Abstract
Restricted pagetoid reticulosis, also known as Woringer-Kolopp disease, represents a rare cutaneous lymphoproliferative disorder categorized as an isolated variant of mycosis fungoides. This report presents a case involving limited pagetoid reticulosis affecting the right upper extremity in a 25-year-old female. The patient had been experiencing plaques on the right upper extremity for a decade. Dermatologic examination revealed well-defined scaly plaques on the right forearm, surrounded by hyperpigmented patches. Skin histopathology demonstrated atypical mononuclear cell infiltration in the lower part of the epidermis, forming nests. Immunohistochemistry indicated CD3+, CD4+, CD5+, CD7+, CD8+, CD30+, and Ki-67-positive staining. Additionally, CD20, CD79α, and PD-1 were negative. Monoclonal rearrangement of T-cells was identified in TCR β and TCR γ through clonality assessment. The diagnosis of limited paget-like reticulocyte hyperplasia was established, leading to surgical resection. A review of the literature affirmed the variable immunophenotype of pagetoid reticulosis, with atypical cells exhibiting four types: (1) CD3+, CD4+, CD8+-type; (2) CD3+, CD4-, CD8+-type; (3) CD3+, CD4-, CD8-type; and (4) CD3+, CD4+, CD8+-type—relatively uncommon in the restrictive type. This case report details the clinical features, histologic and morphologic characteristics, immunohistochemical phenotype, diagnosis, and differential diagnosis of a rare CD3+, CD4+, CD8+ limited pagetoid reticulosis. The lesion was surgically resected, and the patient underwent a 3-year follow-up to observe its prognosis.
Introduction
Pagetoid reticulosis (PR), an exceedingly rare variant of mycosis fungoides, manifests as a T-cell lymphoma with distinctive epidermotropic properties, initially documented by Woringer and Kolopp in 1937.Citation1 The ailment is categorized into two types: limited and disseminated. The former is characterized by isolated erythematous plaques, offering a more favourable prognosis, whereas the latter, less prevalent, exhibits multiple lesions and a relatively poorer prognosis.Citation2 Despite a similar histologic pattern between the two, limited pagetoid reticulosis typically presents as solitary, gradual-growing plaques on the extremities. Histologically, the spiny epidermis reveals infiltration by atypical lymphocytes forming pagetoid structures.Citation4 Pagetoid reticulosis exhibits a variable immunophenotype, with atypical cells falling into four categories: (1) CD3+, CD4+, CD8+-type; (2) CD3+, CD4-, CD8+-type; (3) CD3+, CD4-, CD8-type; and (4) CD3+, CD4+, CD8+-type, the latter being less common in the restricted type.Citation5 An intriguing case of PR is presented herein, featuring a rare immunophenotype characterized by CD4 and CD8 double-positive T cells with strong CD30 positivity. The report delves into the differential diagnosis of other primary cutaneous T-cell lymphomas with similar morphology and immunophenotypic profiles. The discussion highlights the significance of the CD4 CD8 double-positive phenotype in this context.
Table 1 Selected PR Series of Cases and Their Demographic, Clinical, and Pathologic Phenotypic Characteristics
Clinical Information
A 25-year-old woman presented with recurrent erythematous plaques on her right upper limb, persisting for a decade, accompanied by no notable itching. She self-administered various creams of unknown composition, yielding variable outcomes, seeking medical attention at our outpatient clinic six months ago. She had previously undergone unsuccessful treatment for ringworm. Initial diagnoses included common psoriasis and chronic eczema. The patient, physically fit and unmarried with no remarkable family history or drug allergies, denied any significant health issues.
Physical examination shows the patient exhibited an excellent general condition, with no abnormalities detected in the heart, lungs, or abdomen. Dermatologic examination revealed a flaky distribution of ring-shaped red plaques on the right lateral upper arm. These plaques, accompanied by small amounts of adhesive white scales, surrounded a larger area of well-demarcated hyperpigmentation spots.
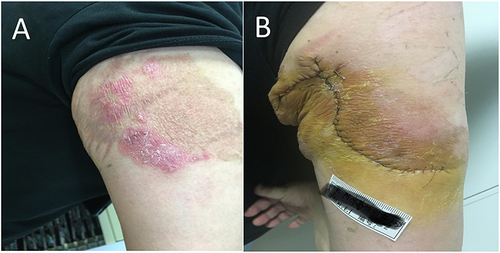
Additionally, stripes of atrophic lines were observed near the armpit (). Laboratory Tests show routine blood and urine stool tests were conducted, all of which returned average results. Total IgE levels were within the normal range. Tests for syphilis and HIV antibodies yielded negative results. Liver and kidney function, electrolytes, blood glucose, and lipid levels were also within normal limits. Chest CT scans showed no abnormalities.
Figure 1 (A) A well-defined semicircular red plaque surrounded by a large pigmented patch is present on the lateral aspect of the right upper arm. (B) Day 10 after surgical removal of skin lesions.
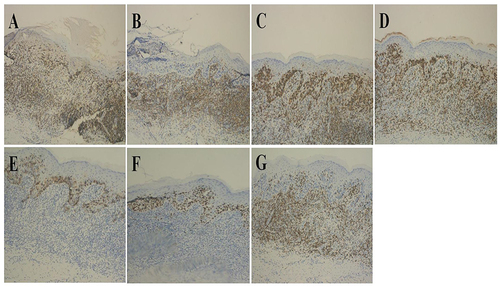
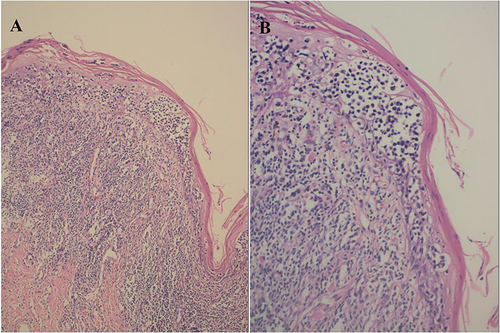
Histopathological examination shows that a skin biopsy of the right upper limb plaque revealed hyperkeratosis, mild epidermal thickening, and heterogeneous single-nucleated cells in the lower epidermis. These cells displayed large, deeply stained, irregular nuclei and perinuclear halos, aggregating into nests resembling Pautrier microabscesses. Banded lymphocytes and histiocytes were observed in the superficial dermal layer ( and ). Immunohistochemistry shows positive staining was observed for CD3, CD4, CD5, CD8, CD30, and Ki-67 (60%). CD7 showed partial positivity (), while PD-1, CD20, and CD79α were negative. T-cell clonality assessment confirmed monoclonal rearrangements in both TCR β and TCR γ, leading to the diagnosis of limited CD4, CD8 double-positive pagetoid reticulosis. The patient’s lesions were surgically excised, and a favourable recovery was observed post-surgery.
Figure 2 (A) Hyperkeratotic epidermis, mild epidermal thickening, and heterogeneous mononuclear cells in the lower epidermis (HE x100). (B) Cells with large, darkly stained, irregular nuclei with perinuclear halos aggregated into nests resembling Pautereum microabscesses. Banded lymphocytes and histiocytes were observed in the superficial dermis (HE x200).
Discussion
Pagetoid Reticulosis (PR), initially reported by Woringer and Kolopp in 1939, is classified into two types: limited (Woringer-Kolopp type) and disseminated (Ketron-Goodman type). Presently, the term PR exclusively refers to the former, characterized as a lazy form of T-cell lymphoma with a favourable prognosis.Citation1,Citation3 PR is typified by red or reddish-brown isolated plaques featuring elevated margins that tend to subside in the center, resulting in circular or arcuate lesions.Citation1,Citation6,Citation7 The skin surface may display hyperkeratosis or ulceration, with visible scales reminiscent of psoriasiform manifestations.Citation8–10 Typically developing at the extremities, PR progresses slowly and may involve localized regional lymph node enlargement.Citation11–13 In this case, the clinical presentation aligned with a psoriasis-like plaque exhibiting a semi-annular shape and hyperpigmentation after fading, located on the forearm—clinically consistent with typical PR manifestations. Atrophic lines in this patient were attributed to prolonged use of topical glucocorticoids. Additionally, hyperpigmented spots surrounding the lesions underwent pathological examination before surgery, revealing no infiltration of xenomorphic cells in the epidermis ().
Histopathologic features of Pagetoid Reticulosis (PR) are characterized by a prominent infiltration of Paget cells within the hyperplastic epidermis, distributed singly or in nests. The epidermis often exhibits hyperkeratosis and hyperkeratosis with hyperplasia and hypertrophy of the stratum spinosum. The subepidermis may show diffuse infiltration of single nucleated cells characterized by large size, dark nuclear staining, irregular morphology, perinuclear halos, and Pautrier’s microabscess-like aggregates. Occasionally, nuclear schizophrenic images may be evident. Reactive lymphocytes and histiocytes are observed in the dermis, with atypical cells sometimes present in this layer.Citation13 The immunophenotypes of pagetoid reticulosis display variability, with four main types identified: (1) CD3+, CD4+, CD8-; (2) CD3+, CD4-, CD8+; (3) CD3+, CD4-, CD8-; and (4) CD3+, CD4+, CD8+. The types of CD3+, CD4+, and CD8+ are less common in the restricted phenotype. High expression of CD30 (>50%) and Ki-67 (50%) is often observed.Citation14 In the reported case, the histologic pattern aligns with typical PR characteristics. However, it is a rare CD4(+) and CD8(+) type with a notably high Ki-67 proliferation index. An infrequent case of Woringer-Kolopp disease involving the right buttock region and extending to the lower thigh has been reported in a 27-year-old male patient. This case changed from an inert clinical behaviour to a locally invasive one during the disease course without dissemination features.Citation15 The widespread expression of CD30 and Ki-67 staining greater than 25% indicates that the cells have a moderate to high proliferation index.Citation16 Therefore, with the widespread expression of CD30 and 60% Ki-67 staining in this case, we speculate that CD4/CD8 double positivity may lead to a higher cell proliferation index, resulting in a transition of clinical manifestations from indolent to aggressive in such patients. However, few reported cases in the current literature having similar presentations. Overall, PR cases tend to have a benign course, with only 7% experiencing recurrence and a favorable prognosis.
The differential diagnosis for Pagetoid Reticulosis (PR) includes several conditions, such as palmoplantar mycosis fungoides (MF), primary epidermal CD8+ cytotoxic T-cell lymphoma, and cutaneous gamma/delta T-cell lymphoma.Citation17 Unlike palmoplantar MF, PR clinically presents with thicker, warty damage, and its tumor cells, distinctly cytoplasmic, differ from typical MF.Citation18 Palmoplantar MF infiltrates constant CD4+ T lymphocytes, while PR is immunophenotyped as CD8+ or CD4-/CD8- and CD4+, exclusively epidermotropic.Citation19 PR often displays high CD30 (up to 50%) and KI-67 (50%) expression, distinguishing it from MF’s CD30-negative and lower proliferation index.Citation20 Primary epidermal CD8+ cytotoxic T-cell lymphoma, marked by acute clinical onset, frequent rashes, and easily ulcerated plaques, can disseminate to viscera and has a poor prognosis.Citation21 Pathologically, it exhibits epidermal edema, blistering, and epidermotropic tumor cells expressing CD3, CD8, and cytotoxicity markers. Cutaneous gamma/delta T-cell lymphoma, a clinically aggressive and disseminated disease, contrasts with PR’s inert and slow-growing nature, which exhibits distinct epidermotropic and Paget features.Citation21 Histopathologically, PR requires differentiation from Paget’s, Bowen’s, and mycosis fungoides.Citation22 Paget’s disease is characterized by larger, richly stained Paget cells expressing epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA).Citation23 Bowen’s disease displays disorganized cells throughout the epidermis with atypical features, nucleoli, and dyskeratotic cells, while PR manifests abnormal cells in the lower epidermis without dyskeratotic cells.Citation24
The optimal treatment for localized PR is surgical excision, followed by radiotherapy (such as superficial X-ray irradiation or high-dose electron beam therapy).Citation25 Treatment options may include psoralen plus ultraviolet A (PUVA) therapy and delta-aminolevulinic acid photodynamic therapy (ALA-PDT).Citation12 Topical treatments such as fluorouracil cream, nitrogen mustard, or intralesional corticosteroid injections can also be used locally, although recurrence is possible.Citation26 For disseminated PR, a comprehensive approach, including surgery, radiotherapy, chemotherapy, and immunotherapy, should be considered.Citation27 Therefore, surgical excision was selected as the treatment options. The lesion appeared as an irregular semicircular brown patch with a size of 10*4 cm excised. Dressings were changed daily for the first 12 days postoperatively, followed by suture removal on the 12th day without applying topical medication. Skin healing progressed generally without complications. Pathological examination of the brown lesion revealed no abnormalities. After three years of follow-up, no evidence of disease recurrence exists. However, considering the relatively short follow-up period, continuous monitoring will be conducted.
Summary
The characteristic feature of this case is the immunohistochemical staining result showing CD4+/CD8+ phenotype, which is extremely rare. This phenotype may indicate a potential for indolent progression to aggressiveness. In the early stages, it is also prone to misdiagnosis as psoriasis or eczema. Therefore, when encountering such patients in the future, early tissue pathology and immunohistochemical examinations should be performed to strive for early diagnosis and treatment.
Ethics Statement
The publications of images were included in the patient’s consent for publication of the case. The Hospital Ethics Committees of the Fifth People’s Hospital of Hainan Province approved the publish the case details.
Consent Statement
The patient provided informed consent for the publication of the case.
Disclosure
Yunfang Zhang and Ming Zhang are the co-first authors of this study. Yuan Li and Huaji Wang are Co-corresponding authors for this study. The authors have no conflicts of interest to declare.
Additional information
Funding
References
- Osto M, Afify O, Musa A, Ahmed U, Rehman R, Mehregan D. Woringer-Kolopp disease (localized pagetoid reticulosis): a systematic review. Int J Dermatol. 2023;62(3):312–321. doi:10.1111/ijd.16224
- Pruksaeakanan C, Teyateeti P, Patthamalai P, Thumrongtharadol J. Primary Cutaneous Lymphomas in Thailand: A 10-Year Retrospective Study. Biomed Res Int. 2021;2021:4057661.
- Schukow C, Ahmed A. Dermatopathology, cutaneous lymphomas. 2023 Feb 16. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Jan 2024
- Stoll JR, Willner J, Oh Y, et al. Primary cutaneous T-cell lymphomas other than mycosis fungoides and Sézary syndrome. Part I: clinical and histologic features and diagnosis. J Am Acad Dermatol. 2021;85(5):1073–1090. doi:10.1016/j.jaad.2021.04.080
- Haghighi B, Smoller BR, LeBoit PE, Warnke RA, Sander CA, Kohler S. Pagetoid reticulosis (woringer-kolopp disease): an immunophenotypic, molecular, and clinicopathologic study. Mod Pathol. 2000;13(5):502–510. doi:10.1038/modpathol.3880088
- Morariu SH, Rotaru M, Vartolomei MD, et al. Pagetoid reticulosis Woringer-Kolopp type, a particular variant of mycosis fungoides: a case report. Rom J Morphol Embryol. 2014;55(4):1469–1472.
- Wang SC, Mistry N. Woringer-Kolopp disease mimicking psoriasis. CMAJ, 187 17 1310 doi: 10.1503/cmaj.141318.
- Gillihan R, Tran C, Fraga GR, Fischer R. Recalcitrant solitary erythematous scaly patch on the foot. Cutis. 2017;99(5):355.
- Torre-Castro J, Carrasco Santos L, Rodríguez-Pinilla SM, Requena L. Pagetoid reticulosis in a 13-year old female. A unique immunohistochemical profile. J Cutan Pathol. 2020;47(5):466–469. doi:10.1111/cup.13622
- Stahly S, Manway M, Lin CC, Sukpraprut-Braaten S. Pagetoid reticulosis: a rare dermatologic malignancy presenting in a middle-aged female. Cureus, 13 10 e18524 doi: 10.7759/cureus.18524.
- Nishikawa Y, Kanemaru S, Mori A, Nagano M, Mochida K, Amano M. Adult T-cell leukemia/lymphoma with pagetoid reticulosis-like skin lesions. Int J Dermatol. 2021;60(9):e342–e344. doi:10.1111/ijd.15446
- Miao Q, Xu X, Bu W, Chen H. A case of pagetoid reticulosis treated with topical photodynamic therapy. Photodiagnosis Photodyn Ther. 2022;37:102649. doi:10.1016/j.pdpdt.2021.102649
- Wei S, Huang W, Xu X. Pagetoid reticulosis positive for cytotoxic CD20 and CD30: a case report. Indian J Pathol Microbiol. 2019;62(2):316–318. doi:10.4103/IJPM.IJPM_717_18
- Mourtzinos N, Puri PK, Wang G, Liu ML. CD4/CD8 double negative pagetoid reticulosis: a case report and literature review. J Cutan Pathol. 2010;37(4):491–496. doi:10.1111/j.1600-0560.2009.01323.x
- Zengin AY, Topkan E, Cimsit G, Yildiz K. Woringer-Kolopp disease coexpressing CD4 and CD8 treated with radiation therapy: a case report. Tumori Journal. 2008;94(5):754–757. doi:10.1177/030089160809400521
- Jacyk WK, Grayson W, Dinkel JE, Requena L. Pagetoid reticulosis with CD30 positivity and cytotoxic/suppressor cells. J Cutan Pathol. 2007;34(8):644–647. doi:10.1111/j.1600-0560.2006.00698.x
- Steffen C. Ketron-Goodman disease, woringer-kolopp disease, and pagetoid reticulosis. Am J Dermatopathol. 2005;27(1):68–85. doi:10.1097/01.dad.0000144160.26647.ab
- Skiljevic D, Bogdanovic Z, Vesic S, Vukicevic-Sretenovic J, Gajic-Veljic M, Medenica L. Pagetoid reticulosis of Woringer-Kolopp. Dermatol Online J. 14(1):18.
- Bouhassoun N, Leteurtre E, Delaporte E, Piette F, Martin De Lassalle E, Lecomte-Houcke M. Cas anatomoclinique de maladie de Woringer et Kolopp. Intérêt de l’étude immunohistochimique [A case study of Woringer-Kolopp disease Immunohistochemical study]. Ann Pathol. 2000;20(4):373–376.
- Corbeddu M, Ferreli C, Pilloni L, Faa G, Cerroni L, Rongioletti F. Pagetoid reticulosis (Woringer-Kolopp disease) in a 2-year-old girl-Case report and review of the literature. JAAD Case Rep, 5 1 104–107 doi: 10.1016/j.jdcr.2018.10.023.
- Haneke E, Tulusan AH, Weidner F. Histological features of ”pagetoid reticulosis” (Woringer-Kolopp) in pre-mycosis fungoides. Arch Dermatol Res. 1977;258(3):265–273. doi:10.1007/BF00561129
- Martínez-Escala ME, González BR, Guitart J. Mycosis Fungoides Variants. Surg Pathol Clin. 2014;7(2):169–189. doi:10.1016/j.path.2014.02.003
- Sergeev I, Molochkov VA, Galil-Ogly GA, Bershchanskaia AM, Paklina OV. Pedzhetoidnyĭ retikulez [Pagetoid reticulosis]. Arkh Patol. 2001;63(4):54–56.
- Mendese GW, Beckford A, Krejci N, Mahalingam M, Goldberg L, Gilchrest BA. Pagetoid reticulosis in a prepubescent boy successfully treated with photodynamic therapy. Clin Exp Dermatol. 2012;37(7):759–761. doi:10.1111/j.1365-2230.2012.04352.x
- Su O, Dizman D, Onsun N, et al. Treatment of localized pagetoid reticulosis with imiquimod: a case report and literature review. J Eur Acad Dermatol Venereol. 2016;30(2):324–326. doi:10.1111/jdv.12718
- Kaufmann F, Kettelhack N, Hilty N, Kempf W. Unilesional plantar mycosis fungoides treated with topical photodynamic therapy - case report and review of the literature. J Eur Acad Dermatol Venereol. 2017;31(10):1633–1637. doi:10.1111/jdv.14160
- Wang T, Liu YH, Zheng HY. Localized pagetoid reticulosis (Woringer-Kolopp disease) completely response to NB-UVB combined with IFN. Dermatol Ther. 2014;27(4):227–229.