Abstract
Background
Acute coronary syndrome (ACS) is the principal cause of death in developing countries including Ethiopia. No study reports the overall patterns of risk factors and burden of in-hospital mortality in Ethiopia. This study, therefore, aimed to assess the magnitude of risk factors, management, and in-hospital mortality of ACS in Ethiopia.
Methods
Electronic searching of articles was conducted using PubMed, Science Direct, EMBASE, Scopus, Hinari, and Google Scholar to access articles conducted in Ethiopia. The Preferred Reporting Items for Systematic Reviews checklist was used for identification, eligibility screening, and selection of articles. Data were extracted with an abstraction form prepared with Microsoft Excel and exported to STATA for analysis. Funnel plot, Begg’s test, and Egger’s test were used to determine publication bias. Heterogeneity between the studies was checked by I2 statistic. The pooled prevalence of risk factors and in-hospital mortality of ACS were estimated using a random-effects meta-analysis model.
Results
Most (59.367%) of the patients had ST-segment elevation myocardial infarction (STEMI). Hypertension (54.814%) was the leading risk factor for ACS followed by diabetes mellitus (38.549%). Aspirin (56.903%) and clopidogrel (55.266%) were most frequently used in patients with STEMI ACS, respectively. The pooled proportion of in-hospital mortality of ACS was 14.82% which was higher in patients with STEMI (16.116%).
Conclusion
The rate of in-hospital mortality is still high which was higher in patients with STEMI. Initiation of treatment must consider the heterogeneity of each patient’s risk factor and reperfusion therapy should be implemented in our setting.
Supplementary Information
The online version contains supplementary material available at https://doi.org/10.1186/s40545-023-00603-7.
Introduction
Acute coronary syndrome (ACS) is a coronary artery disease caused by narrowing or blockage of the coronary artery lumen, resulting in myocardial ischemia or infarction due to insufficient coronary blood perfusion [Citation1, Citation2]. ACS, including unstable angina (UA), ST-elevation myocardial infarction (STEMI), and non-ST-elevation myocardial infarction (NSTEMI) is the main cause of cardiovascular death and disability in the world [Citation3, Citation4]. It is associated with an average of 7.4 million deaths worldwide, 21–22% of all deaths in Europe, and 6–10% of death in sub-Saharan Africa [Citation5, Citation6].
It is an emergency, life-threatening condition, and financial catastrophe due to high out-of-pocket expenditures for in-hospital care [Citation7, Citation8]. Even though, there is advancement in diagnosis and management of ACS, still it is the most common cause of death around the globe including in Ethiopia [Citation9, Citation10]. A study done at Addis Cardiac Hospital, Ethiopia showed that among 300 cardiac patients, 162 (53.7%) of them had ACS [Citation11]. Moreover lower-income countries are facing a double burden of disease because of the higher prevalence of both communicable and non-communicable diseases particularly cardiovascular diseases [Citation10]. These result in frequent hospitalizations, high mortality rate, stretching the already limited resources, and are associated with worse treatment outcomes [Citation9, Citation12].
Even though ACS is a common health problem with devastating consequences, its burden and risk factors are different according to geographical variation [Citation13, Citation14]. Previous study in sub-Saharan Africa reported that diabetes, hypertension and cigarette smoking still account for the most common predisposing risk factors [Citation6]. Dyslipidemia, obesity, advanced age, family history of ischemic heart disease and sedentary life style are other most common risk factors reported from different studies [Citation2, Citation7, Citation10, Citation13]. More than 90% of risk factors are potentially modifiable risk factors using pharmacological and non-pharmacological methods. However, it is difficult to achieve these outcomes in resource-limited countries because of insufficient laboratory setup, lack of reperfusion therapy, cost of medications, and discontinuity of care [Citation11, Citation15, Citation16]. Though several scholars attempted to describe the extent of risk factors, management and in-hospital mortality due to acute coronary syndrome in Ethiopia, there is no a nationwide study on this area; which is an important research gap. Meta-analysis is a key to improving the accuracy of estimates through the use of more data sets. Therefore, this study was aimed to determine the overall magnitude of risk factors, management, and in-hospital mortality of acute coronary syndrome in Ethiopia.
Materials and methods
Search strategy
This systematic review and meta-analysis were conducted and reported per the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA, 2009) requirements for observational studies [Citation17] (Additional file 1). An electronic search for studies was done by two (BK and MG) of the authors from October 15 to November 30, 2021. PubMed, Science Direct, EMBASE, Cochrane Database, Sci-Hub, Scopus, Africa journal of online library, Hinari, and Google Scholar for free articles were searched. In addition, Addis Ababa, Jimma, and Gondar Universities’ institutional repositories were considered to address unpublished articles in Ethiopia. The searching process was carried out using the full title (“Magnitude of Risk Factors, Management and in Hospital Mortality of Acute coronary syndrome in Ethiopia”) and then keywords (magnitude, risk factors, treatment, mortality, acute coronary syndrome, coronary heart disease, Ethiopia). These different keywords were used individually and in combination using Boolean operators “OR, AND or NOT” as well as medical subject heading [MeSH] terms). In addition, searching reference lists of all the included studies (snowball technique) was done to retrieve other studies that are not addressed by our searching stratagem.
Study selection criteria
All available studies and data were incorporated based on the following predefined eligibility criteria.
Inclusion criteria
Study setting and period: All studies conducted in Ethiopia from 2000 to November 30, 2021.
Study design: All facility-based observational studies.
Study population: Age ≥ 18 years old.
Article types: The published and unpublished studies reporting the risk factors of ACS, management, and/or in-hospital mortality.
Language: All searches were limited to articles written in the English language.
Exclusion criteria
We excluded reviews and systematic review articles, case reports, and case series. In addition, articles available only in abstract form were excluded because it was difficult to evaluate their quality and extract all necessary information. In the case of duplicates, only the most recent or most complete publication for each data set for a specific outcome was selected.
Outcome variables
The main outcome of this study was the rate of in-hospital mortality. Other secondary outcomes include magnitudes of risk factors and in-hospital management of ACS.
Data extraction
Essential data were extracted from eligible studies by using Microsoft Excel 2019 spreadsheet format. To ensure data quality and methodological validity, two authors (BK and MG) retrieved the data independently. Data were extracted using the PRISMA standard data extraction format. The following information was considered during data extraction: The last name of the first author and year of publication, the region of the study conducted, study design and period, total sample size, sex, types of ACS, risk factors of ACS, the medication used, overall in-hospital mortality and mortality in each type of ACS. Any discrepancies in the data extraction process were solved through discussion involving all authors.
Quality assessment tools
Data extraction was accompanied by two authors independently according to the Critical Appraisal Checklist recommended by the Joanna Briggs Institute (JBI) [Citation18]. The JBI checklist was composed of ten questions, the scores ranged from zero to ten. The studies which obtained more than 60% were considered as good quality studies. None of them had poor quality status and all of them were included in the present inquiry. In addition, the Alberta Heritage Foundation for Medical Research (AHFMR) standard quality assessment criteria for primary research papers was used to check the quality of included articles [Citation19]. Accordingly, the quality of articles was stated as high, moderate and, poor quality with respective scores of ≥ 70%, 51–69%, and ≤ 50%.
Moreover, the disagreements were resolved by consensus and decided by taking the average score of the two reviewers.
Statistical analysis
Data were extracted by using Microsoft excel 2010 format and exported to STATA 14.0 (STATA, College Station, TX, USA) for further analysis. Data were pooled and a random effect meta-analysis with an estimation of DerSimonian and Laird method was applied to determine the pooled prevalence of risk factors, and in-hospital mortality of ACS, and the result was presented using forest plot and odds ratio (OR) with a 95% confident interval (CI), which were used to report the magnitude of the risk factors and mortality in the results of meta-analyses. The pooled prevalence of risk factors and pooled magnitude of in-hospital mortality of ACS were calculated as a weighted average of the individual summary risk factors and a weighted average of the individual summery mortality or ORs), respectively. Similarly, odds ratio of risk factor is simply defined as the ratio of the odds of the risk factor in group (studies) to the odds of the studies without that particular risk factor. Heterogeneity between studies was assessed by computing Chi-square (I2) test statistics. The I2 values of 0, 25, 50, and 75% were considered as no, low, moderate, and high heterogeneities, respectively [Citation20]; unfortunately, in our study, there was high heterogeneity between the original studies (I2 = 95.6%, p < 0.001). Subgroup analysis was considered to examine how medications are used and in hospital, mortality varies across different studies based on types of ACS. Begg’s funnel plot and Egger's regression were used to check publication bias and a p-value less than < 0.05 was considered statically significant. [Citation21]
Results
Characteristics of studies included in the analysis
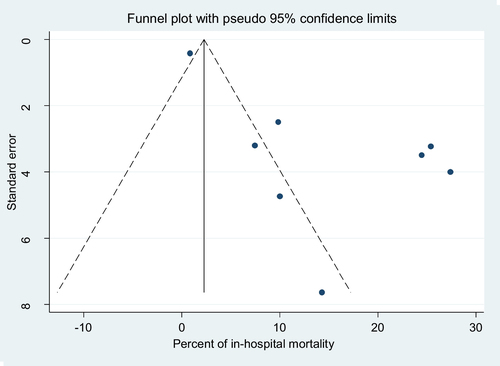
We identified a total of 271 published and 4 from gray literature through database searches. After duplicate papers were removed and a thorough reading of articles’ abstracts, 24 studies were assessed with the eligibility criteria. Accordingly, 16 irrelevant articles were excluded because they did not qualify the eligibility criteria set. Hence, a total of 8 studies were included in the final analysis as they met the inclusion criteria (Fig. ). The articles were published between 2013 and 2021; however, there is one unpublished article that was obtained from the Addis Ababa University repository. The result of both Begg’s and Egger’s tests showed that there was considerable publication bias at < 0.001 p-values and < 0.006, respectively, and assessment of publication bias using a funnel plot in (Fig. ). Most of the studies (6/8, 75%) were cross-sectional studies, others were longitudinal or retrospective follow-up studies.
Fig. 1 Flow diagram of literature search and study selection based on Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA)
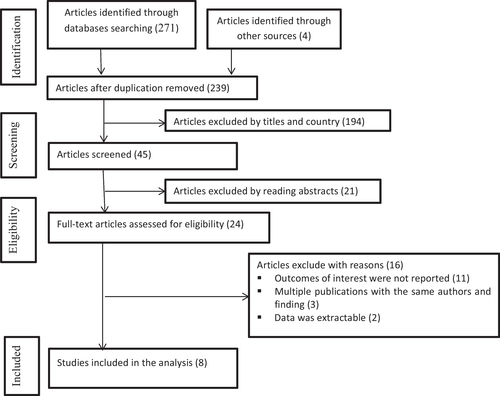
Fig. 2 Funnel plot for the publication bias of the included studies for overall all in-hospital mortality
More than one-half of the studies were conducted in Addis Ababa city (n = 6) others were conducted in the Oromia region (n = 1), and Tigray region (n = 1). Of a total of 1197 study participants, 813(67.92%) of them were females (Additional file 2). Out of the eight studies included in this review and meta-analyses five studies were single-center [Citation22–Citation26] while the rest three being multi-center. All patients presented with acute coronary syndrome were included in all the eight studies as the number of patients in respective hospitals was limited. Only one study [Citation24] was found to be moderate quality (68.18%) when evaluated with a checklist for assessing the quality of quantitative studies adopted from Kmet and Robert (Additional file 2); whereas, the rest articles had high-quality score.
With regard to diagnostic types of ACS, majority of patients had STEMI (59.367%, 95% CI: 44.558–74.176) followed by NSTEMI (23.365%, 95% CI: 16.559–30.171) and then UA (19.899%, 8.092–31.706) (Table ).
Table 1 Characteristics of studies included in the meta-analysis
Magnitudes of risk factors of ACS in Ethiopia
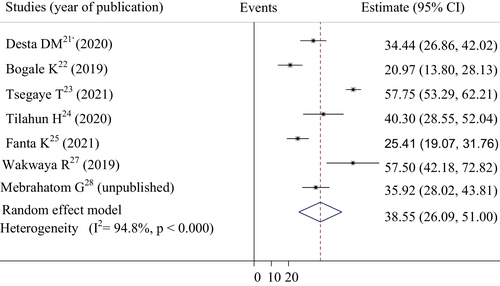
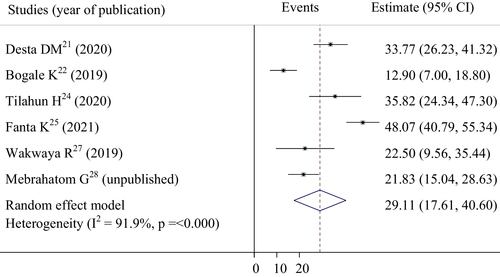
Patterns of risk factors among ACS patients in selected studies are shown in Table and Additional file 2. Hypertension, diabetes mellitus, and dyslipidemia were the three most prevalent risk factors of ACS in Ethiopia, respectively. A total of 7 studies with 1176 study participants were included to assess the pooled magnitude of hypertension, and diabetes mellitus among ACS patients. Accordingly, our pooled analysis showed that more than one-half (54.814%, 95% CI: 45.158–64.470) of ACS patients had hypertension (Fig. ). The pooled prevalence of diabetes mellitus in this systematic review and meta-analysis, we found that was 38.549% (95% CI: 26.095–51.004) (Fig. ). To determine the pattern of dyslipidemia among ACS patients, a total of 2018 participants were included. Consequently, the result showed that nearly one-third of ACS patients (29.108%, 95% CI: 17.612–40.604) had dyslipidemia (Fig. ).
Table 2 Pooled prevalence of risk factors among ACS patients in Ethiopia
Fig. 3 Forest plot of the pooled estimate of percentage hypertension among acute coronary syndrome patients in selected studies
In-hospital management of ACS based on types of ACS in Ethiopia
To determine the medication use pattern, we conducted a subgroup analysis based on diagnostic types of ACS. Anti-platelets, aspirin [56.903% (95% CI: 38.032–75.774)] and clopidogrel [55.266% (95%CI: 35.946–74.58)] were most frequently used in patients with STEMI than NSTEMI and UA. Similarly, more than one-half of patients with STEMI received beta-blockers (BBs) and statins. Primary percutaneous coronary intervention (PCI) was done in 24.558% (95% CI: 3.495–45.621) of patients with STEMI. Patients with UA had most (17.908%) commonly used anti-pain including morphine or fentanyl as compared to patients with NSTEMI (12.009%). Calcium channel blockers were prescribed inpatient with STMEI and UA almost in similar proportion (Additional file 2, Table ).
Table 3 Subgroup analysis of articles describing medications used based on types of ACS
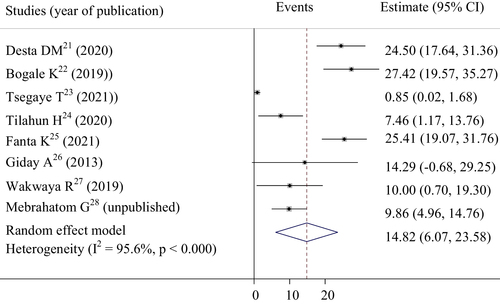
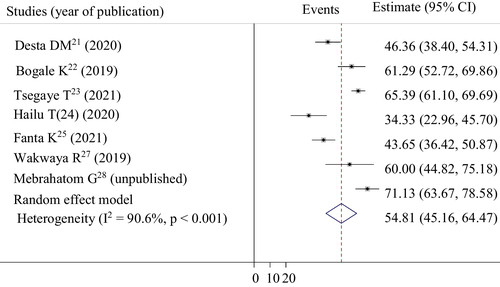
In-hospital mortality of patients with ACS in Ethiopia
In this meta-analysis, we used a total of 1197 ACS patients to determine the overall mortality rate of ACS in Ethiopia. Accordingly, the pooled magnitude of in-hospital mortality of ACS was 14.82% (95% CI: (6.06–23.57) (Fig. ). Results observed from subgroup analysis showed that in-hospital mortality was greatly varied across different types of ACS. The result indicated that patients with STEMI the highest magnitude of in-hospital mortality was reported in which was 16.156% (95% CI: 9.729–22.503) (Table ).
Table 4 Subgroup analysis of studies included on in-hospital mortality by types of ACS
Discussion
Currently, ACS is the leading cause of morbidity, mortality, and, high healthcare cost expenditure in resource-limited countries including Ethiopia. Identification of the risk factors of ACS may be important for clinicians and clinical pharmacists to set effective education programs and appropriate initial treatment. This review summarized magnitudes of risk factors, treatment approach, and prevalence of in-hospital mortality among patients with ACS in Ethiopia. Accordingly, the results of this study indicated that hypertension was the most commonly noted risk factor (54.814%) for ACS among included studies. The result was in line with studies conducted in Canada (59.7%), Sweden (58%), Greece (58.8%), and Kenya (55.56) [Citation30–Citation33].
In contrast, the proportion of hypertension observed in this systematic review and meta-analysis was lower than in studies done in Slovakia (83.5%) and Albania (90.6%) [Citation11, Citation14]. This variation might be due to lack of diagnostic modalities and proficiency in our setting. On the other hand, a study conducted in Mexico showed that cigarette smoking (69.1%), hypertension (57.8%), and dyslipidemia (47.5%) were the three most prevalent risk factors among patients with ACS [Citation34]. Similarly, a study done in South Africa among Asian Indian patients showed that 82% of ACS patients had visceral obesity as the number one risk factor and 60% of participants were cigarette smokers (60%) [Citation35]. Our findings indicated that the prevalence of smoking and obesity were 19.985%, and 15.663%, respectively. Difference in genetic makeup and lifestyle condition might be the possible cause of variations. Diabetes mellitus and dyslipidemia were also the major risk factors for ACS, accounted 38.549%, and 29.108% of risk factors, respectively. A study conducted in Iran showed that the prevalence of hyperlipidemia was 45.9%, and diabetes mellitus was 31.1% [Citation36]. Similarly a report from Japan, Prevention of Atherothrombotic Incidents Following Ischemic Coronary Attack (PACIFIC) Registry, indicated that dyslipidemia and diabetes mellitus were the main risk factors of ACS, 67.2% and 35.0%, respectively [Citation37]. In addition, many other worldwide studies explained dyslipidemia and diabetes mellitus as common risk factors [Citation15, Citation31, Citation32, Citation34]. These might be because dyslipidemia and diabetes mellitus have co-existed risk profiles and associated structural and functional changes in the cardiovascular system with devastating clinical complications [Citation8, Citation13].
Pharmacological and invasive procedural therapy including percutaneous coronary intervention (PCI) or fibrinolysis is very essential to decrease in-hospital mortality [Citation15, Citation30]. The finding of our study revealed that anti-platelets including aspirin and clopidogrel were most frequently used in patients with STEMI than the other two types of ACS, 56.903% and 55.266%, respectively. These were very lower as compared to finding from the Saudi project for assessment of coronary events (SPACE) registry, 98.4%, and 80.1%, respectively [Citation38]. The use of aspirin and clopidogrel were also lower than in studies conducted in Iran (99.4% vs. 98.1%), Brazil (97.6% vs. 88.3%), and Spain (98.0% vs. 97.8%) [Citation36, Citation39, Citation40]. This may give insight into the presence of gaps in the use of guideline-directed in-hospital management of ACS in Ethiopia which might be interesting for the future researcher. Different guidelines including the 2020 European Society of Cardiology Clinical Practice Guidelines recommended antiplatelet for all patients with ACS without contraindications, regardless of the type of ACS or the management strategy [Citation41]. Antiplatelet are the cornerstone of ACS management because they significantly reduce the composite outcome of cardiovascular death, myocardial infarction, and stroke. It also considerably lowers the risk of recurrent ischemic events, including stent thrombosis [Citation31, Citation42].
The use of beta-blockers in STEMI was 51.591% which was lower than studies from Iran (90.9%) and Brazil (80.9%) [Citation36, Citation39]. The same is true for the use of statins, which was 51.803%. This was also lower than findings from India (84.3%), and Japan (80. 4%) [Citation7, Citation37]. This variation might be due to differences in access to care, underlying risk factors, costs, and inconstant availability of drugs in Ethiopia. PCI is the most effective reperfusion therapy for symptomatic ACS patients admitted within 90 h [Citation16]. However, only 24.558% of patients with STEMI received PCI therapy. The result was much lower as compared to studies conducted in Poland (55.5%) and Saudi Arabia (42.6%) [Citation9, Citation38]. Importantly; this result was scored in the absence of using a fibrinolysis agent in Ethiopia. This might be because of problems with PCI service accessibility, limited interventional cardiologists, and delayed admission time to the hospital (range from 4 to 7 days) [Citation22, Citation28]. Now a day, there are only two PCI-centered public hospitals in Ethiopia [Citation43].
In this review, the overall in-hospital mortality due to ACS was 14.82%. The finding was in line with studies conducted in Pakistan (12.2%), Kenya (17%), and sub-Saharan African countries (10%) [Citation44–Citation46]. In contrast, in-hospital mortality found in this study was higher as compared to studies conducted in India (3.9%), China (7.66%), Netherland (3.7%), and Iraq (7.7%) [Citation7, Citation47–Citation49]. The possible causes of variation might be because of delayed initiation of diagnostic and treatment options in our setting. In addition, it might be due to the better availability of reperfusion therapy (PCI, coronary artery bypass graft, and thrombolytic therapy) in those listed countries. Patients with STEMI had higher (16.15%) rate of in-hospital mortality. In contrast, in a study in a central European country, results of the CZECH-2 registry, the rate of mortality was higher in patients with NSTEMI (8.4% for NSTEMI patients, 7.3% for STEMI patients) [Citation50]. The variation might be due to the majority of patients in our study having STEMI (59.367%). The other possible reason for the higher mortality rate in STEMI subtypes of ACS might be the presence of complete blockage of the coronary artery as compared to partial occlusion in NSTEMI and UA.
Limitations of the study
This systematic review and meta-analysis are not free from limitations. The first one is due to the presence of a weak database management system in our country, there may be data not accessible by our search strategy and therefore important measurements, particularly on mortality in each type of ACS might have been missed. In addition, most of the studies done in Ethiopia did not consider the specific name of the medication, dose, and duration of treatment. Due to these, we did not systematically capture data on these key parameters which might have been useful for creating better predictions on in-hospital management of ACS. Moreover, as the study relies on the articles conducted in Ethiopia with variability in study methodologies, the pooled prevalence estimates and conclusions may not be generalized to the rest of the world.
Time to present at a health institution after the onset of signs and symptoms is also a matter which is not addressed by this review. Finally, data were obtained from articles conducted with different methodologies and geographical regions; these may have an impact on the variation in magnitude of risk factors and practice in hospital management. Finally, both published and unpublished articles were included with different methodologies and geographical regions; these may have an impact on the variation in magnitude of risk factors and practice in hospital management.
However, this review provides useful information about the patterns of risk factors that contributed to the development of ACS. Besides, the review provides insight into the burden of ACS-associated mortality at the national level to help policymakers to design cost-effective plans and treatment strategies to combat the ACS burden and improve treatment outcomes.
Conclusion
ACS is a major public health problem in Ethiopia with diverse clinical risk factors. Hypertension was the leading risk factor noted for ACS followed by diabetes mellitus and dyslipidemia. The use of guideline-directed in-hospital management was not comparable to that of registries from different countries in the world. Even though few patients were managed by PCI, we may conclude that the reperfusion therapy rate was almost zero in the absence of a fibrinolysis agent. The rate of in-hospital mortality among ACS patients is still high and the risk of death was higher in patients with STEMI. Initiation of treatment in clinical practice must take into account the heterogeneity of each patient’s risk factor. Health-related policymakers should work on the wide accessibility for the advanced therapies of PCI and thrombolytic following the patients’ socioeconomic status, which ultimately may help improve favorable patients’ in-hospital outcomes.
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit it to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agree to submit this manuscript to journal of SN Comprehensive Clinical Medicine.
Competing interests
The authors declare that they have no conflict of interest.
Supplementary Information
jppp_a_12370155_sm0001.doc
Download MS Word (88.5 KB)jppp_a_12370155_sm0002.xlsx
Download MS Excel (11.2 KB)Funding
Not applicable.
Availability of data and materials
Additional data are supplied as additional material.
Code availability
Not applicable.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Smith JN, Negrelli JM, Manek MB, Hawes EM, Viera AJDiagnosis and management of acute coronary syndrome: an evidence-based updateJ Am Board Fam Med2015282283293 25748771
- Guo JJ, Chen Y, Du W, Peng H, Wang R, Xia Y, Xin P, Wigle PR, Papadimitropoulos EAAntithrombotic therapy and direct medical costs in patients with acute coronary syndrome in Shanghai ChinaValue Health Regional Issues2016199398 1:CAS:528:DC%2BC28XhtFOgu77N
- Shehab A, Al-Dabbagh B, AlHabib KF, Alsheikh-Ali AA, Almahmeed W, Sulaiman K, Al-Motarreb A, Nagelkerke N, Suwaidi JA, Hersi A, Faleh HAGender disparities in the presentation, management, and outcomes of acute coronary syndrome patients: data from the 2nd Gulf Registry of Acute Coronary Events (Gulf RACE-2)PLoS ONE201382e55508 23405162 3566183 1:CAS:528:DC%2BC3sXivFGqtbs%3D
- Zhang H, Goodman SG, Yan RT, Steg PG, Kornder JM, Gyenes GT, Grondin FR, Brieger D, DeYoung JP, Gallo R, Yan ATIn-hospital management and outcomes of acute coronary syndromes in relation to prior history of heart failureEur Heart J Acute Cardiovasc Care201653214222 25766512
- Rayner M, Petersen S. European cardiovascular disease statistics 2000 edition. British Heart Foundation. 2000;14–35.
- Shavadia J, Yonga G, Otieno HA prospective review of acute coronary syndromes in an urban hospital in sub-Saharan Africa: cardiovascular topicsCardiovasc J Afr2012236318321 22836154 3734739
- Mohanan PP, Mathew R, Harikrishnan S, Krishnan MN, Zachariah G, Joseph J, Eapen K, Abraham M, Menon J, Thomas M, Jacob SPresentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: results from the Kerala ACS RegistryEur Heart J2013342121129 22961945
- Zubaid M, Rashed WA, Al-Khaja N, Almahmeed W, Al-Lawati J, Sulaiman K, AlMotarreb A, Amin H, Al-Suwaidi J, Al-Habib KClinical presentation and outcomes of acute coronary syndromes in the gulf registry of acute coronary events (Gulf RACE)Saudi Med J20082922534
- Poloński L, Gąsior M, Gierlotka M, Kalarus Z, Cieśliński A, Dubiel JS, Gil RJ, Rużyłło W, Trusz-Gluza M, Zembala M, Opolski GOriginal article Polish Registry of Acute Coronary Syndromes (PL-ACS) Characteristics, treatments and outcomes of patients with acute coronary syndromes in PolandKardiologia Polska (Polish Heart Journal)2007658861872 17853315
- Shashu BA, Ayele MAThe pattern of coronary artery diseases as diagnosed by coronary angiography and the outcome of Percutaneous Coronary Intervention (PCI) in EthiopiaEthiop J Heal Dev20142811216
- Simoni L, Alimehmeti I, Ceka A, Tafaj E, Gina M, Dibra A, Goda AAdmissions and in hospital outcomes of acute coronary syndromes during corona virus disease 19 pandemic in AlbaniaOpen Access Macedonian J Med Sci.202191593599
- Tolla MT, Norheim OF, Verguet S, Bekele A, Amenu K, Abdisa SG, Johansson KAOutof-pocket expenditures for prevention and treatment of cardiovascular disease in general and specialized cardiac hospitals in Addis Ababa, Ethiopia: a cross-sectional cohort studyBMJ Glob Health20172214
- Smith FG, Brogan RA, Alabas O, Laut KG, Quinn T, Bugiardini R, Gale CPComparative care and outcomes for acute coronary syndromes in Central and Eastern European Transitional countries: a review of the literatureEur Heart J Acute Cardiovasc Care201546537554 25214638
- Alberty R, Studenčan M, Kovář FPrevalence of conventional cardiovascular risk factors in patients with acute coronary syndromes in SlovakiaCent Eur J Public Health20172517784 28399360
- Raposeiras-Roubín S, Abu-Assi E, Cabanas-Grandío P, Agra-Bermejo RM, Gestal-Romarí S, Pereira-López E, Fandiño-Vaquero R, Álvarez-Álvarez B, Cambeiro C, Rodríguez-Cordero M, Lear PWalking beyond the GRACE (global registry of acute coronary events) model in the death risk stratification during hospitalization in patients with acute coronary syndromeCardiovasc Intervent201251111171125
- Shashu BA. The management of coronary artery disease in Ethiopia: emphasis on revascularization. Ethiop J Health Sci. 2021;31(2).
- Moher A, Liberati J, Tetzlaff APreferred reporting items for systematic reviews and meta-analyses: the PRISMA statementAnn Internal Med.20091514264269
- Peters M, Godfrey C, McInerney P, Soares C, Khalil H, Parker D. The Joanna Briggs Institute reviewers’ manual 2015: a methodology for JBI scoping reviews.
- Kmet LM, Cook LS, Lee RC. Standard quality assessment criteria for evaluating primary research papers from a variety of fields.
- Rücker G, Schwarzer G, Carpenter JR, Schumacher MUndue reliance on I2 in assessing heterogeneity may misleadBMC Med Res Methodol20088119
- Borenstein M, Hedges LV, Higgins JP, Rothstein HRA basic introduction to fixed-effect and random-effects models for meta-analysisRes Synth Methods20101297111 26061376
- Desta DM, Nedi T, Hailu A, Atey TM, Tsadik AG, Asgedom SW, Kasahun GG, Ayalew ETreatment outcome of acute coronary syndrome patients admitted to Ayder Comprehensive Specialized Hospital, Mekelle, Ethiopia. A retrospective cross-sectional studyPLoS ONE2020152117
- Bogale K, Mekonnen D, Nedi T, Woldu MATreatment outcomes of patients with acute coronary syndrome admitted to Tikur Anbessa Specialized Hospital, Addis Ababa, EthiopiaClin Med Insights Cardiol20191319
- Tsegaye T, Gishu T, Habte MH, Bitew ZWRecovery rate and predictors among patients with acute coronary syndrome in Addis Ababa, Ethiopia: a retrospective cohort studyRes Reports Clin Cardiol20213012921
- Tilahun H, Yadeta D, Roth GPattern, management and outcome of the acute coronary syndrome in an urban hospital in EthiopiaJ Am Coll Cardiol2020751135073508
- Fanta K, Daba FB, Asefa ET, Melaku T, Chelkeba L, Fekadu G, Gudina EKManagement and 30-day mortality of acute coronary syndrome in a resource-limited setting: insight from Ethiopia. A prospective cohort studyFront Cardiovasc Med.2021817
- Giday A, Weldeyes E, O'Mara JCharacteristics and management of patients with acute coronary syndrome at Tikur Anbessa Specialized Hospital, Addis Ababa, EthiopiaEthiop Med J2013514269272 24696977
- Wakwaya RClinical features and outcome of acute coronary syndrome in patients presenting to the emergency department in Addis Ababa, EthiopiaAustin J Cardiovasc Dis Atherosclerosis20196124723568
- Mebrahatom G, Debebe F, Zewdu T. Assessment of clinical profile and outcome of patients with the acute coronary syndrome in Tikur Anbessa and Aabet Hospitals, Addis Abeba, Ethiopia. 2018;15–22
- Wang JY, Goodman SG, Saltzman I, Wong GC, Huynh T, Dery JP, Leiter LA, Bhatt DL, Welsh RC, Spencer FA, Fox KACardiovascular risk factors and in-hospital mortality in acute coronary syndromes: insights from the Canadian global registry of acute coronary eventsCan J Cardiol2015311214551461 26143140
- Rosengren A, Wallentin L, Simoons M, Gitt AK, Behar S, Battler A, Hasdai DCardiovascular risk factors and clinical presentation in acute coronary syndromesHeart200591911411147 16103541 1769064 1:STN:280:DC%2BD2MvjsFOhtg%3D%3D
- Andrikopoulos G, Terentes-Printzios D, Tzeis S, Vlachopoulos C, Varounis C, Nikas N, Lekakis J, Stakos D, Lymperi S, Symeonidis D, Chrissos DEpidemiological characteristics, management and early outcomes of acute coronary syndromes in Greece: the PHAETHON studyHellenic J Cardiol2016573157166 27451914 1:STN:280:DC%2BC2s3kt1KnsA%3D%3D
- Wachira BW, Owuor AO, Otieno HAAcute management of ST-elevation myocardial infarction in a tertiary hospital in Kenya: Are we complying with practice guidelines?Afr J Emerg Med201443104108
- González-Pacheco H, Vargas-Barrón J, Vallejo M, Piña-Reyna Y, Altamirano-Castillo A, Sánchez-Tapia P, Martínez-Sánchez CPrevalence of conventional risk factors and lipid profiles in patients with acute coronary syndrome and significant coronary diseaseTher Clin Risk Manag201410815821 25328397 4199556
- Ranjith N, Pegoraro RJ, Zaahl MGRisk factors associated with acute coronary syndromes in South African Asian Indian patients (The AIR Study)J Clin Exp Cardiol2011216328
- Kassaian SE, Masoudkabir F, Sezavar H, Mohammadi M, Pourmoghaddas A, Kojouri J, Ghaffari S, Sanaati H, Alaeddini F, Pourmirza B, Mir EClinical characteristics, management and 1-year outcomes of patients with the acute coronary syndrome in Iran: the Iranian Project for Assessment of Coronary Events 2 (IPACE2)BMJ Open2015512113
- Daida H, Miyauchi K, Ogawa H, Yokoi H, Matsumoto M, Kitakaze M, Kimura T, Matsubara T, Ikari Y, Kimura K, Tsukahara KManagement and two-year long-term clinical outcome of acute coronary syndrome in Japan-Prevention of AtherothrombotiC Incidents Following Ischemic Coronary Attack (PACIFIC) RegistryCirc J2013774934 23502993 1:CAS:528:DC%2BC3sXmtlWlt7g%3D
- AlHabib KF, Hersi A, AlFaleh H, AlNemer K, AlSaif S, Taraben A, Kashour T, Bakheet A, Al Qarni A, Soomro T, Malik ABaseline characteristics, management practices, and in-hospital outcomes of patients with acute coronary syndromes: results of the Saudi project for assessment of coronary events (SPACE) registryJ Saudi Heart Assoc2011234233239 23960654 3727434
- Mattos LA, Berwanger O, Santos ES, Reis HJ, Romano ER, Petriz JL, Sousa AC, Neuenschwander FC, Guimarães JI, Andrade JPClinical outcomes at 30 days in the Brazilian Registry of Acute Coronary Syndromes (ACCEPT)Arq Bras Cardiol2013100613
- Barrabés JA, Bardají A, Jiménez-Candil J, del Nogal SF, Bodí V, Basterra N, Marco E, Melgares R, de la Hoz JC, Fernández-Ortiz APrognosis and management of acute coronary syndrome in Spain in 2012: the DIOCLES studyRevista Española de Cardiología (English Edition)201568298106
- Nadarajah R, Gale CThe management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: key points from the ESC 2020 Clinical Practice Guidelines for the general and emergency physicianClin Med2021212206209
- Galli M, Andreotti F, D’Amario D, Vergallo R, Vescovo GM, Giraldi L, Migliaro S, Ameri P, Porto I, Crea FAntithrombotic therapy in the early phase of non-ST-elevation acute coronary syndromes: a systematic review and meta-analysisEur Heart J Cardiovasc Pharmacother2020614356 31350546
- Leuner CJ, Weldegerima AHCardiology services in EthiopiaEur Heart J20183926992700 30289516
- Firdous S, Mehmood MA, Malik UValidity of GRACE risk score as a prognostic marker of in-hospital mortality after acute coronary syndromeJ College Phys Surg Pak JCPSP20172710597601
- Bahiru E, Temu T, Gitura B, Farquhar C, Huffman MD, Bukachi FPresentation, management and outcomes of the acute coronary syndrome: a registry study from Kenyatta National Hospital in Nairobi KenyaCardiovasc J Afr2018294225230 29878033
- N'Guetta R, Yao H, Ekou A, N'Cho-Mottoh MP, Angoran I, Tano M, Konin C, Coulibaly I, Anzouan-Kacou JB, Seka R, Adoh AMPrevalence and characteristics of acute coronary syndromes in a sub-Saharan Africa populationAnnales de cardiologie et d’angeiologie20166525963 26988750 1:STN:280:DC%2BC28fht1OntQ%3D%3D
- Wang Y, Fu R, Wang Z, Bao H, Chen Y, Yang F, Luo X, Liu MAssessing the quality of care for patients with acute myocardial infarction in ChinaClin Cardiol2015386327332 26074496 6711066
- Hoedemaker NP, de Winter RJ, van’t Hof A, Kolkman E, Damman POptimal medical therapy prescription in patients with acute coronary syndrome in the Netherlands: a multicenter pilot registryAm J Cardiovasc Drugs2021212219229 32783182 1:CAS:528:DC%2BB3cXhs1ehsr%2FL
- Hamid MBClinical characteristics and outcomes of acute coronary syndromes in a group of Iraqi PatientsIraqi J Med Sci2016144304309
- Tousek P, Tousek F, Horak D, Cervinka P, Rokyta R, Pesl L, Jarkovsky J, Widimsky PCZECH-2 InvestigatorsThe incidence and outcomes of acute coronary syndromes in a central European country: results of the CZECH-2 registryInt J Cardiol20141732204208 24602321