Abstract
Adolescence and young adulthood are often turbulent periods in a person’s life. There are high rates of accidental deaths, suicide, mental health concerns, substance use, and sexual experimentation. Health care professionals need to conduct holistic assessments of clients in these developmental life stages to identify psychosocial risks and provide targeted early intervention and implement prevention strategies. The most useful psychosocial assessments for most health care professionals are those that can provide a complete picture of the young person’s life and circumstances. This article identifies psychosocial assessment instruments that can be used as an initial assessment and engagement tool with the general population of young people presenting for health care. We review the psychometric properties of each of the instruments, determining what type of instrument is most acceptable to young people, whether any can increase disclosure and improve engagement between young people and health professionals, and whether they have predictive utility. The search strategy complied with the relevant sections of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. A total of 89 published articles were identified, covering 31 different assessment instruments. Results indicated that those that were self-administered were most acceptable to young people, although it is unclear whether pen-and-paper or computer formats were preferred. Most psychosocial assessments can improve rates of disclosure and enhance engagement between young people and health professionals; however, worryingly, we found evidence that clinicians did not always respond to some of the most serious identified risks. Only for one instrument was there any mention of predictive utility. Future research should employ longitudinal approaches to determine the predictive utility of psychosocial assessments and focus on whether the use of new technologies can improve rates of disclosure.
Introduction
Adolescence and young adulthood are significant periods of social, emotional, physical and neurophysiologic development.Citation1 During this time, young people push barriers, take on new roles and responsibilities, and increasingly become more reliant on their peers and less so on their parents and caregivers. While most young people successfully navigate these challenges, there are many who require additional support, with rates of accidental deaths, drinking and driving, suicide, mental health concerns, substance use, and sexually transmitted diseases peaking during this time.Citation2–Citation4 Early identification of these behavioral risks and emotional problems enables health professionals to provide appropriate support and implement preventative strategies, which is likely to lead to significant reductions in rates of morbidity and mortality.Citation5
Although “adolescence” and “young people” continue to be defined in various ways, recently, there has been some consensus, with these terms together understood to concern the ages from 12 to 25 years, as this covers the complete transition from childhood to adulthood.Citation6 Neurophysiologic evidence shows that adolescence is not just a period of transition within the social sphere, but also a period of transition for the brain in which there are distinctly different processes and structures.Citation7,Citation8 For example, research suggests that the adolescent brain may be less responsive to stimuli relative to adults or children, leading adolescents to take greater risks or seek novelty stimuli.Citation1 Historically, services have been split into child and adolescent mental health services for those under 18 years of age, and adult mental health services for those over 18 years. However, these services often differ in their views on diagnosis, etiology, and treatment, which makes the transition between the two particularly difficult.Citation9 This dichotomy of service provision requires young people to not only navigate their developmental transition into adulthood but also navigate a new health care system at the age of 18 years.Citation10,Citation11 Over the past decade, a new model of service delivery that suggests youth specific services should be provided to those aged 12–25 years has been gaining support.Citation12 The aim of these services is to provide continuous and developmentally appropriate support to the young person until they reach adulthood.
When a young person presents for physical or mental health care, it is highly likely that there will be a number of psychosocial issues that should be addressed. While the young person may initially disclose a certain issue, health care professionals should take the opportunity to conduct a holistic assessment of the young person, as this can lead to early intervention or implementation of prevention strategies for issues or risks that may otherwise go unaddressed.Citation13,Citation14 Further, a complete psychosocial assessment provides health professionals with a holistic picture of the young person, which is needed for an individualized treatment program that is likely to lead to better long-term prognosis.Citation15 However, getting young people to speak about risky behaviors or difficult issues is a challenge and is likely to be contingent on trust, confidentiality, and direct questioning.Citation16
Many psychosocial assessment instruments have been developed that provide health care professionals in multidisciplinary contexts with a framework with which to use to discuss with young people their psychological, social, behavioral, and environmental concerns. The effectiveness of these instruments is reliant on their acceptability to young people, their ability to create a space for disclosure and engagement between the young person and health professional, and their predictive utility in identifying possible future risks and concerns.
The current systematic review aimed to identify psychosocial assessment instruments available for use with the general population of young people by clinicians working in primary care and multidisciplinary contexts. The psychosocial instruments of interest were those that could be used during initial contact with the young person and asked about multiple domains of their life in order to improve engagement and understanding between the young person and health professional. The domains included psychological and emotional as well as behavioral, environmental, and social aspects. Specifically, we aimed to identify the characteristics of each of the instruments, including the age it was suitable for, the mode of administration and administration time frame, its psychometric properties, and the context/location in which the instrument had been tested. We were also interested in determining whether there were common domains covered by the instruments. Further, we examined whether young people were willing to complete the assessments and whether this was dependent on the mode of instrument administration, whether the instruments could increase disclosure and engagement between the young person and health care professional, and whether the instrument could predict any future risky behaviors or emotional problems. It was particularly important to identify instruments that could be used across the 12–25 year age range to recognize the emerging service model of youth-specific mental health care.
Methods
A systematic review of the literature was undertaken by reviewing all published studies that describe the use of a psychosocial assessment for young people that could be used in an initial assessment context to improve engagement between the young person and health professional, and provide a complete picture of the young person and their environment. Acceptable articles included all types of trials, systematic reviews, individual instrument reviews, and critical discussions. A “psychosocial assessment” was defined as an assessment or instrument that provides information about multiple psychosocial areas of a young person’s life. The assessment could be self-administered, in the form of a structured or semi-structured interview, or a combination of these. To be considered “psychosocial” the instrument had to cover both psychological and social/environmental aspects. “Young people” were defined as those aged 12–25 years old.
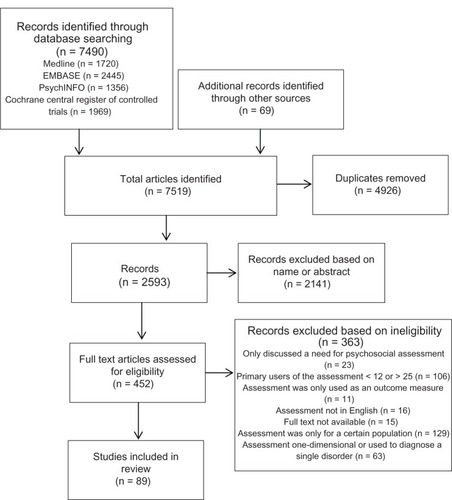
The search methodology and reported findings comply with the relevant sections of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.Citation17 Initially, a broad search strategy was implemented covering all studies published in English between January 1, 1980 and July 12, 2012 from MEDLINE®, Embase, PsycINFO® and the Cochrane Central Register of Controlled Trials databases. The search terms used were: “psychosocial” OR “multidimensional” AND “assess*” OR “measure*” OR “screen” AND “adolescen*” OR “young*” OR “child” OR “tool*”; and “therap*” AND “Engag*.” The Mental Measurements Yearbook database was searched using the terms “psychosocial” OR “multidimensional.” Additionally, all eleven volumes of Test Critiques and the reference books Measures for Clinical Practice,Citation18 Assessment in Psychiatric and Mental Health Nursing,Citation19 Oxford Handbook of Paediatrics,Citation20 Behavioural, Social, and Emotional Assessment of Children and Adolescents,Citation21 Major Psychological Assessment Instruments,Citation22 and The Handbook of Psychological TestingCitation23 were searched by hand to identify any other psychosocial instruments that met the study inclusion criteria. Further studies were identified through searching by hand the references of relevant studies and reviews.
Following the database search, abstracts and titles were scanned and irrelevant studies were removed; the remaining full-text articles were assessed for eligibility by both authors. The final eligibility criteria were that the article evaluated or discussed a psychosocial assessment that was: in English, for young people aged 12–25 years, for use with the general population, did not require proxy input from any other persons, and provided information about multiple psychosocial domains in the young person’s life. Instruments that asked about multiple domains but only provided a single overall score or outcome measure were excluded, as were those primarily used to diagnose a specific mental disorder. Further, instruments stated as only being for those aged 18 years and older were excluded to keep the review manageable; however, it was recognized that this would exclude a number of viable instruments for those in the 18–25-year-old age group.
Although the search was extensive, authors were not contacted to ascertain further information or to obtain unpublished work. A further systematic review for every published article on the identified instruments was not conducted, as the aim was to identify all psychosocial instruments that met the inclusion criteria; it was not to identify every published article on each of the identified instruments. shows the PRISMA flow diagram for study inclusion.
Results
Search results
The search strategy identified 89 published articles covering 31 different psychosocial instruments. Of the 89 articles, 44 were research trials, 40 were individual instrument reviews, and five were systematic reviews. The median number of identified references for each instrument was two, with the most referenced instrument being the HEADSSS assessment with nine identified articles. The key characteristics of the 31 identified instruments are summarized in .
Table 1 Instrument summary
Instrument summary
Acceptable age range
The Structured Pediatric Psychosocial Interview (SPPI) had the lowest recommended minimum age of use, at five years. While the Personal Problems Checklist for Adolescents (PPCA) had an age range of 13–17 years, there were also alternate forms of the instrument for those aged 5–12 years and 18+ years. Taking into account the three versions of the PPCA, this instrument covered the widest possible range of ages. The mean minimum age in reported studies was 11.42 years and the mean maximum age was 20 years.
Administration time
Of all the assessments, the minimum suggested administration time was three minutes, which was for HEADSSS. The maximum suggested administration time was 90 minutes, which was for both HEADSSS and the Life Stressors and Social Resources Inventory-Youth Form (LISRES-Y). HEADSSS had the largest suggested possible administration time range of 87 minutes. The mean administration time for all assessments was 27.53 minutes.
Method and mode of administration
While the aim of each of the instruments identified is to help promote engagement between the young person and health professional through discussions of the young person’s answers/results, many instruments were designed to be initially self-completed either using pen-and-paper or computer-assisted administration formats. Twenty-three instruments were identified as being purely self-administered, two were delivered purely in a structured/semi-structured interview, and six instruments could be delivered via either self-administration or interview. In terms of the mode of administration, at the time of research, 17 instruments were only available in a paper format for completion using a pen, one was only available in a computer/online format; two were only available in a face-to-face interview format; five were available in both paper and online/computer versions; and six were available in all three formats: paper, online/computer, and face-to-face interview.
Validity and reliability
The construct, content, and criterion validity and the internal consistency and test–retest reliability were evaluated for each instrument and are summarized in . Evidence of validity and reliability coefficients was obtained solely from the articles identified within the search strategy. If there was no mention of any type of validity or reliability, evidence was noted as unclear. Evidence of construct validity was found for twelve instruments, content validity was present for 26 instruments, and criterion validity evident for 14 instruments. The Life Experiences Questionnaire (LEQ), Personal Inventory, Brief Life History Inventory (BLHI), and Psychological/Social History Report made no mention of any type of validity. Internal reliability coefficients were available for 19 instruments and test–retest reliabilities available for 12 instruments. Only KIDSCREEN, Behavior Assessment System for Children, Second Edition (BASC-2), Personality Inventory for Youth (PIY), Self-Description Questionnaire 2 (SDQ-2), and the Strengths and Difficulties Questionnaire (SDQ) had evidence for all three types of validity as well as internal and test–retest reliability.
Table 2 Instrument psychometric properties.
Location/context
Half the instruments had been tested in multiple contexts. Eight instruments had only been tested in the initial instrument development or to obtain norms; these occurred in either a school or community context (four in each). Two instruments had only been tested in a general practice setting, one in an emergency department/hospital setting and one in a youth-specific mental health setting.
Domains
To identify the domains covered by each instrument and determine whether common domains existed, the individual domains of each instrument were categorized under one of 43 possible common domain headings. In some cases, domains covered within the instruments could fit more than one common domain category; for example, the HEADSSS assessment includes suicide and depression under the one domain name; therefore, this was included under both the anxiety/depression/mood and suicide domains during categorization. This was the case for a number of instruments and different domains. In other cases, instrument domains were more highly specified than the common domain name may indicate. For example, the Multidimensional Adolescent Assessment Scale (MAAS) included the separate domains of “mother problems,” “father problems,” and “family problems” – these domains were combined and categorized under the common domain name of “family.” The Instrument for Monitoring Adolescent Health Issues and the Psychological/Social History Report separated the domains for exercise and diet, and these were combined and categorized under the common domain name of “eating/body issues.” The Adolescent Health Review (AHR), Guidelines for Adolescent Preventive Services (GAPS), Instrument for Monitoring Adolescent Health Issues, MAAS, and Hilson Adolescent Profile (HAP) all contain separate domains for alcohol, cigarette use, and drug use; these were combined under the common domain name “substance use/abuse.” Finally, the AHR, GAPS, KIDSCREEN, MAAS, BLHI, BASC-2, HAP, LISRES-Y, PPCA, Psychological/Social History Report, Quickview Social History, SDQ-2, and Youth Risk and Resilience Inventory (YRRI) all ask specifically about education and omit work/employment; these were included within the “education/work” common domain category.
The number of domains covered by each instrument ranged from three in the YRRI, to 16 in the HAP. The average number of domains per instrument was nine. The most commonly included category was “social relations,” covered by 21 different instruments. This category included both social and intimate relationships and support. The domains covered by two or more instruments (and the number of instruments that covered them), in order were: social relations (21), education and work (19), mental health (18), physical health (17), emotional distress (15), harm or violence to self or others (12), sexuality (12), family relations (11), substance use/abuse (11), eating/body issues (11), rule-breaking behavior/conduct disorder or legal history (10), home environment (10), anxiety/depression/mood (8), psychosis/mania (8), hyperactivity (8), suicide (6), leisure activities/hobbies (6), self-esteem (5), material well-being/financial status (5), concentration/productivity (5), emotional control (5), autonomy (4), stress (4), somatization (4), family medical/mental health history (4), general risk-taking behavior (4), place in community (3), personality (2), spirituality/religion (2), developmental history (2), and presenting problem (2).
Article results
Acceptability to young people
To determine whether the instruments were acceptable to young people, completion rates and rates of disclosure were investigated. The systematic review of 105 studies reporting health risk behaviors by Brener et alCitation24 found that self-administered questionnaires identified higher rates of risk behaviors than interviewer-administered questionnaires. Patients in the study by Silber and RosenthalCitation25 also indicated that it was initially easier to state their problems on paper using the Mile Square Questionnaire (MSQ) than to state them verbally to the health care provider.
Findings of differences in disclosure rates between online and paper versions of various instruments were mixed. In a pilot study of a computerized version of the SDQ, Truman et alCitation26 found no differences in response rates between the paper and online versions; however, there was significantly better user satisfaction with the online version. The systematic review by Silber and RosenthalCitation25 found that computer-assisted self-administration questionnaires resulted in higher rates of reporting illegal drug use, suicidal behavior, and high-frequency sexual behaviors than paper versions. In contrast, Beebe et alCitation27 found that risk behaviors were generally more likely to be reported using a paper version of the AHR than using an online version. However, this difference was only significant within the domains of alcohol quantity and substance use disorder. Higher scores were also found for a paper version of the Child Health Questionnaire Child Form (CHQ-CF) compared with an Internet version.Citation28 These differences were statistically significant for the domains of general behavior, role functioning – physical, mental health and family activities. However, less data were missing when the Internet version of the CHQ-CF was utilized.
Disclosure and engagement
Disclosure and engagement were evaluated by identifying results focusing on each instrument’s ability to create a space for discussion of relevant domains between the health professional and young person. The introduction of a psychosocial assessment instrument was found to improve engagement between the young person and health professional, thereby improving the clinician’s understanding of the young users and their environment, in the studies by Beebe et al,Citation27 Elliott et al,Citation29 Epner et al,Citation30 Klein et al,Citation31 Parker et al,Citation32 Peake et al,Citation33 Silber and Rosenthal,Citation25 Van Amstel et al,Citation34 and Yi et al.Citation35 Specifically, clinicians in the study by Elliott et al,Citation29 stated that Adquest was able to: identify issues important to the adolescents, identify which domains the young person was ready to discuss right away – and which needed to be returned to at a later time, signal to the young person that it was okay to disclose information about relevant domains, and organize the young person’s thoughts and issues ahead of time by providing them with a format for self-reflection. Further, clinicians felt that the section titles and introductions were able to indicate the organization’s philosophy on domains, provide a “common language” for clinical assessment and discussion, and give permission for them to ask the young person difficult questions. Similar responses were provided by physicians using the MSQ, who stated that the instrument helped “break the ice”; provided a legitimate reason to ask young people about other issues that might be of concern to them; and indicated to young people that doctors were available to them to talk about emotional and psychosocial concerns, not just their presenting physical need.Citation25
Unfortunately, four studies found that clinicians ignored certain domains that were identified as issues for the young person. In the evaluation of GAPS, it was found that general practitioners (GPs) discussed all the identified risk behaviors with the young person in only 23% of cases.Citation30 In 62% of cases, the GP discussed half or more of the identified risk behaviors, and in 15% of cases they discussed fewer than half of the identified risks. Epner et alCitation30 found that GPs were least likely to respond to behaviors regarding weapons and violence or depression and abuse. A follow-up with young participants in the study by Klein et alCitation31 found that adolescents reported receiving less counseling around their identified risks than the clinicians reported they had provided. Van Amstel et alCitation34 found that the inclusion of a HEADSSS stamp on emergency department patient records significantly increased documentation of the education, alcohol, and smoking domains, but that the domains of home environment, substance use/abuse, and sexual activity continued to be ignored by physicians. A retrospective review of 100 medical records and the HEADSSS assessment by Yeo et alCitation36 found only seven records showed that a complete screen had been conducted.
Predictive utility
Only the article by Jacob,Citation37 which reviews the Offer Self-Image Questionnaire, Revised (OSIQ), was found to mention an instrument’s ability to predict future risks or psychosocial issues. The author refers to an earlier longitudinal study conducted by Offer and Offer in 1975, in which the OSIQ was shown to be able to identify “normal”’ adolescent males who were likely to develop minimal psychological problems in the future. No other articles presented information on the predictive utility of the psychosocial assessment instruments.
Discussion
This systematic review has highlighted the many psychosocial assessment instruments that are available to improve engagement between health care professionals and young people who present for health care within a generalist primary care or multidisciplinary context. Most of the instruments were appropriate for use with young people aged 12–20 years. The administration times averaged about half an hour, which is appropriate for many clinical visits, although may be too long in time-restricted general practices.Citation38 The majority of instruments were designed to be initially self-administered using a pen on a paper questionnaire and then to have the answers discussed between the young person and health care professional. This format is likely to suit many contexts, as young people can complete the instrument prior to the appointment, leaving more time to discuss the relevant issues within the session. The contexts and locations in which the instruments had been used varied widely, although it was encouraging to see that half had been used in multiple environments, as it has been recommended that in the future multidisciplinary teams provide health and mental health care.Citation39 In terms of psychometric properties, only about a third had documented validity and reliability. The domains covered by the instruments were varied, although the most common were social relations, education/work, mental health, physical health, emotional distress, harm or violence to self or others, and sexuality – all of which are immediately relevant to the majority of young people.
In terms of acceptability to young people, there is clear evidence for the use of an instrument that is initially self-administered over those delivered via an interview format. This is probably why over 93% of the identified instruments used this method of administration. In terms of whether self-administration should occur by pen-and-paper or computer-assisted formats, the evidence is varied. However, it should be noted that the articles examining the relationship between form of administration and disclosure rates are at least 5–6 years old – technology use has increased dramatically over this period, and young people are likely to be much more familiar and comfortable with computer-assisted formats. Thus, future studies should readdress this issue and extend their investigation into different computer-assisted formats, such as completing the form on a smartphone or tablet device, which are likely to be more private than completing the form on a large desktop computer as was used in the studies identified by this review.
This review provides some evidence that the use of a psychosocial instrument can improve engagement between health professionals and young people, mostly by giving health professionals a legitimate reason to ask difficult questions that otherwise may not have been raised. Unfortunately, much of the support for using psychosocial assessment instruments is derived from the anecdotal views of clinicians, whose jobs they make easier, not from the young people who have to respond to them or from empirical evidence. Additionally, it is very concerning that in four studies, all of which use different instruments, clinicians failed to discuss with the young person some of the most serious risks they had identified. Most concerning is that these studies took place in general practices and community health centers. While it is well recognized that GPs are often time poor,Citation38 it is also known that for young people, a GP is often the first professional they turn to for help.Citation40 Physicians need to respond to all the risks identified by the young person in a confidential and caring manner, as a negative past experience, such as telling a professional about an issue and not receiving an appropriate response, will significantly reduce the likelihood of a young person seeking future help.Citation41 Therefore, if a health professional decides to use an assessment instrument, they must follow-up on any risks that it identifies, not just those they have time for or those they feel comfortable addressing.
Interestingly, there is a significant gap in the literature regarding the ability of psychosocial assessment instruments to predict future psychological disorders or risky behaviors, with only the study by JacobCitation37 mentioning the predictive ability of an instrument – the OSIQ. While it is likely that this evidence is lacking because none of the studies were longitudinal, it is also possible that health professionals are simply not providing long-term follow-up. Having an instrument that clinicians can use to identify possible future issues will reduce rates of morbidity and mortality only if preventative measures are implemented and follow-up is undertaken. Future studies should be prospective to determine whether the instrument has predictive ability and whether health professionals provide the necessary preventive supports.
Overall, the most appropriate instrument in terms of acceptability, engagement, and disclosure is one that is self-administered and then appropriately followed-up by the clinician. It should ask about domains that are relevant to all young people and prioritize those that are immediately relevant, such as social interaction, education and/or employment, mental health and emotional distress, harm to self or others, and sexuality. The currently available instruments that address these domains, are available in a self-administered format, and have been shown to increase engagement and disclosure include the AHR, Adquest, and GAPS. The AHR is the only instrument of these three that has also been tested in multiple contexts.
Limitations
While the thorough search strategy employed by this review identified a large number of psychosocial assessment instruments and evaluative papers for each, a systematic search of every published article for each of the instruments was not conducted. Therefore, it is possible that there is published evidence related to the psychometric properties of some of the instruments that has not been reported.
Conclusion
Psychosocial assessment instruments are essential tools for health care professionals working with young people because they improve detection of risks and engagement by helping clinicians to broach difficult issues. However, if a health professional decides to use a psychosocial instrument and the young person indicates a risky behavior or emotional concern, it is imperative that the health professional makes time to deal with it appropriately.
Self-administered instruments are most acceptable to young people, although it has not been determined whether pen-and-paper or computer-assisted formats are preferred. Only one instrument has been shown to be useful in predicting any type of future risk.
Which tool is most appropriate for a clinician will depend on the domains they are most interested in, their preferred mode of delivery or available resources, available time frame, and whether they work in a multidisciplinary environment. The only tool which is currently available in a self-administered format, covers all domains relevant to most young people, has been tested in multiple contexts, and can be completed in a short period, is the AHR.
Future research should focus on conducting longitudinal studies to determine the predictive utility of these instruments. It would also be beneficial to determine whether there is any empirical evidence to support the anecdotal statements from clinicians concerning levels of engagement and whether young people themselves feel the instruments help them disclose and engage. Additionally, research should be conducted to determine the suitability for instruments such as the GAPS in multidisciplinary contexts, and to determine whether any of the instruments delivered currently by interview, such as the HEADSSS, could be transformed into a self-administered format to increase its acceptability to young people. Such research has the potential to provide clinicians with a wider choice of appropriate instruments to suit their individual and organizational needs.
Disclosure
The authors report no conflicts of interest in this work.
References
- SpearLPThe adolescent brain and age-related behavioral manifestationsNeuroscience and Biobehavioral Reviews200024441746310817843
- MininoAMMortality among teenagers aged 12–19 years: United States, 1999–2006Hyattsville, MDUS Department of Health and Human Services: Centers for Disease Control and Prevention, National Center for Health Statistics2010 http://www.cdc.gov/nchs/data/databriefs/db37.pdf
- MulyeTPParkMJNelsonCDAdamsSHIrwinCEJrBrindisCDTrends in adolescent and young adult health in the United StatesJournal of Adolescent Health200945182419541245
- MerikangasKRHeJPBursteinMLifetime prevalence of mental disorders in US. adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A)Journal of the American Academy of Child and Adolescent Psychiatry2010491098098920855043
- GoldenringJMCohenEGetting into adolescent headsComtemporary Pediatrics19887590
- McGorryPParkerAPurcellRYouth mental health servicesInPsych200682006 http://www.psychology.org.au/publications/inpsych/youth_mental_health/
- GieddJNBlumenthalJJeffriesNOBrain development during childhood and adolescence: a longitudinal MRI studyNature Neuroscience1999210861
- ColrainIMBakerFCChanges in sleep as a function of adolescent developmentNeuropsychology Review201121152121225346
- SinghSPEvansNSirelingLStuartHMind the gap: The interface between child and adult mental health servicesPsychiatric Bulletin2005298292294
- SinghSPTransition of care from child to adult mental health services: the great divideCurrent Opinion in Psychiatry200922438639019417667
- McGorryPPurcellRYouth mental health reform and early intervention: Encouraging early signsEarly Intervention in Psychiatry20093316116222640378
- McGorryPReforming youth mental healthAustralian Family Physician200635531431416680210
- AHRQThe guide to clinical preventive services 2010–2011: Recomendations of the US preventive services task forceUSADepartment of Health and Human Services2011
- RACPRoutine adolescent psychosocial health assessment–Position statementAuthor2008
- DrakeREMueserKTBrunetteMFMcHugoGJA review of treatments for people with severe mental illnesses and co-occuring substance use disordersPsychiatric Rehabilitation JournalSpring2004200427436037415222148
- BoothMLBernardDQuineSAccess to health care among Australian adolescents young people’s perspectives and their sociodemographic distributionJournal of Adolescent Health20043419710314706412
- MoherDLiberatiATetzlaffJAltmanDGThePGPreferred reporting items for systematic reviews and meta-analyses: The PRISMA statementPLoS Med200967e100009719621072
- CorcoranKFischerJMeasures for Clinical Practice: A Sourcebook12nd edNew YorkThe Free Press1987
- BarkerPJAssessment in psychiatric and mental health nursing: In serch of the whole personCheltenham, UKStanley Thornes Publishers1997
- TaskerRCMcClureRJAceriniCLOxford handbook of paediatricsOxfordOxford University Press2008
- MerrellKWBehavioural, soial, and emotional assessment of children and adolescents3rd edNew YorkLawrence Erlbaum Associates2008
- NewmarkCSMajor psychological assessment instruments2nd edBostonAllyn and Bacon1996
- KlinePThe handbook of psychological testingLondonRoutledge1993
- BrenerNDBillyJOGGradyWRAssessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literatureJournal of Adolescent Health200333643645714642706
- SilberTJRosenthalJLUsefulness of a review of systems questionnaire in the assessment of the hospitalized adolescentJournal of Adolescent Health Care19867149523944002
- TrumanJRobinsonKEvansALThe Strengths and Difficulties Questionnaire: A pilot study of a new computer version of the self-report scaleEuropean Child and Adolescent Psychiatry200312191412601559
- BeebeTJHarrisonPAEunkyungPMcRae JrJAEvansJThe effects of data collection mode and disclosure on adolescent reporting of health behaviorSocial Science Computer ReviewWinter20062006244476488
- RaatHMangunkusumoRLandgrafJKloekGBrugJFeasibility, reliability, and validity of adolescent health status measurement by the Child Health Questionnaire Child Form (CHQ-CF): internet administration compared with the standard paper versionQuality of Life Research200716467568517286197
- ElliottJNembhardMGiannoneVSurkoMMedeirosDPeakeKClinical Uses of an Adolescent Intake Questionnaire: Adquest as a Bridge to EngagementSocial Work in Mental Health200431–283102
- EpnerJLevenbergPBSchoenyMEPrimary care providers’ responsiveness to health-risk behaviors reported by adolescent patientsArchives Of Pediatrics and Adolescent Medicine199815287747809701137
- KleinJDAllanMJElsterABImproving adolescent preventive care in community health centersPediatrics2001107231811158465
- ParkerAHetrickSPurcellRPsychosocial assessment of young people: Refining and evaluating a youth friendly assessment interviewAustralian Family Physician201039858558820877754
- PeakeKEpsteinIMirabitoDSurkoMDevelopment and utilization of a practice-based, adolescent intake questionnaire (Adquest): Surveying which risks, worries, and concerns urban youth want to talk aboutSocial Work in Mental Health200431–25582
- Van AmstelLLLafleurDLBlakeKRaising our HEADSS: adolescent psychosocial documentation in the emergency departmentAcademic Emergency Medicine: Official Journal Of The Society For Academic Emergency Medicine200411664865515175203
- YiCHMartynKSalernoJDarling-FisherCSDevelopment and clinical use of rapid assessment for adolescent preventive services (RAAPS) questionnaire in school-based health centers. Journal of Pediatric Healthcare2009 Jan–Feb200923129
- YeoMSMBondLMSawyerSMHealth risk screening in adolescents: room for improvement in a tertiary inpatient settingThe Medical Journal Of Australia2005183842742916225451
- JacobSE‘Offer self-Image questionnaire, revised’: Test reviewJournal of Psychoeducational Assessment1997154373379
- KonradTRLinkCLShackeltonRJIt’s about time: physicians’ perceptions of time constraints in primary care medical practice in three national healthcare systemsMedical Care20104829510020057331
- VreelandBBridging the gap between mental and physical health: A multidisciplinary approachJournal of Clinical Psychiatry200768Suppl4263317539697
- ChownPKangMSanciLNewnhamVBennettDLAdolescent health: Enhancing the skills of general practitioners in caring for young people from culturally diverse backgrounds, GP resource kitSydneyNSW Centre for the Advancement of Adolescent Health and Transcultural Mental Health Centre2008
- RickwoodDDeaneFPWilsonCJCiarrochiJYoung people’s help-seeking for mental health problemsAustralian e-Journal for the Advancement of Mental Health200543 Supplement. www.auseinet.com/journal/vol4iss3suppl/rickwood.pdf
- HarrisonPABeebeTJParkEThe adolescent health review: A brief, multidimensional screening instrumentThe Journal Of Adolescent Health: Official Publication Of The Society For Adolescent Medicine200129213113911472872
- HarrisonPABeebeTJParkERanconeJThe adolescent health review: Test of a computerized screening tool in school-based clinicsJournal of School Health2003731152012621719
- KonoldTRReview of the test Adolescent Psychopathology ScaleThe fourteenth mental measurements yearbook2001 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=JDCLFPKIDEDDFPCNNCPKECFBLNAJAA00&Complete+Reference=S.sh.14%7c6%7c1
- PierselWCReview of the test Adolescent Psychopathology ScaleThe fourteenth mental measurements yearbook2001 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=JDCLFPKIDEDDFPCNNCPKECFBLNAJAA00&Complete+Reference=S.sh.14%7c6%7c1
- GiannoneVMedeirosDElliottJPerezCCarlsonEEpsteinIAdolescents’ self-reported risk factors and desire to talk about family and friends: implications for practice and researchSocial Work in Mental Health200431/2191210
- GladmanMLancasterSA review of the behaviour assessment system for childrenSchool Psychology International2003243276
- MerendaPFBASC: Behavior assessment system for childrenMeasurement and Evaluation in Counseling and Development1996284229232
- TanCSTest review behavior assessment system for children (2nd ed)Assessment for Effective Intervention2007322121124
- MatteiMHKillianGADorfmanWBrief Life History InventoryKeyserDJSweetlandRCTest critiques10Austin, TXPRO-ED, Inc1994102109
- AchenbachTMRuffleTMThe child behavior checklist and related forms for assessing behavioral/emotional problems and competenciesPediatrics in Review812000200021826527110922023
- HoughtonFGleesonMKelleherKThe use of the Child Health Questionnaire (CHQ-CF87) in a rural Irish contextThe Irish Journal of Psychology2003241–23545
- LandgrafJMAbetzLNFunctional status and well-being of children representing three cultural groups: initial self-reports using the CHQ-CF87Psychology and Health1997126839854
- WatersESalmonLAWakeMWrightMHeskethKDThe health and well-being of adolescents: A school-based population study of the self-report Child Health QuestionnaireJournal of Adolescent Health200129214014911472873
- WatersEWrightMWakeMLandgrafJSalmonLMeasuring the health and well-being of children and adolescents: a preliminary comparative evaluation of the Child Health Questionnaire in Australia… including commentary by Stein REKAmbulatory Child Health199952131141
- CumminsRAMccabeMPRomeoYGulloneEValidity Studies the Comprehensive Quality of Life Scale (Comqol): Instrument Development and Psychometric Evaluation on College Staff and StudentsEducational and Psychological MeasurementSummer19941994542372382
- GulloneECumminsRAThe Comprehensive Quality of Life Scale: A psychometric evaluation with an adolescent sampleBehaviour Change1999162127139
- GadomskiABennettSYoungMWissowLSGuidelines for adolescent preventive services: the GAPS in practiceArchives Of Pediatrics and Adolescent Medicine2003157542643212742877
- Carr-GreggMManochaRBullying–effects, prevalence and strategies for detectionAustralian Family Physician20114039810221597508
- CohenEMackenzieRGYatesGLHEADSS, a psychosocial risk assessment instrument: Implications for designing effective intervention programs for runaway youthJournal of Adolescent Health19911275395441772892
- GoldenringJMRosenDSGetting into adolescent heads: an essential updatePatient Care for the Nurse Practitioner200428p
- JonesSMertynEAlhucemaPMonaglePNewallFHEEADSSS assessment for adolescents requiring anticoagulation therapyArchives Of Disease In Childhood201297543043322147745
- SanciLGrabschBChondrosPThe prevention access and risk taking in young people (PARTY) project protocol: a cluster randomised controlled trial of health risk screening and motivational interviewing for young people presenting to general practice and motivational interviewing for young people presenting to general practiceBMC Public Health201212140022672481
- HaynesSDReview of the test Health and Daily Living Form, Second EditionThe fifteenth mental measurements yearbook2003 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=EHFIFPLHFADDFPNPNCPKECGCIEBMAA00&Complete+Reference=S.sh.14%7c1%7c1
- KageeAReview of the test Health and Daily Living Form, Second EditionThe fifteenth mental measurements yearbook2003 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=EHFIFPLHFADDFPNPNCPKECGCIEBMAA00&Complete+Reference=S.sh.14%7c1%7c1
- CalkinsDLWalkerCEHilson adolescent profileKeyserDJSweetlandRCTest critiques9Austin, TXPRO-ED, Inc1992261266
- HessAReview of the test Hilson Adolescent ProfileThe eleventh mental measurements yearbook1992 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=EHFIFPLHFADDFPNPNCPKECGCIEBMAA00&Complete+Reference=S.sh.31%7c1%7c1
- StantonWRWillisMBalandaKPDevelopment of an instrument for monitoring adolescent health issuesHealth Education Research200015218119010751377
- SteinerHPavelskiRPittsTMcQuiveyRThe Juvenile Wellness and Health Survey (JWHS-76): A School Based Screening Instrument for General and Mental Health in High School StudentsChild Psychiatry and Human DevelopmentWinter199819982921411559816733
- RajmilLAlonsoJBerraSUse of a children questionnaire of health-related quality of life (KIDSCREEN) as a measure of needs for health care servicesJournal of Adolescent Health200638551151816635761
- Ravens-SiebererUGoschARajmilLThe KIDSCREEN-52 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 european countriesValue in Health (Wiley-Blackwell)2008114645658
- NewcombMDHubaGJBentlerPMA multidimensional assessment of stressful life events among adolescents: Derivation and correlatesJournal of Health and Social Behavior1981224400415
- CrehanKDReview of the test Life Stressors and Social Resources Inventory-Youth FormThe thirteenth mental measurements yearbook1992 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=EHFIFPLHFADDFPNPNCPKECGCIEBMAA00&Complete+Reference=S.sh.33%7c1%7c1
- DanielsDMoosRHAssessing life stressors and social resources among adolescents: Applications to depressed youthJournal of Adolescent Research199053268289
- OosterhofAReview of the test Life Stressors and Social Resources Inventory-Youth FormThe thirteenth mental measurements yearbook1992 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=EHFIFPLHFADDFPNPNCPKECGCIEBMAA00&Complete+Reference=S.sh.33%7c1%7c1
- MathiesenSGCashSJHudsonWWThe multidimensional adolescent assessment scale: A validation studyResearch on Social Work Practice2002121928
- AllenSJReview of the test Offer Self-Image Questionnaire, RevisedThe twelfth mental measurements yearbook1995 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=HCNGFPKKOFDDEPCLNCPKAHFBGDOEAA00&Complete+Reference=S.sh.14%7c1%7c1
- FurlongMJKarnoMReview of the test Offer Self-Image Questionnaire, RevisedThe twelfth mental measurements yearbook1995 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=HCNGFPKKOFDDEPCLNCPKAHFBGDOEAA00&Complete+Reference=S.sh.14%7c1%7c1
- GrossmanFMReview of the test a Personal InventoryThe ninth mental measurements yearbook1985 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=HBNPFPEIDLDDFPKGNCPKNHOBCBFFAA00&Complete+Reference=S.sh.14%7c1%7c1
- IretonHA personal inventoryJournal of Family Practice19801111371407411034
- RandallJReview of the test A Personal InventoryThe ninth mental measurements yearbook1985 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=HBNPFPEIDLDDFPKGNCPKNHOBCBFFAA00&Complete+Reference=S.sh.14%7c1%7c1
- MartensBReview of the test Personal Problems Checklist for AdolescentsThe tenth mental measurements yearbook1989 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=ACKHFPDKOEDDEPEKNCPKIELBKPIGAA00&Complete+Reference=S.sh.31%7c1%7c1
- McCarthyPPersonal problems checklist for adolescentsKeyserDJSweetlandRCTest critiques10Austin, TXPRO-ED, Inc1994531536
- SantmireTEReview of the test Personal Problems Checklist for AdolescentsThe tenth mental measurements yearbook1989 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=ACKHFPDKOEDDEPEKNCPKIELBKPIGAA00&Complete+Reference=S.sh.31%7c1%7c1
- LacharDGruberCPDevelopment of the personality inventory for youth: A self-report companion to the personality inventory for childrenJournal of Personality Assessment199361181988377104
- MarchantGJRidenourAReview of the test Personality Inventory for YouthThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=ACKHFPDKOEDDEPEKNCPKIELBKPIGAA00&Complete+Reference=S.sh.14%7c5%7c1
- WrobelTALacharDWrobelNHMorganSTGruberCPNeherJAPerformance of the personality inventory for youth validity scalesAssessment19996436737910539983
- MatteiMHKillianMDorfmanWPsychological/social history reportKeyserDJSweetlandRCTest critiques10Austin, TXPRO-ED, Inc1994553561
- BradfordRRutherfordDLJohnAQuality of life in young people: ratings and factor structure of the Quality of Life Profile-Adolescent VersionJournal of Adolescence200225326127412128037
- RaphaelDRukholmEBrownIHill-BaileyPThe quality of life profile—adolescent version: Background, description, and initial validationJournal of Adolescent Health19961953663758934298
- DixonDReview of the test Quickview Social HistoryThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=ACKHFPDKOEDDEPEKNCPKIELBKPIGAA00&Complete+Reference=S.sh.35%7c1%7c1
- StarrERReview of the test Quickview Social HistoryThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=ACKHFPDKOEDDEPEKNCPKIELBKPIGAA00&Complete+Reference=S.sh.35%7c1%7c1
- SalernoJMarshallVDPickenEBValidity and reliability of the rapid assessment for adolescent preventive services adolescent health risk assessmentJournal of Adolescent Health201250659559922626486
- AtlasJReview of the test Self-Description Questionnaire-I, II, IIIThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=OOHBFPJJOLDDEPHCNCPKIBLBCGHLAA00&Complete+Reference=S.sh.30%7c5%7c1
- BoyleGJSelf-description questionaire 2KeyserDJSweetlandRCTest critiques10Austin, TXPRO-ED, Inc1994632643
- GableRReview of the test Self-Description Questionnaire-I, II, IIIThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=OOHBFPJJOLDDEPHCNCPKIBLBCGHLAA00&Complete+Reference=S.sh.30%7c5%7c1
- IsonioSReview of the test Self-Description Questionnaire-I, II, IIIThe thirteenth mental measurements yearbook1998 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=OOHBFPJJOLDDEPHCNCPKIBLBCGHLAA00&Complete+Reference=S.sh.30%7c5%7c1
- LenningsCJLawlerJRSelf concept: A study of marsh’s self description questionnaire (SDQ-2)Social Behavior and Personality1992204243245
- MarshHWParkerJBarnesJMultidimensional adolescent self-concepts: Their relationship to age, sex, and academic measuresAmerican Educational Research Journal1985223422444
- PierselWCReview of the test Structured Pediatric Psychosocial InterviewThe tenth mental measurements yearbook1989 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=OOHBFPJJOLDDEPHCNCPKIBLBCGHLAA00&Complete+Reference=S.sh.32%7c1%7c1
- WebbTEWeryKDKrillCEChildhood hemophilia: Application of a measure of self-reported psychosocial distressThe Journal of Genetic Psychology: Research and Theory on Human Development19851462281282
- WeinbergRAReview of the test Structured Pediatric Psychosocial InterviewThe tenth mental measurements yearbook1989 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=OOHBFPJJOLDDEPHCNCPKIBLBCGHLAA00&Complete+Reference=S.sh.32%7c1%7c1
- GoodmanRMeltzerHBaileyVThe strengths and difficulties questionnaire: A pilot study on the validity of the self-report versionEuropean Child and Adolescent Psychiatry1998731251309826298
- MellorDNormative data for the Strengths and Difficulties Questionnaire in AustraliaAustralian Psychologist2005403215222
- PercyAMcCrystalPHigginsKConfirmatory factor analysis of the adolescent self-report strengths and difficulties questionnaireEuropean Journal of Psychological Assessment20082414348
- RuchkinVJonesSVermeirenRSchwab-StoneMThe strengths and difficulties questionnaire: The self-report version in American urban and suburban youthPsychological Assessment200820217518218557695
- CosdenMReview of the test Youth Risk and Resilience InventoryThe seventeenth mental measurements yearbook2007 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=LCNIFPAIJCDDEPHNNCPKAEFBBBPLAA00&Complete+Reference=S.sh.14%7c1%7c1
- KonaldTRReview of the test Youth Risk and Resilience InventoryThe seventeenth mental measurements yearbook2007 Retreived from http://ovidsp.tx.ovid.com.ezproxyl.canberra.edu.au/sp-3.5.1a/ovidweb.cgi?&S=LCNIFPAIJCDDEPHNNCPKAEFBBBPLAA00&Complete+Reference=S.sh.14%7c1%7c1