Abstract
Thoracoabdominal aortic repair is a high-risk procedure in most experienced centers, not only because of anatomical complexity but also due to the fragility of the patients in whom these aneurysms occur. Such repairs are complex, time-consuming and impose a systemic injury upon the patients, regardless of whether the repair is performed by open surgery or via a fenestrated/branched technique. The substantive risks associated with such repairs include death, dialysis and paralysis. The multilayer flow modulator (MFM) is a disruptive technology which promises a minimally invasive reproducible treatment option, with clinical results demonstrating physiological modulation of the aortic sac with abolition of spinal injury. The mode of action of MFM forces us to completely rethink aneurysm pathogenesis and, consequently, it has been met with much cynicism. We aim to uncloak some of the mystery surrounding the MFM, clarify its mode of action and explore the truth behind its clinical effectiveness.
‘To raise new questions, new possibilities, to regard old problems from a new angle requires creative imagination and marks real advance in science.’
–Albert Einstein, a casualty of aneurysm rupture.
Disruptive technology with multilayer flow modulator (MFM) devices is emerging as an alternative to abrupt aneurysm exclusion and is an unorthodox concept for the management of aneurysmal disease. Patients with thoracoabdominal aortic aneurysm (TAAA) have been classically managed by open surgical repair; but despite surgical advances and the introduction of newer less-invasive techniques, such as hybrid repair or branched endografts, these patients remain a surgical challenge. The high incidence and severity of complications and failure to reproduce acceptable outcomes, even from elite, high-volume centers of excellence, have fueled the drive for a less-invasive, more efficacious and more universally reproducible solution for TAAA repair.
Diverse therapeutic options are offered with the primary aim of preventing aneurysm rupture without compromising branch vessel patency and, thus, preserving distal end-organ perfusion. Although there are no studies that provide direct and objective comparison of the clinical efficacy and/or relative failing of different modalities, trials addressing the individual treatment options are universally disappointing in terms of morbidity and mortality. Currently, clinical practice guidelines do not exist to define the indications for determining which type of intervention is most efficacious or which treatment best suits various patient and/or anatomical characteristics.
Mounting evidence suggests that an aneurysm growth rate based on 3D volume measurements of the abdominal aortic aneurysm and intraluminal thrombus is significantly associated with the need for aortic repair, while the same does not hold for growth rates determined by 2D indices of maximum diameter and intraluminal thrombus thickness Citation[1]. Further still, more sophisticated tools, such as finite element modeling, computational fluid dynamics and individualized fluid suture interaction models using 4D measurements allow for more patient-specific rupture risk analysis.
Contemporary diagnostic tools are now 4D; so, if we can achieve this level of sophistication with imaging, then we must add a similar multiplicity of dimensions to our therapies. Modern therapeutic options should include time as the fourth dimension and try to shift our mindset of instantaneous physical repair, whose long-term outcomes are less than perfect, to a more resilient physiological repair process that lasts.
Aortic aneurysms do not rupture because of tension, pressure or dispensability, that is, increase in sac diameter. Rather, it happens when the stress on the aortic wall at a vulnerable point exceeds the wall’s strength. The development of flow vortices increases peak wall stresses and alters viscoelasticity, plasticity and cellular wall activity; this in turn leads to damage at a particular point on the aneurysm wall Citation[2,3].
The implantation of a covered stent-graft is theoretically thought to reduce stresses and improve hemodynamics to levels similar to those experienced within a normal non-aneurysmal aorta. However, endovascular aortic repair with stiff, noncompliant, covered stent-grafts creates complications due to drag forces acting on the graft and high aortic neck stresses, with the consequences of stent-graft migration and aortic neck dilatation Citation[3,4]. Conversely, the MFM avoids such drawbacks, firstly, because its compliance is similar to that of the native aorta and, secondly, because its propensity for rapid endothelialization means that it quickly becomes embedded within the aortic wall. Therefore, the effect of peak wall stress is grossly diminished Citation[5].
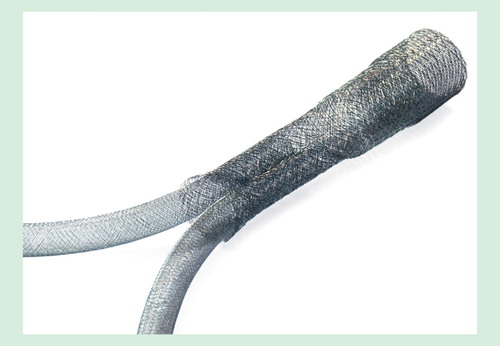
The MFM device is a self-expanding mesh construct of cobalt alloy wires, interconnected in five layers. It is an extremely flexible device with high kinking and fatigue resistance and low total porosity due to its interlocking layers. It channels flow to native side branches and slows the flow vortices within aneurysmal dilatations, leading to the realignment of blood flow. Through this mechanism of flow modulation, the MFM device treats the aneurysm rather than excluding it. A detailed description of the mechanism of action of MFM and its effects on peak wall stress, wall strength, intraluminal thrombus, endothelialization and side branch patency is beyond the scope of the present article, but is described in detail in an editorial by Sultan et al. Citation[5].
Figure 1. Multilayer Flow Modulator device. The flared ends promote aortic wall adherence and reduce the risk of leak at the proximal and distal landing zones.

One of the most promising effects of the MFM is rapid promotion of endothelialization. The endothelium is the most important cell in the vasculature because of its role in vascular hemostasis, cell signaling, smooth muscle cell function and ultimately in arterial healing Citation[6].
The bare metal structure of the MFM provides a framework for organized neointimal growth without occluding side branches. Endothelialization of bare metal stents occurs via three mechanisms: migration of endothelial cells through the stent struts, migration of endothelial and fibroblastic cells from the adjacent aorta at the margins of the stent and through circulating myofibroblasts. The continued laminar flow into major side branches inhibits this process across the branch ostia and maintains patency of the side branches.
The versatility of the MFM is its ability to preserve and enhance flow patterns in arterial side branches. The side branches act as a vacuum, augmenting the lamination and abolishing the vortices, which results in shrinkage of the aneurysm and increased side branch flow. Finite Element Analysis of aneurysms with side branches shows that the MFM eliminates damaging erratic flow vortices by redirecting the flow into laminar flow patterns, thereby reducing peak wall stresses on the aneurysm wall while simultaneously increasing flow into the aneurysm side branches.
Regardless of the mode of repair, the main issues with TAAA repair remain mortality, spinal cord blood supply and visceral hemodynamic compromise. There are specific issues with contemporary endovascular repair relating to the adverse effect on aortic wall compliance, shear stresses and pressures within the aneurysm sac caused by exclusion with relatively stiff, covered endografts, which in turn not only increase rupture risk but also compromise spinal artery perfusion Citation[7,8].
There is mounting evidence to suggest that exclusion of aneurysms may actually subject the sac to greater pressure, inducing an iatrogenically enhanced risk of rupture and pathological loss of branch patency rather than offering the patients a safe aortic repair.
Evidence from the Malmö group Citation[9–15] suggests that stiff, covered endografts, which do not in any way mimic the native arterial wall, may in actual fact have seriously adverse effects on relative intrasac pressures, pulsatile wall motion and spinal perfusion, which can essentially cause more harm than good and enhance rather than decrease the risk of aneurysm rupture and spinal cord ischemia.
Contrary to popular belief, persistent flow between the stent and native wall, that is, endoleak, may in reality be beneficial rather than an adverse prognostic factor in terms of sac expansion. In fact, recognition of the limitations of contemporary endografts has forced investigators to try to overcome such adverse side effects. Lioupis et al. Citation[16] reported the successful investigational use of ‘paraplegia prevention branches’, which intentionally produce temporary endoleak to allow spinal cord perfusion after aneurysm exclusion as an adjuvant to permissive hypertension or spinal fluid drainage. This is a cumbersome approach.
Aneurysm ‘exclusion’ is not the modus operandi of the MFM device; rather, it acts as a scaffold to allow thrombus deposition, endothelialization and flow pattern modulation, while maintaining side vessel patency.
We reported 1-year results from the first subgroup of patients treated with the MFM stent for aortic aneurysm and dissection Citation[17]. The retrospective review encompassed the first 55 of these patients, who were treated on a compassionate basis in 11 countries. There were 31 TAAAs (8 Crawford type I, 3 type II, 9 type III and 11 type IV), 7 arch aneurysms, 3 infrarenal abdominal aortic aneurysms, 8 suprarenal aortic aneurysms and 6 type B dissections. Mean aneurysm diameter was 6.04 ± 1.66 cm and the mean length was 11.58 ± 7.62 cm.
Technical success was 98.2%; there was no paraplegia or perioperative visceral or renal insult. The mean number of side branches covered was 3.7 ± 1.3 per case and 108 stents were deployed. At 1 year, aneurysm-related survival was 93.7%, all-cause survival was 84.8%, intervention-free survival was 92.4%, and all the 202 side branches were patent. There were no stent fractures. At 6 months, the mean rate of sac volume increase was 0.36% per month, resulting in a mean volume increase of 2.14%. At 12 months, the rate of increase had slowed to 0.28% per month, resulting in a total average increase in sac volume of 3.26%. The ratio of thrombus to total volume stayed almost constant over the 12 months at 0.48, while the ratio of flow to total volume fell from 0.21 to 0.12 at 12 months.
Similar results were reported by the STRATO trial investigators Citation[18]. The STRATO trial was conducted under the auspices of the French Ministry of Health to evaluate endovascular repair of type II and III TAAA using MFM in patients with contraindications for open surgery and fenestrated stent-grafts.
This prospective, multicenter, nonrandomized clinical trial recruited 23 patients (19 men; mean age 75.8 years) with Crawford type II (43.5%) and III (56.5%) TAAA with mean diameter of 6.5 cm.
Technical success was 100% and of the 20 patients who had computed tomography scans at 12 months, the primary efficacy outcome of stable aneurysm thrombosis was met in 15 patients. The rate of primary patency of covered branch vessels was 96% (53/55) and at 1 year, aneurysm diameter was stable in 18 of 20 patients. Relative changes in thrombus volume were measured in 17 patients, in whom the mean ratio of residual aneurysm flow volume to total volume had decreased by 28.9% and the mean ratio of thrombus volume to total lumen volume had increased by 21.3%. There were no cases of device migration, loss of device integrity, spinal cord ischemia or aneurysm rupture. The authors concluded that at 1 year, endovascular repair with the MFM is safe and effective while successfully maintaining branch vessel patency.
Acceptable outcomes are possible with the MFM when used under indications for use. However, the MFM technology was globally disseminated prior to the derivation of proper Instructions for Use and was indiscriminately utilized by eager operators with no experience of the MFM to manage unsalvageable patients. This resulted in dismal clinical outcomes as depicted in the series by Sultan et al. Citation[19].
Sultan et al. Citation[19] identified 38 cases in which MFM implantation occurred outside the Instructions for Use. Of these 38 cases, there were 21 cases of aortic rupture; in 10 of these cases, aortic rupture was the primary presentation and in 4 cases, rupture was associated with superior mesenteric artery thrombosis – 2 occurred in mycotic aneurysms and 2 had previous superior mesenteric artery angioplasty. Mortality from aortic rupture was 100%. However, all these cases were done outside of Indications for Use on compassionate grounds due to patient’s co-morbid illness severity and the lack of alternative treatment options that could be as minimally invasive as the MFM. Moreover, in these cases, the MFM was still in its infancy and there was a lack of awareness of the technical parameters for stent deployment. There was no consensus on whether to and by how much to oversize the stent, minimum or maximum overlap, landing zone integrity and length, preoperative visceral artery management, adjuvant medical therapy and stringent follow-up protocols. This raises concern about the naïve and undiscerning release of a new technology outside monitored clinical trials and without expertly drafted guidelines for use.
Others have reported on rupture post MFM implantation, but even when reporting on the negative outcomes, the authors of the various reports have conceded that technical errors were factorial, and have acknowledged that the MFM has therapeutic potential Citation[20–23]. Debing et al. reported early clinical success and aneurysm-related survival in five of the six patients they treated with the MFM, with no stent migrations, retractions, thrombosis, fractures or re-interventions at 6 months Citation[23].
The addition of the MFM to mainstream vascular practice has introduced us to the discipline of bioengineering and compelled us to re-evaluate our core concepts of aneurysm treatment and shift our focus from anatomical to physiological therapies. The mechanism of action of MFM in the management of TAAA still remains elusive to most endovascular specialists. The interplay between pressure, wall stress, shear stress, wall displacement, blood flow vortex development and aneurysm wall dysplasia forms concepts that are not yet part of the contemporary vascular vernacular, and a lack of understanding of the mechanics of the MFM has produced skepticism and trepidation. In order to advance, we need to be open to new concepts.
The key components of MFM function are its manipulation of blood flow, preservation and enhancement of flow into arterial side branches, compliance, encouragement of endothelialization and influence on thrombus formation, all of which reduce peak wall stresses while simultaneously enhancing wall strength and promoting healing. The MFM is not a solution for patients living on borrowed time.
MFM harnesses the body’s innate physiological processes to modulate the aneurysm with no risk of critical shuttering or loss of native side branches. MFM has less operative trauma and shorter procedure time with reduced hospital stay. It is a promising disruptive technology, only in safe hands, and must be utilized under strict Instructions for Use. Its simplicity, consistency and reproducibility will allow rapid endovascular dissemination. It is a disruptive technology that, as with most medical devices, will continue to require further development and technical refinement. Long-term follow-up of the MFM global registry patients is mandatory before establishing a randomized control study. However, when designing clinical trials to evaluate the device, cognizance must be given to the fact that there is a distinct cohort of patients in whom no other treatment option is viable and MFM is their only option.
Premeditatio malorum
The US FDA should anticipate all potential technological pitfalls, but chose to react to disruptive technology with equanimity and not fear the wind of change.
The FDA should exercise equanimity and reflect on how to react in a timely fashion to potential game-changing events. With such stoicism, they should determine the most constructive approach toward MFM technology.
Financial & competing interests disclosure
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
No writing assistance was utilized in the production of this manuscript.
References
- Kontopodis N, Metaxa E, Papaharilaou Y, et al. Value of volume measurements in evaluating abdominal aortic aneurysms growth rate and need for surgical treatment. Eur J Radiol 2014;83:1051-6
- Truijers M, Pol JA, SchultzeKool LJ, et al. Wall stress analysis in small asymptomatic, symptomatic and ruptured abdominal aortic aneurysms. Eur J Vasc Endovasc Surg 2007;33:401-7
- Maier A, Gee MW, Reeps C, et al. A comparison of diameter, wall stress, and rupture potential index for abdominal aortic aneurysm rupture risk prediction. Ann Biomed Eng 2010;38:3124-34
- Molony DS, Kavanagh EG, Walsh MT, et al. A computational study of the magnitude and direction of migration forces in patient-specific abdominal aortic aneurysm stent-grafts. Eur J Vasc Endovasc Surg 2010;40:332-9
- Sultan S, Hynes N, Kavanagh EP, et al. How does the multilayer flow modulator work? The science behind the technical innovation. J Endovasc Ther 2014;21(6):814-21
- Sultan S, Hynes N, Kavanagh EP. Study of Endothelialisation Kinetics of Single Versus Multilayer Arterial Stents. Vasc Med 2014;19(3):221-43
- Wang X, Li X. Fluid-structure interaction based study on the physiological factors affecting the behaviors of stented and non-stented thoracic aortic aneuryms. J Biomech 2011;44(12):2177-84
- Georgakarakos E, Ioannou CV, Papaharilaou Y, et al. Computational evaluation of aortic aneurysm rupture risk: what have we learned so far? J Endovasc Ther 2011;18(2):214-25
- Dias NV, Ivancev K, Kolbel T, et al. Intra-aneurysm Sac pressure in patients with unchanged AAA diameter after EVAR. Eur J Vasc Endovasc Surg 2010;39:35-41
- Dias NV, Ivancev K, Resch TA, et al. Endoleaks after endovascular aneurysm repair lead to nonuniform intrasac pressure. J Vasc Surg 2007;46:197-203
- Linbald B, Dias N, Malina M, et al. Pulsatile wall motion (pwm) measurements after endovsacualr abdominal aortic aneurysm exclusion are not useful in the classification of endoleak. Eur J Vasc Endovasc Surg 2004;28:623-8
- Dias NV, Ivancev K, Mailin M, et al. Intra-aneurysm sac pressure measurements after endovascular aneurysm repair: differences between shrinking, unchanged, and expanding aneurysms with and without endoleaks. J Vasc Surg 2004;39:1229-35
- Sonesson B, Dias N, Malina M, et al. Intra-aneurysm pressure measurements in successfully excluded abdominal aortic aneurysm after endovascular repair. J Vasc Surg 2003;37:733-8
- Resch T, Ivancev K, Lindh M, et al. Persistent collateral perfusion of abdominal aortic aneurysm after endovascular reapir does not lead to progressive change in aneurysm diameter. J Vasc Surg 1998;28:242-9
- Malina M, Lanne T, Ivancev K, et al. Reduced pulsatile wall motion of abdominal aortic aneurysms after endovascular repair. J Vasc Surg 1998;27:624-31
- Lioupis C, Corriveau MM, MacKenzie KS, et al. Paraplegia prevention branches: a new adjuvant for preventing or treating spinal cord injury after endovascular repair of thoracoabdominal aneurysms. J Vasc Surg 2011;54:252-7
- Sultan S, Hynes N. One-year results of the multilayer flow modulator stent in the management of thoracoabdominal aortic aneurysms and type B dissections. J Endovasc Ther 2013;20(3):366-77
- Vaislic CD, Fabiani JN, Chocron S, et al. One-year outcomes following repair of thoracoabdominal aneurysms with the multilayer flow modulator: report from the STRATO trial. J Endovasc Ther 2014;21(1):85-95
- Sultan S, Hynes N, Sultan M, et al. When not to implant the multilayer flow modulator: lessons learned from application outside the indications for use in patients with thoracoabdominal pathologies. J Endovasc Ther 2014;21(1):96-112
- Lazaris AM, Charalampopoulos A, Maheras AN, et al. Flow-diverting multilayer stents: a promising but questionable solution for aortic pathologies. J Endovasc Ther 2013;20(3):378-80
- Antoniou GA, Papas TT, Mazarakis I, et al. Aortic aneurysm rupture following treatment with flow-diverting multilayer stents. J Endovasc Ther 2013;20(6):872-4
- Ferrero E, Gibello L, Ferri M, et al. Aortic arch rupture after multiple multilayer stent treatment of a thoracoabdominal aneurysm. J Vasc Surg 2014;60(5):1348-52
- Debing E, Aerden D, Gallala S, et al. Stenting complex aorta aneurysms with the Cardiatis multilayer flow modulator: first impressions. Eur J Vasc Endovasc Surg 2014;47(6):604-8