Abstract
Primary localized cutaneous nodular amyloidosis (PLCNA) is rare and clinically noncharacteristic, presenting mostly as plaque-like lesions. We report a case of a progressively larger erythematous plaque following a contusion of the skin on the right zygomatic area, which was strangely covered with recurrent scattered 2 mm whiteish blisters to the extent that it was misdiagnosed as a herpesvirus infection several times over a decade. Pathology and special staining diagnosed nodular amyloidosis with milia.
Introduction
Amyloidosis is the accumulation of proteins of the amyloid type in various tissues.Citation1 Primary localized cutaneous nodular amyloidosis is a rare and distinct type of amyloidosis;Citation2 it usually presents as single or multiple firm, waxy nodules or infiltrated plaque and occurs preferentially on the legs and commonly on the face and trunk but can be present anywhere on the skin.Citation3 Milia are benign keratinous cysts most commonly found on the face, especially on the cheeks and eyelids.Citation4 Primary milia emerge spontaneously, and secondary milia result from skin disease or trauma.Citation5 Here, we report an unusual case of primary localized cutaneous nodular amyloidosis associated with recurrent milia that occurred after local trauma.
Case Report
A 54-year-old Chinese female with limited persistent plaque and recurrent pustules for 11 years had an initial appearance of erythema, followed by whiteish pinhead-sized scattered blisters 1–2 days later. The blisters resolved after approximately 1 to 2 weeks, and topical iodophor was ineffective. The patient had been seen at another hospital and was diagnosed with herpes simplex. Oral valacyclovir and topical penciclovir cream were also ineffective. The patient recalled that she had lacerated her right zygomatic area with a wooden comb a few days before the onset of the plaque. Over the past 11 years, the plaque had gradually enlarged, with scattered blisters on the plaque recurring once every 1–2 months.
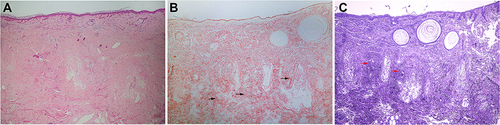
Physical examination revealed a 2×2 cm oval-shaped, well-demarcated, orange-yellow plaque with overlying scattered 2 mm whiteish blisters on the right zygomatic area (). No similar lesions were found elsewhere. Histopathologically, the overlying epidermis showed atrophic changes, and lymphocytes and plasma cells were found in the superficial dermis and around the blood vessels (). The entire dermis and subcutis were filled with eosinophilic, amorphous, and homogeneous amyloid material that was positive for Congo red and Crystal violet staining (the arrows in and represent the sites of amyloid deposition). Some keratin cysts were found in the superficial dermis ( and ). Arsenicum staining, acid staining, periodic acid-Schiff (PAS) staining and direct immunofluorescence (DIF) results were all negative, and all these findings were consistent with a diagnosis of primary localized cutaneous nodular amyloidosis with milia.
Figure 1 Orange‒yellow plaque with overlying scattered 2 mm whiteish blisters on the right zygomatic area.

Figure 2 Three pathological images of nodular amyloidosis. (A) Deposition of acellular amorphous eosinophilic materials over the entire dermis and subcutis (H&E, ×200). (B) The amyloid deposits were positive for Congo red staining, and keratinous cysts were found in the superficial dermis. The arrows indicate the sites of amyloid deposits.(Congo red staining, ×200) (C) The amyloid deposits were positive for crystal violet staining, and keratinous cysts were found in the superficial dermis. The arrows indicate the sites of amyloid deposits. (Crystal violet staining, ×200).
The patient has remained in good general health with no evidence of progression to systemic amyloidosis. Her blood count, blood chemistries, liver and kidney function, antinuclear antibody profile, serum protein electrophoresis and urine protein electrophoresis studies were normal. The patient refused our proposed surgical treatment option but indicated that she would be followed up regularly.
Discussion
Primary localized cutaneous amyloidosis is subdivided into papular, macular, and nodular amyloidosis. Nodular amyloidosis is the rarest type of primary localized cutaneous amyloidosis, presenting as waxy infiltrated plaque and nodules; it is characterized by the deposition of amyloid in the dermis, subcutaneous tissue and small blood vessels of the skin.Citation2 Dermoscopically, nodular amyloidosis shows features similar to granulomatous disease, including an orange background and distal vessels; reddish structureless and whitish area and ulcerations were also reported.Citation6 PLCNA represents a localized dyscrasia of plasma cells and is associated with autoimmune diseases, particularly Sjogren syndrome.Citation7 Plasma cell dyscrasia, possibly caused by an autoimmune disease, may induce the local production and deposition of immunoglobulin light chains.Citation8 Therefore, it is recommended to include anti-nuclear, anti-Ro/SSA and anti-La/SSB in the laboratory tests to exclude autoimmune diseases.
Milia are small, white, multiple, benign, superficial keratinous cysts,Citation9 and they can be divided into primary milia and secondary milia.Citation5 Primary milia are thought to develop from the sebaceous collar of vellus hairs, whereas most secondary milia originate from eccrine ducts rather than the overlying epidermis, hair follicles or sebaceous ducts.Citation10 The diagnosis of primary cutaneous nodular amyloidosis with recurrent milia is very rare and has not been reported.
In our case, the clinical presentation was misleading. Due to the rarity of PLCNA and the presence of milia, it could be easily be mistaken for other diseases, such as cutaneous sarcoidosis, lupus tumidus, pseudolymphoma, facial granuloma, benign lymphocytic infiltration, or herpes simplex virus type 1 (HSV-1) infections. This patient was misdiagnosed with herpes simplex for more than 10 years, and the associated medication was ineffective. Therefore, the clinicopathological correlation as well as subsequent follow-up is very important, since it can help with the correct diagnosis and management decisions.
The trigger for nodular amyloidosis is unclear, and suggested causes are speculative, while in secondary milia, the cause can be medication-related, disease-associated, or trauma-related. Milia are commonly caused by traumatizing superficial abrasions.Citation10 The patient had a history of abrasions, which were thought to be the cause of the milia. However, there is no consensus on whether trauma creates milia through epidermal implantation or by stimulating undifferentiated pilosebaceous cells to proliferate. The classic disease-associated type of milia is postbullous,Citation11 and other diseases include herpes zoster and bullous pemphigoid. Milia have not been found to be associated with nodular amyloidosis. Nevertheless, the recurrent appearance of milia in our case suggests a possible association with amyloid irritation.
In most cases, primary cutaneous nodular amyloidosis is benign and limited to the skin; however, it can progress to systemic disease in approximately 7% to 50% of patients.Citation12 Treatment of localized cutaneous nodular amyloidosis is difficult due to the lack of a consistently effective treatment. Various treatment modalities have been reported to improve the appearance of lesions, including surgical excision, cryotherapy, electrodesiccation and curettage, intralesional steroid injection, and more recently, carbon dioxide laser treatment.Citation13 Moreover, bleeding complications as well as the recurrence of skin lesions should be considered.Citation14 In our case, the medical history of primary cutaneous nodular amyloidosis reached 11 years, and no systemic progression was observed. It is unknown whether the presence of milia alters the risk of progression to systemic disease, and long-term follow-up is necessary. Based on relevant case reports, we recommend a follow-up period of 6 months after histopathological diagnosis.Citation15
Conclusion
This case shows a rare clinical presentation of milia in primary localized cutaneous nodular amyloidosis. We present for the first time that milia is associated with PLCNA and that amyloid may be the causative agent of milia, which contributes to the diagnosis of PLCNA. More studies are needed to verify this relationship between primary localized cutaneous nodular amyloidosis and milia.
Consent
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. Institutional approval was not required for this case study.
Disclosure
The authors report no conflicts of interest related to this work.
Acknowledgments
We thank the patient for her permission to publish this information. This work was supported by the Zhejiang Natural Science Foundation of China (LBZ22H160001).
References
- Mena L, Carrasco C, Folch H, de la Parra R, Carreño L. Primary cutaneous nodular amyloidosis associated with the injection of autologous fat. Clin Exp Dermatol. 2021;46:552–554. doi:10.1111/ced.14429
- Vestery JP, Tidman MJ, Mclaren KM. Primary nodular cutaneous amyloidosis – long-term follow-up and treatment. Clin Exp Dermatol. 1994;19:159–162. doi:10.1111/j.1365-2230.1994.tb01148.x
- Ung CY, Carr NJ, Ardern-Jones MR. Primary cutaneous nodular amyloidosis associated with psoriasis. Clin Exp Dermatol. 2014;39:608–611. doi:10.1111/ced.12347
- Dickison P, Howard V, Wylie B, Smith SD. Localized axillary milia en plaque: a rare cutaneous case presentation of systemic amyloidosis. Clin Exp Dermatol. 2016;41(7):764–767. doi:10.1111/ced.12914
- Yahya H. Idiopathic multiple eruptive milia: report of a case in a Nigerian woman. Niger J Clin Pract. 2018;21:395–396. doi:10.4103/njcp.njcp_43_17
- Rongioletti F, Atzori L, Ferreli C, Pinna A, Aste N, Pau M. A unique dermoscopy pattern of primary cutaneous nodular amyloidosis mimicking a granulomatous disease. J Am Acad Dermatol. 2016;74(1):e9–e10. doi:10.1016/j.jaad.2015.09.026
- Dupont L, Martins Souza PR, Damiani L, Boff AL. Cutaneous nodular amyloidosis: a disfiguring aspect of the face. Am J Dermatopathol. 2019;41:945–947. doi:10.1097/DAD.0000000000001470
- Bellinato F, Rosina P, Sina S, Girolomoni G. Primary nodular localized cutaneous amyloidosis of the scalp associated with systemic lupus erythematosus. Arch Rheumatol. 2022;37(1):145–147. doi:10.46497/ArchRheumatol.2022.8817
- Nambudiri VE, Habib N, Arndt KA, Kane KS. Milia en plaque of the nose: report of a case and successful treatment with topical tretinoin. Pediatrics. 2014;133:e1373–e1376. doi:10.1542/peds.2013-1728
- Berk DR, Bayliss SJ. Milia: a review and classification. J Am Acad Dermatol. 2008;59(6):1050–1063. doi:10.1016/j.jaad.2008.07.034
- Hisa T, Goto Y, Taniguchi S, Nakanishi T, Kakudo K, Takigawa M. Post-bullous milia. Australas J Dermatol. 1996;37(3):153–154. doi:10.1111/j.1440-0960.1996.tb01037.x
- Kalajian AH, Waldman M, Knable AL. Nodular primary localized cutaneous amyloidosis after trauma: a case report and discussion of the rate of progression to systemic amyloidosis. J Am Acad Dermatol. 2007;57:S26–S29. doi:10.1016/j.jaad.2006.12.014
- Fernandes C, Éthier V, Marouan S, Chababi-Atallah M, Veilleux M. Localized ulcerative nodular amyloidosis presenting as ulcerative panniculitis, an unusual clinical manifestation: a case report. SAGE Open Med Case Rep. 2019;7:1–3.
- Weidner T, Illing T, Elsner P. Primary localized cutaneous amyloidosis: a systematic treatment review. Am J Clin Dermatol. 2017;18:629–642. doi:10.1007/s40257-017-0278-9
- Woollons A, Black MM. Nodular localized primary cutaneous amyloidosis: a long-term follow-up study. Br J Dermatol. 2001;145:105–109. doi:10.1046/j.1365-2133.2001.04291.x
