Abstract
Background
Problem-based learning (PBL) has made a major shift in support of student learning for many medical school curricula around the world. Since curricular development of PBL in the early 1970s and its growth in the 1980s and 1990s, there have been growing numbers of publications providing positive and negative data in regard to the curricular effectiveness of PBL. The purpose of this study was to explore supportive data for the four core objectives of PBL and to identify an interface between the objectives of PBL and a learner-centered paradigm.
Methods
The four core PBL objectives, ie, structuring of knowledge and clinical context, clinical reasoning, self-directed learning, and intrinsic motivation, were used to search MEDLINE, the Education Resources Information Center, the Educator’s Reference Complete, and PsycINFO from January 1969 to January 2011. The literature search was facilitated and narrowed if the published study included the following terms: “problem-based learning”, “medical education”, “traditional curriculum”, and one of the above four PBL objectives.
Results
Through a comprehensive search analysis, one can find supportive data for the effectiveness of a PBL curriculum in achieving the four core objectives of PBL. A further analysis of these four objectives suggests that there is an interface between PBL objectives and criteria from a learner-centered paradigm. In addition, this review indicates that promotion of teamwork among students is another interface that exists between PBL and a learner-centered paradigm.
Conclusion
The desire of medical schools to enhance student learning and a need to provide an environment where students construct knowledge rather than receive knowledge have encouraged many medical schools to move into a learner-centered paradigm. Implementation of a PBL curriculum can be used as a prevailing starting point to develop not only a learner-centered paradigm, but also to facilitate a smooth curricular transition from a teacher-centered paradigm to a learner-centered paradigm.
Introduction
Problem-based learning (PBL) was created and initially implemented at McMaster University in Hamilton, ON, Canada, in 1969. The stakeholders at McMaster University were eager to introduce a new learning tool to reduce the faculty’s role as a primary information giver and to replace passive learning by students with an active learning process. At McMaster University, PBL was implemented into a medical curriculum in which small-group study of clinical problems with self-directed learning and self-assessment techniques were implemented.Citation1 Soon after, PBL was positively received by a few other medical schools, including the University of Limburg at Maastricht (The Netherlands), the University of Newcastle (Australia), and the University of New Mexico (US),Citation1 and subsequently was implemented in a few medical schools in the UK. In addition, PBL rapidly found its way into other disciplines, including education, law, business, and professional health sciences.Citation1,Citation2 In the years 1970–1990, over 60 medical schools adopted the PBL curriculum around the world.Citation1 Today, the vast majority of medical schools in Canada and approximately 80% of medical schools in the US have integrated PBL into their curricula. However, in half of the medical schools in the US, only a small portion (less than 10%) of their preclinical curriculum has been delivered in a PBL format.Citation3
In the early 1970s, the stakeholders at McMaster University described PBL as a learning tool in which learners focused on a problem and used their previously gained knowledge in order to think rationally about solving the problem. In this manner, it was suggested that PBL would motivate students to participate in active intellectual processes at higher cognitive levels which ultimately would enhance student learning and knowledge retention.Citation4 During the implemented PBL, students were introduced to the learning strategies related to problem-solving, self-directed learning, and small-group tutorials, in which tutors played an important role in facilitating student group discussions.
Since 1970, PBL has been used in different formats to assist the curricula of different medical schools in enhancing student learning and clinical skills. The most frequently used PBL format is characterized as generating a series of carefully chosen problems to be presented to students in a small group setting. The problems are simulated with authentic patient cases in which patients complain about a disease or disorder with clinical signs and symptoms. The student group meets twice a week for 2 or 3 hours per each meeting. Between these meetings, group members are expected to spend significant time on self-directed learning to find relevant information for further group discussions. Usually, students are free to choose their own resources. In the meetings, the student group discusses and analyzes the main points of a problem and synthesizes possible explanations and working hypotheses for the problem. During each group discussion, the group is guided by a faculty member (a tutor) whose assignment is to stimulate group discussion and to evaluate and monitor group members’ contribution and progress in solving the problem. In addition, occasional lectures relevant to the problem may be given by the tutor. PBL problems are designed so that the student group is focused on simpler problems and progressively approaches more complex problems. For instance, the student group may work on insulin and its effect on carbohydrates and fatty acid metabolism before the group works on diabetic patient cases. This progressive sequence allows students to acquire knowledge using simpler problems, and use their knowledge, with newly added information, to solve more complicated clinical problems effectively. In addition, it is important to provide training for student groups to collaborate effectively with each other prior to receiving the problems and assignments.Citation5,Citation6
A learner-centered paradigm is a shift in higher education where lecture-based presentations and a passive transmission of knowledge from faculty to students is no longer the core of curriculum and student learning.Citation7 Rather, students are actively involved in their learning and are motivated to explore information actively to synthesize and construct new knowledge. Many colleges and schools have attempted to depart from a teacher-centered environment and move toward a learner-centered environment.Citation7,Citation8 This paradigm shift causes colleges and universities to ask how students are learning rather than how faculty are teaching. However, a paradigm shift does not occur overnight, and takes significant amounts of time and effort from administration, faculty, and students to facilitate the transition to a new environment. A systematic review of published studies was conducted in the present review to explore supportive data for the four core objectives of PBL. In addition, a further analysis of these published studies was carried out to indicate whether there was an interface between PBL objectives and a learner-centered paradigm.
Methods
The MEDLINE database was searched using different combinations of keywords (see ) from January 1969 to January 2011. Because the MEDLINE database provided only journals relevant to healthcare, it was important to include other educational journals. As a result, the following key words: “problem based learning”, “medical education”, “traditional curriculum”, and “self-directed learning” were used to search the Education Resources Information Center for 1969–2011 which produced three articles, the Educator’s Reference Complete for 1980–2011 which produced three articles, and PsycINFO for 1969–2011 which produced one article. Papers were included if they met the criteria of PBL being implemented in a medical school and provided comparative data between PBL and traditional curricula.
Table 1 MEDLINE was used to search different combinations of key words in order to find supportive and relevant data regarding PBL curriculum in medical schools
Results
Huba and Freed have elegantly outlined and compared the criteria for teacher-centered and learner-centered paradigms ().Citation7 As Huba and Freed point out, student learning is the ultimate goal that the educators should focus on and, as a result, they must shift from a traditional teaching model to a learner-centered model.Citation7 In a learner-centered environment, students are more active in a teamwork manner than a teacher-centered paradigm. Similarly, faculty are more engaged in accommodating and facilitating discussions among students, are encouraged to be innovative in teaching and assessment, integrate more disciplines into their teaching, and faculty and students assess student learning together.Citation7 On the other hand, in a teacher-centered paradigm, the focus is on how well a faculty teaches. Questions such as how well organized and accurate the lectures are, how well the presenters maintain student interest, and how well the material is presented, are the focus of teacher-centered instruction.
Table 2 Comparison of criteria and activities implemented in a teacher-centered paradigm and a learner-centered paradigmCitation7
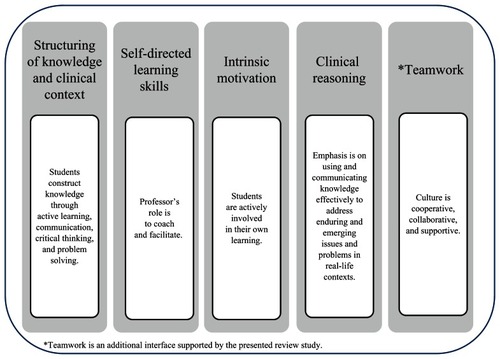
There are four major objectives of PBL that were well established by Barrows in 1986, which included structuring of knowledge and clinical context, clinical reasoning, self-directed learning skills, and intrinsic motivation.Citation9 These objectives were originally established to expose students to real-life problems so that students could learn the craft of examining a patient’s clinical problem, diagnosing it, and making an informed decision about appropriate action and treatment to remedy the problem. compares the PBL objectives of Barrows with a few criteria from the learner-centered model, and demonstrates an interface between all four objectives of PBL (gray box) and the listed learner- centered criteria (white box). In the following sections, a series of interfaces between PBL objectives and learner-centered criteria are presented and discussed.
Structuring of knowledge and clinical context
Student learning is based on structuring of knowledge rather than a passive memorization of facts. In order to structure knowledge, students analyze a problem, utilize their prior knowledge, and use and process new information to solve a problem or cope with an assignment. In a comparative study conducted by Van der Veken et al three different curricula (conventional, integrated contextual, and PBL) were compared using Vermunt’s Inventory of Learning Styles to identify differences in student learning. In comparing PBL with the traditional curriculum, while students from the PBL curriculum gained fewer benefits from rote learning, rehearsing, and ability to express study content in a personal manner, they gained higher benefits in knowledge and self-regulation of learning.Citation10 In another study conducted by Visschers-Pleijers et al in which 48 medical students participated in six focus group interviews, the authors assessed how the PBL curriculum assisted students in integrating and applying knowledge in their learning. Their assessment results indicated that the main learning effects for students were retention, understanding, integration, and application of knowledge.Citation11 In addition, Kamin et al showed that a series of cases, presented in a PBL curriculum, assisted students in structuring their knowledge, conceptualizing how to handle difficult situations, differentiating between abnormal and normal physical examination findings, and developing critical thinking skills.Citation12 In a specific disease state, ie, hypertension, Shin et al showed that the graduates of their medical school with a PBL curriculum were more up to date on knowledge of the management of hypertension than graduates of a traditional curriculum.Citation13 The ability to structure knowledge in order to construct a correct answer is an important skill during clinical examinations in medical curricula. In a comparison study of PBL and traditional curricula, it has been suggested that PBL students perform better on clinical examinations than on basic science examinations.Citation14
The above studies match well with a learner-centered environment that encourages students to construct knowledge through active learning, communication, critical thinking, and problem solving.Citation7 Structuring knowledge can assist students in using their knowledge more effectively in order to solve ill-defined medical cases. For instance, it has been suggested that the reason some students do not remember facts and concepts of a discipline or do not know when to use their knowledge, compared with experts (faculty) who do remember their knowledge, is that faculty’s knowledge is well structured and organized in their memories.Citation15 This indicates assignments and problems that assist students in structuring their knowledge can promote the quality of student thinking and learning.
Clinical reasoning
Clinical reasoning skills are essential components of both didactic and experiential education at medical schools. They assist students in examining a patient’s history, performing a physical examination, and evaluating all relevant clinical and laboratory data in order to achieve an effective therapeutic outcome. In a meta-analysis study, the effect of PBL during preclinical experience was assessed. The results indicated that the PBL experience was perceived very positively during the preclinical phase of student training and assisted students in building up their clinical competence during their first clerkship experiences.Citation16 In a similar study, in which a comparison was made between PBL and traditional curricula for clinical performance in a third-year medical clerkship, the results indicated that the preclinical PBL enhanced third-year students’ clinical performance.Citation17 Characteristics and outcome data from PBL and traditional curricula were compared by Distlehorst et al. In several of their clerkship performance assessments, PBL students performed significantly better than students from the traditional curriculum.Citation18 In a series of studies conducted by Barrows, it was indicated that PBL enhanced student clinical reasoning and problem solving skills.Citation9,Citation19 It has been suggested that, in a PBL curriculum, the student’s approach to solving a clinical case is different compared with a traditional curriculum. In a PBL curriculum, students not only study the clinical concepts of a case, but they also study the basic and social science concepts of the case in order to develop clinical reasoning skills.Citation20
In a learner-centered environment, students establish their reasoning strategies by communicating their knowledge to address emerging issues in real-life contexts.Citation7 Quellmalz and Hoskyn have established many different reasoning strategies that can be applied in a learner-centered paradigm. A few of these reasoning strategies include comparing, error analysis, constructing support, analyzing perspectives, decision- making, investigation, experimental inquiry, problem- solving, and invention.Citation21 A closer look at these reasoning strategies and the PBL curriculum indicates that the PBL curriculum accommodates many of these reasoning strategies during student group discussions to encourage students to use their clinical reasoning more effectively.Citation9,Citation17,Citation19
Self-directed learning skills
Self-directed learning skills demonstrate that students are self-guided and know how to use their knowledge and resources to complete problems or assignments.Citation8,Citation22 Schmidt et al have described the roles of PBL tutors as facilitators in student group discussions, who share their knowledge when the assigned problems turn out to be too complex or when there is a lack of essential knowledge for the group to progress effectively with their discussions.Citation23 This is in line with the role of faculty in a learner-centered paradigm, ie, “ professor’s role is to coach and facilitate” rather than being the primary information giver.Citation7 In another study, Watmough et al conducted a study in which 45 physicians were interviewed to evaluate the impact of a PBL curriculum on their education and practice 6 years after their graduations. The study results indicated that the physicians felt they were clinically well prepared, with good clinical and communication skills, and had good self-directed learning and research skills. However, they felt their basic science knowledge level was weaker than traditional graduates.Citation24 In a comprehensive review study comparing PBL and traditional medical curricular conducted by Koh et al it was shown that self-directed learning skills from a PBL curriculum were rated by students as moderate.Citation25 However, their systematic review indicated that PBL had a positive effect on physicians’ performance and competence after graduation. In a similar review study, Rao and Rao showed that PBL is the most effective way to foster students to be independent thinkers and problem solvers by becoming self-directed learners to gather necessary information to resolve specific clinical problems.Citation26 Rahman et al conducted a 2-year study to assess the knowledge and attitude of students before and after implementation of a PBL curriculum. They demonstrated that the implementation of PBL significantly improved student skills in clinical knowledge, attitude, and practice. A majority of their students stated that PBL enhances self-directed learning.Citation27 In another study conducted from 1999 to 2002 in a medical school in India, the investigator indicated that the implementation of a PBL curriculum, alongside their traditional didactic curriculum, improved students’ motivation in self-directed learning and benefited student learning by relating a clinical condition to a basic science mechanism.Citation28 In addition, in a review conducted by Norman and Schmidt, it was suggested that PBL enhanced student self-directed learning and made students more enthusiastic learners.Citation5
As a result of the role of the faculty as facilitator, rather than primary information giver, self-directed learning is strongly promoted in a learner-centered model. It has been suggested that when the faculty’s role is to guide and coach, they provide an environment for students to discuss, explore the available resources, and use their own knowledge to make an informed judgment.Citation8,Citation22,Citation29
Intrinsic motivation
Behavioral psychologists have suggested that motivation plays an important role in student learning.Citation30 As a result, many medical schools are interested in implementing PBL because of its potential to enhance student motivation in learning. However, there is scarce research regarding the effect of PBL on intrinsic motivation. In a study by White, a PBL curriculum was compared with a traditional curriculum during the first and second academic years. The results indicated that the PBL curriculum had a positive impact on students, who found themselves motivated to learn, and were able to direct their motivation into effective transition from the classroom into their clerkship training. The authors concluded that self-regulated learning facilitated the transition from basic sciences to experiential experiences.Citation31 Indeed, Langelotz et al compared student motivation in learning from both traditional and PBL curricula during their fourth clinical semester, and found that the PBL in the surgical curriculum increased students motivation.Citation32 Similarly, Chang et al found that in a comparison between PBL and traditional curricula, students in a PBL curriculum cultivated their interest in anesthesia, increased their motivation to learn actively, and were more enthusiastic in anesthesia research.Citation33 Barrows and Tamblyn suggested that PBL increased student intrinsic motivation in learning, students were able to define their learning approach, and students decided what was important and relevant for their learning.Citation34
In a learner-centered paradigm, students are actively involved in their own learning because they are motivated. In a study conducted by Cheang, a series of surveys was developed to determine the effect of the learner-centered paradigm in enhancing students’ intrinsic motivation to complete a pharmacy course. The results of this study indicated that goal orientation, control of learning, and self-efficacy, which were a few domains of motivation, were significantly improved and assisted students in developing learning skills and self-awareness.Citation35 Similarly, Spencer and Phipps, in their learner-centered study of a drug literature evaluation course, suggested that students had more control of their learning environment and had multiple opportunities to demonstrate their learning.Citation36
Teamwork
Teamwork is a trend that is clearly evident in the PBL curriculum in which student groups develop a common goal to complete a clinical case assignment. It has been suggested that a PBL curricular implementation can accommodate the needs for developing teamwork skills,Citation37 and PBL medical graduates, compared with traditional medical graduates, have learned better communication and teamwork skills.Citation38 Because the success of each individual is tied to the success of the team, students are motivated to help each other, which in turn promotes cooperative learning.Citation39 In addition, students who work on teamwork assignments achieve a high understanding of complex and difficult problems that is often challenging to achieve individually.Citation40 One apparent PBL objective, although not listed in the four objectives of Barrow, is teamwork. Teamwork is also one of the learner-centered criteria ()Citation7 which states that the culture of learning is cooperative, collaborative, and supportive () or, in other words, the culture is noncompetitive. In both PBL and a learner-centered paradigm, team members feel their contributions are appreciated and valued, that they make collective decisions, and focus on common goals. As Michaelsen and Sweet point out, teamwork provides an environment in which team members progress well, achieve a depth of understanding, identify their strengths and weaknesses, and the group develops into a self-managed learning team.Citation40
Discussion
The fast-paced stream of medical information, a high expectation from the medical accreditation and national board examination agencies, an intensive trend of basic science learning followed by demanding clinical training, and diverse student learning have encouraged many faculty and stakeholders at medical schools to innovate new curricular designs to promote student learning. There are virtually three curricula that are implemented by most medical schools in the US, ie, lecture-based, problem-based, and a combination of both. While the lecture-based curriculum is one of the most widely used instructional techniques, its effectiveness has been criticized and questioned for many years.Citation41 On the other hand, PBL has been cited by mounting literature as an effective curriculum that actively engages students in their learning.Citation2,Citation9,Citation34 However, a few data have brought into question the effectiveness of PBL in improving student overall learning and knowledge and the improvement of patient’s health, physicians’ knowledge and performance,Citation42–Citation44 or have suggested that a PBL curriculum does not teach problem solving better than a traditional curriculum. Citation45 Despite the fact that the PBL curriculum has been endorsed by the Association of American Medical CollegesCitation46 and the World Federation of Medical Education,Citation47 surprisingly, there are few published data providing conclusive evidence that a PBL curriculum fosters more qualified physicians than any other curricula.
Despite a variation in the lengths of PBL curricula (at a course level versus at a program level) presenting a challenge in this study in terms of providing a pattern of consistent measures of the effectiveness of PBL, one can create an interface between PBL and a learner-centered paradigm. During the last 40 years, PBL has represented a major shift in educational practice, particularly in medical schools, and is one of the most studied and researched curricula in higher education. Citation34 On the other hand, since the mid 1980s, as a product of the Joint Task Force on Student Learning appointed by the American Association for Higher Education, the American College Personnel Association, and the National Association of Student Personnel Administrators, many universities and colleges have departed from a teacher-centered paradigm and moved toward a learner-centered paradigm.Citation7,Citation48
As suggested in the results section of this review, in a learner-centered paradigm, students construct knowledge through active learning, communication, critical thinking, and problem solving, which are also skills accommodated by a PBL curriculum. Structuring of knowledge and clinical context is a challenging task for medical students and often requires the faculty’s intervention to facilitate this skill. In a PBL curricular activity, collaborative learning is encouraged to conduct effective discussions, integrate new information, and apply prior knowledge which, in turn, provides an environment where students can construct knowledge.Citation11
Clinical reasoning plays an important role in developing qualified physicians because it reinforces a cognitive process by which a clinical case is reviewed, analyzed, and explored to diagnose or suggest a therapeutic solution to a disease.Citation49 In other words, clinical reasoning skills develop when a student uses his/her knowledge effectively to review and address clinical issues in real-life contexts. Barrows, in his study, indicated that a PBL curriculum promotes clinical reasoning skills.Citation9 In a teacher-centered paradigm, students often face “black and white” assignments that are also called “well-defined”. A pattern of solving these problems does not prepare students for real-life problems that often are “gray” or “ill-defined”.Citation7 On the other hand, in a learner-centered environment, students are challenged to deal with “real-life” problems to promote their knowledge and skills in areas of inquiry, reasoning, and problem solvingCitation7 which ultimately will assist them in developing their clinical reasoning skill. Promoting self-directed learning skills is a challenging process for faculty members and students. In a learner-centered paradigm, the role of the faculty is to coach and facilitate,Citation7 which ultimately encourages students to be self-guided and know how to use their knowledge and resources to complete a clinical case assignment.Citation8,Citation22 There is increasing evidence that, in a PBL curriculum, compared with a traditional curriculum, students are more self-directed and enthusiastic learners, which ultimately promotes graduates to be life-long learners.Citation9,Citation50,Citation51 In an interesting study, medical students’ engagements in borrowing study material from libraries was compared between PBL students and traditional students. The results revealed that PBL students borrowed more material (67 books/student/year) than the traditional students (43 books/student/year). In addition, this difference was amplified during the clerkship, ie, 40 books/student/year compared with 11 books/student/year.Citation52 The latter result indicated that students were enthusiastic learners, with a desire to explore and acquire more information in a self-directed manner.
Intrinsic motivation has been identified as one of the driving factors that ignites student’s interest in issues relevant to problems. When students are confronted with problems that they do not understand easily, they will actively seek information to solve the presented problems.Citation53 In line with the criterion for a learner-centered paradigm that states students are actively involved in their own learning, students must be motivated in order to be involved actively in their learning. Attending presentations and watching a series of faculty notes, the trends in a teacher-centered paradigm, do not support student learning.
This review suggests that there is an additional interface, ie, teamwork, which exists between PBL and learner-centered curricula. In teamwork, each team member brings a diverse set of knowledge, skills, experience, and expertise, not only to complement but also to support one another’s strengths.Citation54 Collaborative learning is a trend that is evident in a PBL curriculum in which students have a common goal to complete a clinical case assignment. The most recent Accreditation Council for Graduate Medical Education standards in 2011 emphasizes the role of teamwork in training medical residents. This standard states that “Residents must care for patients in an environment that maximizes effective communication. This must include the opportunity to work as a member of effective interprofessional teams that are appropriate to the delivery of care in the specialty”.Citation55 This statement stresses the importance of teamwork in the graduate medical education, which is consistent with the teamwork that PBL and learner-centered curricula accommodate. The teamwork objective, although it is not listed in the four objectives of Barrow, corresponds to one of the learner-centered criteria () that identifies the culture of learning as cooperative, collaborative, and supportive ().
In addition to the interfaces between a PBL paradigm and a learner-centered paradigm identified above, Huba and Freed have developed eight hallmarks for a learner-centered paradigm.Citation56 Many of these hallmarks are also supported by the PBL curriculum, ie, learners are actively involved and receive feedback, apply knowledge to enduring and emerging issues and problems, and integrate discipline-based knowledge and general skills.
Finally, it is worth mentioning that tutors have a critical role in the PBL process. A tutor’s way of coaching can change the interface between a PBL curriculum and a learner-centered paradigm. In order to maintain the interface between these two curricula, special attention needs to be paid to train tutors in a PBL process. For instance, when tutors are confronted with problems in group work, such as students who do not actively participate in group discussions or do not contribute to achieve the goals of the study, those tutors who implement solutions to problems or cases are characterized as teachers in a teacher-centered paradigm rather than facilitators in a learner-centered paradigm.Citation57
The information presented in this review shows that there is adequate support to create an interface between the objectives of PBL and a learner-centered paradigm. In addition, the faculty’s role as a facilitator, involving students in evaluating student learning, and intertwining teaching and assessment, are other components of a learner-centered paradigm that often are visible in a PBL curriculum. These parallel matches indicate that implementing a PBL curriculum can facilitate a smooth transition from a teacher-centered paradigm to a learner-centered paradigm. The Flexner report of 1910 has influenced medical education in the US and Canada in a positive way.Citation58 This report emphasized the importance of applying alternative instructional methods that stressed active learning for medical students. Indeed, what Flexner was referring to was similar to what PBL and learner-centered curricula refer to regarding replacing student’s passive learning with an active learning process. However, it is important to stress that a theoretical well-matched alignment between a PBL objective and a learner-centered criterion does not justify an interface between a PBL curriculum and a learner-centered paradigm. In other words, there must be existing data to support a coherent curricular interface.
It is worth mentioning that this review has a number of limitations. Firstly, the Educator’s Reference Complete database did not provide data prior to January 1969 (data were only available for 1980 on wards). Secondly, whilst the literature search yielded compelling data that PBL supports student learning, the impact of PBL on improving physician interaction and communication with patients and other healthcare providers has not been researched to any significant extent. Lastly, the inconsistency in the development and implementation of different PBL formats among medical schools made this review a challenging task to provide a pattern of consistent measures of the effectiveness of PBL.
Conclusion
Data published since 1969 in regards to PBL and traditional curricula in medical schools have been explored and reviewed. A comparison between these two curricula suggests that there are similarities between PBL objectives and curricular benefits that a learner-centered paradigm provides. This paper is distinguished from other articles with regard to the effects of PBL curriculum in medical schools because it depicts a supportive interface between a few criteria from a learner-centered paradigm and the four major objectives of PBL. Because of this coherent interface, medical schools interested in departing from a teacher-centered environment and moving toward a learner-centered environment can implement a PBL curriculum to begin a smooth shift from their current teaching model.
Acknowledgment
The author would like to sincerely thank Cari Bauman, an Intern Pharmacist at Pacific University School of Pharmacy, for providing valuable comments on the manuscript.
Disclosure
The author reports no conflicts of interest in this work.
References
- NevilleANormanJGeoffRPBL in the undergraduate MD program at McMaster University: Three iterations in three decadesAcad Med20078237037417414193
- BarrowsHSProblem-based learning in medicine and beyond: A brief overviewNew Directions for Teaching and Learning199668312
- KinkadeSA snapshot of the status of problem-based learning in US medical schools, 2003–04Acad Med20058030030115734817
- NeufeldVRBarrowsHSThe “McMaster Philosophy”: An approach to medical educationJ Med Educ197449104010504444006
- NormanGRSchmidtHGEffectiveness of problem-based learning curricula: Theory, practice and paper dartsMed Educ20003472172810972750
- SchmidtHGLoyensSMProblem-based learning is compatible with human cognitive architecture: Commentary on Kirschner, Sweller, and ClarkEduc Psychol2006429197
- HubaMEFreedJELearner-Centered Assessments on College Campuses, Shifting the Focus From Teaching to LearningNeedham Heights, MAAllyn and Bacon2004
- KarimiRArendtCSCawleyPLearning bridge: Curricular integration of didactic and experiential educationAm J Pharm Educ201074 Article 48
- BarrowsHSA taxonomy of problem-based learning methodsMed Educ1986204814863796328
- Van der VekenJValckeMMuijtjensAThe potential of the inventory of learning styles to study students’ learning patterns in three types of medical curriculaMed Teach20083086386918821163
- Visschers-PleijersAJDolmansDHde GraveWSStudent perceptions about the characteristics of an effective discussion during the reporting phase in problem-based learningMed Educ20064092493116925644
- KaminCDeterdingRLowryMStudent’s perceptions of a virtual PBL experienceAcad Med2002771161116212431939
- ShinJHHaynesRBJohnstonMEEffect of problem-based, self-directed undergraduate education on life-long learningCMAJ19931489699768257470
- ThomasREProblem-based learning: Measurable outcomesMed Educ1997313203299488851
- KurfissJGCritical thinking: Theory, research, practice, and possibilitiesASHE-ERIC higher education report No 21988Washington, DCThe George Washington University, Graduate School of Education and Human Development1988
- HeymanSNRechesASafadiRIntroduction of a brief problem-based-learning (PBL) experience in traditional medical faculty curriculumHarefuah200714643543817760396
- RichardsBFOberKPCariaga-LoLRatings of students’ performances in a third-year internal medicine clerkship: A comparison between problem-based and lecture-based curriculaAcad Med1996711871898615938
- DistlehorstLHDawsonERobbsRSProblem-based learning outcomes: The glass half-fullAcad Med20058029429915734816
- BarrowsHSFeltovichPJThe clinical reasoning processMed Educ19872186913574170
- IvesTJDeloatchKHIshaqKSIntegration of medicinal chemistry and pharmacotherapeutics courses: A case-based, learner-centered approachAm J Pharm Educ199862406411
- QuellmalzESHoskynJClassroom assessment of reasoning strategiesPhyeGDHandbook of Classroom AssessmentSan Diego, CAAcademic Press1997
- KarimiRCawleyPArendtCSLearning bridge tool to improve student learning, preceptor training, and faculty teamworkAm J Pharm Educ 2011200175 Article 46
- SchmidtHGDe GraveWSDe VolderMLExplanatory models in the processing of science text: The role of prior knowledge activation through small-group discussionJ Educ Psychol198981610619
- WatmoughSDO’SullivanHTaylorDGraduates from a reformed undergraduate medical curriculum based on tomorrow’s doctors evaluate the effectiveness of their curriculum 6 years after graduation through interviewsBMC Med Educ2010101820074350
- KohGCKhooHEWongMLThe effects of problem-based learning during medical school on physician competency: A systematic reviewCMAJ2008178344118166729
- RaoKHRaoRHPerspectives in medical education. Implementing a more integrated, interactive and interesting curriculum to improve Japanese medical educationKeio J Med200756758417906418
- RahmanMERahmanSMusaAKKnowledge and attitude of clinical students on problem based learningMymensingh Med J20041312512915284685
- GhoshSCombination of didactic lectures and case-oriented problemsolving tutorials toward better learning: Perceptions of students from a conventional medical curriculumAdv Physiol Educ20073119319717562910
- CorneskyRLazarusWContinuous Quality Improvement in the Classroom: A Collaborative ApproachPort Orange, FLCornesky and Associates Inc1995
- BiehlerRFSnowmanJPsychology Applied to Teaching10th edBoston, MAHoughton Mifflin Company2002
- WhiteCBSmoothing out transitions: How pedagogy influences medical students’ achievement of self-regulated learning goalsAdv Health Sci Educ Theory Pract20071227929716767503
- LangelotzCJunghansTGüntherNProblem-based learning for surgery. Increased motivation with less teaching personnel?Chirurg20057648148615891932
- ChangCHYangCYSeeLCHigh satisfaction with problembased learning for anesthesiaChang Gung Med J20042765466215605905
- BarrowsHSTamblynRMProblem-based Learning: An Approach to Medical EducationNew YorkSpringer1980
- CheangKEffect of learner-centered teaching on motivation and learning strategies in a third-year pharmacotherapy courseAm J Pharm Educ2009734219564985
- HarpeSPhippsLBEvaluating student perceptions of a learnercentered drug literature evaluation courseAm J Pharm Educ200972 Article 135
- SellnowDDAhlfeldtSLFostering critical thinking and teamwork skills via a problem-based learning (PBL)Communication Teacher2005193338
- PrinceKJvan EijsPWBoshuizenHPvan der VleutenCPScherpbierAJGeneral competencies of problem-based learning (PBL) and non-PBL graduatesMed Educ20053939440115813762
- SmithKACooperative learning: Making “group work” workSutherlandTEBonwellCCUsing Active Learning in College Classes: A Range of Options for FacultySan Francisco, CAJossey- Bass1996
- MichaelsenLKSweetMFundamental principles and practices of team-based learningMichaelsenLKParmeleeDXMcMahonKKLevineRETeam-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving LearningSterling, VAStylus Publishing2008
- GuskinALearning more, spending lessAbout Campus199749
- MaudsleyGDo we all mean the same thing by “problem-based learning”? A review of the concepts and a formulation of the ground rulesAcad Med19997417818510065058
- ChangGCookDMaguireTProblem-based learning: Its role in undergraduate surgical educationCan J Surg19953813217882203
- SmitsPVerbeekJDe BuisonjeCProblem based learning in continuing medical education: A review of controlled evaluation studiesBMJ200232415315611799034
- BerksonLProblem-based learning: Have the expectations been met?Acad Med1993687988
- MullerSPhysicians for the 21st century: Report of the project panel of the general professional education of the physician and college preparation for medicineJ Med Educ19845911 Pt 21208
- WaltonHJMatthewsMBEssentials of problem based learningMed Educ1989235425582593886
- Joint Task Force on Student LearningLearning Principles and Collaborative ActionWashington, DCAmerican Association for Higher Education1998
- NormanGResearch in clinical reasoning: Past history and current trendsMed Educ20053941842715813765
- NormanGRSchmidtHGThe psychological basis of problem-based learning: A review of the evidenceAcad Med1992675575651520409
- Saarinen-RahiikaHBinkleyJMProblem-based learning in physical therapy: A review of the literature and overview of the McMaster University experiencePhys Ther1998781952079474111
- BlumbergPMichaelJDevelopment of self-directed learning behavioursTeaching and Learning in Medicine1992438
- HuntJUsing intrinsic motivation to teach young childrenPersonality Growth and LearningLondon, UKLongman1971
- GivenBSimmonsSThe interdisciplinary health-care team: Fact or fiction?Nurs Forum197716165185244357
- Accreditation Council for Graduate Medical Education2010 Available at: https://www.aamc.org/download/181516/data/2010_acgme_approved_standards.pdfAccessed March 26, 2011
- HubaMEFreedJELearner-Centered Assessments on College Campuses, Shifting the Focus From Teaching to LearningNeedham Heights, MAAllyn and Bacon2004
- DolmansDHWolfhagenIHvan der VleutenCPSolving problems with group work in problem-based learning: Hold on to the philosophyMed Educ20013588488911555227
- FlexnerAMedical Education in the United States and CanadaCarnegie Foundation for Higher Education1910 Available at: http://www.carnegiefoundation.org/sites/default/files/elibrary/Carnegie_Flexner_Report.pdfAccessed March 26, 2011.