Abstract
Background
Surgical management of breast cancer in large-breasted women presents a real challenge. This study aims to evaluate the outcome of therapeutic reduction mammoplasty in large-breasted women with breast cancer using superior and superomedial pedicles, situated at any breast quadrant except for the central and upper medial quadrants.
Methods
Fifty women with breast cancer and large breasts underwent simultaneous bilateral reduction mammoplasty. The weight of the tissue removed ranged from 550 g to 1050 g and the tumor-free safety margins by frozen section were in the range of 4 cm to 12 cm.
Results
The age of the patients ranged from 36 to 58 (median 43) years and tumor size ranged from 1 cm to 4 cm. The cosmetic outcomes were excellent in 32 patients (64%), good in 15 (30%) patients, and fair in three patients (6%). The follow-up period was 8–36 (mean 20) months, with no local recurrence or systemic metastasis.
Conclusion
Therapeutic reduction mammoplasty using superior and superomedial pedicles was shown to be oncologically safer than traditional conservative surgery. This oncoplastic procedure yields a satisfactory esthetic outcome with lower morbidity in large-breasted women with breast cancer.
Introduction
Breast conservation is a valuable component of breast cancer treatment, with a survival outcome equivalent to that of mastectomy.Citation1,Citation2 The treatment of breast cancer in large-breasted patients represents a great challenge to both surgeons and radiation oncologists, with such patients representing about 30%–40% of women undergoing breast-conserving therapy.Citation3 After traditional breast conservation therapy, 20%–30% of patients were reported to have poor cosmetic results.Citation4
Patients with macromastia treated with breast conservation therapy develop more complications and unacceptable cosmesis due to heterogeneous distribution of radiotherapy dose and suboptimal positioning of the breast between treatment sessions.Citation5,Citation6
Bilateral reduction mammoplasty when performed simultaneously using a superomedial pedicle results in a better esthetic result and improves oncological safety, because the tissues removed will include any lesion in the upper outer, lower outer, or lower inner quadrants, with a wider safety margin. Also, it offers a means of obtaining smaller and symmetrical breasts that tolerate radiotherapy more easily.Citation7
The oncoplastic concept is based on the possibility of performing large resections according to breast reduction techniques.Citation8 The goal of this paper is to report our results for bilateral mammoplastic reduction techniques in patients with large breasts using medial and superomedial pedicles.
Materials and methods
Fifty large-breasted women with early breast cancer were enrolled in this study. Standard criteria for breast conservation therapy were maintained in all selected patients with a single tumor confirmed by preoperative mammography. Oncologic exclusion criteria were inability to obtain tumor-free safety margins after reasonable attempts, multicentric carcinoma, inflammatory breast cancer, contraindication to radiotherapy, and infiltrating lobular carcinoma due to a high incidence of multicentricity, and the need for preoperative magnetic resonance imaging which was not feasible. Nononcologic exclusion criteria were small breast size, centrally located tumors, comorbidity, and the patient’s own treatment preference ().
Preoperative marking was performed according to the site of the tumor. The superior pedicle was used for tumors located in the lower inner quadrant (), while the superomedial pedicle was used mainly for tumors in the upper outer and lower outer regions. The same marking was performed for the other breast simultaneously ().
De-epithelialization of skin in the medial parts of the designed flap was done (). After tumor excision with a good safety margin (4–12 cm, ), the specimen was examined by frozen section in order to evaluate the safety margins.
In our series, we started first with the diseased breast, and after assessment of adequate tumor free safety margins, the same procedure in the contralateral breast was done to assure symmetry (). All patients were referred to the Clinical Oncology and Nuclear Medicine Department where they received radiotherapy and adjuvant chemotherapy according to the stage and type of tumor. Follow-up after stitch removal was weekly for one month, monthly for 6 months, every 3 months for one year, every 6 months for 2 years, and then yearly. All patients were evaluated for postoperative complications, and esthetic and oncologic outcomes. The esthetic outcomes were evaluated after 6 months and classified according to both surgeon and patient judgment as excellent, good, fair, and poor.
Results
The age of the patients ranged from 36 to 58 (median 43) years. Twenty-eight patients had tumors at the upper outer quadrant, 18 patients at the lower outer quadrant, and four patients at the lower inner quadrant. The size of the tumor ranged from 1 cm to 4 cm. Most of the patients were diagnosed as having infiltrating ductal carcinoma (44 patients, 88%). The weight of tissue removed ranged from 550 g to 1050 g. The tumor-free safety margins ranged from 4 cm to 12 cm.
Wound dehiscence was the commonest postoperative complication. It occurred in four patients, which was minor and affecting less than half of the longitudinal scar in three patients, and was managed conservatively. The fourth patient had secondary infection with dehiscence affecting more than half of the longitudinal scar and was managed by secondary suturing after infection control.
Moreover, two patients developed partial necrosis of the areola; these were small areas and were managed by debridement of the edges and secondary suturing. Another two patients developed a small firm area along the suture line 9 months postoperatively and were investigated by son mammography and Tru-cut biopsy, revealing traumatic fat necrosis that was surgically excised.
Six months postoperatively, the cosmetic outcome was judged by 32 women (64%) as excellent ( and ), 15 women (30%) patients showed good results (), and the other three patients (6%) rated the outcome as fair (). No local recurrence or systemic metastasis was noticed during the follow-up period, which ranged from 8 to 36 (mean 20) months.
Discussion
The management of cancer in the large ptotic breast poses many difficulties for surgeons performing traditional breast conservation therapy and for the radiation oncologist, due to heterogeneous distribution of the radiation dose. There are also the associated problems of chronic radiation-induced pain, fibrosis, and a poor cosmetic result after radiotherapy.Citation9
Mastectomy is associated with asymmetry which is not acceptable. If a large-breasted patient were to undergo complete mastectomy and decide not to undergo a reconstruction procedure, the contralateral breast could cause intolerable asymmetry and discomfort due to the huge breast volume and weight.Citation10
Appropriate surgical treatment of early breast cancer in the large-breasted woman who is a candidate for breast conservation therapy requires good knowledge of the basic mammoplastic techniques to deal with the various technical modifications needed for each individual case.Citation11 Local control could be a determinant of survival in a percentage of affected women, and large free margins of resection are recommended by the pioneers of breast conservative treatment.Citation12,Citation13
Denewer used the pectoralis major myomammary flap in large-breasted women as a method of reconstruction.Citation14 Reported advantages were that the donor side is reduced, with reconstruction of the other breast resulting in adjustment of the volume of both breasts in the same sitting, there is no loss of pectoralis major function because only a part of the muscle is used with easy transference, the nipple/areola complex is reconstructed during the same surgery, and four-quadrant biopsies can be taken from the healthy breast to be used in follow-up.Citation15 The main disadvantage of this procedure is symmastia.
With the introduction of skin-sparing and nipple-sparing mastectomies as reliable and safe surgical procedures that facilitate immediate breast reconstruction, the challenge of the large breast persists. Denewer et al developed a new modification for the extended latissimus dorsi flap using the visualized fat overlying the serratus anterior muscle with its own blood supply driven directly from the thoracic branch of the thoracodorsal artery. This richly vascularized fat adds significant bulk with a decreased incidence of fat necrosis, enabling the surgeon to reconstruct a larger breast size without a contralateral reduction operation or an implant, with a low flap complication rate.Citation16,Citation17
In this study, reduction therapeutic mammoplasty was used for the management of early breast cancer in large-breasted women, and we consider it to be a more conservative and less radical procedure.
Caruso et al evaluated the outcomes in 61 cases treated using reduction mammoplasty and reported five cases of skin complications and one case of partial nipple necrosis.Citation8 In the present study, four patients (8%) developed wound dehiscence and two cases of partial areolar necrosis. However, Munhoz et al reported an immediate complication rate of 17.6%, comprising skin necrosis (8.1%), infection (2.7%), partial necrosis of the nipple-areola complex (2.7%), dehiscence (1.35%), and total necrosis of the nipple-areola complex (1.35%).Citation18 Skin necrosis and wound dehiscence are the most often reported complications after therapeutic reduction mammoplasty.Citation19 Obese patients, smokers, and diabetics carry an increased risk of developing local complications.Citation20
In our study, there was no conversion to mastectomy due to the easy attainment of tumor-free safety margins in all cases, as a result of wider excision being possible in large breasts. McCulley and MacMillan reported a series of 50 breast cancer patients treated with therapeutic mammoplasty, in which four patients (8%) required reoperation due to surgical margin involvement.Citation21 Chang et al evaluated the degree of patient satisfaction and cosmetic results, and 20/37 women (54%) and 14/20 women (70%) reported excellent results.Citation7 We now report similar results from our study. Caruso et al reported one case (1.6%) of local recurrence with a follow-up period of 68 months,Citation8 and Chang et al showed a zero recurrence rate.Citation7 No local recurrence was observed in our short-term study, but a further long-term study is needed to assess the long-term outcome of this surgical procedure in Egyptian women as regards the risk of local recurrence.
Conclusion
Therapeutic reduction mammoplasty for early breast cancer in large-breasted women is a surgically and oncologically safe procedure that yields satisfactory esthetic results with lower morbidity.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgment
The authors gratefully acknowledge the contribution of Osama El-Damshety to this research.
Figure 1 Preoperative marking using the superior pedicle for a tumor located in the lower inner quadrant (green circle).
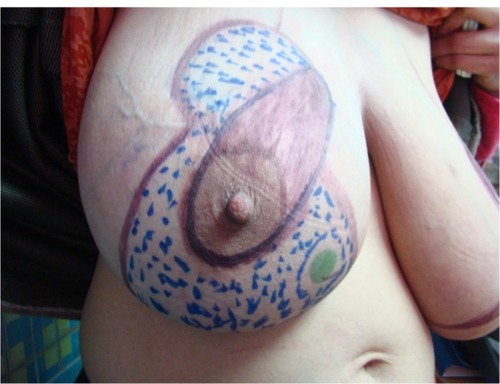
Figure 2 Preoperative marking using the superomedial pedicle; the lined green areas will be de-epithelized and the doted black areas will be resected with a safety margin where the tumor is located in the upper outer quadrant.

Table 1 Patients and tumor characteristics
References
- FisherBAndersonSBryantJTwenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancerN Engl J Med20023471233124112393820
- VeronesiUCascinelliNMarianiLTwenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancerN Engl J Med2002321227123212393819
- DundasKLAtyeoJCoxJWhat is a large breast? Measuring and categorizing breast size for tangential breast radiation therapyAustralas Radiol20075158959317958698
- BajajAKKonPSObergKCMilesADAesthetic outcomes in patients undergoing breast conservation therapy for the treatment of localized breast cancerPlast Reconstr Surg20041141442144915509931
- TaylorMEPerezCAHalversonKJFactors influencing cosmetic results after conservation therapy for breast cancerInt J Radiat Oncol Biol Phys1995317537647860386
- ChengCWDasIJSteaBThe effect of the number of computed tomographic slices on dose distributions and evaluation of treatment planning systems for radiation therapy of intact breastInt J Radiat Oncol Biol Phys1994301831958083113
- ChangEJohnsonNWebberBBilateral reduction mammoplasty in combination with lumpectomy for treatment of breast cancer in patients with macromastiaAm J Surg200418764765115135684
- CarusoFCatanutoGDe MeoLOutcomes of bilateral mammoplasty for early stage breast cancerEur J Surg Oncol2008341143114717981430
- BouvetMSingletarySEAmesFCombined breast conserving surgery and bilateral reduction mammoplasty facilitates postoperative radiotherapy and improves cosmesis in patients with early stage breast cancer and large pendulous breastBreast Dis19967236238
- Hernanz De La FuenteFReganoSVegaAReduction mammoplasty: an advantageous option for breast conserving surgery in large-breasted patientsSurg Oncol201019e95e10219716288
- Hernanz De La FuenteFGómez FleitasMMartínez GarcíaFReduction mammoplasty in breast cancer surgeryCir Esp200985140146 Spanish19264296
- Early Breast Cancer Trialists’ Collaborative GroupEffects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trialsLancet200536695032087210616360786
- NielsenHMVergaardMOvergaardJDanish Breast Cancer Cooperative GroupStudy of failure pattern among high-risk breast cancer patients with or without postmastectomy radiotherapy in addition to adjuvant systemic therapy: long-term results from the Danish Breast Cancer Cooperative Group DBCG 82 b and c randomized studiesJ Clin Oncol2006242268227516618947
- DenewerAMyomammary flap of pectoralis major muscle for breast reconstruction: new techniqueWorld J Surg19972157618943178
- DenewerASetitAFaroukOOutcome of pectoralis major myomammary flap for post-mastectomy breast reconstruction: extended experienceWorld J Surg2007311382138617514508
- DenewerAFaroukOCan nipple-sparing mastectomy and immediate breast reconstruction with modified extended latissimus dorsi muscular flap improve the cosmetic and functional outcome among patients with breast carcinoma?World J Surg2007311169117717464533
- DenewerASetitAHusseinOFaroukOSkin-sparing mastectomy with immediate breast reconstruction by a new modification of extended latissimus dorsi myocutaneous flapWorld J Surg2008322586259218224468
- MunhozAMMontagEArrudaEGCritical analysis of reduction mammoplasty techniques in combination with conservative breast surgery for early breast cancer treatmentPlast Reconstr Surg20061171091110316582770
- FitzalFNehrerGDeutingerMJakeszRGnantMNovel strategies in oncoplastic surgery for breast cancer: immediate partial reconstruction of breast defectsEur Surg200739330339
- MunhozAMFilassiJRAldrighiCBilateral reduction mammoplasty for immediate breast conservation surgery reconstruction and intraoperative radiotherapy: a preliminary reportAesthetic Plast Surg2007319410017205249
- McCulleySMacMillanRTherapeutic mammoplasty – analysis of 50 consecutive casesBr J Plast Surg20055890290716043153






