Abstract
The diagnostic assessment of pelvic floor function and anatomy is moving from the fringes to the mainstream of obstetrics and gynecology. This is largely due to the realization that pelvic floor trauma in labor is common, generally overlooked, and is a major factor in the causation of pelvic organ prolapse. Modern imaging methods such as MRI and 3D ultrasound have enabled us to diagnose such abnormalities reliably and accurately, most commonly in the form of an avulsion of the puborectalis muscle off its insertion on the os pubis. Major trauma to the levator muscle can also be palpated – a skill that is available to every clinician, requiring neither investment nor specialized equipment. In this article, I will attempt to summarize current knowledge of pelvic floor trauma, with particular emphasis on diagnosis of delivery-related damage to the levator ani muscle. Perineal and anal sphincter trauma will not be covered in detail.
Medscape: Continuing Medical Education Online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education through the joint sponsorship of Medscape, LLC and Expert Reviews Ltd. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians. Medscape, LLC designates this educational activity for a maximum of 1.0 AMA PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test and/or complete the evaluation at www.medscapecme.com/journal/expertob; (4) view/print certificate.
Learning objectives
Upon completion of this activity, participants should be able to:
• Review the incidence and etiology of the most common types of injury to the levator ani muscle and the impact of these injuries on female pelvic organ prolapse
• Describe a methodology for palpating the levator ani that correlates with information provided by imaging and the utility of this assessment in clinical practice
• Examine risk assessment and prevention strategies for levator ani muscle trauma
Financial & competing interests disclosure
EDITOR
Elisa Manzotti, Editorial Director, Future Science Group, London, UK.
Disclosure:Elisa Manzotti has disclosed no relevant financial relationships.
CME AUTHOR
Désirée Lie, MD, MSEd
Clinical Professor, Family Medicine, University of California, Irvine, Orange, California; Director of Research and Patient Development, Family Medicine, University of California, Irvine, Medical Center, Rossmoor, CA, USA.
Disclosure:Désirée Lie, MD, MSEd, has disclosed the following relevant financial relationship: she served as a nonproduct speaker for: ‘Topics in Health’for Merck Speaker Services.
AUTHORAND CREDENTIALS
Hans Peter Dietz, MD, PhD
Sydney Medical School Nepean, Nepean Hospital, Penrith, Australia.
Disclosure:Hans Peter Dietz, MD, PhD, has disclosed the following relevant financial relationships:
Acted as a paid consultant for: AMS; CCS (Sydney, NSW, Australia). Accepted speakers fees from: Astellas; General Electric Company; AMS. Has been the beneficiary of equipment loans from: Brüel & Kjær; Toshiba; GE Ultrasound. Tecsana GmbH have supplied the author’s unit with Epi-No devices in support of an ongoing randomized controlled trial.
This illustration is not entirely correct, as in most cases there appears to be very little or no muscle left on the bone since the tear occurs at the insertion rather than in the muscle belly. However, the figure correctly describes the most common form of trauma, affecting the right puborectalis muscle, with retraction of muscle fibers perianally, and its most common cause at the time (i.e., forceps delivery).
Reproduced with permission from Citation[2].
![Figure 1. Right-sided avulsion seen from the caudal view.This illustration is not entirely correct, as in most cases there appears to be very little or no muscle left on the bone since the tear occurs at the insertion rather than in the muscle belly. However, the figure correctly describes the most common form of trauma, affecting the right puborectalis muscle, with retraction of muscle fibers perianally, and its most common cause at the time (i.e., forceps delivery).Reproduced with permission from Citation[2].](/cms/asset/0757342e-da07-480e-af50-3eecc1947250/ierb_a_11205123_f0001_b.jpg)
The vulva, mons pubis, clitoris, perineal muscles and perineum to the anus, as well as peri- and postanal skin and and some of the fibrofatty tissue of the ischiorectal fossa have been removed to allow access to the puborectalis muscle.
Reproduced with permission from Citation[61].
![Figure 2. Intact puborectalis muscle in a fresh cadaver, dissected from caudally.The vulva, mons pubis, clitoris, perineal muscles and perineum to the anus, as well as peri- and postanal skin and and some of the fibrofatty tissue of the ischiorectal fossa have been removed to allow access to the puborectalis muscle.Reproduced with permission from Citation[61].](/cms/asset/9fa10ebe-25a4-4ad3-8f99-affded343fcd/ierb_a_11205123_f0002_b.jpg)
The two arrows indicate the gap between urethra and puborectalis insertion that can conveniently be palpated to determine muscle integrity.
Reproduced with permission from Citation[61].
![Figure 3. The appearance of the puborectalis muscle in a rendered volume in the axial plane, using translabial 3D ultrasound with speckle reduction imaging.The two arrows indicate the gap between urethra and puborectalis insertion that can conveniently be palpated to determine muscle integrity.Reproduced with permission from Citation[61].](/cms/asset/5efbd0d3-3708-42e5-8e04-37204d21f16c/ierb_a_11205123_f0003_b.jpg)
(A) Shows appearances immediately postpartum, with the avulsed muscle exposed by a large vaginal tear. (B) Shows a rendered volume (axial plane, translabial 3D ultrasound) 3 months postpartum. (C) Shows MRI findings (single slice in the axial plane) at 3.5 months postpartum.
Reproduced with permission from Citation[14].
![Figure 4. Right-sided puborectalis avulsion after normal vaginal delivery at term.(A) Shows appearances immediately postpartum, with the avulsed muscle exposed by a large vaginal tear. (B) Shows a rendered volume (axial plane, translabial 3D ultrasound) 3 months postpartum. (C) Shows MRI findings (single slice in the axial plane) at 3.5 months postpartum.Reproduced with permission from Citation[14].](/cms/asset/8fba29c9-5e10-4de6-b520-bc0ac845499a/ierb_a_11205123_f0004_b.jpg)
(A) Shows a normal muscle, (B) an avulsion injury.
Reproduced with permission from Citation[20].
![Figure 5. Digital palpation of the puborectalis muscle insertion.(A) Shows a normal muscle, (B) an avulsion injury.Reproduced with permission from Citation[20].](/cms/asset/5600a066-f2ed-4df9-bd7d-84fed4047256/ierb_a_11205123_f0005_b.jpg)
L: Left; R: Right.
Reproduced with permission from Citation[20].
![Figure 6. Suggested schematic for the documentation of puborectalis trauma, modified Oxford grading and grading of resting tone.L: Left; R: Right.Reproduced with permission from Citation[20].](/cms/asset/c2221f7b-ef6a-495b-b33c-bfb7997b49ad/ierb_a_11205123_f0006_b.jpg)
It is evident that the pelvic sidewall is smoothly denuded of muscle, that is, that the morphological abnormality documented here is an ‘avulsion’ of the puborectalis muscle insertion.
Reproduced with permission from Citation[61].
![Figure 7. Typical right-sided avulsion injury in a rendered volume, axial plane.It is evident that the pelvic sidewall is smoothly denuded of muscle, that is, that the morphological abnormality documented here is an ‘avulsion’ of the puborectalis muscle insertion.Reproduced with permission from Citation[61].](/cms/asset/7f64f5b9-b5ca-4975-9fef-b0c07c957bca/ierb_a_11205123_f0007_b.jpg)
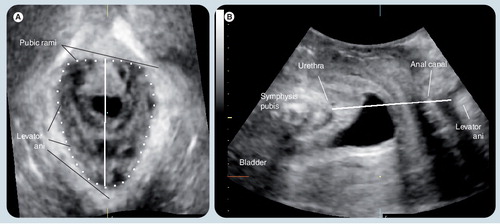
This plane, while not always sufficient to diagnose avulsion injury, defines the levator hiatus, is used to determine hiatal dimensions and distensibility, and serves as a convenient reference plane for tomographic ultrasound imaging.
(A) represents a reference image in the coronal plane. (B–I) Show slices parallel to the plane of minimal hiatal dimensions. (B & C) Are 5 and 2.5 mm below this plane, respectively. (D) Represents the plane of minimal dimensions. (E–I) Are 2.5–12.5 mm above this plane, encompassing the entire insertion of the puborectalis. (B) Is clearly below the muscle insertion (short arrows). (I) Is starting to show much thinner muscle, probably representing iliococcygeus rather than puborectalis (long arrows).
Modified with permission from Citation[37].
![Figure 9. Assessment of the puborectalis muscle by tomographic or multislice ultrasound.(A) represents a reference image in the coronal plane. (B–I) Show slices parallel to the plane of minimal hiatal dimensions. (B & C) Are 5 and 2.5 mm below this plane, respectively. (D) Represents the plane of minimal dimensions. (E–I) Are 2.5–12.5 mm above this plane, encompassing the entire insertion of the puborectalis. (B) Is clearly below the muscle insertion (short arrows). (I) Is starting to show much thinner muscle, probably representing iliococcygeus rather than puborectalis (long arrows).Modified with permission from Citation[37].](/cms/asset/113db7a8-786f-4a41-92f6-213b2f5adc3a/ierb_a_11205123_f0009_b.jpg)
(A) An avulsion on the patient’s right (marked by *). (B) Intact muscle on the patient’s left. (C) Tomographic representation of the puborectalis muscle in the same patient, with the avulsion evident in most slices (marked by *).
Reproduced with permission from Citation[39].
![Figure 10. 2D parasagittal oblique views of the puborectalis muscle obtained by translabial ultrasound.(A) An avulsion on the patient’s right (marked by *). (B) Intact muscle on the patient’s left. (C) Tomographic representation of the puborectalis muscle in the same patient, with the avulsion evident in most slices (marked by *).Reproduced with permission from Citation[39].](/cms/asset/869cf6a0-b9d7-45a2-b3ee-6fb0c1b9c832/ierb_a_11205123_f0010_b.jpg)
FDVD: Vaginal operative forceps or vacuum delivery.
Reproduced with permission from Citation[43].
![Figure 11. Relationship between age at first delivery and levator avulsion.FDVD: Vaginal operative forceps or vacuum delivery.Reproduced with permission from Citation[43].](/cms/asset/71a9873c-3fda-4984-8a9a-ce41bc9cd47a/ierb_a_11205123_f0011_b.jpg)
Antepartum and postpartum ultrasound images (single-slice axial planes in the plane of minimal hiatal dimensions) of a patient with left-sided avulsion after forceps delivery. (A) The hiatal area on maximum Valsalva at 38 weeks was 15.6 cm2. (B) It was measured at 29.3 cm2 at 4 months postpartum.
Reproduced with permission fromCitation[61].
![Figure 12. The effect of levator avulsion on hiatal dimensions.Antepartum and postpartum ultrasound images (single-slice axial planes in the plane of minimal hiatal dimensions) of a patient with left-sided avulsion after forceps delivery. (A) The hiatal area on maximum Valsalva at 38 weeks was 15.6 cm2. (B) It was measured at 29.3 cm2 at 4 months postpartum.Reproduced with permission fromCitation[61].](/cms/asset/e1e34bdd-2893-4c67-a196-2581803c5acd/ierb_a_11205123_f0012_b.jpg)
Delivery-related trauma to the levator ani muscle is increasingly attracting attention from gynecologists, colorectal surgeons, urologists and physiotherapists, rediscovered with the help of modern cross-sectional imaging methods after a hiatus of 60 years. Many women who have given birth naturally are affected by pelvic floor trauma, and so are their partners. Health professionals deal with the eventual consequences of such trauma, especially female pelvic organ prolapse (FPOP) and fecal incontinence. The integrity of the levator ani or, more specifically, the integrity of the puborectalis muscle that forms the levator hiatus, is the best-defined etiological factor in the pathogenesis of FPOP. As a result, any diagnostic assessment of a patient with prolapse is incomplete without evaluation of the puborectalis muscle. This should have been obvious 100 years ago after Halban and Tandler in Vienna (Austria) described major abnormalities of the levator ani on dissection in women with severe pelvic organ prolapse Citation[1]. De Lee was evidently aware of levator tears as a consequence of vaginal childbirth in the 1930s, as seen in , reproduced from the 7th Edition of his textbook, dated 1938 Citation[2].
Gainey, a Kansas City (MO, USA) obstetrician, reported the incidence of levator tears in a large series of women after vaginal childbirth in 1943 Citation[3]. Gainey detected such trauma in approximately 20% of vaginally parous women, with a preponderance of right-sided trauma, a finding that agrees well with modern data. Incredibly, this knowledge appears to have become lost, and current textbooks of obstetrics and gynecology do not contain any reference to levator trauma.
Until recently ‘pelvic floor trauma’ meant perineal and vaginal tears, damage to the anal sphincter and possibly pudendal nerve trauma. In developing countries especially, pelvic floor trauma also includes fistulae, but these are uncommon in developed countries with good intrapartum care. Anal sphincter trauma has received much attention over the last 20 years and will not be dealt in this article, the focus of which is on levator trauma. We now know that ‘pelvic floor trauma’ is much more than what we have been taught to identify and repair in the delivery suite. In 10–30% of all women who have given birth normally there is serious macroscopic damage to the puborectalis component of the levator ani muscle Citation[4–7], with incidence varying markedly owing to demographics and obstetric practice.
The levator ani is a muscular plate surrounding a central v-shaped hiatus, forming the caudal part of the abdominal envelope. As such, it encloses the largest potential hernial portal in the human body, the ‘levator hiatus’, containing the urethra, vagina and anorectum. Its peculiar shape and function is a compromise between priorities that seem virtually impossible to reconcile. On the one hand, abdominal contents have to be secured against gravity, and on the other hand solid and liquid wastes have to be evacuated. In addition there are the requirements of reproduction: intercourse and childbirth. The latter is the most extreme of tasks required of the pelvic floor, particularly in view of the size of the baby’s head. There are other mammalian species in which giving birth is fraught with danger, but even in the great apes childbirth is a very minor event compared with in humans.
The levator ani is thought to consist of several major subdivisions, and there is considerable confusion in the literature with regards to the nomenclature and distinctions between pubococcygeus, pubovaginalis, puboperinealis, puborectalis, iliococcygeus and coccygeus muscles. Some of these terms do not comply with the basic rule that muscles should be named for their origin and insertion, since there is no component of the levator ani that runs from the os pubis to the coccyx. Hence, the term ‘pubococcygeus’ is simply inappropriate. In addition, since these muscles cannot currently be distinguished easily, neither clinically nor on imaging, or even on cadaver dissection, the author considers only the puborectalis muscle (as the v-shaped muscle originating on the os pubis/the inferior pubic ramus and surrounding the anorectal angle posteriorly) and the iliococcygeus muscle. The latter is a sheet of muscle that acts as a continuation of the puborectalis cranially and laterally. While the fiber direction is somewhat different from the puborectalis, on vaginal palpation the iliococcygeus muscle is palpable as a continuation of the puborectalis above the inferior pubic ramus in the lateral vagina, extending from the pelvic sidewall to the ischial spine and the coccyx.
shows a fresh cadaver dissection of the levator ani muscle, with the puborectalis forming a V-shaped structure approximately as thick as a 5th finger (digitus minimus), anchored to the inferior pubic ramus and the body of the os pubis ventrally. This dissection approach demonstrates the muscle as seen from below or caudally, and shows clearly that puborectalis/iliococcygeus are a contiguous functional entity. The left side of the image is the patient’s right side, the symphysis pubis is at the top. demonstrates the appearance of the puborectalis on 3D pelvic floor ultrasound, in a ‘rendered volume’, that is, a semitransparent representation of volume data. The arrows indicate the gap between muscle insertion and urethra, which is important for palpation.
The pelvic floor in childbirth
The levator ani muscle plays a major role in childbirth. It has to distend enormously Citation[8], and the degree of required distension varies greatly between individuals, by at least a factor of five Citation[9]. The levator hiatus has to enlarge from 15–25 cm2 in most young nulliparous women Citation[10] to 60–80 cm2Citation[9] in order to birth a term-sized fetal head. Experimental data from muscle physiology research suggest that skeletal muscle will not lengthen to more than 150% of its original length without suffering permanent damage Citation[11], with the degree of trauma proportional to the work expended in elongating the muscle to a given degree. Hence it is remarkable that in many women the puborectalis does not suffer any significant trauma despite much greater degrees of distension. In approximately half of all women there is no appreciable change in distensibility or morphological appearance after vaginal delivery. It is not understood how this should be possible, but we assume that it is somehow due to the protective hormonal effects of pregnancy. It is not difficult to appreciate that the biomechanical properties of this muscle might have some effect on the progress of labor: a more distensible muscle appears to be associated with a shorter second stage of labor and possibly also with delivery mode Citation[12,13].
As mentioned previously, trauma to the levator ani muscle after childbirth was first reported in a research paper in 1943, only to be forgotten for 60 years. It is difficult to believe, but this major form of maternal birth trauma, easily palpable vaginally and occasionally visible in the delivery suite in women with large vaginal tears Citation[14], is missing from our obstetric and midwifery textbooks, and has only recently been rediscovered by imaging specialists using MRI and 3D/4D ultrasound . Most commonly, appearances are those of an ‘avulsion’, that is, a traumatic dislodgment of the muscle from its bony insertion. This entity, avulsion of the puborectalis muscle, has now also been confirmed on cadaver dissection Citation[15].
There are other forms of localized or generalized morphological abnormalities, such as isolated defects of the inferior aspects of the iliococcygeus muscle, but they are less common. Irreversible overdistension (‘microtrauma’) of the muscle without actual tears appears to occur more frequently, but of course such changes can only be detected if antenatal imaging is available for comparison. Appearances are rarely consistent with pudendal neuropathy, which in the past was considered the main etiological factor in pelvic floor dysfunction Citation[16,17]. Finally, it is possible that, in patients with longstanding severe FPOP, there may be secondary effects caused by constant pressure/distension and disuse. Such effects may, in principle, be reversible, as opposed to neuropathy or muscle trauma.
Diagnosis by palpation
As mentioned previously, diagnosis of levator muscle tears is possible by palpation, although this requires substantial teaching, and the learning curve seems to be quite long Citation[18–21]. The main challenge is the distinction between partial and complete trauma, especially in women with poor muscle function and/or atrophy. Until recently, assessment of levator function, if undertaken at all, was limited to grading muscle strength and endurance, using the modified Oxford grading system first suggested by Laycock Citation[22]. Physiotherapists have a long history of using palpation to assess skeletal muscle and some, with appropriate postgraduate training, have extended their skills to include digital assessment of pelvic floor muscle (PFM) by the vaginal or transanal route. In the physiotherapy literature there are many reports of palpation to assess PFM contraction, and some describing the identification of pain and trigger points, and even evaluation of muscle tone Citation[23]. However, although clinical anecdote suggests that some physiotherapists recognize other characteristics concerning muscle morphology (e.g., holes, gaps, ridges and scarring), it is difficult to find any literature describing the techniques needed to do this or their accuracy or repeatability. Mantle noted that with training and experience, a physiotherapist might be able to discern muscle integrity, scarring and the width between the medial borders of the PFMs with palpation Citation[24].
In 1943, Gainey published the findings of a palpatory assessment of 1000 women delivered by him personally Citation[3]. Gainey described trauma to what he called the ‘pubococcygeus’ muscle, and from his description it is quite clear that he did detect avulsion injuries of the puborectalis. In fact, the prevalence of such defects quoted by him (∼20% in primiparous women) agrees very well with modern work using MRI Citation[25] and pelvic floor ultrasound Citation[4,6,7]. Evidently, if it was possible to palpate such trauma in 1943, it should be possible to do so today.
explain how palpatory assessment of the puborectalis muscle may be undertaken. To assess morphological integrity the palpating finger is placed parallel to the urethra, with the tip of the finger at the bladder neck, and its palmar surface pressed against the posterior/dorsal surface of the symphysis pubis. If the muscle is intact then there will be just enough room to fit the palpating finger between the urethra medially and the insertion of the puborectalis muscle laterally. If there is no muscle palpable on the posterior surface of the os pubis and the inferior pubic ramus immediately lateral to a finger placed parallel to the urethra, and if this finger can be moved over the inferior pubic ramus without encountering any contractile tissue for another 2–3 cm, then this implies an avulsion injury on this side. The extent of avulsion varies greatly, and there is also a spectrum of incomplete injuries: generalized thinning of the muscle, partial avulsion of the most inferior aspects (with the most cranial aspects of the puborectalis still adhering to the inferior pubic ramus) and partial avulsion of more cranial aspects, palpable as a hole, slit or gap in the insertion of the superior aspects of the puborectalis, or in the inferior aspects of the iliococcygeus muscle. From recent research it seems that partial trauma is not associated with prolapse or symptoms of prolapse Citation[26], but it is conceivable that partial trauma may affect other aspects of pelvic floor function, such as continence Citation[27], or act as a marker for other, hitherto unrecognized, forms of trauma. While the importance of such partial trauma remains unclear, a complete avulsion detected on palpation is clearly associated with reduced contraction strength of the muscle Citation[21,28], as well as with symptoms and signs of prolapse Citation[28,29].
Avulsion often seems to have an impact on adjacent or contralateral intact muscle. After unilateral avulsion, the intact contralateral puborectalis may become spastic and very tender, a hitherto unrecognized cause of chronic pelvic pain and dyspareunia. After bilateral avulsion, there may be generalized hypertrophy of the iliococcygeus, resulting in a levator shelf that is almost as strong as the original, just somewhat higher, and of course wider, especially in the transverse or coronal dimension.
Currently, the assessment of levator function by physiotherapists, nurse continence advisors, gynecologists and urologists is (at best) limited to grading ‘squeeze and lift’. We propose a visual recording system for findings obtained on palpation of the puborectalis muscle . Such a system should include both some form of strength grading for ‘squeeze and lift’ bilaterally, as well as grading for resting tone (conveniently graded 0–5 to accord with the Oxford system, see for a suggested scale).
In addition, one should attempt a morphological assessment of the puborectalis muscle and document findings either as defects or gaps or thinning. The documentation system proposed in could form the basis of teaching efforts to improve on our palpatory assessment skills and would allow easier communication among clinical practitioners and researchers.
Clearly, digital palpation of the puborectalis muscle is a skill that requires significant training, most conveniently in a unit that allows for instant comparison with findings on imaging. Without additional training, agreement between a clinical assessor and imaging is likely to be poor Citation[18–20]. However, there is no doubt that assessment of the puborectalis muscle by palpation is within reach of any practitioner in the field. The emerging literature on the clinical relevance of levator defects detected on imaging implies that this skill should be well worth acquiring.
Diagnosis by ultrasound imaging
It apepars that the diagnosis of levator trauma is more repeatable when undertaken by imaging. While MRI was the first method used to assess the levator ani Citation[30], it suffers from a number of obvious shortcomings: cost, accessibility, the inability to use MRI in women with ferrous implants, issues with claustrophobia in some women, the lack of dynamic imaging and problems with defining correct planes, since very few currently used systems allow true volume imaging. Most of those shortcomings do not apply to ultrasound, especially not to translabial 3D/4D ultrasound performed using technology that was developed for fetal imaging and that is now available in virtually all major obstetrics and gynecology units in the developed world. While transvaginal ultrasound has been used to image the levator ani Citation[13,31,32], this requires side-firing endoprobes that are not in general use and rarely found in obstetrics and gynecology imaging departments.
The diagnosis of levator trauma by transperineal (or perineal, or introital) ultrasound was first described in 2004 on ‘rendered volumes’, that is, semitransparent representations of blocks of volume ultrasound data , using Voluson-type systems and 3D/4D curved array volume transducers that were developed for fetal imaging Citation[33]. This form of 3D ultrasound relies on fast mechanical movement of a curved array within the 3D transducer, acquiring volume data without any need for manual transducer movement or external position sensors. Both aperture and acquisition angles should be set to at least 70°. Acquisition angles of 70°, commonly the maximum of 3D transducers for obstetric imaging, are usually sufficient to document trauma to the muscle insertion, but to allow imaging of the entire hiatus in a patient with severe prolapse volumes have to be wider. The current maximum, 85°, enables visualization of severe ‘ballooning’ Citation[34] of the hiatus, at acceptable spatial resolutions and at a volume frequency of approximately 2 Hz. At lower acquisition angles, up to 20 Hz can be reached. This implies that temporal resolution in any plane is superior to MRI, while spatial resolution of structures within the levator hiatus up to approximately 4 cm depth is often comparable to MRI. Higher spatial resolutions can be reached with endoprobes, but the use of such transducers entails the disadvantages of local distortion and invasiveness, and to date there are no side-firing endoprobes on the market that can provide for dynamic imaging (i.e., 4D volume acquisition).
The diagnosis of avulsion by 3D ultrasound has been shown to be highly reproducible, in particular compared with palpation Citation[6,20]. Modern 3D ultrasound systems commonly allow tomographic or multislice imaging (tomographic ultrasound imaging; i.e., serial cross-sections at arbitrarily variable interslice intervals and angles). Diagnosis by tomographic ultrasound is probably currently the most repeatable technique Citation[35], although tomographic imaging may overdiagnose complete avulsion compared with digital palpation Citation[36], since minor remnants of muscle may be inapparent on tomographic ultrasound imaging. shows identification of the plane of minimal dimensions as reference plane, and demonstrates a tomographic representation of the entire puborectalis muscle, based on this reference plane, with an interslice interval of 2.5 mm. Tomographic ultrasound is probably best performed by bracketing the area of interest, with the lowermost slice just below the insertion of the puborectalis muscle as shown in Citation[37]. The topmost slices in a tomographic representation probably represent iliococcygeus Citation[38] rather than puborectalis since they show the levator to be thinner and in close proximity to the obturator foramen.
Avulsion can be diagnosed with 2D ultrasound using the simplest and most commonly available abdominal curved array transducers . However, since there is no clearly identifiable point of reference for parasagittal translabial planes, it is more difficult to be certain of a complete avulsion, and as a result repeatability is probably inferior Citation[39].
Regardless of which imaging method is used, palpation and imaging are best seen as complementary rather than mutually exclusive. Frequently, one method will allow a better appreciation of findings obtained by the other method. The palpating finger provides biomechanical information on tone and contractility that is not currently available on imaging, and minor muscle remnants may be identified more reliably. On the other hand, imaging information is more objective and reproducible, and it provides information on deeper structures that are not accessible on palpation.
Risk factors
All cases of avulsion documented thus far, whether by MRI, palpation or by ultrasound, were found in women who had delivered vaginally Citation[28,40,41]. It is probable that factors such as birthweight, length of second stage, size of the fetal head, and vacuum/forceps delivery increase the probability of avulsion injury Citation[4,5,7,42]. Forceps seem to be more traumatic than vacuum delivery Citation[10], especially rotational forceps Citation[42]. Epidural analgesia may partly or completely paralyze the levator ani, reducing the amount of work necessary to distend the muscle, and therefore the probability of trauma Citation[11]. These latter findings raise the possibility that changes to obstetric practice may reduce the incidence of major levator trauma. One may hypothesize that avoidance of forceps delivery, especially rotational forceps Citation[42], liberal use of epidural analgesia and a low threshold for cesarean delivery in obstructed labor, should have the potential to substantially reduce the likelihood of pelvic floor trauma. Fortunately, modern obstetrics already appears to be moving in this direction, even if, curiously, this is deplored by many in the field.
Ideally, one would of course want to prevent levator trauma altogether – either by avoiding vaginal childbirth in women at high risk of avulsion, or by antenatal intervention designed to reduce vulnerability. In order to prevent levator avulsion, we would need predictors that can be determined during pregnancy. It is plausible that the risk of trauma will depend not just on the required distension, but also on the biomechanical properties of muscle and muscle–bone interface (which are hitherto undefined). It is therefore not surprising that avulsion appears to be associated with maternal age at first delivery Citation[4,5,43] – a worrying finding in view of the continuing trend towards delayed childbearing in developed societies. The likelihood of major levator trauma at vaginal delivery seems to triple during the reproductive years – from under 15% at age 20 years to over 50% at 40 years . Unfortunately, at the moment it seems impossible to predict levator trauma from antenatal history and ultrasound data Citation[44].
What about antenatal intervention? In theory, PFM exercises may alter the biomechanical properties of the levator ani muscle. Since the pelvic floor of athletes seems to be more elastic Citation[45], it is conceivable that a dedicated program of antenatal PFM exercises might increase elasticity and reduce trauma. Another way to increase elasticity of the levator ani may be to successively dilate it antenatally, using a vaginal dilator such as the Epi-No™ (Tecsana GMBH, Munich, Germany) device Citation[46,47].
Consequences of levator trauma
Not surprisingly, the effect of avulsion on muscle function is substantial. Contraction strength as estimated by Oxford grading Citation[21] and instrumented speculum Citation[28] is reduced by approximately one third, an observation that may help diagnose levator trauma. Many symptomatic women unable to contract the levator ani appear to be suffering from avulsion, often bilateral Citation[48]. Avulsion results in a hiatus that is larger (by 20–30%), especially in the coronal plane Citation[49], more distensible and less contractile Citation[28,41]. However, the effect of avulsion does not seem to be mediated solely through an increase in hiatal diameters or area. Other factors clearly play a role. It is very probable that avulsion is a marker for trauma to fascial structures that we are currently unable to assess properly Citation[50]. shows the effect of avulsion on hiatal dimensions in a patient after forceps delivery at term.
Prolapse
Levator avulsion is associated with anterior and central compartment prolapse and probably represents the missing link (or a large part of the missing link) between childbirth and prolapse Citation[29]. The larger a defect is, both in width and depth, the more likely are symptoms and/or signs of prolapse Citation[35]. Levator avulsion seems to at least triple the risk of significant anterior and central compartment prolapse, with much less of an effect on posterior compartment descent. This effect does not seem to be mediated exclusively by ballooning or abnormal distensibility of the levator hiatus Citation[50], which also is associated with prolapse Citation[34].
It is not clear as to why it often takes decades for symptoms to develop, although DeLancey’s ‘ship in dock’ hypothesis provides a plausible explanation Citation[51]. One should also point out that there are many women who present with prolapse without having suffered an avulsion injury. As mentioned previously, there are other deleterious effects of childbirth on the levator ani, resulting in traumatic, irreversible overdistension Citation[10], and then there are young nulliparous women who show evidence of abnormal hiatal distensibility and pelvic organ descent that is very likely congenital Citation[52]. Avulsion in itself may only be responsible for 30–40% of all cases of symptomatic prolapse – but these may well be the most difficult forms of prolapse to treat surgically since avulsion is a risk factor for prolapse recurrence after pelvic reconstructive surgery Citation[53,54].
Urinary incontinence
Many laypeople and medical practitioners, as well as physiotherapists and continence nurse practitioners, assume that urinary incontinence is a sign of a weak pelvic floor. This may not be true. We have recently shown that levator avulsion is negatively associated with stress urinary incontinence (SUI) and urodynamic stress incontinence. This association remained negative even after controlling for eight potential confounders, including all forms of FPOP Citation[55]. Similar findings have since been reported using MRI Citation[27]. Why is it that there should be no major effect of puborectalis muscle trauma on SUI or urodynamic stress incontinence, considering that PFM training is a recognized and proven therapeutic intervention in women with SUI Citation[56]? If the puborectalis muscle is part of the urinary continence mechanism, shouldn’t it matter if one or both insertions of this muscle are disconnected from the inferior pubic ramus, rendering it badly dysfunctional?
First, we ought to consider that the therapeutic success of PFM training does not prove a role of the puborectalis muscle in stress urinary continence. After all, PFM training affects not just the puborectalis muscle but probably trains all muscular structures innervated by the sacral segments. Second, there are several other potential mechanisms by which childbirth might affect urinary continence. Denervation is the most obvious candidate since we have good evidence on the deleterious effect of vaginal birth on the pudendal nerve and its branches Citation[17]. Damage to the urethral rhabdosphincter or the longitudinal smooth muscle of the urethra may also be mediated through other factors such as devascularization. Then, there is the issue of pressure transmission, probably mediated through the pubourethral ligaments and/or suburethral tissues. Finally, there is reflex activation of muscular structures preceding a cough in most nulliparous women. Clearly, much research will be needed before we can claim to understand the pathophysiological basis for SUI.
Fecal incontinence
The second major clinical symptom that has at times been attributed to an abnormal puborectalis muscle (via an opening of the anorectal angle) is fecal incontinence, but we have found no significant association between this symptom and levator trauma Citation[57]. It therefore appears improbable that any intervention targeting levator dimensions or function would have a major impact on fecal continence. Any improvement in symptoms is more likely to be due to other associated therapeutic effects.
Sexual function
The puborectalis muscle has been called the ‘love muscle’ by sections of the popular press. It is likely that avulsion, especially if bilateral, would have some effect on sexual function. To date, however, we have only anecdotal information on this issue. Considering the popularity of cosmetic genitoplasty procedures aiming to ‘tighten’ the vagina, this may become an important consideration in the future. In some women the site of the avulsion remains tender, even after decades. Some women and their partners notice a marked difference in sexual relations after the birth of their first child. Other couples do not notice any change. For obvious reasons this is not an issue that is easy to investigate.
Clinical repercussions
Major morphological abnormalities of the levator ani probably affect surgical outcomes. A study using MRI demonstrated that recurrence after anterior colporrhaphy was much more likely in women with an abnormal pelvic floor Citation[58]. The author’s unit has recently shown that avulsion is associated with prolapse after hysterectomy, anti-incontinence and prolapse operations, especially after anterior repair Citation[53,54]. In view of the current, often acrimonious discussion regarding the use of mesh implants in reconstructive surgery, this association may turn out to be of major clinical importance. In the opinion of the author it makes little sense to perform a traditional anterior repair in women with bilateral avulsion and severe ballooning since such a procedure is very likely to fail.
Future developments
Prediction
One approach to reducing the incidence of levator trauma in childbirth would be to target preventative intervention in high-risk groups. This would require individual predelivery risk assessment, which may not be feasible with current technology Citation[44].
Prevention
The ultimate preventative intervention is of course elective cesarean section (CS). In view of the ever-increasing CS rate, it is quite possible that pelvic floor trauma will cease to be much of an issue within a generation. However, as mentioned previously, many women clearly do not need an operation to deliver their baby and preserve an intact pelvic floor, and it would be an enormous waste of resources to institute a policy of universal CS. Quite apart from resource issues, CS has very substantial downsides, both for the mother and her infant, the nature and magnitude of which are beyond the scope of this article. Clearly, CS would only be a potential option in women shown to be at high risk of trauma – and we currently have no means to identify those women prior to labor. Other forms of prevention may potentially be more practicable, such as attempts to change the biomechanical properties of the muscle–bone interface or the muscle and connective tissue of the pelvic floor in general. This may not be as far-fetched as it sounds. As mentioned previously, there is a commercially available device, the Epi-No, that is used to dilate the perineum and vagina in the last few weeks of pregnancy, and this device has been shown to reduce perineal trauma Citation[46]. The Epi-No is currently under investigation regarding a potential role in pelvic floor protection Citation[47].
Treatment
Is there anything that we can do to repair avulsion injury, either immediately after childbirth or at a later date? Surgical failure due to suture dislodgment seems very probable in the postpartum setting, given the quality of the tissues and the fact that there is no opportunity for splinting or immobilization. The author knows of four failed attempts at repairing avulsion by direct suturing after childbirth. Direct repair may have to wait several months and may have to utilize autologous fascia or mesh. An attempt using fascia lata was reported in 2009 Citation[59], but it seems that neither indication (fecal incontinence) nor surgical approach (through the ischiorectal fossa) or postoperative imaging (static MRI) were appropriate. In a different approach, it may be possible to compensate for avulsion defects as well as for excessive distensibility or ‘ballooning’ by employing minimally invasive concepts. However, it very likely will be many years before any reconstructive surgical technique can be regarded as proven and ready for general use.
Expert commentary
At present, many (if not most) obstetricians and gynecologists, and most urogynecologists and female urologists, are unaware of the levator ani as a significant component of pelvic organ support, and most have never assessed this structure. Obstetricians are largely unaware of the very substantial damage to this muscle that occurs in childbirth, even though levator trauma may be openly visible in women with large vaginal tears, and even though the problem was first described over 70 years ago. Surgeons dealing with FPOP are only just beginning to realize that levator trauma may well be the single most important etiological factor in the pathogenesis of prolapse, and in prolapse recurrence after surgery.
However, this rather negative assessment of the current situation also implies that there is enormous potential for progress. The number of researchers working in this field is growing by the month, and the increasing availability of modern imaging, both MRI and 3D/4D ultrasound, enables more and more clinicians to diagnose anatomical and functional abnormalities of the levator ani. Presently, the main challenge is to establish diagnostic criteria and to provide teaching and educational resources. However, while diagnosis has to come first, it remains useless unless there is effective treatment or, even better, prevention. Fortunately, first efforts at primary and secondary prevention are likely to bear fruit within the next 2 years.
Five-year view
Over the next 5 years, the diagnosis of levator trauma will become standardized, both on MRI and on ultrasound imaging, and more widespread as clinicians realize that they finally have the opportunity to identify a major etiological factor of FPOP. Hopefully, palpation of levator function and morphology will start to become an integral part of a clinical gynecological examination. The prevalence in different populations will be described, and the most important risk factors, both demographic and obstetric, will be identified. The first antenatal and intrapartum intervention studies will hopefully provide us with the means to reduce the incidence of such trauma. The biomechanical properties of pelvic floor structures will be defined properly, allowing more meaningful computer modeling of vaginal birth. And at last, after a full century of delay, we will learn how to repair levator defects surgically, or at least compensate for them, hopefully by minimally invasive means. Pelvic reconstructive surgery is about to enter a new, exciting phase in its development as we finally become able to address underlying disease processes rather than just their clinical manifestations.
Table 1. Modified Oxford grading.
Table 2. Proposed scale for the grading of levator resting tone.
Key issues
• Trauma to the puborectalis component of the levator ani (‘puborectalis avulsion’) is common after vaginal childbirth, occurring in 10–35% of women after vaginal delivery.
• It occurs during crowning of the fetal head and is more likely after forceps delivery, especially rotational forceps.
• Such trauma is usually occult but may be identified visually immediately after childbirth in women with large vaginal tears.
• Avulsion can be identified by MRI and on ultrasound, with 4D translabial ultrasound being the most convenient and cost effective.
• Avulsion reduces contraction strength of the puborectalis muscle and can result in marked hiatal asymmetry.
• Avulsion is a major etiological factor in the pathogenesis of female pelvic organ prolapse, especially cystocele and uterine prolapse.
• Avulsion increases the likelihood of prolapse recurrence after reconstructive surgery.
• The main priorities for future research should be prediction, prevention and surgical treatment of this form of trauma.
References
- Halban J, Tandler J. Anatomie und Aetiologie der Genitalprolapse beim Weibe. Braumueller, Vienna, Austria (1907).
- De Lee J. The Principles and Practice of Obstetrics (7th Edition). WB Saunders Company, PA, USA (1938).
- Gainey HL. Post-partum observation of pelvic tissue damage. Am. J. Obstet. Gynecol.46, 457–466 (1943).
- Dietz H, Lanzarone V. Levator trauma after vaginal delivery. Obstet. Gynecol.106, 707–712 (2005).
- Kearney R, Miller J, Ashton-Miller J, Delancey J. Obstetric factors associated with levator ani muscle injury after vaginal birth. Obstet. Gynecol.107(1), 144–149 (2006).
- Dietz HP, Steensma AB. The prevalence of major abnormalities of the levator ani in urogynaecological patients. BJOG113(2), 225–230 (2006).
- Valsky DV, Lipschuetz M, Bord A et al. Fetal head circumference and length of second stage of labor are risk factors for levator ani muscle injury, diagnosed by 3-dimensional transperineal ultrasound in primiparous women. Am. J. Obstet. Gynecol.201, 91.e1–e7 (2009).
- Lien KC, Mooney B, DeLancey JO, Ashton-Miller JA. Levator ani muscle stretch induced by simulated vaginal birth. Obstet. Gynecol.103(1), 31–40 (2004).
- Svabik K, Shek K, Dietz H. How much does the levator hiatus have to stretch during childbirth? Br. J. Obstet. Gynaecol.116, 1657–1662 (2009).
- Shek K, Dietz H. The effect of childbirth on hiatal dimensions: a prospective observational study. Obstet. Gynecol.113, 1272–1278 (2009).
- Brooks S, Zerba E, Faulkner J. Injury to muscle fibres after single stretches of passive and maximally stimulated muscle in mice. J. Physiol.488(2), 459–469 (1995).
- Lanzarone V, Dietz H. Three-dimensional ultrasound imaging of the levator hiatus in late pregnancy and associations with delivery outcomes. Aust. N. Z. J. Obstet. Gynaecol.47(3), 176–180 (2007).
- Balmforth J, Toozs-Hobson P, Cardozo L. Ask not what childbirth can do to your pelvic floor but what your pelvic floor can do in childbirth. Neurourol. Urodyn.22(5), 540–542 (2003).
- Dietz H, Gillespie A, Phadke P. Avulsion of the pubovisceral muscle associated with large vaginal tear after normal vaginal delivery at term. Aust. N. Z. J. Obstet. Gynaecol.47, 341–344 (2007).
- Wallner C, Wallace C, Maas C et al. A high resolution 3D study of the female pelvis reveals important anatomical and pathological details of the pelvic floor. Neurourol. Urodyn.28(7), 668–670 (2009).
- Swash M, Snooks SJ, Henry MM. Unifying concept of pelvic floor disorders and incontinence. J. R. Soc. Med.78(11), 906–911 (1985).
- Allen RE, Hosker GL, Smith AR, Warrell DW. Pelvic floor damage and childbirth: a neurophysiological study. BJOG97(9), 770–779 (1990).
- Dietz HP, Hyland G, Hay-Smith J. The assessment of levator trauma: a comparison between palpation and 4D pelvic floor ultrasound. Neurourol. Urodyn.25(5), 424–427 (2006).
- Kearney R, Miller JM, Delancey JO. Interrater reliability and physical examination of the pubovisceral portion of the levator ani muscle, validity comparisons using MR imaging. Neurourol. Urodyn.25(1), 50–54 (2006).
- Dietz HP, Shek KL. Validity and reproducibility of the digital detection of levator trauma. Int. Urogynecol. J.19, 1097–1101 (2008).
- Dietz HP, Shek C. Levator avulsion and grading of pelvic floor muscle strength. Int. Urogynecol. J.19(5), 633–636 (2008).
- Laycock J. Assessment and treatment of pelvic floor dysfunction. PhD, University of Bradford, Bradford, UK (1992).
- Devreese AM, Staes F, De Weerdt W et al. Clinical evaluation of pelvic floor muscle function in continent and incontinent women. Neurourol. Urodyn.23(3), 190–197 (2004).
- Mantle J. Urinary function and dysfunction. In: Physiotherapy in Obstetrics and Gynaecology. Mantle J, Haslam J, Barton S (Eds). Butterworth Heinemann, Edinburgh, UK (2004).
- DeLancey JO, Kearney R, Chou Q, Speights S, Binno S. The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet. Gynecol.101(1), 46–53 (2003).
- Bernardo M, Shek K, Dietz H. Does partial avulsion of the levator ani matter for symptoms or signs of pelvic floor dysfunction? Int. Urogynecol. J. (2010) (In press).
- Morgan D, Cardoza P, Guire K, Fenner D, DeLancey J. Levator ani defect status and lower urinary tract symptoms in women with pelvic organ prolapse. Int. Urogynecol. J.21(1), 47–52 (2010).
- DeLancey J, Morgan D, Fenner D et al. Comparison of levator ani muscle defects and function in women with and without pelvic organ prolapse. Obstet. Gynecol.109(2), 295–302 (2007).
- Dietz H, Simpson J. Levator trauma is associated with pelvic organ prolapse. Br. J. Obstet. Gynaecol.115, 979–984 (2008).
- Debus-Thiede G. Magnetic resonance imaging (MRI) of the pelvic floor. In: Pelvic Floor Reeducation – Principles and Practice. Schuessler B, Laycock J, Norton P, Stanton SL (Eds). Springer, London, UK, 78–82 (1994).
- Toozs-Hobson P, Athanasiou S, Khullar V, Boos K, Anders K, Cardozo LD. Does vaginal delivery damage the pelvic floor? Neurourol. Urodyn.16(5), 385–386 (1997).
- Athanasiou S, Chaliha C, Toozs-Hobson P, Salvatore S, Khullar V, Cardozo L. Direct imaging of the pelvic floor muscles using two-dimensional ultrasound: a comparison of women with urogenital prolapse versus controls. Br. J. Obstet. Gynaecol.114(7), 882–888 (2007).
- Dietz H. Ultrasound imaging of the pelvic floor: 3D aspects. Ultrasound Obstet. Gynecol.23(6), 615–625 (2004).
- Dietz H, De Leon J, Shek K. Ballooning of the levator hiatus. Ultrasound Obstet. Gynecol.31, 676–680 (2008).
- Dietz H. Quantification of major morphological abnormalities of the levator ani. Ultrasound Obstet. Gynecol.29, 329–334 (2007).
- Moegni F, Shek K, Dietz HP. Diagnosis of Levator avulsion injury: a comparison of three methods. Int. Urogynecol. J. (2010) (In press).
- Dietz HP. Tomographic ultrasound of the pelvic floor: which levels matter most? Ultrasound Obstet. Gynecol.33, 698–703 (2009).
- Kashihara H, Shek K, Dietz H. Can we identify the limits of the puborectalis muscle on tomographic translabial ultrasound? Int. Urogynecol. J. (2010) (In press).
- Dietz HP, Shek KL. Levator trauma can be diagnosed by 2D translabial ultrasound. Int. Urogynecol. J.20, 807–811 (2009).
- Dietz H. Levator trauma in labor: a challenge for obstetricians, surgeons and sonologists. Ultrasound Obstet. Gynecol.29(4), 368–371 (2007).
- Abdool Z, Shek K, Dietz H. The effect of levator avulsion on hiatal dimensions and function. Am. J. Obstet. Gynecol.201(1), 89.e1–e5 (2008).
- Krofta L, Otcenasek M, Kasikova E, Feyereisl J. Pubococcygeus–puborectalis trauma after forceps delivery: evaluation of the levator ani muscle with 3D/4D ultrasound. Int. Urogynecol. J.20, 1175–1181 (2009).
- Dietz H, Simpson J. Does delayed childbearing increase the risk of levator injury in labor? Aust. N. Z. J. Obstet. Gynaecol.47, 491–495 (2007).
- Shek K, Dietz H. Can levator avulsion be predicted antenatally? Am. J. Obstet. Gynecol. DOI: 10.1016/j.ajog.2009.11.038 (2010) (Epub ahead of print).
- Kruger J, Dietz H, Murphy B. Pelvic floor function in elite nulliparous athletes and controls. Ultrasound Obstet. Gynecol.30, 81–85 (2007).
- Kovacs G, Heath P, Heather C. First Australian trial of the birth-training device Epi-No: a highly significantly increased chance of an intact perineum. Aust. N. Z. J. Obstet. Gynaecol.44, 347–348 (2004).
- Shek K, Langer S, Chantarasorn V, Dietz H. Does the Epi-No device prevent levator trauma? A randomised controlled trial. Ultrasound Obstet. Gynecol. (2010) (In print).
- Sarma S, Hersch M, Siva S, Dietz H, Moore K. Women who cannot contract their pelvic floor muscles: avulsion or denervation? Neurourol. Urodyn.28(S1), 680–681 (2009).
- Otcenasek M, Krofta L, Baca V et al. Bilateral avulsion of the puborectal muscle: magnetic resonance imaging-based three-dimensional reconstruction and comparison with a model of a healthy nulliparous woman. Ultrasound Obstet. Gynecol.29, 692–696 (2007).
- Franco A, Shek K, Kirby A, Fynes M, Dietz H. Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? Int. Urogynecol. J.20(S2), S145–S146 (2009).
- DeLancey JO. Anatomy. In: Textbook of Female Urology and Urogynaecology. Cardozo L, Staskin D (Eds). Isis Medical Media, London, UK, 112–124 (2001).
- Dietz H, Shek K, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet. Gynecol.25, 580–585 (2005).
- Dietz HP, Chantarasorn V, Shek KL. Levator avulsion is a risk factor for cystocele recurrence. Ultrasound Obstet. Gynecol. DOI: 10.1002/uog.7678 (2010) (Epub ahead of print).
- Model A, Shek KL, Dietz HP. Do levator defects increase the risk of prolapse recurrence after pelvic floor surgery? Neurourol. Urodyn.28(S1), 888–889 (2009).
- Dietz H, Kirby A, Shek K, Bedwell P. Does avulsion of the puborectalis muscle affect bladder function? Int. Urogynecol. J.20(8), 967–972 (2009).
- Wilson PD, Hay Smith EJ, Nygaard IE et al. Adult conservative management. In: Incontinence: Third International Consultation on Incontinence. Abrams P, Cardozo L, Khoury S, Wein A (Eds). Health Publications Ltd, Paris, France, 855–964 (2005).
- Chantarasorn V, Shek KL, Dietz HP. Levator avulsion is not associated with fecal incontinence. Int. Urogynecol. J.20(S2), S169–S170 (2009).
- Adekanmi OA, Freeman RM, Jackson SA, Puckett M, Bombieri L, Waterfield M. Do the anatomical defects associated with cystocoele affect the outcome of anterior repair? A clinical and radiological study. Int. Urogynecol. J.20, 1369–1377 (2009).
- Shobeiri S, Chimpiri A, Allen AC, Nihira M, Quiroz LH. Surgical reconstitution of a unilaterally avulsed symptomatic puborectalis muscle using autologous fascia lata. Obstet. Gynecol.114(S2), 480–482 (2009).
- Dietz HP, Shek KL. The quantification of levator muscle resting tone by digital assessment. Int. Urogynecol. J.19, 1489–1493 (2008).
- Dietz HP. Pelvic floor assessment: a review. Fetal Matern. Med. Rev.20, 49–66 (2009).
Pelvic floor muscle trauma
To obtain credit, you should first read the journal article. After reading the article, you should be able to answer the following, related, multiple-choice questions. To complete the questions and earn continuing medical education (CME) credit, please go to www.medscapecme.com/journal/expertob. Credit cannot be obtained for tests completed on paper, although you may use the worksheet below to keep a record of your answers. You must be a registered user on Medscape.com. If you are not registered on Medscape.com, please click on the New Users: Free Registration link on the left hand side of the website to register. Only one answer is correct for each question. Once you successfully answer all post-test questions you will be able to view and/or print your certificate. For questions regarding the content of this activity, contact the accredited provider, [email protected]. For technical assistance, contact [email protected]. American Medical Association’s Physician’s Recognition Award (AMA PRA) credits are accepted in the US as evidence of participation in CME activities. For further information on this award, please refer to www.ama-assn.org/ama/pub/category/2922.html. The AMA has determined that physicians not licensed in the US who participate in this CME activity are eligible for AMA PRA Category 1 Credits™. Through agreements that the AMA has made with agencies in some countries, AMA PRA credit is acceptable as evidence of participation in CME activities. If you are not licensed in the US and want to obtain an AMA PRA CME credit, please complete the questions online, print the certificate and present it to your national medical association.
Activity Evaluation: Where 1 is strongly disagree and 5 is strongly agree
1. A 55-year-old woman presents to her women’s health provider noting that she “feels something” in her vagina. Her medical history is significant for 3 full-term vaginal deliveries. Which of the following findings would confirm the practitioner’s suspicion of an avulsion injury to the puborectalis muscle?
□ A Palpable flaccid muscle
□ B Narrow hiatus with pain with palpation
□ C Absence of contractile tissue with palpation over the inferior pubic ramus
□ D Fingertip width space between the urethra and puborectalis muscle laterally
2. Which of the following imaging modalities would be most appropriate to confirm this suspected injury?
□ A Magnetic resonance imaging (MRI)
□ B Computed tomographic (CT) scan
□ C 2D ultrasound
□ D 3D or 4D ultrasound
3. Female pelvic organ prolapse (FPOP) is confirmed in this patient. Which of the following points should be included in discussion with this patient?
□ A Avulsion injuries are common post childbirth and may not lead to FPOP for several years
□ B Avulsion injury as an etiology of her FPOP is unlikely because her symptoms were not noted in the immediate postpartum period
□ C FPOP secondary to avulsion is readily repairable with a low risk for recurrence
□ D Levator avulsion is associated with a high incidence of stress urinary incontinence
4. A 30-year-old nulliparous woman reports that she is hoping to become pregnant. She reports that her older sister has had surgery for FPOP due to an avulsion injury, and she is concerned that she may be at risk for this condition following delivery. While explaining to her that a number of factors may affect the likelihood of avulsion injury and that it is not possible to accurately predict which women will sustain such an injury, you explain that:
□ A Epidural analgesia during delivery is associated with a higher incidence of avulsion
□ B Delivery of a first child before the age of 30 is associated with a lower incidence
□ C Ultrasonographic examination prior to delivery can predict her likelihood of injury and would be cause to recommend a cesarean delivery
□ D Use of forceps or vacuum during delivery, if necessary, will reduce the likelihood of injury