Abstract
Transgender adolescents seek gender-affirming medical care to address gender identity and incongruence. Improved understanding of the dermatologic impact of gender-affirming medical care such as pubertal suppression, hormone therapy, and surgeries can enhance patient outcome. Pubertal suppression treats dysphoria associated with development of secondary sex characteristics, including androgen-driven acne. Gender-affirming hormone therapy influences acne and hair development in transgender adolescents. Dermatologists can help manage skin effects associated with chest binding and gender-affirming hormone therapy and surgery. Provision of patient-centered gender-affirming care in dermatologic and multidisciplinary settings is essential to improve skin and overall outcomes of gender-affirming therapy.
Introduction
Adolescents and young adults have been increasingly seeking care at gender clinics to discuss gender incongruence or dysphoria.Citation1,Citation2 Approximately 0.6% of adults in the United States are transgender.Citation3 Younger people more frequently identify as transgender, with 1.8% of American high school students identifying as such in 2017.Citation4 Up to 2.7% of high school students identified as transgender and/or gender non-conforming in certain states.Citation5
Feelings of gender dysphoria may begin developing as early as the age of 7 years.Citation6 Improved understanding and social destigmatization of gender incongruence have contributed to more transgender patients seeking gender-affirming care.Citation7 Gender-affirming care for adolescents may involve psychosocial care, pubertal suppression, hormone therapy, and/or surgeries.Citation8 This study aims to review: 1) the impact of gender-affirming care on skin and skin conditions in transgender adolescents; 2) management strategies of common dermatological conditions associated with gender-affirming care, and 3) creating a welcoming care environment for transgender adolescents to engage in dermatologic care. For this review, adolescence refers to the period between onset of puberty and 18 to match language in reviewed publications. Young adult refers to those between the ages of 18 and 25.Citation9 Use of “youth” refers to both adolescents and young adults.
Terminology and Definitions
Terms related to transgender health evolve over time and may not be accepted by all members of transgender communities.Citation10,Citation11 We specified the definitions of common terms and concepts related to transgender health in . In this review, we will use the term transgender as an umbrella term for persons whose gender identity is incongruent with one’s assigned sex at birth.Citation12 We will also use the terms describing health of transmasculine, transfeminine, or non-binary populations based on terms used in primary references. Usage of terms differs based on individual preference, as they describe personal gender experiences.Citation11 Providers should use language and terminology that their patients prefer.Citation13
Table 1 Definitions of Common Terms Related to Transgender Health
Overview of Gender-Affirming Care and Implications for Skin Conditions
Pubertal suppression via gonadotropin-releasing hormone (GnRH) agonists delays development of secondary sex characteristics. GnRH agonists inhibit pubertal androgen production, thus reducing androgen-mediated skin issues.Citation18,Citation19
Hormone therapy usually involves using testosterone for transmasculine patients and estrogen for transfeminine patients to develop secondary sex characteristics congruent with their gender identity. Testosterone therapy can cause acne and androgenic alopecia, while estrogen therapy could reduce acne but does not sufficiently reduce unwanted hair.Citation13,Citation20–22
Gender-affirming surgeries further reduce dysphoria. As with other surgical procedures, scarring can present clinical concerns.Citation23,Citation24
Components of gender-affirming care, their dermatological effects, and corresponding management strategies are summarized in .
Table 2 Gender-Affirming Effect and Dermatological Impact of Pubertal Suppression
Acne Epidemiology and Impact of Pubertal Suppression on Acne
Acne affects approximately 85% of patients between the ages of 12–25.Citation33 Acne is the third highest cause of disability-adjusted life year loss among skin diseases and the most common condition seen between the ages of 15–24 in outpatient dermatology practices.Citation34,Citation35 Acne typically starts in puberty due to hormonal changes.Citation36 Severity of acne increases with Tanner stage.Citation37,Citation38 Gender dysphoria also increases around ages 10–13 as endogenous puberty begins and transgender adolescents undergo undesired Tanner development stages.Citation39 Timing of pubertal acne and increasing levels of gender dysphoria thus overlap in transgender adolescents.
Reversible pubertal suppression via gonadotropin-releasing hormone (GnRH) agonists reduces dysphoria in transgender adolescents. Pubertal suppression, typically used from initiation of puberty up until age 16, delays the development of secondary sex characteristics and reduces associated gender dysphoria.Citation11,Citation40,Citation41 Pubertal suppression provides time to explore gender identity before making informed decisions on gender-affirming hormone therapy.Citation39,Citation42–45 Multiple guidelines recommend pubertal suppression to reduce gender dysphoria for transgender adolescents starting puberty above Tanner stage 2 in the absence of contraindications.Citation42,Citation46,Citation47 Pubertal suppression in transgender adolescents significantly improves general functioning and decreases depressive symptoms and suicidal ideation.Citation48–50
Pubertal suppression could alleviate acne, reducing gender dysphoria and acne mental health burdens.Citation51 In adults, GnRH agonists have been used to treat acne and hirsutism by suppressing androgen production.Citation52,Citation53 Pubertal suppression can temporarily exacerbate acne by simulating luteinizing hormone and follicle-stimulating hormone.Citation39 This transient effect generally resolves with continued pubertal suppression.Citation39
Patients receiving pubertal suppression and estrogen/testosterone therapy concurrently required lower doses of hormones to reach gender expression goals compared to patients receiving estrogen/testosterone therapy alone.Citation54 The impact of pubertal suppression on acne incidence and severity, as well as other long-term skin health outcomes, remains to be explored.Citation55 Increased research would help inform healthcare providers on the effects of pubertal suppression.
Impact of Gender-Affirming Hormone Therapy on Acne
For transmasculine adolescents, testosterone therapy can generate or worsen acne.Citation13 In transmasculine individuals taking testosterone, acne commonly develops over the lower third of the face, chest, upper arms, and back – similar in location to hormonal acne in cisgender individuals.Citation13,Citation56
Few studies explored acne epidemiology in transgender adolescents. For transmasculine adolescents using Lynestrenol (a progestin) to induce amenorrhea, acne significantly increased after starting testosterone in combination with Lynestrenol.Citation57 Acne became most prevalent between 6 and 12 months of testosterone therapy for adolescents starting testosterone therapy after pubertal suppression.Citation58 29.6% of young transmasculine adults aged 18–21 experienced acne over 2 years of testosterone treatment, in a study of 988 transmasculine patients.Citation59 Younger age at time of testosterone initiation increases acne incidence, and participants between the ages of 18–25 had the greatest acne risk.Citation59 Transgender young men between 18–29 experience the most moderate-to-severe acne compared to older transgender men.Citation60 Severity of acne presentation has not been systemically studied in transgender adolescents.
Little data exists on dermatologic effects of hormone therapy for transfeminine patients. Estrogen therapy and spironolactone, an anti-androgen, reduce sebum and decrease acne in transfeminine adults.Citation21,Citation61,Citation62
GnRH agonists into adulthood or selective estrogen receptor modulators (SERMs) have been reported for use in gender-affirming therapy for non-binary individuals.Citation63,Citation64 SERMs contribute to skin elasticity in softness in post-menopausal cisgender women, but dermatologic effects have not been explored for non-binary patients.Citation63
Mental Health Among Acne Patients and in Transgender Adolescents
Studies have thoroughly documented acne’s association with mental health comorbidities in the general population. Acne increases depression and anxiety among adolescents.Citation65 Adolescent females tend to have worse mental health burden than adolescent males.Citation66–68
Increasing acne severity in adolescents correlates increased social impairment, lower attachment to friends, and less experience with romantic relationships.Citation69 Increasing perceived social stigma due to acne predicts quality of life impairment among adolescents and young adults.Citation70 Adolescents and young adults with acne have increased association with suicide (either ideation, attempt, or death).Citation71 Concerns about perceived adverse effects, effectiveness of acne treatments, and perceived medical provider trivialization exacerbate psychological impact.Citation72
Few studies linking acne with adverse mental health outcomes focus on transgender and gender non-conforming adolescents, despite their disproportionate mental health burden.Citation73,Citation74 Transgender adolescents experience more bullying in school and have a severalfold higher suicide risk than cisgender adolescents.Citation4,Citation75,Citation76 10% reported leaving school due to mistreatment and lack of support from teachers and peers.Citation77 Transgender and non-binary youth experience increased risk of negative mental health outcomes in comparison to cisgender sexual minority adolescents.Citation78 Socially transitioned transgender pre-pubescent children between 3–12 years have depression and anxiety levels comparable to their cisgender siblings and age-matched peers, suggesting social support throughout transition may reduce negative mental health outcomes.Citation79 Family-connectedness, teacher support, and feeling safe in one’s community protect against negative mental health outcomes among transgender adolescents.Citation5,Citation80 Receiving gender-affirming hormone therapy decreases depression and suicidality and improves well-being.Citation49,Citation81,Citation82
Transmasculine adults receiving testosterone with current moderate-to-severe acne (defined by the patient) reported increased anxiety and depression symptoms compared to those who never had acne in a survey of 283 patients.Citation83 Further research could help characterize how acne’s mental health burden affects not only adults but adolescent transgender patients as well.
Medical provider practices promoting inclusivity improve transgender patient mental health outcomes. Transgender adolescents tend to seek dermatological care from doctors who identify as a sexual or gender minority because of the expectation they will be more respectful toward and more knowledgeable about transgender patient skin conditions.Citation84 More research could characterize how provider-patient relationships affect mental health among transgender adolescents, as most existing literature focuses on transgender adults’ relationships with medical providers. 25.4% of transgender adults postponed medical care when sick because of anticipated discrimination from healthcare providers, and 19% were at some point refused medical treatment due to their gender identity.Citation77,Citation85 Transgender adults reported better mental health if they felt respected by their physician.Citation86 Transgender adults’ perceived healthcare provider comfort with their gender identity predicts wellbeing, independent of health status.Citation87
Current Management Strategies for Acne: Considerations for a Gender Diverse Population
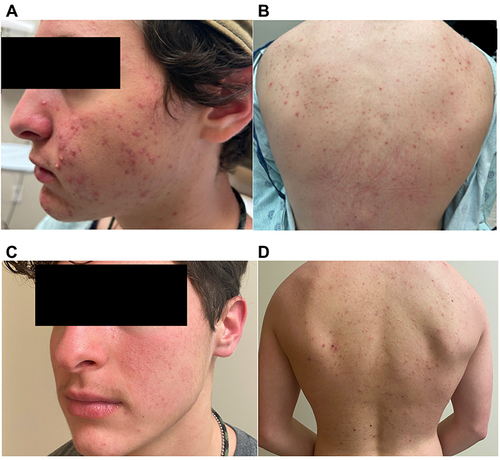
Healthcare providers should proactively address acne as a side effect of gender-affirming care. Successful management of acne results in noticeable improvements when comparing before () and after () treatment.
Figure 1 (A and B) Images of patient before acne treatment (C and D) Improved acne after 3 months of oral doxycycline, benzoyl peroxide wash, and topical tretinoin followed by 2 months of isotretinoin.
Before initiating acne treatment, providers should conduct an organ inventory to assess childbearing potential as many acne treatments are teratogenic.Citation13 In patients who can become pregnant and need teratogenic medication, contraceptive needs and sexual behaviors should not be assumed but rather thoughtfully explored. While conducting organ inventory, providers should use general terms such as “chest” and “genitalia” instead of “breast”, “vagina”, or “penis” to avoid triggering gender dysphoria.Citation88 Pregnancy can occur in transmasculine patients with retained functional uterus and ovaries during and after testosterone therapy if they engage in penis-vagina sexual intercourse with sperm-producing partners.Citation89 Contraception is important for transmasculine persons who can become pregnant who require teratogenic acne mediations, as discussed in detail in the following isotretinoin section.Citation90 Transmasculine patients who have undergone hysterectomy and/or bilateral oophorectomy would not need contraception while taking teratogenic medications.Citation88
With no current evidence-based guidelines for treating hormonal acne in testosterone therapy, treatment plans use guidelines established for treating acne in cisgender persons not receiving hormone therapy.Citation51 Acne is classified as mild, moderate, or severe. Mild acne encompasses having some comedones and no more than a few papules/pustules, moderate acne has some papules/pustules and no more than one nodule, and severe acne consists of having more than one nodule.Citation26
Mild Acne
Topical retinoids like adapalene and tretinoin treat mild to moderate comedonal and inflammatory acne. Topical trifarotene has been specifically studied for treating truncal acne,Citation25 which may be more prominent in patients with testosterone-induced acne. Topical retinoids carry a teratogenic risk and providers should advise patients appropriately.
Topical antibiotics like clindamycin and erythromycin manage mild to moderate acne. Topical antibiotics are often combined with topical benzoyl peroxide to mitigate the risk of resistance and improve effectiveness.Citation26
Topical antiandrogens, such as clascoterone, treat both inflammatory and non-inflammatory facial acne with minimal adverse effects or safety concerns.Citation91 Although clascoterone clinical trials did not document gender-affirming hormone therapy use in participants, topical antiandrogens in transmasculine patients could reduce testosterone action in the skin and curb acne development.Citation27
Moderate-to-Severe Acne
Oral antibiotics, such as doxycycline and minocycline, treat moderate-to-severe acne or acne affecting a large body surface area.Citation28 As doxycycline carries possible teratogenic risk, providers should notify and counsel patients with childbearing potential.Citation92
Spironolactone effectively treats acne in cisgender women.Citation93 Transfeminine patients report improvement in their acne with spironolactone treatment in addition to other anti-androgenic effects which facilitate their transition goals.Citation21 In transmasculine patients, although spironolactone may hypothetically improve acne, it may contradict transition goals by causing irregular bleeding and gynecomastia.Citation94 As an anti-androgen, spironolactone is counterproductive to testosterone therapy.Citation95 Spironolactone carries a teratogenic potential that should be addressed in patients with childbearing potential.Citation96
Hormonal contraceptives address contraception as part of acne treatment but are generally not used as a primary treatment for acne in transmasculine patients.Citation13 Combined oral contraceptives (COCs) containing ethinyl estradiol both treat acne and provide contraception in cisgender women.Citation97 For transmasculine patients, COCs have feminizing effects which may contradict transition goals.Citation98 Progestin-only contraceptives, such as norethinsterone (also known as norethindrone), cease uterine bleeding in alignment with transition goals for transmasculine patients. However, progestin-only contraceptives (including long-acting reversible contraception) could exacerbate acne.Citation13
Oral isotretinoin is indicated for managing scarring acne, moderate acne refractory to other treatments, severe acne, and acne causing psychosocial distress.Citation26 As isotretinoin’s severe teratogenic effects may lead to fetal death, the US Food and Drug Administration requires all patients taking it to be registered in the iPLEDGE program. Effective December 13th, 2021, iPLEDGE program categorizes patients into “patients who can become pregnant” and “patients who cannot get pregnant.”Citation99 While the new gender-neutral classification may not be completely inclusive, it moves towards more inclusive care. iPLEDGE requires patients who can get pregnant to receive monthly contraceptive counseling and pregnancy testing in addition to committing to either complete abstinence with sperm-producing partners or consistent use of two forms of contraception.Citation100 Testosterone therapy, even if amenorrhea is achieved, is neither a reliable contraception method nor a contraindication to other forms of contraception.Citation90,Citation101 In patients who qualify for isotretinoin treatment and are under the age of 18 years, a parent or a legal guardian should read, understand, and sign iPLEDGE.Citation100 However, adolescent patients should be reassured that their confidentiality will be preserved except in cases of abuse that legally require disclosure.
Dermatologic Impacts of Chest Binding, Tucking, and Packing
Although not gender-affirming measures usually provided by clinicians, healthcare providers should familiarize themselves with chest binding, tucking, and packing and associated dermatologic impacts.
Many young transmasculine patients use chest binding to flatten the chest and relieve gender dysphoria before they can get gender-affirming chest reconstruction surgery.Citation102–104 They commonly use commercial binders designed for tight compression, although some use other methods (including elastic bandages or tape) based on financial means and/or parental support.Citation105 Chest binding prevents misgendering and promotes safety and confidence.Citation104 Binding, especially with high frequency, can cause physical side effects.Citation105,Citation106 Chest size correlates with dermatological problems when binding.Citation105 Acne, itch, skin infection, and skin changes affect most who bind.Citation102 33.3% and 45.1% of youth who bind experience acne and itch respectively within the first year of binding, in a survey of 1800 individuals.Citation103 Skin changes, such as skin infection and reduced elasticity, have lower prevalence and a later onset.Citation103 Decreased skin elasticity from chest binding limits options for and/or negatively influences the outcome of gender-affirming chest reconstruction surgery.Citation31,Citation107–109 For patients with decreased skin elasticity, more extensive chest incisions may be required for gender-affirming chest surgery to avoid wrinkling and unevenness of excess skin, resulting in more scarring.Citation110 Prevention of unwanted chest development through pubertal suppression decreases need for chest binding.Citation103
Providers can manage symptoms associated with binding while recognizing the importance of binding for safety and mental health. Aside from addressing acne, providers can help reduce itch with topical emollients.Citation111 Skin infections diagnosed early and treated with appropriate antibiotics have good outcome.Citation112 Although 82.3% of transgender patients recognize the importance of discussing binding with healthcare providers, 56.3% feel safe and comfortable initiating conversation about binding.Citation102 Insensitivity and lack of understanding from healthcare professionals present a large obstacle to care.Citation113 Currently, almost all trans youth report learn about binding online, not in healthcare settings.Citation105 Reduced time binding lessens physical symptoms, but the balance between side effects and benefits of binding depends on the informed decision of the patient.Citation103,Citation106 Health providers can help patients determine their binder sizing and improve accessibility for commercial binders, especially if patients have parental or financial obstacles.Citation104 These measures could help reduce long-term skin and tissue changes.
Similar to binding, tucking or packing help relieve dysphoria non-surgically.Citation114 Tucking in transfeminine individuals involves placing testes upwards, close to the inguinal canal, and securing external genitalia between the legs to flatten the lower pelvis.Citation114,Citation115 70% of transfeminine patients report tucking, with 28%, 21%, and 12% experiencing itch, rash, and skin infection respectively.Citation115 In a survey of 79 transfeminine adults, itching, rash, and testicular pain were the most commonly reported health effects.Citation116 For itch and rash in the groin area, topical emollients to repair skin barrier and antihistamines to suppress the itch-scratch-itch cycle can help.Citation117 Skin infection should be diagnosed and treated promptly with the appropriate antibiotics.Citation112 Transmasculine patients may also “pack” or use “packers” in the underwear to give the appearance of a bulge.Citation114,Citation118 This may cause irritation of tissue in the area.Citation118 Further research is needed to inform clinicians on how to address dermatologic effects of tucking or packing.
Hair Therapy: Impacts of Gender-Affirming Hormone Therapy and Dermatological Strategies to Reduce Gender Dysphoria
Hair growth and/or removal can be an essential element of gender-affirming therapy.Citation119 There is limited data on hair growth for transmasculine adolescents on testosterone. Preliminary data suggests topical minoxidil can help growth of pigmented hair in desired patterns in transmasculine adolescents, including those with limited access to testosterone therapy.Citation120 In transmasculine adults, testosterone therapy significantly increases facial, chest, and abdominal hair growth.Citation121,Citation122 Androgenic alopecia from testosterone therapy, seen in some young adults, may be treated by 5-alpha-reductase inhibitors like finasteride.Citation29 However, 5-alpha-reductase inhibitors may reduce systemic testosterone effects.Citation20,Citation123
84% of transgender women receiving estrogen still report persistent excess facial and body hair.Citation22 This may affect transfeminine adolescents, depending on the stage of puberty. Treatment with cyproterone acetate (note: not available in the USA), an anti-androgen, either alone or in combination with estrogens, reduces the need for facial shaving in transfeminine patients in late adolescence.Citation30
As hormone therapy and pubertal suppression affect hair distribution, temporary solutions like wigs, hair extensions, and hair drawing could facilitate desired gender expression until hormonal effects on hair stabilize. After hair distribution stabilizes, patients can consider more permanent solutions such as hair transplant and hairline lowering surgery.Citation124
For patients who desire hair removal, solutions like shaving, waxing, and depilatory creams may not achieve the desired transition effect. Transfeminine patients can use laser hair removal to safely and effectively reduce unwanted hair.Citation125 Laser hair removal uses light to target hair melanin to destroy follicular bulbs and usually takes up to 6 sessions, each spaced 6 weeks apart.Citation125–127 Laser hair removal is less effective in patients with fairer hair and/or darker skin.Citation128
Transfeminine patients can also reduce unwanted hair via electrolysis. In electrolysis, probes use electrical current to destroy hair follicles.Citation128 Electrolysis can remove any hair color and performs well with fairer hair, unlike laser hair removal.Citation129 Electrolysis often spans over a year or more, with sessions every one or two weeks. Patients report more pain with electrolysis compared to laser hair removal.Citation129,Citation130 Transfeminine patients note inability and/or unwillingness to grow out facial hair for electrolysis.Citation128
Patients who have undergone hair treatment as part of their transition have reported less distress, better subjective well-being, and more body satisfaction compared to their peers.Citation128,Citation131 Transition hair goals should be explored and not assumed based on cisnormative standards. Providers should explore the patients’ hair pattern prior to and during transitioning, family history of hair loss and hirsutism, and possible underlying endocrine and skin conditions that may affect the hair. Patients can be asked to bring model photos and/or draw lines of desired hair distribution.
Dermatological Considerations for Gender-Affirming Surgery
Transmasculine adolescents can undergo gender-affirming chest reconstruction surgery, also known as “top surgery.”Citation31 Top surgery improved quality of life, functioning, and mental health, as testosterone therapy alone was inadequate in relieving gender dysphoria.Citation17,Citation132 Patients may choose “keyhole” or “periareolar” surgery, associated with less scarring.Citation31,Citation133 Patients with reduced skin elasticity or more chest tissue often undergo the “double incision free nipple graft” procedure instead, associated with increased scarring but better outcomes.Citation31,Citation133,Citation134
Isotretinoin may lead to delayed wound healing persisting up to one year after discontinuation, posing a challenge gender-affirming surgery recovery.Citation26 Transgender patients with recent or upcoming surgeries with truncal acne could use oral antibiotics instead to reduce inflammation and scarring and optimize surgical outcomes.Citation13
After gender-affirming surgery, providers should review scar aftercare with patients. Silicone gel improves outcome of surgical wounds.Citation135 Ablative laser resurfacing can remodel scars, and non-ablative lasers help reduce redness of scars.Citation136 Surgical revision techniques, such as a Z-plasty, improve scar aesthetics.Citation137 Transgender patients also get tattoos to cover scars.Citation138 Specialized medical tattooing, known as dermatography, smoothens scars and improves aesthetics.Citation139 Treatment of top surgery scars with a novel topical spironolactone gel resulted in significantly higher patient satisfaction compared with silicone gel alone. Because testosterone could exacerbate scar tissue and keloid development, topical spironolactone could reduce scarring while avoiding undesired anti-androgenic systemic effects of oral spironolactone.Citation32
Hypertrophic scars and keloids can develop because of surgery.Citation31,Citation40,Citation140 Care for keloids generally consists of intralesional corticosteroid injections.Citation141 Other treatments for keloids include silicone gel/sheets, cryotherapy, radiation, and laser therapy.Citation23,Citation24,Citation142 Data regarding keloid treatment comes from general population studies, so further research on how keloid treatments may interact with gender-affirming therapy could help inform care.
Scar revision and treatment for hypertrophic scars applies to other gender-affirming surgeries. For instance, some transmasculine young adults undergo hysterectomy.Citation143 Scarring can be reduced through minimally invasive hysterectomies.Citation144,Citation145 Other gender-affirming surgeries, which most patients undergo at an older age, include vaginoplasty, metoidioplasty, phalloplasty, and breast augmentation surgery.Citation146–150
Improving General Care for Transgender Adolescents: Creating a Welcoming Clinical Setting
Creating a welcoming clinical environment is key to providing a positive healthcare experience for transgender adolescents.Citation13 Some transgender patients avoid seeking healthcare due to anticipated discrimination, cisnormativity, or harassment within healthcare settings.Citation151 Transgender knowledge incompetency of providers and staff, inadequate insurance, and socioeconomic barriers prevent ideal healthcare for transgender patients.Citation152
A successful medical encounter with a transgender patient starts with fostering a gender-inclusive environment including gender-neutral intake forms with no identity assumptions, available all-gender restrooms, and welcoming signs that show support and alliance to transgender patients.Citation101,Citation153 Familiarity with common terminology used by transgender patients facilitates patient-provider conversations.Citation13 Patient-centered language adaptation includes but is not limited to the names and pronouns the patients use in addition to their terms for sexual orientation, gender identity, sexual behavior, and anatomy.Citation11 As some transgender people use names different from the names listed in the medical or legal records, patients should be routinely asked how they should be addressed.Citation13 As sexual orientation and gender identity are fluid, providers should routinely explore and document them on medical records.Citation13 Patients have positively responded to routine collection of sexual orientation and gender identity, which has been advocated for in dermatologic care.Citation154
Providers introducing themselves with their pronouns or wearing pronoun pins may further promote a gender-inclusive environment.Citation13 Physical examination should focus on relevant body parts to the chief complaint with obtaining constant consent prior to examining each body part and bearing in mind that some patients may wear chest binders or other gender-affirming devices.Citation13 To further strengthen rapport, patients should be empowered to take the lead in showing the body parts that are both relevant to the encounter and the patient is comfortable with showing.Citation155
Multidisciplinary Care
Acne treatments may interfere with transition goals, as anti-androgenic compounds and some hormonal contraceptives contradict gender expression goals for transmasculine patients while isotretinoin interferes with wound healing for gender-affirming surgeries. Acne treatment prescribers should also consider logistics behind prescribing acne medications (ie iPLEDGE) or teratogenic risks for patients. Providers should hold a thorough and gender-affirming discussion with transgender patients to better set expectations and learn about transition goals.
Isotretinoin has been associated with psychiatric disturbances such as depression, anxiety, and suicidality.Citation156 Conversely, other studies report that isotretinoin improves depressive symptoms and quality of life in patients with moderate and severe acne.Citation157 Of note, transgender persons have a higher prevalence of depression, anxiety, and suicidality compared to their cisgender peers.Citation158 Providers should routinely screen and monitor for signs of depression and mental health comorbidities in transgender patients, especially those receiving isotretinoin.
Optimal care for transgender patients fosters their transition goals and physical/mental well-being. To achieve this, healthcare providers should ensure multidisciplinary care with clear communication between the patients’ dermatologist, primary care provider, hormone provider, gender-affirming surgeon, reproductive health specialist, and mental health provider.Citation13
Conclusion
To provide comprehensive care to transgender adolescents, providers should understand the dermatological impact of gender-affirming therapy. Increased research on transgender healthcare would clarify skin impacts of gender-affirming therapy. Further research is needed to characterize the impact of GnRH agonists on skin in transgender adolescents. Research should explore whether testosterone-induced acne can be prevented or mitigated. Information about how estrogen therapy affects acne and acne medication considerations for transfeminine patients is lacking. Studies investigating whether acne treatment improves mental health outcomes in transgender teenagers receiving hormone therapy can help providers address side effects with the most impact. Studies should monitor how emerging gender-affirming therapies affect the skin and establish care guidelines that address skin effects while achieving gender affirmation goals.
Patient Consent
The patient in has provided informed consent for the publication of images.
Disclosure
Dr Yeung is supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases under award numbers L30AR076081 and K23AR075888. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or US Department of Veterans Affairs. The authors report no other conflicts of interest in this work.
References
- Bonifacio HJ, Rosenthal SM. Gender Variance and Dysphoria in Children and Adolescents. Pediatr Clin North Am. 2015;62(4):1001–1016. doi:10.1016/j.pcl.2015.04.013
- Chen M, Fuqua J, Eugster EA. Characteristics of Referrals for Gender Dysphoria Over a 13-Year Period. J Adolesc Health. 2016;58(3):369–371. doi:10.1016/j.jadohealth.2015.11.010
- Flores AR, Herman JL, Gates GJ, Brown TN How Many Adults Identify as Transgender in the United States?; 2016. Available from: https://williamsinstitute.law.ucla.edu/publications/trans-adults-united-states/. Accessed May 18, 2022.
- Johns MM, Lowry R, Andrzejewski J, et al. Transgender Identity and Experiences of Violence Victimization, Substance Use, Suicide Risk, and Sexual Risk Behaviors Among High School Students - 19 States and Large Urban School Districts, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(3):67–71. doi:10.15585/mmwr.mm6803a3
- Eisenberg ME, Gower AL, McMorris BJ, Rider GN, Shea G, Coleman E. Risk and Protective Factors in the Lives of Transgender/Gender Nonconforming Adolescents. J Adolesc Health. 2017;61(4):521–526. doi:10.1016/j.jadohealth.2017.04.014
- Zaliznyak M, Bresee C, Garcia MM. Age at First Experience of Gender Dysphoria Among Transgender Adults Seeking Gender-Affirming Surgery. JAMA Netw Open. 2020;3(3):e201236. doi:10.1001/jamanetworkopen.2020.1236
- Skordis N, Kyriakou A, Dror S, Mushailov A, Nicolaides NC. Gender dysphoria in children and adolescents: an overview. Hormones. 2020;19(3):267–276. doi:10.1007/s42000-020-00174-1
- Mahfouda S, Moore JK, Siafarikas A, et al. Gender-affirming hormones and surgery in transgender children and adolescents. Lancet Diabetes Endocrinol. 2019;7(6):484–498. doi:10.1016/S2213-8587(18)30305-X
- Scales PC, Benson PL, Oesterle S, Hill KG, Hawkins JD, Pashak TJ. The dimensions of successful young adult development: a conceptual and measurement framework. Appl Dev Sci. 2016;20(3):150–174. doi:10.1080/10888691.2015.1082429
- Turban JL, Ehrensaft D. Research Review: gender identity in youth: treatment paradigms and controversies. J Child Psychol Psychiatry. 2018;59(12):1228–1243. doi:10.1111/jcpp.12833
- Rafferty J, Yogman M, Baum R. Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents. Pediatrics. 2018;142(4). doi:10.1542/peds.2018-2162
- Gamarel KE, Reisner SL, Laurenceau J-P, Nemoto T, Operario D. Gender minority stress, mental health, and relationship quality: a dyadic investigation of transgender women and their cisgender male partners. J Family Psychol. 2014;28(4):437. doi:10.1037/a0037171
- Radi R, Gold S, Acosta JP, Barron J, Yeung H. Treating Acne in Transgender Persons Receiving Testosterone: a Practical Guide. Am J Clin Dermatol. 2022;23(2):219–229. doi:10.1007/s40257-021-00665-w
- Guss C, Shumer D, Katz-Wise SL. Transgender and gender nonconforming adolescent care: psychosocial and medical considerations. Curr Opin Pediatr. 2015;27(4):421–426. doi:10.1097/MOP.0000000000000240
- Matsuno E, Budge SL. Non-binary/genderqueer identities: a critical review of the literature. Current Sexual Health Rep. 2017;9(3):116–120. doi:10.1007/s11930-017-0111-8
- Goldhammer H, Malina S, Keuroghlian AS. Communicating With Patients Who Have Nonbinary Gender Identities. Ann Fam Med. 2018;16(6):559–562. doi:10.1370/afm.2321
- Olson-Kennedy J, Warus J, Okonta V, Belzer M, Clark LF. Chest Reconstruction and Chest Dysphoria in Transmasculine Minors and Young Adults: comparisons of Nonsurgical and Postsurgical Cohorts. JAMA Pediatr. 2018;172(5):431–436. doi:10.1001/jamapediatrics.2017.5440
- Robeva R, Assyov Y, Tomova A, Kumanov P. Acne vulgaris is associated with intensive pubertal development and altitude of residence--A cross-sectional population-based study on 6200 boys. Eur J Pediatr. 2013;172(4):465–471. doi:10.1007/s00431-012-1907-1
- Napolitano M, Ruggiero G, Monfrecola G, Megna M. Acne prevalence in 9 to 14-year-old old patients attending pediatric ambulatory clinics in Italy. Int J Dermatol. 2018;57(11):1320–1323. doi:10.1111/ijd.14138
- Marks DH, Senna MM. Androgenetic Alopecia in Gender Minority Patients. Dermatol Clin. 2020;38(2):239–247. doi:10.1016/j.det.2019.10.010
- Giltay EJ, Gooren LJ. Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females. J Clin Endocrinol Metab. 2000;85(8):2913–2921. doi:10.1210/jcem.85.8.6710
- Marks DH, Hagigeorges D, Manatis-Lornell AJ, Dommasch E, Senna MM. Excess hair, hair removal methods, and barriers to care in gender minority patients: a survey study. J Cosmet Dermatol. 2020;19(6):1494–1498. doi:10.1111/jocd.13164
- Betarbet U, Blalock TW. Keloids: a Review of Etiology, Prevention, and Treatment. J Clin Aesthet Dermatol. 2020;13(2):33–43.
- Commander SJ, Chamata E, Cox J, Dickey RM, Lee EI. Update on Postsurgical Scar Management. Semin Plast Surg. 2016;30(3):122–128. doi:10.1055/s-0036-1584824
- Tan J, Thiboutot D, Popp G, et al. Randomized Phase 3 evaluation of trifarotene 50 μg/g cream treatment of moderate facial and truncal acne. J Am Acad Dermatol. 2019;80(6):1691–1699. doi:10.1016/j.jaad.2019.02.044
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945–973.e933. doi:10.1016/j.jaad.2015.12.037
- Marks DH, Mansh MD. Potential Role for Topical Antiandrogens in the Management of Acne Among Patients Receiving Masculinizing Hormone Therapy. JAMA Dermatol. 2020;156(12):1380–1381. doi:10.1001/jamadermatol.2020.4380
- Webster GF, Graber EM. Antibiotic treatment for acne vulgaris. Semin Cutan Med Surg. 2008;27(3):183–187. doi:10.1016/j.sder.2008.07.001
- Motosko CC, Tosti A. Dermatologic Care of Hair in Transgender Patients: a Systematic Review of Literature. Dermatol Ther (Heidelb). 2021;11(5):1457–1468. doi:10.1007/s13555-021-00574-0
- Tack LJW, Heyse R, Craen M, et al. Consecutive Cyproterone Acetate and Estradiol Treatment in Late-Pubertal Transgender Female Adolescents. J Sex Med. 2017;14(5):747–757. doi:10.1016/j.jsxm.2017.03.251
- McEvenue G, Xu FZ, Cai R, McLean H. Female-to-Male Gender Affirming Top Surgery: a Single Surgeon’s 15-Year Retrospective Review and Treatment Algorithm. Aesthetic Surgery J. 2018;38(1):49–57. doi:10.1093/asj/sjx116
- Tanini S, Calabrese S, Fisher AD, Maggi M, Lo Russo G. When Testosterone Needs to be Contrasted: a Preliminary Study of Scar Prevention in Transmen Top Surgery with an Innovative Galenic Preparation. Aesthetic Plast Surg. 2020;44(3):1006–1013. doi:10.1007/s00266-020-01678-2
- Lynn DD, Umari T, Dunnick CA, Dellavalle RP. The epidemiology of acne vulgaris in late adolescence. Adolesc Health Med Ther. 2016;7:13–25. doi:10.2147/AHMT.S55832
- Ho T, Taylor MT, Marathe KS, Lucky AW, Barbieri JS. Most common pediatric skin conditions managed in outpatient dermatology clinics in the United States stratified by race and ethnicity. Pediatr Dermatol. 2021;38(Suppl 2):129–131. doi:10.1111/pde.14693
- Hay RJ, Johns NE, Williams HC, et al. The global burden of skin disease in 2010: an analysis of the prevalence and impact of skin conditions. J Invest Dermatol. 2014;134(6):1527–1534. doi:10.1038/jid.2013.446
- Friedlander SF, Eichenfield LF, Fowler JF, Fried RG, Levy ML, Webster GF. Acne epidemiology and pathophysiology. Semin Cutan Med Surg. 2010;29(2 Suppl 1):2–4. doi:10.1016/j.sder.2010.04.002
- Mancini AJ, Baldwin HE, Eichenfield LF, Friedlander SF, Yan AC. Acne life cycle: the spectrum of pediatric disease. Semin Cutan Med Surg. 2011;30(3 Suppl):S2–5. doi:10.1016/j.sder.2011.07.003
- Lucky AW, Biro FM, Huster GA, Morrison JA, Elder N. Acne vulgaris in early adolescent boys. Correlations with pubertal maturation and age. Arch Dermatol. 1991;127(2):210–216. doi:10.1001/archderm.1991.01680020078009
- Panagiotakopoulos L. Transgender medicine - puberty suppression. Rev Endocr Metab Disord. 2018;19(3):221–225. doi:10.1007/s11154-018-9457-0
- Kosche C, Mansh M, Luskus M, et al. Dermatologic care of sexual and gender minority/LGBTQIA youth, Part 2: recognition and management of the unique dermatologic needs of SGM adolescents. Pediatr Dermatol. 2019;36(5):587–593. doi:10.1111/pde.13898
- Leibowitz S, de Vries ALC. Gender dysphoria in adolescence. Int Rev Psychiatry. 2016;28(1):21–35. doi:10.3109/09540261.2015.1124844
- Hembree WC, Cohen-Kettenis PT, Gooren L, et al. Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: an Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2017;102(11):3869–3903. doi:10.1210/jc.2017-01658
- Giordano S, Holm S. Is puberty delaying treatment ‘experimental treatment’? Int J Transgend Health. 2020;21(2):113–121. doi:10.1080/26895269.2020.1747768
- Delemarre-van de Waal HA, Cohen-Kettenis PT. Clinical management of gender identity disorder in adolescents: a protocol on psychological and paediatric endocrinology aspects. Eur J Endocrinology Eur J Endocrinol. 2006;155(suppl_1):S131–S137. doi:10.1530/eje.1.02231
- Brik T, Vrouenraets L, de Vries MC, Hannema SE. Trajectories of Adolescents Treated with Gonadotropin-Releasing Hormone Analogues for Gender Dysphoria. Arch Sex Behav. 2020;49(7):2611–2618. doi:10.1007/s10508-020-01660-8
- World Professional Association for Transgender Health. Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People [7th Version]; 2012.
- Pediatric Endocrine Society. Pediatric Endocrine Society Statement Against Public Discourse That Risks the Well-Being of Transgender and Gender Diverse Youth and Their Families; 2019.
- de Vries AL, Steensma TD, Doreleijers TA, Cohen-Kettenis PT. Puberty suppression in adolescents with gender identity disorder: a prospective follow-up study. J Sex Med. 2011;8(8):2276–2283. doi:10.1111/j.1743-6109.2010.01943.x
- Tordoff DM, Wanta JW, Collin A, Stepney C, Inwards-Breland DJ, Ahrens K. Mental Health Outcomes in Transgender and Nonbinary Youths Receiving Gender-Affirming Care. JAMA Network Open. 2022;5(2):e220978. doi:10.1001/jamanetworkopen.2022.0978
- Turban JL, King D, Carswell JM, Keuroghlian AS. Pubertal Suppression for Transgender Youth and Risk of Suicidal Ideation. Pediatrics. 2020;145(2):e20191725. doi:10.1542/peds.2019-1725
- Ragmanauskaite L, Kahn B, Ly B, Yeung H. Acne and the Lesbian, Gay, Bisexual, or Transgender Teenager. Dermatol Clin. 2020;38(2):219–226. doi:10.1016/j.det.2019.10.006
- Faloia E, Filipponi S, Mancini V, Morosini P, De Pirro R. Treatment with a gonadotropin-releasing hormone agonist in acne or idiopathic hirsutism. J Endocrinol Invest. 1993;16(9):675–677. doi:10.1007/BF03348907
- Barros B, Thiboutot D. Hormonal therapies for acne. Clin Dermatol. 2017;35(2):168–172.
- Jensen RK, Jensen JK, Simons LK, Chen D, Rosoklija I, Finlayson CA. Effect of Concurrent Gonadotropin-Releasing Hormone Agonist Treatment on Dose and Side Effects of Gender-Affirming Hormone Therapy in Adolescent Transgender Patients. Transgender Health. 2019;4(1):300–303.
- Rew L, Young CC, Monge M, Bogucka R. Review: puberty blockers for transgender and gender diverse youth—a critical review of the literature. Child Adolesc Ment Health. 2021;26(1):3–14. doi:10.1111/camh.12437
- Lucky AW. Hormonal correlates of acne and hirsutism. Am J Med. 1995;98(1a):89s–94s. doi:10.1016/S0002-9343(99)80064-3
- Tack LJ, Craen M, Dhondt K, Vanden Bossche H, Laridaen J, Cools M. Consecutive lynestrenol and cross-sex hormone treatment in biological female adolescents with gender dysphoria: a retrospective analysis. Biol Sex Differ. 2016;7:14. doi:10.1186/s13293-016-0067-9
- Stoffers IE, de Vries MC, Hannema SE. Physical changes, laboratory parameters, and bone mineral density during testosterone treatment in adolescents with gender dysphoria. J Sex Med. 2019;16(9):1459–1468. doi:10.1016/j.jsxm.2019.06.014
- Thoreson N, Park JA, Grasso C, et al. Incidence and Factors Associated With Acne Among Transgender Patients Receiving Masculinizing Hormone Therapy. JAMA Dermatol. 2021;157(3):290–295. doi:10.1001/jamadermatol.2020.5347
- Yeung H, Ragmanauskaite L, Zhang Q, et al. Prevalence of moderate to severe acne in transgender adults: a cross-sectional survey. J Am Acad Dermatol. 2020;83(5):1450–1452. doi:10.1016/j.jaad.2020.02.053
- Swink SM, Castelo-Soccio L. Dermatologic considerations for transgender and gender diverse youth. Pediatr Dermatol. 2021;38(Suppl 2):58–64. doi:10.1111/pde.14685
- Endly DC, Miller RA. Oily Skin: a review of Treatment Options. J Clin Aesthet Dermatol. 2017;10(8):49–55.
- Xu JY, O’Connell MA, Notini L, Cheung AS, Zwickl S, Pang KC. Selective Estrogen Receptor Modulators: a Potential Option For Non-Binary Gender-Affirming Hormonal Care? Front Endocrinol (Lausanne). 2021;12:701364. doi:10.3389/fendo.2021.701364
- Notini L, Earp BD, Gillam L, et al. Forever young? The ethics of ongoing puberty suppression for non-binary adults. J Med Ethics. 2020;46(11):743. doi:10.1136/medethics-2019-106012
- Natsuaki M, Yates T. Adolescent Acne and Disparities in Mental Health. Child Dev Perspect. 2021;2:15.
- Aktan S, Ozmen E, Sanli B. Anxiety, depression, and nature of acne vulgaris in adolescents. Int J Dermatol. 2000;39(5):354–357. doi:10.1046/j.1365-4362.2000.00907.x
- Kubota Y, Shirahige Y, Nakai K, Katsuura J, Moriue T, Yoneda K. Community-based epidemiological study of psychosocial effects of acne in Japanese adolescents. J Dermatol. 2010;37(7):617–622. doi:10.1111/j.1346-8138.2010.00855.x
- Jones-Caballero M, Chren MM, Soler B, Pedrosa E, Peñas PF. Quality of life in mild to moderate acne: relationship to clinical severity and factors influencing change with treatment. J Eur Acad Dermatol Venereol. 2007;21(2):219–226. doi:10.1111/j.1468-3083.2006.01907.x
- Halvorsen JA, Stern RS, Dalgard F, Thoresen M, Bjertness E, Lien L. Suicidal ideation, mental health problems, and social impairment are increased in adolescents with acne: a population-based study. J Invest Dermatol. 2011;131(2):363–370. doi:10.1038/jid.2010.264
- Davern J, O’Donnell AT. Stigma predicts health-related quality of life impairment, psychological distress, and somatic symptoms in acne sufferers. PLoS One. 2018;13(9):e0205009. doi:10.1371/journal.pone.0205009
- Xu S, Zhu Y, Hu H, et al. The analysis of acne increasing suicide risk. Medicine. 2021;100(24):e26035. doi:10.1097/MD.0000000000026035
- Ip A, Muller I, Geraghty AWA, Platt D, Little P, Santer M. Views and experiences of people with acne vulgaris and healthcare professionals about treatments: systematic review and thematic synthesis of qualitative research. BMJ Open. 2021;11(2):e041794. doi:10.1136/bmjopen-2020-041794
- Reisner SL, Vetters R, Leclerc M, et al. Mental health of transgender youth in care at an adolescent urban community health center: a matched retrospective cohort study. J Adolesc Health. 2015;56(3):274–279. doi:10.1016/j.jadohealth.2014.10.264
- Veale JF, Watson RJ, Peter T, Saewyc EM. Mental Health Disparities Among Canadian Transgender Youth. J Adolesc Health. 2017;60(1):44–49. doi:10.1016/j.jadohealth.2016.09.014
- Becerra-Culqui TA, Liu Y, Nash R, et al. Mental Health of Transgender and Gender Nonconforming Youth Compared With Their Peers. Pediatrics. 2018;141(5). doi:10.1542/peds.2017-3845.
- Di Giacomo E, Krausz M, Colmegna F, Aspesi F, Clerici M. Estimating the Risk of Attempted Suicide Among Sexual Minority Youths: a Systematic Review and Meta-analysis. JAMA Pediatr. 2018;172(12):1145–1152. doi:10.1001/jamapediatrics.2018.2731
- Liszewski W, Peebles JK, Yeung H, Arron S. Persons of Nonbinary Gender - Awareness, Visibility, and Health Disparities. N Engl J Med. 2018;379(25):2391–2393. doi:10.1056/NEJMp1812005
- Price-Feeney M, Green AE, Dorison S. Understanding the Mental Health of Transgender and Nonbinary Youth. J Adolesc Health. 2020;66(6):684–690. doi:10.1016/j.jadohealth.2019.11.314
- Olson KR, Durwood L, DeMeules M, McLaughlin KA. Mental Health of Transgender Children Who Are Supported in Their Identities. Pediatrics. 2016;137(3):e20153223. doi:10.1542/peds.2015-3223
- Taliaferro LA, McMorris BJ, Rider GN, Eisenberg ME. Risk and Protective Factors for Self-Harm in a Population-Based Sample of Transgender Youth. Arch Suicide Res. 2019;23(2):203–221. doi:10.1080/13811118.2018.1430639
- Allen LR, Watson LB, Egan AM, Moser CN. Well-being and suicidality among transgender youth after gender-affirming hormones. Clin Practice Pediatric Psychol. 2019;7(3):302. doi:10.1037/cpp0000288
- Green AE, DeChants JP, Price MN, Davis CK. Association of Gender-Affirming Hormone Therapy With Depression, Thoughts of Suicide, and Attempted Suicide Among Transgender and Nonbinary Youth. J Adolesc Health. 2022;70(4):643–649. doi:10.1016/j.jadohealth.2021.10.036
- Braun H, Zhang Q, Getahun D, et al. Moderate-to-Severe Acne and Mental Health Symptoms in Transmasculine Persons Who Have Received Testosterone. JAMA Dermatol. 2021;157(3):344–346. doi:10.1001/jamadermatol.2020.5353
- Covelli I, Ahrens K, Onchiri FM, Inwards-Breland D, Boos MD. Influence of gender and sexual identity on adolescent skin health. Pediatr Dermatol. 2021;38(Suppl 2):65–72. doi:10.1111/pde.14686
- Cruz TM. Assessing access to care for transgender and gender nonconforming people: a consideration of diversity in combating discrimination. Soc Sci Med. 2014;110:65–73. doi:10.1016/j.socscimed.2014.03.032
- Riggs DW, Coleman K, Due C. Healthcare experiences of gender diverse Australians: a mixed-methods, self-report survey. BMC Public Health. 2014;14:230. doi:10.1186/1471-2458-14-230
- Stanton MC, Ali S, Chaudhuri S. Individual, social and community-level predictors of wellbeing in a US sample of transgender and gender non-conforming individuals. Cult Health Sex. 2017;19(1):32–49. doi:10.1080/13691058.2016.1189596
- Krempasky C, Harris M, Abern L, Grimstad F. Contraception across the transmasculine spectrum. Am J Obstet Gynecol. 2020;222(2):134–143. doi:10.1016/j.ajog.2019.07.043
- Light AD, Obedin-Maliver J, Sevelius JM, Kerns JL. Transgender men who experienced pregnancy after female-to-male gender transitioning. Obstet Gynecol. 2014;124(6):1120–1127. doi:10.1097/AOG.0000000000000540
- Yeung H, Chen SC, Katz KA, Stoff BK. Prescribing isotretinoin in the United States for transgender individuals: ethical considerations. J Am Acad Dermatol. 2016;75(3):648–651. doi:10.1016/j.jaad.2016.03.042
- Hebert A, Thiboutot D, Stein Gold L, et al. Efficacy and Safety of Topical Clascoterone Cream, 1%, for Treatment in Patients With Facial Acne: two Phase 3 Randomized Clinical Trials. JAMA Dermatol. 2020;156(6):621–630. doi:10.1001/jamadermatol.2020.0465
- Nahum GG, Uhl K, Kennedy DL. Antibiotic use in pregnancy and lactation: what is and is not known about teratogenic and toxic risks. Obstet Gynecol. 2006;107(5):1120–1138. doi:10.1097/01.AOG.0000216197.26783.b5
- Grandhi R, Alikhan A. Spironolactone for the Treatment of Acne: a 4-Year Retrospective Study. Dermatology. 2017;233(2–3):141–144. doi:10.1159/000471799
- Layton AM, Eady EA, Whitehouse H, Del Rosso JQ, Fedorowicz Z, van Zuuren EJ. Oral Spironolactone for Acne Vulgaris in Adult Females: a Hybrid Systematic Review. Am J Clin Dermatol. 2017;18(2):169–191. doi:10.1007/s40257-016-0245-x
- Angus L, Leemaqz S, Ooi O, et al. Cyproterone acetate or spironolactone in lowering testosterone concentrations for transgender individuals receiving oestradiol therapy. Endocr Connect. 2019;8(7):935–940. doi:10.1530/EC-19-0272
- Oge LK, Broussard A, Marshall MD. Acne Vulgaris: diagnosis and Treatment. Am Fam Physician. 2019;100(8):475–484.
- Fox L, Csongradi C, Aucamp M, du Plessis J, Gerber M. Treatment Modalities for Acne. Molecules. 2016;21(8):1063. doi:10.3390/molecules21081063
- Carswell JM, Roberts SA. Induction and Maintenance of Amenorrhea in Transmasculine and Nonbinary Adolescents. Transgend Health. 2017;2(1):195–201. doi:10.1089/trgh.2017.0021
- Administration UFaD. iPLEDGE Risk Evaluation and Mitigation Strategy (REMS). Available from: https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/ipledge-risk-evaluation-and-mitigation-strategy-rems. Accessed Jun 6, 2022.
- iPLEDGE. Prescriber isotretinoin educational kit. Available from: https://www.dermla.com/wp-content/uploads/2021/09/Prescriber-Isotretinoin-Educational-Kit-1.pdf. Accessed Jun 6, 2022.
- Yeung H, Luk KM, Chen SC, Ginsberg BA, Katz KA. Dermatologic care for lesbian, gay, bisexual, and transgender persons: terminology, demographics, health disparities, and approaches to care. J Am Acad Dermatol. 2019;80(3):581–589. doi:10.1016/j.jaad.2018.02.042
- Jarrett BA, Corbet AL, Gardner IH, Weinand JD, Peitzmeier SM. Chest Binding and Care Seeking Among Transmasculine Adults: a Cross-Sectional Study. Transgender Health. 2018;3(1):170–178. doi:10.1089/trgh.2018.0017
- Peitzmeier SM, Silberholz J, Gardner IH, Weinand J, Acevedo K. Time to First Onset of Chest Binding-Related Symptoms in Transgender Youth. Pediatrics. 2021;147(3). doi:10.1542/peds.2020-0728
- Julian JM, Salvetti B, Held JI, Murray PM, Lara-Rojas L, Olson-Kennedy J. The Impact of Chest Binding in Transgender and Gender Diverse Youth and Young Adults. J Adolescent Health. 2021;68(6):1129–1134. doi:10.1016/j.jadohealth.2020.09.029
- Peitzmeier S, Gardner I, Weinand J, Corbet A, Acevedo K. Health impact of chest binding among transgender adults: a community-engaged, cross-sectional study. Cult Health Sex. 2017;19(1):64–75. doi:10.1080/13691058.2016.1191675
- Peitzmeier SM, Gardner IH, Weinand J, Corbet A, Acevedo K. Chest binding in context: stigma, fear, and lack of information drive negative outcomes. Cult Health Sex. 2022;24(2):284–287. doi:10.1080/13691058.2021.1970814
- Wilson SC, Morrison SD, Anzai L, et al. Masculinizing Top Surgery: a Systematic Review of Techniques and Outcomes. Ann Plast Surg. 2018;80(6):679–683. doi:10.1097/SAP.0000000000001354
- Perez-Alvarez IM, Zolper EG, Schwitzer J, Fan KL, Del Corral GA. Incidence of Complications in Chest Wall Masculinization for the Obese Female-to-Male Transgender Population: a Case Series. World J Plast Surg. 2021;10(2):14–24. doi:10.52547/wjps.10.2.14
- Etemad SA, Furuyama WM, Winocour JS. Double Incision Mastectomy with Free Nipple Graft for Masculinizing Chest Wall Surgery. Plast Reconstr Surg Glob Open. 2020;8(11):e3184. doi:10.1097/GOX.0000000000003184
- Monstrey S, Selvaggi G, Ceulemans P, et al. Chest-Wall Contouring Surgery in Female-to-Male Transsexuals: a New Algorithm. Plast Reconstr Surg. 2008;121(3):849–859. doi:10.1097/01.prs.0000299921.15447.b2
- Kang S-Y, Um J-Y, Chung B-Y, Kim J-C, Park C-W, Kim H-O. Differential Diagnosis and Treatment of Itching in Children and Adolescents. Biomedicines. 2021;9(8):919. doi:10.3390/biomedicines9080919
- Tognetti L, Martinelli C, Berti S, et al. Bacterial skin and soft tissue infections: review of the epidemiology, microbiology, aetiopathogenesis and treatment: a collaboration between dermatologists and infectivologists. J Eur Acad Dermatol Venereol. 2012;26(8):931–941. doi:10.1111/j.1468-3083.2011.04416.x
- Lee A, Simpson P, Haire B. The binding practices of transgender and gender-diverse adults in Sydney, Australia. Cult Health Sex. 2019;21(9):969–984. doi:10.1080/13691058.2018.1529335
- Tollinche LE, Van Rooyen C, Afonso A, Fischer GW, Yeoh CB. Considerations for Transgender Patients Perioperatively. Anesthesiol Clin. 2020;38(2):311–326. doi:10.1016/j.anclin.2020.01.009
- Poteat T, Malik M, Cooney E. 2148 Understanding the health effects of binding and tucking for gender affirmation. J Clin Translational Sci. 2018;2(S1):76. doi:10.1017/cts.2018.268
- Malik M, Cooney EE, Brevelle J-M, Poteat T. Tucking Practices and Attributed Health Effects in Transfeminine Individuals. Transgender Health. 2022. doi:10.1089/trgh.2022.0064
- Swamiappan M. Anogenital Pruritus - An Overview. J Clin Diagn Res. 2016;10(4):We01–03.
- Williamson C. Providing Care to Transgender Persons: a Clinical Approach to Primary Care, Hormones, and HIV Management. J Assoc Nurses AIDS Care. 2010;21(3):221–229. doi:10.1016/j.jana.2010.02.004
- Bared A, Epstein JS. Hair Transplantation Techniques for the Transgender Patient. Facial Plast Surg Clin North Am. 2019;27(2):227–232. doi:10.1016/j.fsc.2018.12.005
- Pang KC, Nguyen TP, Upreti R. Case Report: successful Use of Minoxidil to Promote Facial Hair Growth in an Adolescent Transgender Male. Front Endocrinol (Lausanne). 2021;12:725269. doi:10.3389/fendo.2021.725269
- Wierckx K, Van de Peer F, Verhaeghe E, et al. Short- and long-term clinical skin effects of testosterone treatment in trans men. J Sex Med. 2014;11(1):222–229.
- Motosko CC, Zakhem GA, Pomeranz MK, et al. Effect of testosterone on chests and abdomens of transgender men. J Am Acad Dermatol. 2019;81(2):634–636. doi:10.1016/j.jaad.2019.01.030
- Irwig MS. Is there a role for 5α-reductase inhibitors in transgender individuals? Andrology. 2021;9(6):1729–1731.
- Capitán L, Simon D, Meyer T, et al. Facial Feminization Surgery: simultaneous Hair Transplant during Forehead Reconstruction. Plast Reconstr Surg. 2017;139(3):573–584. doi:10.1097/PRS.0000000000003149
- Vilenchik V, Thomas K, Baker L, Hitchens E, Keith D. Laser therapy is a safe and effective treatment for unwanted hair in adults undergoing male to female sex reassignment. Clin Exp Dermatol. 2021;46(3):541–543. doi:10.1111/ced.14466
- Sabra JJ, Fang CX, Kundu RV, Knowledge-Based A. Assessment of Dermatological Care for Transgender Women. Transgend Health. 2018;3(1):71–73. doi:10.1089/trgh.2018.0001
- Gao Y, Maurer T, Mirmirani P. Understanding and Addressing Hair Disorders in Transgender Individuals. Am J Clin Dermatol. 2018;19(4):517–527. doi:10.1007/s40257-018-0343-z
- Bradford NJ, Rider GN, Spencer KG. Hair removal and psychological well-being in transfeminine adults: associations with gender dysphoria and gender euphoria. J Dermatolog Treat. 2021;32(6):635–642. doi:10.1080/09546634.2019.1687823
- Harris K, Ferguson J, Hills S. A comparative study of hair removal at an NHS hospital: luminette intense pulsed light versus electrolysis. J Dermatolog Treat. 2014;25(2):169–173. doi:10.3109/09546634.2012.715239
- Görgü M, Aslan G, Aköz T, Erdoğan B. Comparison of alexandrite laser and electrolysis for hair removal. Dermatol Surg. 2000;26(1):37–41. doi:10.1046/j.1524-4725.2000.99104.x
- Testa RJ, Rider GN, Haug NA, Balsam KF. Gender confirming medical interventions and eating disorder symptoms among transgender individuals. Health Psychol. 2017;36(10):927–936. doi:10.1037/hea0000497
- Mehringer JE, Harrison JB, Quain KM, Shea JA, Hawkins LA, Dowshen NL. Experience of Chest Dysphoria and Masculinizing Chest Surgery in Transmasculine Youth. Pediatrics. 2021;147(3). doi:10.1542/peds.2020-013300
- Kamali A, Sigurjónsson H, Gran I, et al. Improved surgical outcome with double incision and free nipple graft in gender confirmation mastectomy. Plast Reconstr Surg Glob Open. 2021;9(7):e3628. doi:10.1097/GOX.0000000000003628
- Ammari T, Sluiter EC, Gast K, Kuzon WM. Female-to-Male Gender-Affirming Chest Reconstruction Surgery. Aesthetic Surgery J. 2019;39(2):150–163. doi:10.1093/asj/sjy098
- de Giorgi V, Sestini S, Mannone F, et al. The use of silicone gel in the treatment of fresh surgical scars: a randomized study. Clin Exp Dermatol. 2009;34(6):688–693. doi:10.1111/j.1365-2230.2008.03096.x
- Garg S, Dahiya N, Gupta S. Surgical scar revision: an overview. J Cutan Aesthet Surg. 2014;7(1):3–13. doi:10.4103/0974-2077.129959
- Aasi SZ. Z-plasty made simple. Dermatol Res Pract. 2010;2010:982623. doi:10.1155/2010/982623
- Ragmanauskaite L, Kim J, Zhang Q, et al. Self-reported tattoo prevalence and motivations in transgender adults: a cross-sectional survey. Dermatol Online J. 2020;26(12). doi:10.5070/D32612051353.
- Drost BH, van de Langenberg R, Manusama OR, et al. Dermatography (Medical Tattooing) for Scars and Skin Grafts in Head and Neck Patients to Improve Appearance and Quality of Life. JAMA Facial Plast Surg. 2017;19(1):16–22. doi:10.1001/jamafacial.2016.1084
- Naides AI, Schultz JJ, Shulzhenko NO, Keith JD. Chest Masculinization Technique and Outcomes in 72 Double-incision Chest-contouring Procedures with Free Nipple Grafting. Plastic Reconstructive Surgery. 2021;9(3):e3459. doi:10.1097/GOX.0000000000003459
- Trisliana Perdanasari A, Torresetti M, Grassetti L, et al. Intralesional injection treatment of hypertrophic scars and keloids: a systematic review regarding outcomes. Burns Trauma. 2015;3:14. doi:10.1186/s41038-015-0015-7
- Mercer NS. Silicone gel in the treatment of keloid scars. Br J Plast Surg. 1989;42(1):83–87. doi:10.1016/S0007-1226(89)90119-7
- Committee Opinion No. 685: care for Transgender Adolescents. Obstet Gynecol. 2017;129(1):e11–e16. doi:10.1097/AOG.0000000000001861
- Bretschneider CE, Sheyn D, Pollard R, Ferrando CA. Complication Rates and Outcomes After Hysterectomy in Transgender Men. Obstet Gynecol. 2018;132(5):1265–1273. doi:10.1097/AOG.0000000000002936
- McCarus SD. Scar assessment for patients undergoing minimal invasive hysterectomy. Surg Technol Int. 2014;25:150–156.
- Kailas M, Lu HMS, Rothman EF, Safer JD. Prevalence and Types of Gender-Affirming Surgery Among A Sample of Transgender Endocrinology Patients Prior to State Expansion of Insurance Coverage. Endocrine Practice. 2017;23(7):780–786. doi:10.4158/EP161727.OR
- de Blok CJM, Staphorsius AS, Wiepjes CM, Smit JM, Nanayakkara PWB, den Heijer M. Frequency, Determinants, and Satisfaction of Breast Augmentation in Trans Women Receiving Hormone Treatment. J Sex Med. 2020;17(2):342–348. doi:10.1016/j.jsxm.2019.10.021
- Gaither TW, Awad MA, Osterberg EC, et al. Postoperative Complications following Primary Penile Inversion Vaginoplasty among 330 Male-to-Female Transgender Patients. J Urol. 2018;199(3):760–765. doi:10.1016/j.juro.2017.10.013
- van der Sluis WB, Smit JM, Pigot GLS, et al. Double flap phalloplasty in transgender men: surgical technique and outcome of pedicled anterolateral thigh flap phalloplasty combined with radial forearm free flap urethral reconstruction. Microsurgery. 2017;37(8):917–923. doi:10.1002/micr.30190
- Bordas N, Stojanovic B, Bizic M, Szanto A, Djordjevic ML. Metoidioplasty: surgical Options and Outcomes in 813 Cases. Front Endocrinol (Lausanne). 2021;12:760284. doi:10.3389/fendo.2021.760284
- Kcomt L, Gorey KM, Barrett BJ, McCabe SE. Healthcare avoidance due to anticipated discrimination among transgender people: a call to create trans-affirmative environments. SSM Popul Health. 2020;11:100608. doi:10.1016/j.ssmph.2020.100608
- Safer JD, Coleman E, Feldman J, et al. Barriers to healthcare for transgender individuals. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):168–171. doi:10.1097/MED.0000000000000227
- Boos MD, Yeung H, Inwards-Breland D. Dermatologic care of sexual and gender minority/LGBTQIA youth, Part I: an update for the dermatologist on providing inclusive care. Pediatr Dermatol. 2019;36(5):581–586. doi:10.1111/pde.13896
- Haider A, Adler RR, Schneider E, et al. Assessment of Patient-Centered Approaches to Collect Sexual Orientation and Gender Identity Information in the Emergency Department: the EQUALITY Study. JAMA Netw Open. 2018;1(8):e186506. doi:10.1001/jamanetworkopen.2018.6506
- Hashemi L, Weinreb J, Weimer AK, Weiss RL. Transgender care in the primary care setting: a review of guidelines and literature. Fed Pract. 2018;35(7):30–37.
- Marqueling AL, Zane LT. Depression and suicidal behavior in acne patients treated with isotretinoin: a systematic review. Semin Cutan Med Surg. 2005;24(2):92–102. doi:10.1016/j.sder.2005.04.003
- Huang YC, Cheng YC. Isotretinoin treatment for acne and risk of depression: a systematic review and meta-analysis. J Am Acad Dermatol. 2017;76(6):1068–1076.e1069. doi:10.1016/j.jaad.2016.12.028
- Johnson B, Leibowitz S, Chavez A, Herbert SE. Risk Versus resiliency: addressing depression in lesbian, gay, bisexual, and transgender youth. Child Adolesc Psychiatr Clin N Am. 2019;28(3):509–521. doi:10.1016/j.chc.2019.02.016
