; and persistent diarrhea, which lasts 14 days or longer [Citation18]. Viruses are the main cause of acute diarrhea both in developed and underdeveloped nations, especially during the winter. No matter the etiology or severity of the process, supportive rehydration therapy is the cornerstone of treatment, and its fast and early adoption is linked to a positive outcome. It should also be combined with proper nutritional support [Citation7, Citation19].
Since pathogens cannot be identified in more than 90% of diarrhea cases, empirical antibiotic therapy is advised. The clinical value of empiric antibiotic therapy should, however, be evaluated against the risk of side effects and the possibility of removing healthy bacteria [Citation20]. Resistance is frequently linked to increased antibiotic use in hospitals. The rates of resistance shown in multidrug-resistant nosocomial infections are significantly influenced by the usage patterns of antibiotics [Citation21–Citation23]. The expense of treatment has gone up along with the increased morbidity and mortality in many patients due to the rising resistance [Citation10, Citation22]. The ability of the underprivileged population to access contemporary healthcare will unquestionably be compromised by rising healthcare costs. Furthermore, most hospitals in developing countries had a higher than 30% rate of improper antibiotic use [Citation24].
Antibiotic use is estimated to be inappropriate in 20–50% of cases, according to estimates [Citation25]. This leads to more side effects, higher costs, and a high rate of antibiotic resistance (AMR) in community infections [Citation25]. In severe diarrhea, antibiotics are most commonly misused for viral and self-limiting illnesses. About 70–80% of all diarrheal episodes are caused by viral infections, such as rotavirus [Citation26]. Due to the self-limiting nature of acute diarrhea, complexity and length of time required to identify the pathogen, routine use of antibiotics is not advised in the majority of cases [Citation27]. In a joint statement released in 2004, the World Health Organization (WHO) and the United Nations International Children’s Emergency Fund (UNICEF) suggested treating severe diarrhea in children with the low-osmolality oral rehydration solution (ORS) and zinc tablet [Citation28].
Only in cases of serious bloody diarrhea or dysentery are antibiotics advised. Unfortunately, reports from several parts of the world indicated that improper use of antibiotics in the management of diarrhea is widespread [Citation29]. To support the implementation of antibiotic stewardship programs (ASP) in various healthcare settings, antibiotics utilization pattern indicators could be assessed as useful standards [Citation30–Citation32]. For the purpose of developing a regional intervention program to encourage responsible use of antibiotics, prevent the spread of Antimicrobial Resistance (AMR), and lower the cost of acute diarrhea therapy, it is critical to understand the scope and pattern of antibiotic use for acute diarrhea in the community. As a result, this study was carried out at Hiwot Fana Specialized University Hospital, to analyze the pattern of antibiotic use for the treatment of acute diarrheal diseases.
Methods
Study setting and period
This study was carried out at Hiwot Fana Specialized University Hospital, a comprehensive teaching hospital for Haramaya University located in Harar town, 526 km to the east of Ethiopia’s capital, Addis Ababa. It is now the primary teaching and referral hospital in the country’s eastern region. Internal medicine, gynecology, obstetrics, surgery, dentistry, antenatal care, ophthalmology, hospital pharmacy, dermatology, and an antiretroviral therapy clinic are among the services provided by the hospital. From September 1 to September 30, 2022, a cross-sectional study design was used to assess the antibiotics utilization pattern for the management of acute diarrheal diseases in this hospital.
Study design
An institution-based cross-sectional study was conducted retrospectively, using quantitative approach to assess antibiotic utilization pattern for the treatment of acute diarrheal disease.
Source population
The source was all diarrheal patient records at Hiwot Fana Specialized University Hospital.
Study population
The study included patient charts used for the diagnosis and treatment of acute diarrheal disease at Hiwot Fana Specialized University Hospital from August 1, 2021 to August 31, 2022.
Sample size determination and sampling technique
To obtain the largest possible minimum sample size for this study, it was calculated using the single population proportion formula, assuming a 95% confidence interval, a 5% margin of error, and a prevalence of 50% and calculated with following formula:where n = sample size, Z
1−α/2 = standard normal variable at (1 − α) % confidence level and α (level of significance) was taken to be 5% (95% confidence level is used = 1.96), P = prevalence rate estimate for the population (50%), d = margin of the tolerated sampling error (0.5)
As a result, the n value was calculated and found to be around 384. The number of medical cards (population size, N) of patients who were treated for acute diarrheal disease within study period was 3752. Since the population size was less than 10,000 (N = 3752), a reduction formula was utilized using STAT CALC of Epi Info software and the actual sample size was found to be about 332. A systematic sampling technique was used to identify the patient charts. The sampling interval was determined by dividing the total number of patient charts by the sample size, yielding the interval (k = 11), and every 11th chart was selected. The first patient chart was chosen by lottery from the first to the eleventh patient chart, based on the time order of the records.
Data collection tools and procedures
Data abstraction formats were used to collect data retrospectively. The information acquired included the patients’ sociodemographic and clinical features, as well as patterns of antibiotic use over the study period. The patient chart, laboratory data, and medications were all utilized, as well as the prescriber profile. The data collection approach includes essential points that can quantitatively address main drug usage issues during antibiotic use. Every relevant fact was captured in the patient’s medication records.
Study variables
Explanatory variables included gender, age, duration, prescriber’s profession, and laboratory tests of stool characteristics, while the dependent variable was antibiotic utilization pattern.
Data processing and analysis
IBM SPSS Statistics version 27 was used to process and analyze the collected data. To provide the frequency and percentage distributions of the variables included in the study, descriptive statistics were used, followed by cross-tabulation. The outcome was presented in the form of narratives, tables, and figures.
Data quality control
A pretest was performed at the Jinela Health Center to determine whether the data collection format was valid and reliable, and the completeness of the data collection format was checked prior to the actual data collection. Data cleaning was also performed accordingly.
Results
Sociodemographic characteristics of the patients
There were 3752 patient records documented as diagnosed with acute diarrheal diseases within study period (August 1, 2022 to August 31, 2022). A total of 332 patient records were included in the study. Among 332 patients, 183 (55.12%) were males and 149 (44.88%) were females. Children under 5 years of age were 48.80% and patients > 65 years were 6.63% (Table ).
Table 1 Sociodemographic characteristics of the acute diarrhea patients at Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
Clinical characteristics
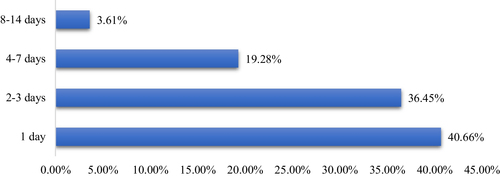
A review for the history of the cases shows that, 121 (36.45%) patients had experienced the illness for 2–3 days (Fig. ). Most patients reported diarrhea-related illnesses, such as fever 142 (42.77%), vomiting 194 (58.43%), cough 23 (6.93%), chills 7 (2.11%), headache 29 (8.74%), abdominal cramps 109 (32.83%) and loss of appetite 26 (7.83%). From all patients, 84 (25.31%) of them had mild to moderate dehydration, while six patients (1.81%) had severe dehydration, which required intravenous fluid therapy.
Stool characteristics
From 332 patients, 237 (71.38%) patients had a stool examination ordered and 119 (50.21%) stool specimens were recorded positive as 81 (34.18%) were with unspecified bacteria and 57 (24.05%) contain amoeba, giardia, and ascariasis. Majority, 85.24% of stools were non-bloody and 14.76% have blood in stools (Fig. ). The percentage of patients with bloody diarrhea that has received antibiotics was (100%), watery (86.26%) and mucoid (64.36%) (Table ).
Fig. 2 Stool characteristics of patients diagnosed with the acute diarrhea at Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
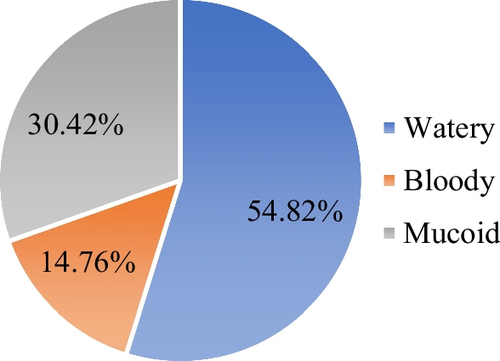
Table 2 Antibiotics prescription by age groups and stool characteristics for acute diarrhea patients at Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
Treatment patterns of acute diarrheal diseases
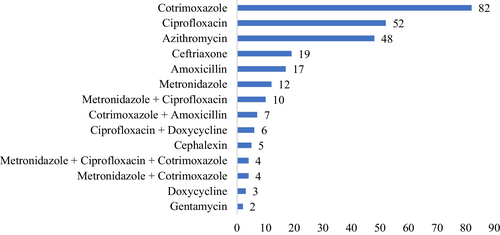
The patient’s record shows that, the number of antibiotics prescribed for single patient ranged from 1 to 3 drugs. About 81.63% of cases received at least one antibiotic drug, while 18.37% of them received no antibiotics. Specifically, 72.28% of patients received one, 8.13% received 2, and 1.21% received 3 antibiotics during the episode of diarrhea. There are nine types of antibiotics that prescribed for acute diarrhea treatment. Cotrimoxazole (30.26%), Ciprofloxacin (19.19%), Azithromycin (17.71%), Ceftriaxone (7.01%) and Amoxicillin (6.27%) were the most frequently prescribed antibiotics. In the same manner, of 162 under five children, 136 (83.95%) were prescribed with at least one antibiotic (Table ). Of 332 patients, 151 (49.83) patients were prescribed with ORS, while 6 patients prescribed with IV fluid for treatment of dehydration. Other medications prescribed were; Paracetamol 139 (41.87%), Albendazole 23 (6.93%), Mebendazole 17 (5.12%), Ibuprofen 16 (4.83%), Diclofenac 14 (4.22%), Multivitamin 11 (3.31%), Tramadol 10 (3.01%), Metoclopramide 9 (2.71%), Omeprazole 7 (2.11%), Tinidazole 7 (2.111%), and Hyoscine 5 (1.51%) (Fig. ).
Adherence to standard treatment guidelines
The adherence to Standard Treatment Guideline (STG) was routinely assessed to show the appropriateness of antibiotics prescribing pattern. The result shows that 116 (34.94%) cases were treated in line with STG, while 216 (65.06%) cases were not treated according to National Standard Treatment Guideline recommendations (Table ).
Table 3 Antibiotic utilization patterns based on STG for acute diarrheal diseases in Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
Prescriber profile on acute diarrheal diseases
Most of the acute diarrheal patients were treated by Medical Interns, 149 (44.88%), General Practitioners, 61 (18.37%) and Nurses, 61 (18.37%). About 44 (13.25%) of patient records had no name of prescribers. The better proportion of antibiotic prescription in line with STG was among Senior Physicians (64.71%) and General Practitioners (55.74%), while Nurses (75.41%) and Medical Interns (65.77%) prescriptions were not in line with National Standard Treatment Guideline recommendations (Table ).
Table 4 Antibiotic usage for the acute diarrheal diseases of health professionals in Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
Antibiotic prescribing predictors
At the bivariate level, the predictors of antibiotic prescribing, age (P = 0.013) and number of medicines prescribed (P < 0.006), were significantly associated with antibiotic prescribing. Antibiotic drugs were 2.46 times more likely to be given to patients under the age of 12 than to patients 65 and older (AOR 2.46, CI 1.23–4.36). When compared to those who received one or two antibiotics per prescription, those who received three or more drugs per prescription were more likely to receive an antibiotic. Hence, patient taking four drugs have more than three times probability of antibiotic prescribed for them (AOR 3.25, CI 1.51–33.52) (Table ).
Table 5 Bivariate analysis of predictors of the prescribed antibiotics for acute diarrheal disease in Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
The full analysis model fitness test was performed to confirm the suitability and found analysis model containing all predictors was statistically significant, χ 2 (5, N = 332) = 76.95, P < 0.001, indicated that the model was able to distinguish between the respondents who had been prescribed antibiotics and those who had not. Hosmer and Lemeshow test also supported the model fitness (χ 2 = 6.382, df = 6, P = 0.613). The model as a whole also explained between 58.4% (Cox and Snell R square) and 78.1% (Nagelkerke R square) of the variance in antibiotic prescription and correctly classified 64.33% of those who had one. According to the model’s sensitivity, it correctly identified 59.6% of the group with antibiotic prescribed. Furthermore, the specificity was 67.4%. Age (P = 0.011) and number of medicines prescribed (P < 0.002) significantly associated with antibiotic prescribing after adjusting for potential confounders using multivariate logistic regression (Table ). There is a significant increase in antibiotic prescribing with an increase in the number of medicines prescribed (P < 0.002). The odds of prescribing antibiotics increased by 2.44 units for every unit increase in the number of medicines prescribed (COR 2.44; 95% CI 2.06–4.32).
Table 6 Multivariate analysis of predictors of the prescribed antibiotics for acute diarrheal disease in Hiwot Fana Specialized University Hospital; August 1, 2021 to August 31, 2022
Discussion
General prescribing pattern
This institution-based cross sectional study has investigated the pattern of antibiotic use for acute diarrheal diseases in Hiwot Fana Specialized University Hospital, Harar, Ethiopia. In the present study, 81.63% of patients have received at least one antibiotic drug. This result is slightly lower than study done at Bishoftu General Hospital, Ethiopia which was 86.8% [Citation33] and far higher than the findings of the studies carried out in different parts of the world such as India with 71% [Citation34], China 60.8% [Citation35], and Thailand 45.1% [Citation36] that had received an antibiotic drug for acute diarrheal disease. There could be a number of causes for the high prescription rate for antibiotics. The high level of routine empirical treatments observed in resource-poor nations is primarily a result of the increased occurrence of infectious diseases in developing countries, which increases the number of antibiotics prescribed [Citation37]. The other factor can be patient pressure on doctors [Citation38].
Antibiotic self-medication was reported to be common and about 44–45.1% in Ethiopia and Eritrea, according to several studies and a comprehensive review [Citation39–Citation41]. This finding may indicate that patients are more likely to directly or indirectly request antibiotic prescriptions from doctors as they are heavily involved in self-medicating with antibiotics [Citation42]. The trend of King Chulalongkorn Memorial Hospital, Thailand with better prescribing pattern may be due to advanced practice and knowledge toward antibiotics rational use, enhanced education and control of over the counter drugs and better trend of following the standard treatment guideline recommendations [Citation36].
For the 332 patients treated for acute diarrhea that were included in the current study, a total of 737 medications were prescribed, resulting in an average of 2.72 drugs per prescription, which is similar to study done in south India with 2.7 [Citation43], but much higher than the WHO standard (1.6–1.8) [Citation44], as well as some results from the comparable investigations carried out across Ethiopia, which revealed an average of 1.64–1.90 medications per encounter [Citation45–Citation52]. However, when compared to several other study results from Ethiopia, Sudan, India, and Saudi Arabia, which were found an average value of 2.02–4.2 medicines per encounter, this number is the comparable one [Citation30, Citation31, Citation53–Citation60]. This shows that, prescribers should restrict medicine prescriptions to only patients that are absolutely essential, because polypharmacy can expose patients to unfavorable drug effects and raise patient costs.
The percentage of encounters in this study when at least one antibiotic was prescribed was 41.52%, which is much higher than the WHO standard value of 20–26.2%. This result is comparable with study done in Bahawalpur, Pakistan which was 48.6% [Citation61]. Similar studies carried out in various nations indicated that a percentage of encounters with antibiotics were between 9.1 and 38.4%, which is less than the result reported by the current study [Citation31, Citation43, Citation47, Citation48, Citation56]. On the other hand, the result is lower than those of other comparable studies with a range of 52.3–75.1% [Citation51, Citation52, Citation54, Citation55, Citation59, Citation61, Citation62].
In present study, 83.95% of children under 5 years with acute diarrhea have received at least one antibiotic drug which is lower than study done in Bishoftu General Hospital, Ethiopia with 92.6% [Citation33]. However, higher than the findings of the studies conducted in Central Region Province of Thailand, Delhi, India, and Puducherry, India, where the percentage of patients prescribed on antibiotics were 72.6%, 64%, and 22%, respectively [Citation63–Citation65]. The percentage of acute diarrheal patients treated not in line with STG was 65.06%, which is slightly better than other study done in Bishoftu, Ethiopia with 72.3% [Citation33]. However, the result is higher in percentage than the finding of the study carried out in China at 51.3% [Citation35] and Thailand at 48.9% [Citation36]. However, other study conducted in South Thailand, indicated that 73.8% of antibiotics prescribed were in line with STG for diarrheal disease treatment [Citation66]. The most commonly prescribed drugs for acute diarrheal diseases were Cotrimoxazole (30.6%), Ciprofloxacin (19.19%) and Azithromycin (17.71%) in the present study. The finding is different from other study conducted in Thailand [Citation63] and Ethiopia [Citation33] as both studies indicated greater than 50% prescription was only Cotrimoxazole.
Antibiotic prescribing predictors
This study discovered a significant correlation between patient age and number of medications for antibiotics prescribed. Antibiotic prescriptions were found to be associated with being under the age of 12 as they got the highest proportion of antibiotics when compared to the other patient categories which is similar to research from Eritrea [Citation40], Bangladesh [Citation67], Yemen [Citation68], and Cameroon [Citation69]. According to the results of the current study, prescribing three or more medications per prescription was highly associated with prescribing antibiotics.
Antibiotics were about 2.55 times more likely to be prescribed to patients under the age of 12 than to subjects of 65 years and older (AOR 2.55, 95% CI 1.45–3.87). When compared to subjects who received one or two drugs per prescription, those who received more than two drugs were 2.77 times more likely to receive an antibiotic (AOR 2.77, 95% CI 1.84–7.56). The odds of prescribing antibiotics were increased by 2.44 units for every one unit increase in the number of medicines prescribed (COR 2.44; 95% CI 2.06–4.32). It is consistent with study done in Asmara, which found that probabilities increased by 2.02 for every one-unit increase (P < 0.001; OR 2.02; 95% CI 1.62–2.52) [Citation40] and Zambia, where it was shown that odds rise by 2.7 for every one-unit increase (P < 0.001; OR 2.68, 95% CI 2.20–3.25) [Citation70].
The current study limitation is that, it was conducted in only one hospital and so cannot be generalized to other facilities. However, because Hiwot Fana Specialized University Hospital is the only tertiary hospital in the research area, the current study can provide a picture of how antibiotics are used in East Ethiopia. This study discovered a significant incidence of incorrect antibiotic use, which may fuel rising antimicrobial resistance and associated costs on a national and worldwide scale. In general, the study determined the prevalence of antibiotic use, identified the types of antibiotics used in the treatment of acute diarrheal illness, and rated prescribers’ adherence to standard treatment guidelines.
Conclusion
The present study revealed that there was high overuse of antibiotics for both adults and children with acute diarrheal disease in Hiwot Fana Specialized University Hospital. The most common antibiotics prescribed were Cotrimoxazole, Ciprofloxacin and Azithromycin. The proportion of prescriptions containing an antibiotic was 41.52%, which is much higher than WHO-recommended standard (20–26.2%). The average number of prescriptions per encounter fell just short of WHO recommendations, and adherence to the Standard Treatment Guideline (STG) was also inadequate. Antibiotic prescribing revealed a strong correlation with patient age and the number of medications per prescription. Thus, to reduce antibiotics overuse, health professionals have to follow the national standard treatment guidelines.
Author contributions
BD, SY, ZK and AM contributed to the original idea. BD and SY drafted the manuscript. ZK and AM participated in drafting the manuscript. BD and ZK developed the survey tool. BD and ZK collected the data with data collectors. BD performed data analysis and drafted the results. SY and AM critically reviewed and edited the manuscript. BD oversaw the entire project, from survey tool development to data analysis. The final manuscript was reviewed by all of the authors. All authors read and approved the final manuscript.
Declarations
Ethics approval and consent to participate
The study protocol was approved by the Research and Ethics Committee of Dire Dawa University’s College of Medicine and Health Science (DDU/REC/P/096/22). To protect study participants’ privacy and the confidentiality of personal data, the names of study participants were withheld from the data collection format and all others procedures were carried out in accordance with the applicable guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they do not have any competing interests.
Abbreviations
| ADR | = | Adverse drug reaction |
| AMR | = | Antimicrobial resistance |
| ASP | = | Antimicrobial Stewardship Program |
| EML | = | Essential Medicine List |
| ORS | = | Oral rehydration salt |
| STG | = | Standard treatment guideline |
| UNICEF | = | United Nations International Children’s Emergency Fund |
| WHO | = | World Health Organization |
Acknowledgements
The authors would like to thank the Hiwot Fana Specialized University Hospital Management and Record Department for their permission and support in carrying out the study, as well as all staff at the working card center who assisted us greatly in data collection. Our deep appreciation also goes to data collectors.
Funding
This study received no specific funding from public, commercial, or not-for-profit funding agencies.
Availability of data and materials
On reasonable request, the data used and analyzed during this study can be obtained from the corresponding author.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Cunha CBAntimicrobial Stewardship Programs: principles and practiceMed Clin North Am2018102797803 30126571 10.1016/j.mcna.2018.04.003
- Katzung BGBasic and clinical pharmacology201714New YorkMcGraw-Hill Education
- Browne AJ, Chipeta MG, Haines-Woodhouse G, et al.Global antibiotic consumption and usage in humans, 2000–18: a spatial modelling studyLancet Planet Heal20215e893e904 10.1016/S2542-5196(21)00280-1
- Hutchings MI, Truman AW, Wilkinson BAntibiotics: past, present and futureCurr Opin Microbiol2019517280 1:CAS:528:DC%2BC1MXitV2msbjP 31733401 10.1016/j.mib.2019.10.008
- Kotwani A, Wattal C, Joshi PC, Holloway KIrrational use of antibiotics and role of the pharmacist: an insight from a qualitative study in New Delhi, IndiaJ Clin Pharm Ther201237308312 1:STN:280:DC%2BC38zlsFeitA%3D%3D 21883328 10.1111/j.1365-2710.2011.01293.x
- Nicolini G, Sperotto F, Esposito SCombating the rise of antibiotic resistance in childrenMinerva Pediatr2014663139 1:STN:280:DC%2BC2crhs1ehtA%3D%3D 24608580
- Meisenheimer ES, Epstein C, Thiel DAcute diarrhea in adultsAm Fam Physician20221067280 35839362
- Zinner SHAntibiotic use: present and futureNew Microbiol200730321325 1:CAS:528:DC%2BD2sXhtVWnsr3L 17802919
- Patel N, Patel D, Desai HAntimicrobial utilization pattern among pediatric inpatients of a tertiary care hospital in Central GujaratNatl J Physiol Pharm Pharmacol201991
- World Health OrganizationWHO expert committee on specifications for pharmaceutical preparations. World Health Organization technical report series2011GenevaWorld Health Organization
- DACA. Antimicrobial use, resistance and containment baseline survey syntheses of finding. 2009;1–160.
- Silva ML, Cargnello C, Aulois-Griot M, Dumartin CAntibiotic misuse: how to evaluate the costs?Med Mal Infect201949485494 1:STN:280:DC%2BB3M%2Fitl2rsg%3D%3D 30954321 10.1016/j.medmal.2019.03.012
- Kaier KEconomic implications of the dynamic relationship between antibiotic use and hospital-acquired infectionsValue Health2012158793 22264976 10.1016/j.jval.2011.09.005
- Stein K, Farmer J, Singhal S, Marra F, Sutherland S, Quiñonez CThe use and misuse of antibiotics in dentistry: a scoping reviewJ Am Dent Assoc2018149869884.e5 30261952 10.1016/j.adaj.2018.05.034
- Machowska A, Stålsby Lundborg CDrivers of irrational use of antibiotics in EuropeInt J Environ Res Public Health2018 10.3390/ijerph16010027 30583571 6338985
- Chen J, Sidibi AM, Shen X, Dao K, Maiga A, Xie Y, Hesketh TLack of antibiotic knowledge and misuse of antibiotics by medical students in Mali: a cross-sectional studyExpert Rev Anti Infect Ther202119797804 1:CAS:528:DC%2BB3MXktVKmsg%3D%3D 33251896 10.1080/14787210.2021.1857731
- Valerie Nemeth; Nicholas Pfleghaar. Diarrhea—StatPearls—NCBI Bookshelf. StatPearls Publishing. 2021.
- Gessesse DN, Tarekegn AAPrevalence and associated factors of diarrhea among under-five children in the Jawi district, Awi Zone Ethiopia, 2019. Community based comparative cross-sectional studyFront Pediatr20221019 10.3389/fped.2022.890304
- Goodgame RWViral causes of diarrheaGastroenterol Clin North Am200130779795 1:STN:280:DC%2BD3MrktVChtQ%3D%3D 11586557 10.1016/S0889-8553(05)70210-7
- Istúriz RE, Carbon CAntibiotic use in developing countriesInfect Control Hosp Epidemiol200021394397 10879571 10.1086/501780
- Yates RRNew intervention strategies for reducing antibiotic resistanceChest199911524S27S 1:STN:280:DyaK1M7otF2ntQ%3D%3D 10084456 10.1378/chest.115.suppl_1.24S
- Patterson JEAntibiotic utilizationChest2001119426S430S 1:STN:280:DC%2BD3M7ltFSmug%3D%3D 11171780 10.1378/chest.119.2_suppl.426S
- Weinstein RAControlling antimicrobial resistance in hospitals: infection control and use of antibioticsEmerg Infect Dis20017188192 1:STN:280:DC%2BD3MzpsFShuw%3D%3D 11294703 2631704 10.3201/eid0702.010206
- Farthing M, Salam MA, Lindberg G, Dite P, Khalif IS-LEAcute diarrhea in adults and children: a global perspective. World Gastroenterology Organisation global guidelinesJ Clin Gastroenterol2012471220 10.1097/MCG.0b013e31826df662
- Steinman MA, Gonzales R, Linder JA, Landefeld CSChanging use of antibiotics in community-based outpatient practice, 1991–1999Ann Intern Med200313819911999
- Thapar N, Sanderson IRDiarrhoea in children: an interface between developing and developed countriesLancet2004363641653 14987892 10.1016/S0140-6736(04)15599-2
- Wingate D, Phillips SF, Lewis SJ, Malagelada JR, Speelman P, Steffen R, Tytgat GNJGuidelines for adults on self-medication for the treatment of acute diarrhoeaAliment Pharmacol Ther200115773782 1:CAS:528:DC%2BD3MXks1Kisbc%3D 11380315 10.1046/j.1365-2036.2001.00993.x
- Walker CLF, Fontaine O, Young MW, Black REZinc and low osmolarity oral rehydration salts for diarrhoea: a renewed call to actionBull World Health Organ200987780786 2755312 10.2471/BLT.08.058990
- Bhatnagar S, Lodha R, Choudhury P, Sachdev HPS, Shah N, Narayan S, Wadhwa N, Makhija P, Kunnekel K, Ugra DRecommendations IAP guidelines 2006 on management of acute diarrheaIndian Pediatr200744380 17536143
- Atif M, Azeem M, Saqib A, Scahill SInvestigation of antimicrobial use at a tertiary care hospital in Southern Punjab, Pakistan using WHO methodologyAntimicrob Resist Infect Control20176112 10.1186/s13756-017-0199-7
- Atif M, Sarwar MR, Azeem M, Umer D, Rauf A, Rasool A, Ahsan M, Scahill SAssessment of WHO/INRUD core drug use indicators in two tertiary care hospitals of Bahawalpur, Punjab, PakistanJ Pharm Policy Pract2016918 10.1186/s40545-016-0076-4
- Ahmadi F, Zarei EPrescribing patterns of rural family physicians: a study in Kermanshah Province, IranBMC Public Health20171717 10.1186/s12889-017-4932-1
- Tulu S, Tadesse T, Alemayehu Gube AAssessment of antibiotic utilization pattern in treatment of acute diarrhoea diseases in Bishoftu General Hospital, Oromia EthiopiaAdv Med2018201816 10.1155/2018/2376825
- Pathak D, Pathak A, Marrone G, Diwan V, Lundborg CSAdherence to treatment guidelines for acute diarrhoea in children up to 12 years in Ujjain, India—a cross-sectional prescription analysisBMC Infect Dis20111119 10.1186/1471-2334-11-32
- Hou FQ, Wang Y, Li J, Wang GQ, Liu YManagement of acute diarrhea in adults in China: a cross-sectional surveyBMC Public Health2013 10.1186/1471-2458-13-41 24321034 3979040
- Supcharassaeng S, Suankratay CAntibiotic prescription for adults with acute diarrhea at King Chulalongkorn Memorial Hospital, ThailandJ Med Assoc Thail201194545550
- Castelnuovo GEmpirically supported treatments in psychotherapy: towards an evidence-based or evidence-biased psychology in clinical settings?Front Psychol20101110
- Stivers T, Timmermans SArriving at no: patient pressure to prescribe antibiotics and physicians’ responsesSoc Sci Med2021290 34006432 10.1016/j.socscimed.2021.114007
- Ateshim Y, Bereket B, Major F, Emun Y, Woldai B, Pasha I, Habte E, Russom MPrevalence of self-medication with antibiotics and associated factors in the community of Asmara, Eritrea: a descriptive cross sectional surveyBMC Public Health201919726 10.1186/s12889-019-7020-x 31182071 6558833
- Amaha ND, Weldemariam DG, Abdu N, Tesfamariam EHPrescribing practices using WHO prescribing indicators and factors associated with antibiotic prescribing in six community pharmacies in Asmara, Eritrea: a cross-sectional studyAntimicrob Resist Infect Control2019817 10.1186/s13756-019-0620-5
- Mekonnen S, Getnet M, Dumessa EEpidemiology of self-medication in Ethiopia: a systematic review and meta-analysis of observational studiesBMC Pharmacol Toxicol201819112
- Tesfamariam S, Anand IS, Kaleab G, Berhane S, Woldai B, Habte E, Russom MSelf-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, EritreaBMC Public Health20191919 10.1186/s12889-019-6470-5
- Ps P, Rudra JT, Vasanthi P, Sushitha U, Sadiq MJ, Narayana GAssessment of drug use pattern using World Health Organization core drug use indicators at Secondary Care Referral Hospital of South IndiaCHRISMED J Health Res20152223 10.4103/2348-3334.158683
- Ghei PHow to investigate drug use in health facilities. Selected drug use indicatorsHealth Policy (New York)19953473 10.1016/0168-8510(95)90068-3
- Bekele NA, Tadesse JPrescription auditing based on World Health Organization (WHO) prescribing indicators: a case of Dilla University referral hospitalJ Drug Deliv Ther201882125 10.22270/jddt.v8i6-s.2165
- Admassie E, Begashaw B, Hailu WAssessment of drug use practices and completeness of prescriptions in Gondar University Teaching Referral HospitalIJPSR20134265275
- Asrade BAssessment of completeness of prescription and rational drug use practice at Felege Hiwot Referral Hospital, North West EthiopiaJ Health Med Nurs2019601625
- Yilma Z, Mekonnen T, Siraj EA, Agmassie Z, Yehualaw A, Debasu Z, Tafere C, Ararsie MAssessment of prescription completeness and drug use pattern in Tibebe-Ghion comprehensive specialized hospital, Bahir Dar, EthiopiaBiomed Res Int2020 10.1155/2020/8842515 33134391 7593717
- Desalegn AAAssessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital, south Ethiopia: a cross-sectional studyBMC Health Serv Res2013 10.1186/1472-6963-13-170 23647871 3651314
- Tigist G, Yohannes T, Mekonnen SEvaluation of the prescribing practice based on World Health Organization core prescribing indicators in Hiwot Fana Specialized University Hospital, Harar, eastern EthiopiaJ Drug Deliv Ther201662530
- Dessie B, Atalaye G, Diress E, Getahun APractice towards rational drug use at Finotselam and Asirade Zewudie Hospitals based on WHO core drug use indicators, Northwest EthiopiaSci World J2020202015 10.1155/2020/1634294
- Kasahun GG, Demoz GT, Asayehegn AT, Gebrehiwot LG, Tesfay GM, Desta DMEvaluation of pattern of drug use in tertiary health care setting in central Tigray using WHO prescribing indicatorsAdv pharmacoepidemiol drug saf202092285
- Mengistu G, Misganaw D, Tsehay T, Alemu BK, Bogale KAssessment of drug use pattern using WHO core prescribing indicators at outpatient settings of governmental hospitals in dessie townDrug Healthc Patient Saf202012237244 33273863 7708261 10.2147/DHPS.S266749
- Gashaw T, Sisay M, Mengistu G, Amare FInvestigation of prescribing behavior at outpatient settings of governmental hospitals in eastern Ethiopia: an overall evaluation beyond World Health Organization core prescribing indicatorsJ Pharm Policy Pract201811111 10.1186/s40545-018-0152-z
- Rabie D, Kheder SI. Assessment of prescribing and dispensing practices based on WHO core prescribing indicators in hospital and community pharmacies in Khartoum State—Sudan. 2020.
- Mahmood A, Elnour AA, Ali AAA, Hassan NAGM, Shehab A, Bhagavathula ASEvaluation of rational use of medicines (RUM) in four government hospitals in UAESaudi Pharm J201624189196 27013912 10.1016/j.jsps.2015.03.003
- Mamo DB, Alemu BKRational drug-use evaluation based on world health organization core drug-use indicators in a Tertiary Referral Hospital, Northeast Ethiopia: a cross-sectional studyDrug Healthc Patient Saf2020121521 1:CAS:528:DC%2BB3cXhtFGktLnE 32021478 6970620 10.2147/DHPS.S237021
- Akodo J, Chijioke-Nwauche IEvaluation of drug use pattern in Lulu Brigg’s Health Centre, University of Port Harcourt, Nigeria using WHO, prescribing indicatorsPharmainnov J20176506510
- Sisay M, Mengistu G, Molla B, Amare F, Gabriel TEvaluation of rational drug use based on World Health Organization core drug use indicators in selected public hospitals of eastern Ethiopia: a cross sectional studyBMC Health Serv Res20171719 10.1186/s12913-017-2097-3
- Yousif BME, Supakankunti SGeneral practitioners’ prescribing patterns at primary healthcare centers in national health insurance, Gezira, SudanDrugs Real World Outcomes20163327332 27747832 5042943 10.1007/s40801-016-0087-0
- Atif M, Sarwar MR, Azeem M, Naz M, Amir S, Nazir KAssessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, PakistanBMC Health Serv Res20161619 10.1186/s12913-016-1932-2
- Shelat PR, Kumbar SKAnalysis of out door patients’ prescriptions according to World Health Organization (WHO) prescribing indicators among private hospitals in Western IndiaJ Clin Diagn Res20159FC01-4 25954629
- Howteerakul N, Higginbotham N, Dibley MJAntimicrobial use in children under five years with diarrhea in a central region province, ThailandSoutheast Asian J Trop Med Public Health200435181187 1:STN:280:DC%2BD2czntVWnsw%3D%3D 15272767
- Singh J, Bora D, Sachdeva V, Sharma RS, Verghese TPrescribing pattern by doctors for acute diarrhoea in children in Delhi, IndiaJ Diarrhoeal Dis Res199513229231 1:STN:280:DyaK28vjsF2guw%3D%3D 8838825
- Priyadarshini K, Raj V, Balakrishnan SAudit of use of antibiotics and zinc supplement in childhood diarrheaJ Pharmacol Pharmacother20134204205 23960426 3746304 10.4103/0976-500X.114601
- Osatakul S, Puetpaiboon AAppropriate use of empirical antibiotics in acute diarrhoea: a cross-sectional survey in southern ThailandAnn Trop Paediatr200727115122 17565808 10.1179/146532807X192480
- Syed A, Mosaddek MPrescribing practice of antibiotics for outpatients in Bangladesh: rationality analysisAm J Pharmacol201811008
- Alshakka M, Said K, Babakri M, Ansari M, Aldhubhani A, Azmi Hassali M, Mohamed Ibrahim MIA study on antibiotics prescribing pattern at outpatient department in four hospitals in Aden-YemenJ Pharm Pract Community Med201628893 10.5530/jppcm.2016.3.5
- Chem ED, Anong DN, Akoachere JFKTPrescribing patterns and associated factors of antibiotic prescription in primary health care facilities of Kumbo East and Kumbo West Health Districts, North West CameroonPLoS ONE201813118 10.1371/journal.pone.0193353
- Lukali V, Michelo CFactors associated with irrational drug use at a district hospital in Zambia: patient record-based observationsMed J Zambia2015422530