When I began my training in medical oncology 5 years ago, I quickly found myself involved in a Phase III trial of a novel vitamin D analog for patients with advanced, inoperable hepatocellular carcinoma. I must admit to being somewhat surprised that a simple vitamin (albeit a novel analog) was being investigated in the treatment of cancer and more so that it had reached a Phase III trial. But how misplaced was my surprise?
In fact, the link between vitamin D and cancer has been postulated since the 1930s, when Peller and Stephenson first suggested that sunlight exposure may lower the risk of cancer Citation[1]. Since then, much work has been carried out to investigate vitamin D and novel analogs in both the treatment and prevention of cancer. There has been a lot of media interest in this subject recently, and indeed, when ‘googling’ vitamin D, one of the first hits you encounter is an advertisement for vitamin D, stating that it ‘may lower cancer risk’. In this editorial, we will discuss some of the recent evidence looking at the potential role of vitamin D in the treatment and prevention of cancer.
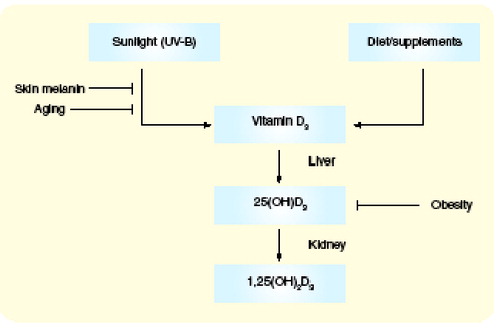
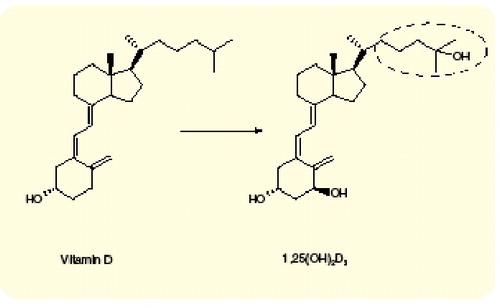
Vitamin D can be obtained from the diet or synthesized in the skin from 7-dihydrocholesterol (to cholecalciferol or vitamin D3) in response to ultraviolet (UV)-B from sunlight. Vitamin D3 is converted from 25-hydroxylated to 25-hydroxycholecalciferol [25(OH)D3] in the liver and from there it is transported to the kidney where it is 1-hydroxylated (by 1α-hydroxylase) to the active form 1,25-dihydroxycholecalciferol [1,25(OH)2D3] . The level of 25(OH)D3 reflects sunlight exposure and dietary intake and is often used as a marker of vitamin D stores. There are, however, only a few foods rich in vitamin D (most notably fatty fish) and therefore dietary vitamin D intake usually comes from fortified dairy products or supplementation. In temperate climates, 90–95% of circulating 25(OH)D3 is derived from sunlight Citation[2].
Vitamin D & its analogs in the treatment of cancer
The discovery of vitamin D receptor (VDR) expression on numerous types of cancer cells stimulated interest in the use of vitamin D as an anticancer agent. It has also been shown that a variety of cancer cells possess 1α-hydroxylase activity, thereby enabling them to convert circulating 25(OH)D3 to 1,25(OH)2D3 (calcitrol). Initial in vitro studies demonstrated that vitamin D could induce differentiation and inhibit proliferation of hematopoietic and cancer cells. However, the potential therapeutic use of vitamin D was limited by its tendency to cause hypercalcemia. The ‘common wisdom’ was that doses of calcitrol sufficient to achieve exposure similar to those seen in in vitro models could not be safely given because hypercalcemia intervened Citation[3]. In the clinical setting, two approaches have been utilized to overcome this problem: the dosing schedule of calcitriol has been altered and novel vitamin D analogs have been developed, which efficiently activate the VDR without inducing hypercalcemia.
Calcitriol
Both alternative routes of administration and intermittent dosing schedules have been explored with calcitriol in an attempt to achieve higher plasma concentrations (preclinical data suggest a strong dose–response relationship). A weekly, oral regimen developed by Beer and colleagues has allowed administration of higher doses (with the desired serum levels achieved) of calcitriol, both as a single agent and in combination with cytotoxic chemotherapy, with acceptable toxicity, in the treatment of androgen-independent prostate cancer. The results have been encouraging [4–6]. Indeed, this is now being investigated in a randomized, placebo-controlled trial. However, one problem facing further trials of oral calcitriol is that, at the dose used in these studies (0.5 µg/kg), patients are required to consume 70–100 capsules at one time, which obviously has significant implications for compliance.
Another regimen being explored is subcutaneous administration on alternate days Citation[7] and, while this seems to allow higher doses, and therefore higher plasma concentrations, data from this regimen are less mature.
Vitamin D analogs
Vitamin D analogs usually differ from naturally occurring vitamin D in their side chain and vary in their ability to bind to the VDR. Hundreds of analogs are under clinical development currently. One of those furthest along in the clinical setting is EB1089, a novel 1,25(OH)2D3 synthetic analog, with strong antiproliferative effects both in vitro and in vivo, combined with a reduced calcemic activity [8–10]. It has been shown to be 50–200-times more potent than 1,25(OH)2D3, with respect to regulation of cell growth and differentiation, in almost every cell type studied Citation[11]. After acceptable toxicity findings in Phase I studies, EB1089 proceeded to two Phase II trials in inoperable hepatocellular carcinoma and inoperable pancreatic cancer [12,13]. While hypercalcemia was still the most commonly experienced significant side effect in both studies, it tended to resolve quickly. There were no objective responses in the pancreatic study, but in the hepatocellular study, two patients achieved complete responses and a further significant number had disease stabilization. Therefore, EB1089 proceeded to a randomized, placebo-controlled, double-blind trial in 747 patients with advanced, inoperable hepatocellular carcinoma, with a primary end point of overall survival Citation[14]. Patients were well matched according to Barcelona Clinic liver cancer (BCLC) staging, age, sex, prevalence of underlying cirrhosis and Okuda stage. Unfortunately, there was no difference in survival observed between the two groups, but EB1089 remains in clinical development in other tumor types.
Vitamin D in the prevention of cancer
Over the past 30 years, many studies have addressed the role of vitamin D in cancer prevention. While these have examined a number of tumor types, the most compelling evidence is in relation to colon cancer, which will be discussed. The studies fall mainly into two groups: those comparing the amount of sunlight with cancer risk and those comparing vitamin D status with cancer risk.
Sunlight & colon cancer risk
Garland and Garland first suggested a link between sunlight and colon cancer in 1980 Citation[15]. They constructed scatter plots of solar radiation in the USA versus colon cancer mortality rate (per 100,000 population), having initially classed all the US states as metropolitan or nonmetropolitan, based on the theory that, in metropolitan areas, shading by structures and a predominance of indoor occupations would alter the amount of solar radiation the population received. They found an inverse association between solar radiation and age-adjusted colon cancer mortality rates for white males residing in metropolitan states but, interestingly, the inverse association noted between solar radiation and age-adjusted colon cancer mortality rates for white males in nonmetropolitan states (where one would assume a greater effect of sunlight on vitamin D status) was less. Since then, further studies (not just in the USA) have supported this link.
Grant also conducted a study investigating geographical variation in cancer mortality rates in the USA and found that 13 different malignancies all exhibited inverse correlations between mortality rates and UV-B radiation Citation[16]. He concluded that the annual number of premature deaths from cancer in the USA due to lower UV-B exposures was 21,700 for white Americans, 1400 for black Americans and 500 for Asian–Americans and other ethnic minorities.
However, using sunlight exposure as a surrogate for vitamin D levels has a number of important drawbacks. In any one area receiving a certain level of solar radiation, each individual’s vitamin D level can vary greatly, depending on many other factors. No two individuals will have equal exposure to the sun, which can be greatly influenced by occupation, behavior related to sun exposure, exercise and even clothing worn. In addition, race is very important, as melanin is a very effective filter against UV-B, and therefore African–Americans have much higher degrees of vitamin D deficiency. Age and body mass index (BMI) also influence the amount of vitamin D synthesis in response to sunlight. Indeed, in one study of plasma vitamin D and colorectal cancer risk, average UV sunlight based on residence was more weakly correlated with 25(OH)D concentrations than were other predictors, such as BMI, physical activity and vitamin D intake Citation[17].
Vitamin D status & colon cancer risk
A number of large, prospective, observational cohort studies have investigated the link between vitamin D status and colon cancer risk, reviewed recently by Gorham and colleagues Citation[2]. Out of four studies that examined measured serum 25(OH)D3 and colon cancer risk, two found a statistically significant correlation and two did not. A total of 14 further studies examined reported vitamin D intake and colon cancer risk. Of these, seven found a statistically significant correlation (although two of these were only significant after certain factors were adjusted for) and seven did not (although some suggested an association that did not reach statistical significance).
The problem with these large cohort observational studies is that they are not designed specifically for this question. They all correct for a variety of factors, including age, BMI, race, aspirin intake, occupation, diet and amount of physical activity, but each study includes different corrective factors. Similarly, many do not take into account the amount of sunlight each individual is exposed to, and with only estimations of actual Vitamin D status, it is difficult to read too much into these findings. However, the authors feel that, based on the cumulative findings from these studies, the National Cancer Institute (NCI) should officially recommend vitamin D supplementation for cancer prevention. This, of course, leads to a further debate with regards to the level of supplementation (although a suggested amount of 1000 IU/day is given by the authors, with fairly sound basis), who to supplement, what age should supplementation begin and how long should the supplementation last, to give but a few examples, all of which would then lead to questions of safety. In fact, Garland and colleagues discuss the safety of chronic vitamin D supplementation in a further review published recently, suggesting that 1000 IU is indeed safe and that potential side effects of vitamin D overdosage, such as bone demineralization, hypercalcemia or nephrocalcinosis, generally only occur with daily dosing in excess of 10000 IU on a chronic basis Citation[18].
Vitamin D: the future
We believe vitamin D (and its analogs) in the treatment of cancer have not yet taken the oncology world by storm, but may have a role in combination with cytotoxic chemotherapy in the future.
In terms of prevention, while one cannot deny that the evidence supporting a link between vitamin D and cancer is compelling, we think the medical community is unlikely to embrace the suggested steps regarding widespread vitamin D supplementation suggested by Gorham and colleagues until a specifically designed, adequately powered, prospective, randomized study, which measures actual vitamin D serum levels, and corrects for all other factors important in vitamin D status provides conclusive proof that vitamin D supplementation does prevent colon (or all) cancer. The question is, would such a trial be feasible? Probably not, although perhaps a formal meta-analysis of the available data would lend weight to the argument.
It has also been suggested that vitamin D may be inversely associated with colonic adenoma recurrence Citation[19] (based on the findings of a study that again used dietary and supplement histories rather than actual vitamin D levels), and here is an area where a randomized, placebo-controlled trial of vitamin D, with a knowledge of actual vitamin D levels, would be a possibility.
References
- Peller S, Stephenson CS. Skin irritation and cancer in the United States Navy. Am. J. Med. Sci. 194, 326–333 (1937).
- Gorham ED, Garland CF, Garland FC et al. Vitamin D and prevention of colorectal cancer. J. Steroid Biochem. Mol. Biol. 97(1–2), 179–194 (2005).
- Mangelsdorf DJ, Thummel C, Beato M et al. The nuclear receptor superfamily: the second decade. Cell 83(6), 835–839 (1995).
- Beer TM, Munar M, Henner WD. A Phase I trial of pulse calcitriol in patients with refractory malignancies: pulse dosing permits substantial dose escalation. Cancer 91(12), 2431–2439 (2001).
- Beer TM, Lemmon D, Lowe BA, Henner WD. High-dose weekly oral calcitriol in patients with a rising PSA after prostatectomy or radiation for prostate carcinoma. Cancer 97(5), 1217–1224 (2003).
- Beer TM, Eilers KM, Garzotto M, Egorin MJ, Lowe BA, Henner WD. Weekly high-dose calcitriol and docetaxel in metastatic androgen-independent prostate cancer. J. Clin. Oncol. 21(1), 123–128 (2003).
- Smith DC, Johnson CS, Freeman CC, Muindi J, Wilson JW, Trump DL. A Phase I trial of calcitriol (1,25-dihydroxycholecalciferol) in patients with advanced malignancy. Clin. Cancer Res. 5(6), 1339–1345 (1999).
- Colston KW, Mackay AG, James SY, Binderup L, Chander S, Coombes RC. EB1089: a new vitamin D analogue that inhibits the growth of breast cancer cells in vivo and in vitro. Biochem. Pharmacol. 44(12), 2273–2280 (1992).
- Haq M, Kremer R, Goltzman D, Rabbani SA. A vitamin D analogue (EB1089) inhibits parathyroid hormone-related peptide production and prevents the development of malignancy-associated hypercalcemia in vivo. J. Clin. Invest. 91(6), 2416–2422 (1993).
- Mathiasen IS, Colston KW, Binderup L. EB 1089, a novel vitamin D analogue, has strong antiproliferative and differentiation inducing effects on cancer cells. J. Steroid Biochem. Mol. Biol. 46(3), 365–371 (1993).
- Hansen CM, Maenpaa PH. EB 1089, a novel vitamin D analog with strong antiproliferative and differentiation-inducing effects on target cells. Biochem. Pharmacol. 54(11), 1173–1179 (1997).
- Dalhoff K, Dancey J, Astrup L et al. A Phase II study of the vitamin D analogue Seocalcitol in patients with inoperable hepatocellular carcinoma. Br. J. Cancer 89(2), 252–257 (2003).
- Evans TR, Colston KW, Lofts FJ et al. A Phase II trial of the vitamin D analogue Seocalcitol (EB1089) in patients with inoperable pancreatic cancer. Br. J. Cancer 86(5), 680–685 (2002).
- Beaugrand M, Sala M, Degos F et al. Treatment of advanced hepatocellular carcinoma by Seocalcitol (a vitamin D analogue): an international randomized double-blind placebo-controlled study in 747 patients. J. Hepatol. 42(Suppl. 2)(17), (Abstract) (2005).
- Garland CF, Garland FC. Do sunlight and vitamin D reduce the likelihood of colon cancer? Int. J. Epidemiol. 9(3), 227–231 (1980).
- Grant WB. An estimate of premature cancer mortality in the US due to inadequate doses of solar ultraviolet-B radiation. Cancer 94(6), 1867–1875 (2002).
- Giovannucci E. The epidemiology of vitamin D and cancer incidence and mortality: a review (United States). Cancer Causes Control 16(2), 83–95 (2005).
- Garland CF, Garland FC, Gorham ED et al. The role of vitamin D in cancer prevention. Am. J. Public Health 96(2), 252–261 (2006).
- Hartman TJ, Albert PS, Snyder K et al. The association of calcium and vitamin D with risk of colorectal adenomas. J. Nutr. 135(2), 252–259 (2005).