Abstract
The role of light-based technologies in dermatology has expanded dramatically in recent years. Lasers and intense pulsed light have been used to safely and effectively treat a diverse array of cutaneous conditions, including vascular and pigmented lesions, tattoos, scars, and undesired hair, while also providing extensive therapeutic options for cosmetic rejuvenation and other dermatologic conditions. Dermatologic laser procedures are becoming increasingly popular worldwide, and demand for them has fueled new innovations and clinical applications. These systems continue to evolve and provide enhanced therapeutic outcomes with improved safety profiles. This review highlights the important roles and varied clinical applications that lasers and intense pulsed light play in the dermatologic practice.
Laser and intense pulsed light principles
Laser is an acronym, which represents light amplification by the stimulated emission of radiation. An understanding of the fundamental properties of laser light is essential to appreciate its clinical effects on the skin.Citation1,Citation2 First, laser light is monochromatic, meaning that the emitted light is composed of a single wavelength. This is determined by the medium of the laser system through which the light passes. Second, laser light is coherent – traveling in phase spatially and temporally. Third, laser light is collimated – emitted in a parallel manner with minimal divergence.
Laser light may be absorbed, reflected, transmitted, or scattered when applied to the skin. In order for a clinical effect to occur, light must be absorbed by tissue. Absorption of laser light is determined by chromophores – the target molecules found in the skin, which have specific wavelength absorption profiles. The three primary endogenous cutaneous chromophores are water, melanin, and hemoglobin; whereas tattoo ink represents an exogenous chromophore. Upon absorption of laser energy by the skin, photothermal, photochemical, or photomechanical effects may occur. The cutaneous depth of penetration of laser energy is dependent upon absorption and scattering. In the epidermis, there is minimal light scattering, whereas in the dermis there is significant scatter due to the high concentration of collagen fibers. The amount of scattering of laser energy is inversely proportional to the wavelength of light. The depth of laser energy increases with wavelength until the mid-infrared region of the electromagnetic spectrum, at which point dermal penetration becomes more superficial due to increased absorption within tissue water.
The theory of selective photothermolysis proposed by Anderson and ParrishCitation3 in 1983 has been pivotal in the advancement of laser surgery. It explains the mechanism by which controlled destruction of a cutaneous target can be achieved without significant injury to surrounding tissue. Three principles are crucial to the process. First, an appropriate wavelength should be employed that can be absorbed preferentially by the targeted tissue chromophore. Second, the pulse duration of the laser must be shorter than the chromophore’s thermal relaxation time, which is the time required for the target to lose half of its peak temperature following irradiation. Third, the fluence (or energy) must be sufficient to achieve destruction of the target within the appropriate time interval. These factors guide the selection of lasers and intense pulsed light (IPL) appropriate for a specific skin target or lesion.
Lasers can be further classified by their mode of light emission. Continuous wave (CW) lasers produce a continuous beam of light with long exposure durations that can cause nonselective tissue damage. Quasi-CW mode produces interrupted emissions of constant laser energy by shuttering the CW beam into short intervals. Pulsed laser systems emit high-energy laser light in ultrashort pulse durations with relatively long interpulse time intervals. They can be long pulsed (LP) or very short pulsed such as the quality-switched (QS) nanosecond and picosecond laser systems.
IPL is a nonlaser filtered flash lamp device. Unlike lasers, IPL devices emit polychromatic, noncoherent, and noncollimated light (420–1,400 nm) with varying pulse durations. The wider range of light can be absorbed by a variety of chromophores, making IPL less selective than lasers. As such, cutoff filters are often used to narrow the spectrum of emitted wavelengths and render the device more specific.
Treatment of vascular lesions
Vascular lesions are frequently treated with lasers and IPL due to the systems’ ability to specifically target intravascular oxyhemoglobin. This endogenous chromophore has three primary absorption peaks within the visible light spectrum: 418, 542, and 577 nm. Oxyhemoglobin absorbs the laser light, which is subsequently converted to heat and transferred to the vessel wall causing coagulation and vessel closure. Treatment with vascular-specific lasers causes inhomogeneous heating within dermal blood vessels due to their varying sizes, but results in effective and efficient treatment of small- and large-diameter blood vessels.Citation4 Historically, multiple laser systems were shown to be effective in the treatment of vascular lesions, but several fell out of favor due to high rates of adverse effects. The most commonly used vascular lasers in current clinical practice are the potassium titanyl phosphate (KTP, 532 nm), pulsed dye laser (PDL, 585–595 nm), alexandrite (755 nm), diode (800–810, 940 nm), and neodymium-doped yttrium aluminum garnet (Nd:YAG, 532 and 1,064 nm). In addition, IPL with appropriate filters can be used to treat certain vascular lesions.Citation5
The KTP laser is effective in the treatment of numerous superficial vascular lesions, particularly facial telangi-ectasias.Citation6,Citation7 Treatments are well tolerated and adverse effects include erythema, edema, and crusting. One of the advantages of the KTP laser is that postoperative purpura and erythema are minimized. Its shorter wavelength results in decreased tissue penetration and limited absorption by hemoglobin in deeper vessels. Given that there is considerable absorption of 532 nm energy by melanin, caution must be exercised when treating patients with darker skin.
The PDL is a highly effective laser for the treatment of a wide range of vascular lesions and is considered the workhorse vascular laser in many practices due to its favorable clinical efficacy and low risk profile. The PDL has successfully been used to treat port-wine stains,Citation8–Citation17 facial telangiectasias,Citation18–Citation20 hemangiomas,Citation21–Citation25 pyogenic granulomas,Citation26 Kaposi’s sarcoma,Citation27 and poikiloderma of Civatte.Citation28 In addition, PDL is highly effective in the treatment of hypertrophic and keloid scars,Citation29–Citation31 striae distensae,Citation32,Citation33 verrucae,Citation34,Citation35 angiofibromas,Citation36 lymphangiomas, and many other dermatologic conditions.Citation37–Citation49 Fluences ranging 5–10 J/cm2 using 3–10 mm spot sizes with a minimal to no pulse overlap reduces unwanted thermal injury. Adverse effects include postoperative purpura, transient dyspigmentation, and rarely vesiculation, crusting, and scarring. Newer PDLs with longer wavelengths and extended pulse durations have enabled deeper tissue penetration and improved clinical outcomes ().
Figure 1 Facial erythema and prominent telangiectasias in a patient with rosacea before (A) and after two 595 nm pulsed dye laser (PDL) treatments (B).

IPL has also been used to effectively treat a variety of vascular lesions, including facial telangiectasias, capillary malformations, poikiloderma of Civatte, venous malformations, and infantile hemangiomas.Citation5,Citation50–Citation52 Its noncoherent light emits wavelengths ranging from 420 to 1,400 nm. Filters are used to limit the wavelengths emitted by the device in order to improve dermal penetration and minimize absorption of energy by other chromophores. IPL energy is delivered as a series of single, double, or triple pulse sequences with pulse durations of 2–25 milliseconds and interpulse delays of 10–500 milliseconds. Longer pulse durations are used to more effectively heat deeper vessels, thereby reducing the risk of purpura and hyperpigmentation.
Prominent leg veins are a common cosmetic concern and can be challenging to treat. Sclerotherapy is highly effective for leg veins and is considered the gold standard treatment; however, it can be associated with significant adverse effects such as ulceration, allergic reactions, and telangiectatic matting.Citation53,Citation54 The KTP and PDL lasers as well as IPL have shown efficacy in the treatment of small vessels measuring <1 mm.Citation55–Citation57 The treatment of larger and/or deeper vessels requires longer wavelengths and pulse durations. The LP alexandrite (755 nm), diode (800 nm), and Nd:YAG (1,064 nm) lasers have each been successful in eradicating small- to medium-sized veins.Citation57–Citation59
Treatment of hypertrophic scars, keloids, and striae
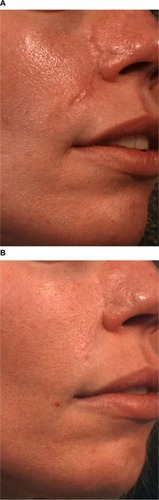
Hypertrophic scars and keloids are abnormal wound responses to cutaneous injury and are marked by excessive collagen formation. They are difficult to treat and have high recurrence rates following conventional treatments such as surgical excision, dermabrasion, radiation, and intralesional therapy.Citation60–Citation62 Many studies have been published in which scars treated with PDL resulted in improvement in erythema, texture, pliability, and pain, with minimal side effects.Citation29–Citation31,Citation63 Significant clinical improvement of hypertrophic scars is often observed after one or two PDL treatments, with greatest responses observed with the use of lower energy densitiesCitation64 (). Adjunctive therapies to PDL such as intralesional corticosteroids or 5-fluorouracil are most useful for resistant keloids and/or actively proliferating hypertrophic scars.Citation65,Citation66 Adverse effects after PDL treatment are mild and include purpura that typically dissipates in several days and temporary dyspigmentation that resolves spontaneously over time. More recently, ablative fractional lasers have been shown to improve hypertrophic scars and are often combined with topical delivery of corticosteroids for improved efficacy.Citation67,Citation68
Figure 2 Hypertrophic and erythematous surgical scar before (A) and after two pulsed dye laser (PDL) treatments (B).
Striae distensae are common atrophic lesions that are often associated with obesity, pregnancy, puberty, and exogenous steroid use. They initially present as slightly erythematous to pink atrophic bands, termed striae rubra. They gradually become hypopigmented and fibrotic and are referred to as striae alba. Striae have been treated successfully with low-fluence PDL, with stria rubra showing greater clinical response to treatment than mature striae alba.Citation32,Citation63 Fractional ablative and nonablative lasers have also been shown to improve the pigmentation and texture of striae distensae.Citation69,Citation70
Treatment of pigmented lesions
Cutaneous pigmented lesions are frequent targets of laser and IPL treatment. QS lasers are highly effective in lightening or eliminating benign epidermal and dermal pigmented lesions such as solar lentigines, ephelides, café au lait macules, seborrheic keratoses, melanocytic nevi, blue nevi, nevi of Ota/Ito, infraorbital hyperpigmentation, drug-induced hyperpigmentation, Becker’s nevi, and nevi spilus. These same lasers have also been used to treat amateur, professional, and traumatic tattoos. The red and infrared wavelengths of the QS lasers target melanin within melanosomes (as is the case with pigmented lesions) and various carbon-based material or organometallic dyes (as is the case with tattoos), with limited injury to adjacent normal tissue.Citation71 A variety of different lasers (including CW and quasi-CW systems) have been used to treat pigmented lesions in the past; however, they are not currently in wide use due to significant risk of scarring and dyspigmentation.Citation72–Citation74 The short pulsed QS and picosecond systems commonly used to treat pigmented lesions and tattoos today include Nd:YAG (532 and 1,064 nm), ruby (694 nm), and alexandrite (755 nm) lasers.
The QS ruby was the first system developed to treat pigmented lesions and tattoos and was widely and successfully used;Citation75–Citation82 however, its 694 nm wavelength required caution in patients with darker skin tones due to its energy being so strongly absorbed by melanin with a greater risk of hypopigmentation.Citation83,Citation84 The subsequent development of QS alexandrite and Nd:YAG lasers were also shown to effectively treat pigmented lesions and tattoos with the advantage that their longer wavelengths could safely treat darker skin and penetrate into the deeper dermis.Citation85–Citation100 Most recently, Q-switched lasers that generate picosecond domain pulses have been commercially introduced with an even greater ability to target and destroy cutaneous pigment and inkCitation101 ().
Effective tattoo removal necessitates the use of an appropriate wavelength that is preferentially absorbed by the specific ink color within the tattoo.Citation102 Black pigment absorbs wavelengths from red through the infrared spectrum and can thus be treated with QS ruby, QS alexandrite, or QS Nd:YAG lasers. The QS ruby or alexandrite lasers can safely target blue and green inks since these pigments absorb in the 600–800 nm range, whereas only the 532 nm QS Nd:YAG laser can clear red, orange, and yellow inks. Cosmetic tattoo inks that are typically tan, white, or rust colored are difficult to treat because they frequently contain iron oxide and titanium dioxide compounds that undergo a chemical reaction upon laser irradiation to a black and insoluble form (ferric oxide to ferrous oxide).Citation103 Professional tattoos are more difficult and require additional sessions to eliminate than amateur tattoos, given the dense dermal concentration of ink in the former. Adverse effects of laser tattoo removal include transient pigmentary alteration (hypo- and hyperpigmentation), systemic allergic or localized granulomatous tissue reactions, ignition of explosive particles in traumatic tattoos, and atrophic scars.Citation104,Citation105
IPL devices have also been used to treat benign pigmented lesions including ephelides and solar lentigines, with significant lesional improvement observed after a series of monthly treatments.Citation106–Citation108 They are relatively ineffective in the treatment of tattoos because of their inability to deliver short pulses that can target and pulverize ink particles.
Hair removal
Safe and long-lasting hair reduction in cosmetically undesirable locations can be achieved with a variety of lasers and IPL devices. These systems emit red and infrared light with wavelengths ranging 600–1,200 nm, which are capable of targeting melanin in the hair shaft, follicular epithelium, and hair matrix.Citation109–Citation111 Since melanin is also normally present in the epidermis, it presents as another competing source for laser energy absorption and can lead to undesirable epidermal damage. Concomitant epidermal cooling sources help to minimize unwanted thermal injury (particularly in patients with darker skin) during treatment. While pulse durations of 10–100 milliseconds are typically used (in keeping with the thermal relaxation time of most hair follicles), the biological target in laser hair removal is the follicular stem cell, which is located in the bulge region or dermal papilla of the hair follicle. Since these stem cells do not always contain significant amounts of melanin and may not be directly adjacent to the targeted pigmented structures, longer pulse durations than those outlined are often necessary for heat diffusion from the follicular shaft to the desired end-target.Citation112 Permanent hair reduction without significant adverse effects has been achieved despite the use of prolonged pulse durations.Citation113
LP ruby (694 nm), alexandrite (755 nm), diode (800 nm), and Nd:YAG (1,064 nm) lasers as well as IPL (590–1,200 nm) have been shown, through numerous published studies, to achieve long-lasting hair reduction with a low incidence of adverse effects.Citation110,Citation114–Citation128 The optimal laser or IPL selection is determined by the patient’s skin type. The LP ruby laser is best used in pale-skinned patients with Fitzpatrick skin phototypes I–III,Citation114 whereas the LP alexandrite and diode lasers can be safely used in individuals with slightly darker skin (Fitzpatrick skin phototypes I–IV). The LP Nd:YAG laser system is considered the safest option for darker skinned patients due to the decreased risk of epidermal injury by its longer wavelength.Citation129 Using specific cutoff filters, the IPL system can also be used for hair reduction in patients with paler skin. While significant hair reduction can be seen after one treatment, multiple treatment sessions at monthly time intervals improves the clinical outcome.Citation125,Citation126 Adverse effects after laser or IPL treatments include blistering, crusting, dyspigmentation, and rarely scarring. It is important to select the appropriate laser system with correct treatment parameters and caution should be exercised in patients with tans or intrinsically dark skin.
Ablative laser resurfacing
Laser skin resurfacing has evolved significantly over the past 2 decades. It was first popularized in the mid-1990s following the introduction of the pulsed carbon dioxide (CO2) laser system for the treatment of facial rhytides and atrophic acne scars.Citation130 The 10,600 nm wavelength emitted by a CO2 laser is absorbed by intracellular water, resulting in tissue heating and vaporization. The pulsed CO2 laser produces discrete areas of tissue vaporization while minimizing thermal injury to surrounding tissue that can be associated with scarring and hypopigmentation. Subsequent to the development of the pulsed and scanned CO2 laser systems, the erbium-doped yttrium aluminum garnet (Er:YAG) laser was introduced. Its 2,940 nm wavelength also resulted in controlled skin ablation with minimal thermal injury. Because the Er:YAG system creates little thermal reaction in the skin, tissue tightening is not as dramatic as that seen after CO2 laser treatment. On the other hand, the minimal thermal injury created by Er:YAG laser irradiation leads to quicker postoperative healing and fewer side effects.
While numerous cosmetic applications of pulsed and scanned CO2 and Er:YAG ablative lasers have been reported, they have been most frequently used for facial rejuvenation of photodamaged skin, including rhytides and dyschromia.Citation131–Citation138 Atrophic acne and traumatic scars also can be effectively treated with ablative lasers.Citation139,Citation140 Impressive skin tightening has been demonstrated with CO2 laser skin resurfacing due to the thermal effect on dermal collagen.Citation141,Citation142 Ablative lasers have been successfully used to treat verrucae vulgaris, seborrheic keratosis, syringoma, xanthelasma, onychodystrophy, actinic keratosis, and Zoon’s balanitis among other dermatologic conditions.Citation143–Citation145
While extremely effective, prolonged side effects and complications associated with ablative laser resurfacing were reported.Citation146–Citation150 Frequently encountered posttreatment reactions include intense erythema and edema, which can persist for several weeks to months.Citation148 Milia and acne can be experienced, particularly in individuals with a previous history of acne and in treatment of scars.Citation147 Infections are relatively uncommon, but patients with a history of herpes labialis should receive prophylactic oral antiviral therapy to reduce the incidence of latent herpes reactivation.Citation151,Citation152 Postinflammatory hyperpigmentation occurs not infrequently, particularly in patients with darker skin tones or after aggressive laser treatment.Citation153 Delayed hypopigmentation is far less common – typically observed several months (>6 months) after treatmentCitation147 and develops more frequently with CO2 laser ablation than with Er:YAG. Hypertrophic scarring is another infrequent complication that can result from aggressive laser technique, infection, and poor wound management. Rarely seen is ectropion formation, which can occur when lax periocular skin is vaporized in patients with a previous history of lower blepharoplasty.
Nonablative laser resurfacing
Nonablative laser systems were developed primarily to reduce the risk of adverse effects and the extensive postoperative recovery period associated with ablative laser resurfacing. There are several nonablative laser and IPL devices, most of which emit infrared light. They include the Nd:YAG (1,064 and 1,320 nm), diode (980 and 1,450 nm), erbium: glass (Er:glass, 1,540 nm), and IPL (500–1,200 nm) systems. Similar to ablative lasers, they primarily target dermal water, which causes collagen heating and dermal remodeling. Unlike their ablative counterparts; however, epidermal injury and tissue vaporization does not occur due to the concomitant application of epidermal cooling. Clinical applications of nonablative lasers include facial and nonfacial rhytides and scars.Citation154–Citation157 Treatments are typically performed in a series of three or more monthly sessions to achieve optimal clinical results.Citation154–Citation157 Because the epidermis is spared from damage, nonablative lasers can be safely used on nonfacial skin and are associated with speedier recovery and lower incidence of postoperative side effects compared with ablative lasers. Posttreatment erythema and edema resolve within 24–48 hours, which is typical, but other significant side effects are rare. Blister formation is an uncommon complication stemming from insufficient epidermal cooling.
Fractional laser skin resurfacing
Fractional photothermolysis was introduced in 2004,Citation158 thereby revolutionizing laser skin resurfacing. Fractional laser systems target tissue water and produce microscopic treatment zones of controlled width, depth, and densities in the skin. These three-dimensional thermal damage zones are referred to as “microscopic thermal zones” (MTZs) and are the fundamental units of fractional photothermolysis. In contrast to full-field resurfacing, only a fraction of the skin is removed. The energy in the fractionated columns of the laser induces thermal damage without affecting neighboring tissue. Adjacent unaffected tissue serves as a source for healing and rapid epidermal repair via migration. The targeted damage with MTZ stimulates neocollagenosis and collagen remodeling.Citation159,Citation160 As a result, fractionated photothermolysis minimizes the risk of complications and reduces recovery times seen with the aforementioned resurfacing lasers. Fractional technology has been applied to both ablative and nonablative laser systems. Ablative fractional lasers produce MTZ of epidermal and dermal tissue vaporization, whereas nonablative fractional lasers induce epidermal and dermal coagulation without tissue vaporization.
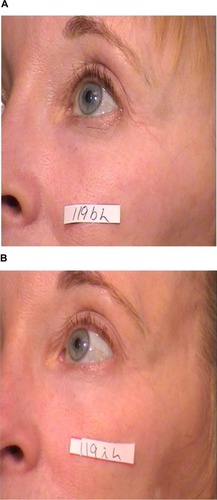
Several nonablative fractional lasers are commercially available, including Nd:YAG (1,440 nm), diode (1,440 nm), erbium (1,410, 1,540, and 1,550 nm), and thulium (1,927 nm) laser systems. These lasers are frequently used for the treatment of facial and nonfacial rhytides, dyschromia, and scars. Although facial skin treatments result in superior clinical outcomes, nonfacial skin treatments are also impressive. Clinical studies have demonstrated significant improvement of facial rhytides, atrophic acne scars, hypertrophic scars, and enlarged pores when treated with various nonablative fractional lasersCitation161–Citation168 (). The successful treatment of melasma with nonablative lasers has been less consistent.Citation169,Citation170
Figure 4 Periocular rhytides before (A) and after three nonablative fractionated erbium (1,550 nm) laser treatments (B).
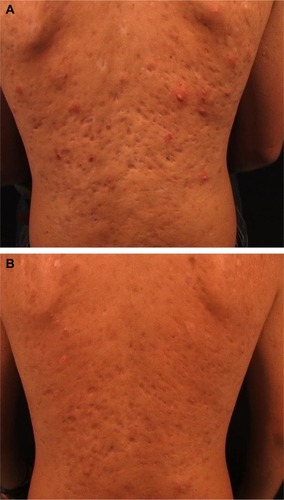
The ablative CO2 and Er:YAG fractionated lasers are both highly effective in the treatment of photoaged skin and yield similar clinical efficacy and rapid recovery.Citation171–Citation173 Ablative fractionated lasers have also been used to successfully treat acne scars, including severe scars on a variety of anatomic locationsCitation174,Citation175 (). Treatments are typically performed as a single procedure due to their robust clinical results compared with nonablative fractional lasers.
Figure 5 Severe atrophic acne scars on the back of a young man before (A) and 6 months after one ablative fractionated carbon dioxide (CO2) laser treatment (B).
Although fractionated ablative and nonablative lasers have a superior safety profile compared with their nonfractionated counterparts, side effects and complications can still occur. Patients often encounter posttreatment erythema and edema following nonablative fractional resurfacing that typically resolve within 3 days.Citation176 Erythema that extends beyond 4 days is considered prolonged and is reported in <1% of patients. In contrast, erythema that lasts beyond 1 month following ablative fractional laser treatment is considered prolonged and is seen in ~12.5% of patients.Citation177 A 590 nm light-emitting diode system has been shown to reduce post-fractional laser erythema.Citation178 Herpes simplex virus infection is the most common infectious complication following fractionated laser treatment, affecting up to 2% of patients.Citation177 It is generally recommended to treat patients prophylactically if they have a history of facial herpes simplex virus or if perioral laser treatment is performed. Bacterial infection is comparatively low with an incidence of 0.1%.Citation177 Antibacterial prophylaxis can be useful prior to ablative fractionated laser resurfacing. In addition, transient acneiform eruptions can develop following fractionated laser resurfacing in up to 10% of patients, especially those with a history of acne.Citation177 Moderate-to-severe acne flares can be treated with a short course of tetracycline-based antibiotics. Milia also develop in approximately 20% of treated patients and can be minimized by avoiding occlusive emollients.Citation177 Postinflammatory hyperpigmentation is another possible complication, although less frequently encountered when compared with nonfractional lasers. The incidence can be >12% in patients with darker phototypes (III–VI).Citation179 Delayed-onset hypopigmentation, hypertrophic scarring, and the development of vertical and horizontal bands are extremely rare complications of ablative fractional resurfacing.Citation180–Citation182
Laser phototherapy
The effective treatment of a variety of dermatologic diseases with ultraviolet (UV) phototherapy has long been established. Psoriasis has been treated with broadband and narrowband UVB light as well as psoralen with UVA for decades with significant clinical response. The xenon chloride excimer laser (308 nm) has been used to treat psoriasis as well, demonstrating clearing of psoriatic plaques with fewer treatments than narrow-band UVB treatment.Citation183–Citation186 One of the significant advantages of the excimer laser is that it targets only affected areas of skin, thereby preventing unnecessary exposure of normal tissue to UV radiation. Numerous studies have shown the clinical efficacy of the excimer laser for the treatment of various forms of psoriasis, including a multicenter study which demonstrated that 84% of patients reached 75% improvement or better after 10 or fewer treatments.Citation184 Treatments are often well tolerated, but adverse effects include blistering, erythema, and hyperpigmentation. Although clinically effective, treatment limitations include relative expense of therapy, time constraints when faced with large surface areas of psoriasis, and unknown risk of carcinogenesis.
The excimer laser has also been found to be as effective as narrow-band UVB in the treatment of vitiligo, with studies demonstrating greater than 75% repigmentation in patches of vitiligo after treatment.Citation187 These significant response rates are achieved in a relatively short treatment time period compared with traditional phototherapy.Citation188 Other conditions that have shown clinical response to the excimer laser include atopic dermatitis, alopecia areata, allergic rhinitis, folliculitis, granuloma annulare, lichen planus, mycosis fungoides, palmoplantar pustulosis, pityriasis alba, CD30+ lymphoproliferative disorder, leukoderma, prurigo nodularis, localized scleroderma, and genital lichen sclerosus.Citation189
Conclusion
Laser and IPL systems have diverse clinical applications throughout the field of dermatology and are constantly evolving. These technologies have facilitated the treatment of benign vascular and pigmented lesions, unwanted hair, tattoos, hypertrophic scars, keloids, rhytides, as well as dermatologic diseases such as psoriasis and vitiligo. Laser resurfacing, including ablative and nonablative fractional treatments have yielded excellent cosmetic results with improved safety profiles and recovery. Refinement of existing devices and the development of novel technologies will continue to expand the role of lasers and IPL in the future and enable practitioners to deliver the most cutting-edge and sophisticated treatments for a wider range of cutaneous conditions.
Disclosure
The authors report no conflicts of interest in this work.
References
- TanziELLuptonJRAlsterTSLasers in dermatology: four decades of progressJ Am Acad Dermatol2003491131 quiz 31–3412833005
- AndersonRRParrishJAThe optics of human skinJ Invest Dermatol198177113197252245
- AndersonRRParrishJASelective photothermolysis: precise microsurgery by selective absorption of pulsed radiationScience198322045965245276836297
- AstafyevaLGGadeRSchmidtWDLednevaGPWollinaUFasslerDLaser heating of biological tissue with blood vessels: modeling and clinical trialsOpt Spectrosc20061005789796
- WatHWuDCRaoJGoldmanMPApplication of intense pulsed light in the treatment of dermatologic disease: a systematic reviewDermatol Surg201440435937724495252
- WestTBAlsterTSComparison of the long-pulse dye (590–595 nm) and KTP (532 nm) lasers in the treatment of facial and leg telangiectasiasDermatol Surg19982422212269491116
- BecherGLCameronHMoseleyHTreatment of superficial vascular lesions with the KTP 532-nm laser: experience with 647 patientsLasers Med Sci201429126727124401943
- DoverJSGeronemusRSternRSO’HareDArndtKADye laser treatment of port-wine stains: comparison of the continuous-wave dye laser with a robotized scanning device and the pulsed dye laserJ Am Acad Dermatol1995322 Pt 12372407829709
- TanOTSherwoodKGilchrestBATreatment of children with port-wine stains using the flashlamp-pulsed tunable dye laserN Engl J Med198932074164212913507
- AlsterTTanOTLaser treatment of benign cutaneous vascular lesionsAm Fam Physician19914425475541858611
- AlsterTSWilsonFTreatment of port-wine stains with the flashlamp-pumped pulsed dye laser: extended clinical experience in children and adultsAnn Plast Surg19943254784848060071
- FitzpatrickRELoweNJGoldmanMPBordenHBehrKLRuiz-EsparzaJFlashlamp-pumped pulsed dye laser treatment of port-wine stainsJ Dermatol Surg Oncol199420117437487962935
- KauvarANGeronemusRGRepetitive pulsed dye laser treatments improve persistent port-wine stainsDermatol Surg19952165155217773599
- SommerSSheehan-DareRAPulsed dye laser treatment of port-wine stains in pigmented skinJ Am Acad Dermatol200042466767110727315
- WaldorfHAAlsterTSMcMillanKKauvarANGeronemusRGNelsonJSEffect of dynamic cooling on 585-nm pulsed dye laser treatment of port-wine stain birthmarksDermatol Surg19972386576629256912
- ShiWWangJLinYTreatment of port wine stains with pulsed dye laser: a retrospective study of 848 cases in Shandong Province, People’s Republic of ChinaDrug Des Devel Ther2014825312538
- AlsterTSTanziELCombined 595-nm and 1,064-nm laser irradiation of recalcitrant and hypertrophic port-wine stains in children and adultsDermatol Surg2009356914918 discussion 918–91919397657
- LoweNJBehrKLFitzpatrickRGoldmanMRuiz-EsparzaJFlash lamp pumped dye laser for rosacea-associated telangiectasia and erythemaJ Dermatol Surg Oncol19911765225251828257
- Ruiz-EsparzaJGoldmanMPFitzpatrickRELoweNJBehrKLFlash lamp-pumped dye laser treatment of telangiectasiaJ Dermatol Surg Oncol19931911100010038245298
- JasimZFWooWKHandleyJMLong-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical thresholdDermatol Surg2004301374014692924
- AshinoffRGeronemusRGCapillary hemangiomas and treatment with the flash lamp-pumped pulsed dye laserArch Dermatol199112722022051990985
- GardenJMBakusADPallerASTreatment of cutaneous hemangiomas by the flashlamp-pumped pulsed dye laser: prospective analysisJ Pediatr19921204 Pt 15555601552392
- PoetkeMPhilippCBerlienHPFlashlamp-pumped pulsed dye laser for hemangiomas in infancy: treatment of superficial vs mixed hemangiomasArch Dermatol2000136562863210815856
- ShenLZhouGZhaoJPulsed dye laser therapy for infantile hemangiomas: a systemic review and meta-analysisQJM2015108647348025376585
- KwonSHChoiJWByunSYEffect of early long-pulse pulsed dye laser treatment in infantile hemangiomasDermatol Surg201440440541124460784
- GoldbergDJScialesCWPyogenic granuloma in children. Treatment with the flashlamp-pumped pulsed dye laserJ Dermatol Surg Oncol199117129609621960269
- MarchellNAlsterTSSuccessful treatment of cutaneous Kaposi’s sarcoma by the 585-nm pulsed dye laserDermatol Surg199723109739759357509
- WheelandRGApplebaumJFlashlamp-pumped pulsed dye laser therapy for poikiloderma of CivatteJ Dermatol Surg Oncol199016112162299018
- AlsterTSImprovement of erythematous and hypertrophic scars by the 585-nm flashlamp-pumped pulsed dye laserAnn Plast Surg19943221861908192370
- AlsterTSWilliamsCMTreatment of keloid sternotomy scars with 585 nm flashlamp-pumped pulsed-dye laserLancet19953458959119812007739306
- AlsterTSNanniCAPulsed dye laser treatment of hypertrophic burn scarsPlast Reconstr Surg19981026219021959811021
- McDanielDHAshKZukowskiMTreatment of stretch marks with the 585-nm flashlamp-pumped pulsed dye laserDermatol Surg19962243323378624657
- JimenezGPFloresFBermanBGunja-SmithZTreatment of striae rubra and striae alba with the 585-nm pulsed-dye laserDermatol Surg200329436236512656814
- TanOTHurwitzRMStaffordTJPulsed dye laser treatment of recalcitrant verrucae: a preliminary reportLasers Surg Med19931311271378426521
- KauvarANMcDanielDHGeronemusRGPulsed dye laser treatment of wartsArch Fam Med1995412103510407496552
- HoffmanSJWalshPMorelliJGTreatment of angiofibroma with the pulsed tunable dye laserJ Am Acad Dermatol1993295 Pt 17907918227558
- WeingoldDHWhitePFBurtonCSTreatment of lymphangioma circumscriptum with tunable dye laserCutis19904553653662357907
- AlsterTSWilsonFFocal dermal hypoplasia (Goltz’s syndrome). Treatment of cutaneous lesions with the 585-nm flashlamp-pumped pulsed dye laserArch Dermatol199513121431447857109
- AlsterTSInflammatory linear verrucous epidermal nevus: successful treatment with the 585 nm flashlamp-pumped pulsed dye laserJ Am Acad Dermatol1994313 Pt 15135148077487
- HandrickCAlsterTSLaser treatment of atrophoderma vermiculataJ Am Acad Dermatol200144469369511260551
- TanziEAlsterTSPulsed dye laser treatment of multiple eccrine hidrocystomas: a novel approachDermatol Surg2001271089890011722530
- CliffSFelixRHSinghLHarlandCCThe successful treatment of lupus pernio with the flashlamp pulsed dye laserJ Cutan Laser Ther199911495211360426
- RaulinCSchmidtCHellwigSCutaneous lupus erythematosus-treatment with pulsed dye laserBr J Dermatol199914161046105010606850
- EisenDAlsterTSUse of a 585 nm pulsed dye laser for the treatment of morpheaDermatol Surg200228761561612135520
- WelshJHSchroederTLLevyMLGranuloma faciale in a child successfully treated with the pulsed dye laserJ Am Acad Dermatol1999412 Pt 235135310426931
- CurrieCLMonkBEPulsed dye laser treatment of necrobiosis lipoidica: report of a caseJ Cutan Laser Ther19991423924111360467
- KaufmanAJTreatment of elastosis perforans serpiginosa with the flashlamp pulsed dye laserDermatol Surg200026111060106211096396
- SchonermarkMPSchmidtCRaulinCTreatment of sebaceous gland hyperplasia with the pulsed dye laserLasers Surg Med19972143133169328977
- HughesPSTreatment of molluscum contagiosum with the 585-nm pulsed dye laserDermatol Surg19982422292309491117
- GoldmanMPTreatment of benign vascular lesions with the Photoderm VL high-intensity pulsed light sourceAdv Dermatol1997135035219551153
- RaulinCSchroeterCAWeissRAKeinerMWernerSTreatment of port-wine stains with a noncoherent pulsed light source: a retrospective studyArch Dermatol1999135667968310376695
- JayHBorekCTreatment of a venous-lake angioma with intense pulsed lightLancet199835190961129439501
- WeissMAHsuJTNeuhausISadickNSDuffyDMConsensus for sclerotherapyDermatol Surg201440121309131825418805
- WeissRADoverJSLaser surgery of leg veinsDermatol Clin2002201193611859592
- ReichertDEvaluation of the long-pulse dye laser for the treatment of leg telangiectasiasDermatol Surg19982477377409693667
- RaulinCWeissRASchonermarkMPTreatment of essential telangiectasias with an intense pulsed light source (PhotoDerm VL)Dermatol Surg19972310941945 discussion 945–9469357506
- MeestersAAPitassiLHCamposVWolkerstorferADierickxCCTranscutaneous laser treatment of leg veinsLasers Med Sci201429248149224220848
- McDanielDHAshKLordJNewmanJAdrianRMZukowskiMLaser therapy of spider leg veins: clinical evaluation of a new long pulsed alexandrite laserDermatol Surg199925152589935096
- KauvarANLouWWPulsed alexandrite laser for the treatment of leg telangiectasia and reticular veinsArch Dermatol2000136111371137511074700
- AlsterTZaulyanovLLaser scar revision: a reviewDermatol Surg200733213114017300597
- SobankoJFAlsterTSLaser treatment for improvement and minimization of facial scarsFacial Plast Surg Clin North Am201119352754221856540
- SobankoJFAlsterTSManagement of acne scarring, part I: a comparative review of laser surgical approachesAm J Clin Dermatol201213531933022612738
- AlsterTSHandrickCLaser treatment of hypertrophic scars, keloids, and striaeSemin Cutan Med Surg200019428729211149609
- ManuskiattiWFitzpatrickREGoldmanMPEnergy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585-nm flashlamp-pumped pulsed-dye laserJ Am Acad Dermatol200145455756511568747
- ManuskiattiWFitzpatrickRETreatment response of keloidal and hypertrophic sternotomy scars: comparison among intralesional corticosteroid, 5-fluorouracil, and 585-nm flashlamp-pumped pulsed-dye laser treatmentsArch Dermatol200213891149115512224975
- AlsterTLaser scar revision: comparison study of 585-nm pulsed dye laser with and without intralesional corticosteroidsDermatol Surg2003291252912534508
- WaibelJSWulkanAJShumakerPRTreatment of hypertrophic scars using laser and laser assisted corticosteroid deliveryLasers Surg Med201345313514023460557
- AndersonRRDonelanMBHivnorCLaser treatment of traumatic scars with an emphasis on ablative fractional laser resurfacing: consensus reportJAMA Dermatol2014150218719324336931
- MalekzadFShakoeiSAyatollahiAHejaziSThe safety and efficacy of the 1540nm non-ablative fractional XD probe of star lux 500 device in the treatment of striae alba: before-after studyJ Lasers Med Sci20145419419825653821
- Tretti ClementoniMLavagnoRA novel 1565 nm non-ablative fractional device for stretch marks: a preliminary reportJ Cosmet Laser Ther201517314815525633176
- MurphyGFShepardRSPaulBSMenkesAAndersonRRParrishJAOrganelle-specific injury to melanin-containing cells in human skin by pulsed laser irradiationLab Invest19834966806856656199
- ArndtKAArgon laser treatment of lentigo malignaJ Am Acad Dermatol19841069539576736338
- ChanHHFungWKYingSYKonoTAn in vivo trial comparing the use of different types of 532 nm Nd:YAG lasers in the treatment of facial lentigines in Oriental patientsDermatol Surg200026874374910940060
- BailinPLRatzJLLevineHLRemoval of tattoos by CO2 laserJ Dermatol Surg Oncol198061299710016782144
- ReidWHMillerIDMurphyMJPaulJPEvansJHQ-switched ruby laser treatment of tattoos; a 9-year experienceBr J Plast Surg19904366636692257415
- ScheibnerAKennyGWhiteWWheelandRGA superior method of tattoo removal using the Q-switched ruby laserJ Dermatol Surg Oncol19901612109110982262615
- AshinoffRGeronemusRGRapid response of traumatic and medical tattoos to treatment with the Q-switched ruby laserPlast Reconstr Surg19939158418458460187
- AchauerBMNelsonJSVander KamVMApplebaumRTreatment of traumatic tattoos by Q-switched ruby laserPlast Reconstr Surg19949323183238310023
- GoldbergDJStampienTQ-switched ruby laser treatment of congenital neviArch Dermatol199513156216237741560
- NehalKSLevineVJAshinoffRThe treatment of benign pigmented lesions and tattoos with the Q-switched ruby laser. A comparative study using the 5.0- and 6.5-mm spot sizeDermatol Surg19962286836868780759
- RaulinCSchonermarkMPGreveBWernerSQ-switched ruby laser treatment of tattoos and benign pigmented skin lesions: a critical reviewAnn Plast Surg19984155555659827962
- OnoITateshitaTEfficacy of the ruby laser in the treatment of Ota’s nevus previously treated using other therapeutic modalitiesPlast Reconstr Surg19981027235223579858169
- GrevelinkJMDukeDvan LeeuwenRLGonzalezEDeCosteSDAndersonRRLaser treatment of tattoos in darkly pigmented patients: efficacy and side effectsJ Am Acad Dermatol19963446536568601656
- KonoTNozakiMChanHHMikashimaYA retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of OtaLasers Surg Med200129215615911553904
- KilmerSLLaser eradication of pigmented lesions and tattoosDermatol Clin2002201375311859593
- FitzpatrickREGoldmanMPTattoo removal using the alexandrite laserArch Dermatol199413012150815147986123
- AlsterTSQ-switched alexandrite laser treatment (755 nm) of professional and amateur tattoosJ Am Acad Dermatol199533169737601949
- StaffordTJLizekRBollJTanOTRemoval of colored tattoos with the Q-switched alexandrite laserPlast Reconstr Surg19959523133207824611
- LeuenbergerMLMulasMWHataTRGoldmanMPFitzpatrickREGrevelinkJMComparison of the Q-switched alexandrite, Nd:YAG, and ruby lasers in treating blue-black tattoosDermatol Surg199925110149935085
- LamAYWongDSLamLKHoWSChanHHA retrospective study on the efficacy and complications of Q-switched alexandrite laser in the treatment of acquired bilateral nevus of Ota-like maculesDermatol Surg20012711937941 discussion 941–94211737127
- GreenDFriedmanKJTreatment of minocycline-induced cutaneous pigmentation with the Q-switched Alexandrite laser and a review of the literatureJ Am Acad Dermatol2001442 Suppl34234711174411
- JangKAChungECChoiJHSungKJMoonKCKohJKSuccessful removal of freckles in Asian skin with a Q-switched alexandrite laserDermatol Surg200026323123410759799
- AlsterTSWilliamsCMTreatment of nevus of Ota by the Q-switched alexandrite laserDermatol Surg19952175925967606368
- AlsterTSGuptaSNMinocycline-induced hyperpigmentation treated with a 755-nm Q-switched alexandrite laserDermatol Surg20043091201120415355359
- KilmerSLLeeMSGrevelinkJMFlotteTJAndersonRRThe Q-switched Nd:YAG laser effectively treats tattoos. A controlled, dose-response studyArch Dermatol199312989719788352621
- TseYLevineVJMcClainSAAshinoffRThe removal of cutaneous pigmented lesions with the Q-switched ruby laser and the Q-switched neodymium: yttrium-aluminum-garnet laser. A comparative studyJ Dermatol Surg Oncol199420127958007798410
- KilmerSLWheelandRGGoldbergDJAndersonRRTreatment of epidermal pigmented lesions with the frequency-doubled Q-switched Nd:YAG laser. A controlled, single-impact, dose-response, multicenter trialArch Dermatol199413012151515197986124
- FergusonJEAugustPJEvaluation of the Nd/YAG laser for treatment of amateur and professional tattoosBr J Dermatol199613545865918915151
- JonesARoddeyPOrengoIRosenTThe Q-switched ND:YAG laser effectively treats tattoos in darkly pigmented skinDermatol Surg1996221299910019078310
- TroiliusAMEffective treatment of traumatic tattoos with a Q-switched Nd:YAG laserLasers Surg Med19982221031089484703
- FreedmanJRKaufmanJMetelitsaAIGreenJBPicosecond lasers: the next generation of short-pulsed lasersSemin Cutan Med Surg201433416416825830248
- HaedersdalMBech-ThomsenNWulfHCSkin reflectance-guided laser selections for treatment of decorative tattoosArch Dermatol199613244034078629843
- AndersonRRGeronemusRKilmerSLFarinelliWFitzpatrickRECosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatmentArch Dermatol19931298101010148352605
- AshinoffRLevineVJSoterNAAllergic reactions to tattoo pigment after laser treatmentDermatol Surg19952142912947728477
- TaylorCRLaser ignition of traumatically embedded firework debrisLasers Surg Med19982231571589510099
- BjerringPChristiansenKIntense pulsed light source for treatment of small melanocytic nevi and solar lentiginesJ Cutan Laser Ther20002417718111350673
- KawadaAShiraishiHAsaiMClinical improvement of solar lentigines and ephelides with an intense pulsed light sourceDermatol Surg200228650450812081680
- SasayaHKawadaAWadaTHiraoAOisoNClinical effectiveness of intense pulsed light therapy for solar lentigines of the handsDermatol Ther201124658458622515674
- LaskGElmanMSlatkineMWaldmanARozenbergZLaser-assisted hair removal by selective photothermolysis. Preliminary resultsDermatol Surg19972397377399311365
- NanniCAAlsterTSA practical review of laser-assisted hair removal using the Q-switched Nd:YAG, long-pulsed ruby, and long-pulsed alexandrite lasersDermatol Surg1998241213991405 discussion 14059865211
- DierickxCCHair removal by lasers and intense pulsed light sourcesDermatol Clin200220113514611859588
- AltshulerGBAndersonRRMansteinDZenzieHHSmirnovMZExtended theory of selective photothermolysisLasers Surg Med200129541643211891730
- RogachefskyASSilapuntSGoldbergDJEvaluation of a new super-long-pulsed 810 nm diode laser for the removal of unwanted hair: the concept of thermal damage timeDermatol Surg200228541041412030874
- GrossmanMCDierickxCFarinelliWFlotteTAndersonRRDamage to hair follicles by normal-mode ruby laser pulsesJ Am Acad Dermatol19963568898948959946
- DierickxCCGrossmanMCFarinelliWAAndersonRRPermanent hair removal by normal-mode ruby laserArch Dermatol199813478378429681347
- McDanielDHLordJAshKNewmanJZukowskiMLaser hair removal: a review and report on the use of the long-pulsed alexandrite laser for hair reduction of the upper lip, leg, back, and bikini regionDermatol Surg199925642543010469087
- NanniCAAlsterTSLaser-assisted hair removal: side effects of Q-switched Nd:YAG, long-pulsed ruby, and alexandrite lasersJ Am Acad Dermatol1999412 Pt 116517110426883
- GarciaCAlamoudiHNakibMZimmoSAlexandrite laser hair removal is safe for Fitzpatrick skin types IV–VIDermatol Surg200026213013410691941
- EremiaSLiCYUmarSHNewmanNLaser hair removal: long-term results with a 755 nm alexandrite laserDermatol Surg2001271192092411737124
- HandrickCAlsterTSComparison of long-pulsed diode and long-pulsed alexandrite lasers for hair removal: a long-term clinical and histologic studyDermatol Surg200127762262611442611
- CamposVBDierickxCCFarinelliWALinTYManuskiattiWAndersonRRHair removal with an 800-nm pulsed diode laserJ Am Acad Dermatol200043344244710954655
- LouWWQuintanaATGeronemusRGGrossmanMCProspective study of hair reduction by diode laser (800 nm) with long-term follow-upDermatol Surg200026542843210816229
- GoldbergDJSilapuntSHair removal using a long-pulsed Nd:YAG laser: comparison at fluences of 50, 80, and 100 J/cmDermatol Surg200127543443611359488
- LorenzSBrunnbergSLandthalerMHohenleutnerUHair removal with the long pulsed Nd:YAG laser: a prospective study with one year follow-upLasers Surg Med200230212713411870792
- WeissRAWeissMAMarwahaSHarringtonACHair removal with a non-coherent filtered flashlamp intense pulsed light sourceLasers Surg Med199924212813210100650
- SadickNSWeissRASheaCRNagelHNicholsonJPrietoVGLong-term photoepilation using a broad-spectrum intense pulsed light sourceArch Dermatol2000136111336134011074695
- AlsterTSBryanHWilliamsCMLong-pulsed Nd:YAG laser-assisted hair removal in pigmented skin: a clinical and histological evaluationArch Dermatol2001137788588911453807
- TanziELAlsterTSLong-pulsed 1064-nm Nd:YAG laser-assisted hair removal in all skin typesDermatol Surg2004301131714692920
- ChanCSDoverJSNd:YAG laser hair removal in Fitzpatrick skin types IV to VIJ Drugs Dermatol201312336636723545924
- AslamAAlsterTSEvolution of laser skin resurfacing: from scanning to fractional technologyDermatol Surg201440111163117225285818
- WaldorfHAKauvarANGeronemusRGSkin resurfacing of fine to deep rhytides using a char-free carbon dioxide laser in 47 patientsDermatol Surg199521119409467582831
- LoweNJLaskGGriffinMEMaxwellALowePQuiladaFSkin resurfacing with the ultrapulse carbon dioxide laser. Observations on 100 patientsDermatol Surg19952112102510297496669
- FitzpatrickREGoldmanMPSaturNMTopeWDPulsed carbon dioxide laser resurfacing of photo-aged facial skinArch Dermatol199613243954028629842
- AlsterTSGargSTreatment of facial rhytides with a high-energy pulsed carbon dioxide laserPlast Reconstr Surg19969857917948823015
- RossEVMillerCMeehanKOne-pass CO2 versus multiple-pass Er:YAG laser resurfacing in the treatment of rhytides: a comparison side-by-side study of pulsed CO2 and Er:YAG lasersDermatol Surg200127870971511493293
- RostanEFFitzpatrickREGoldmanMPLaser resurfacing with a long pulse erbium:YAG laser compared to the 950 ms pulsed CO(2) laserLasers Surg Med200129213614111553900
- AlsterTSNanniCAWilliamsCMComparison of four carbon dioxide resurfacing lasers. A clinical and histopathologic evaluationDermatol Surg1999253153158 discussion 15910193958
- AlsterTSCutaneous resurfacing with CO2 and erbium: YAG lasers: preoperative, intraoperative, and postoperative considerationsPlast Reconstr Surg19991032619632 discussion 633–6349950554
- AlsterTSWestTBResurfacing of atrophic facial acne scars with a high-energy, pulsed carbon dioxide laserDermatol Surg1996222151154 discussion 154–1558608377
- WaliaSAlsterTSProlonged clinical and histologic effects from CO2 laser resurfacing of atrophic acne scarsDermatol Surg1999251292693010594623
- FitzpatrickRERostanEFMarchellNCollagen tightening induced by carbon dioxide laser versus erbium: YAG laserLasers Surg Med200027539540311126433
- AlsterTSBellewSGImprovement of dermatochalasis and periorbital rhytides with a high-energy pulsed CO2 laser: a retrospective studyDermatol Surg2004304 Pt 1483487 discussion 48715056134
- WollinaUAblative erbium:YAG laser treatment of idiopathic chronic inflammatory non-cicatricial balanoposthitis (Zoon’s disease) – a series of 20 patients with long-term outcomeJ Cosmet Laser Ther201012312012320429688
- AlbertiniJGHolckDEFarleyMFZoon’s balanitis treated with Erbium:YAG laser ablationLasers Surg Med200230212312611870791
- OmiTNumanoKThe role of the CO2 laser and fractional CO2 laser in dermatologyLaser Therapy2014231496024771971
- TanziELAlsterTSSingle-pass carbon dioxide versus multiple-pass Er:YAG laser skin resurfacing: a comparison of postoperative wound healing and side-effect ratesDermatol Surg2003291808412534517
- BernsteinLJKauvarANGrossmanMCGeronemusRGThe short- and long-term side effects of carbon dioxide laser resurfacingDermatol Surg19972375195259236869
- NanniCAAlsterTSComplications of carbon dioxide laser resurfacing. An evaluation of 500 patientsDermatol Surg19982433153209537005
- Sriprachya-AnuntSFitzpatrickREGoldmanMPSmithSRInfections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skinDermatol Surg1997237527535 discussion 535–5369236870
- TanziELAlsterTSSide effects and complications of variable-pulsed erbium:yttrium-aluminum-garnet laser skin resurfacing: extended experience with 50 patientsPlast Reconstr Surg2003111415241529 discussion 1530–153212618614
- AlsterTSLuptonJRPrevention and treatment of side effects and complications of cutaneous laser resurfacingPlast Reconstr Surg20021091308316 discussion 317–31811786830
- GoldbergDJWhitworthJLaser skin resurfacing with the Q-switched Nd:YAG laserDermatol Surg19972310903906 discussion 906–9079357499
- KimYJLeeHSSonSWKimSNKyeYCAnalysis of hyperpigmentation and hypopigmentation after Er:YAG laser skin resurfacingLasers Surg Med2005361475115662626
- LuptonJRWilliamsCMAlsterTSNonablative laser skin resurfacing using a 1540 nm erbium glass laser: a clinical and histologic analysisDermatol Surg200228983383512269878
- TanziELWilliamsCMAlsterTSTreatment of facial rhytides with a nonablative 1,450-nm diode laser: a controlled clinical and histologic studyDermatol Surg200329212412812562339
- TanziELAlsterTSComparison of a 1450-nm diode laser and a 1320-nm Nd:YAG laser in the treatment of atrophic facial scars: a prospective clinical and histologic studyDermatol Surg2004302 Pt 115215714756642
- DoshiSNAlsterTS1,450 nm long-pulsed diode laser for nonablative skin rejuvenationDermatol Surg2005319 Pt 212231226 discussion 122616176775
- MansteinDHerronGSSinkRKTannerHAndersonRRFractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injuryLasers Surg Med200434542643815216537
- HantashBMBediVPKapadiaBIn vivo histological evaluation of a novel ablative fractional resurfacing deviceLasers Surg Med20073929610717311274
- HantashBMMahmoodMBFractional photothermolysis: a novel aesthetic laser surgery modalityDermatol Surg200733552553417451574
- AlsterTSTanziELLazarusMThe use of fractional laser photothermolysis for the treatment of atrophic scarsDermatol Surg200733329529917338686
- ChrastilBGlaichASGoldbergLHFriedmanPMSecond-generation 1,550-nm fractional photothermolysis for the treatment of acne scarsDermatol Surg200834101327133219040687
- HuSChenMCLeeMCYangLCKeoprasomNFractional resurfacing for the treatment of atrophic facial acne scars in Asian skinDermatol Surg200935582683219397671
- WannerMTanziELAlsterTSFractional photothermolysis: treatment of facial and nonfacial cutaneous photodamage with a 1,550-nm erbium-doped fiber laserDermatol Surg2007331232817214675
- KunishigeJHKatzTMGoldbergLHFriedmanPMFractional photothermolysis for the treatment of surgical scarsDermatol Surg201036453854120187893
- LinJYWargerWCIziksonLAndersonRRTannousZA prospective, randomized controlled trial on the efficacy of fractional photothermolysis on scar remodelingLasers Surg Med201143426527221500220
- WaibelJWulkanAJLupoMBeerKAndersonRRTreatment of burn scars with the 1,550 nm nonablative fractional Erbium laserLasers Surg Med201244644144622674649
- SaediNPetrellKArndtKDoverJEvaluating facial pores and skin texture after low-energy nonablative fractional 1440-nm laser treatmentsJ Am Acad Dermatol201368111311823098639
- KatzTMGlaichASGoldbergLHFirozBFDaiTFriedmanPMTreatment of melasma using fractional photothermolysis: a report of eight cases with long-term follow-upDermatol Surg20103681273128020666816
- LeeHMHawSKimJKChangSELeeMWSplit-face study using a 1,927-nm thulium fiber fractional laser to treat photoaging and melasma in Asian skinDermatol Surg201339687988823465065
- JihMHGoldbergLHKimyai-AsadiAFractional photothermolysis for photoaging of handsDermatol Surg2008341737818053047
- JungJYLeeJHRyuDJLeeSJBangDChoSBLower-fluence, higher-density versus higher-fluence, lower-density treatment with a 10,600-nm carbon dioxide fractional laser system: a split-face, evaluator-blinded studyDermatol Surg201036122022202921070459
- TierneyEPHankeCWFractionated carbon dioxide laser treatment of photoaging: prospective study in 45 patients and review of the literatureDermatol Surg20113791279129022988990
- TierneyEPTreatment of acne scarring using a dual-spot-size ablative fractionated carbon dioxide laser: review of the literatureDermatol Surg201137794596121682795
- HedelundLHaakCSTogsverd-BoKBoghMKBjerringPHaedersdalMFractional CO2 laser resurfacing for atrophic acne scars: a randomized controlled trial with blinded response evaluationLasers Surg Med201244644745222766970
- GraberEMTanziELAlsterTSSide effects and complications of fractional laser photothermolysis: experience with 961 treatmentsDermatol Surg2008343301305 discussion 305–30718190541
- MetelitsaAIAlsterTSFractionated laser skin resurfacing treatment complications: a reviewDermatol Surg201036329930620100273
- AlsterTSWanitphakdeedechaRImprovement of postfractional laser erythema with light-emitting diode photomodulationDermatol Surg200935581381519397672
- ChanHHMansteinDYuCSShekSKonoTWeiWIThe prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in AsiansLasers Surg Med200739538138517518354
- TanKLKurniawatiCGoldMHLow risk of postinflammatory hyperpigmentation in skin types 4 and 5 after treatment with fractional CO2 laser deviceJ Drugs Dermatol20087877477718720695
- FifeDJFitzpatrickREZacharyCBComplications of fractional CO2 laser resurfacing: four casesLasers Surg Med200941317918419291745
- AvramMMTopeWDYuTSzachowiczENelsonJSHypertrophic scarring of the neck following ablative fractional carbon dioxide laser resurfacingLasers Surg Med200941318518819291746
- AsawanondaPAndersonRRChangYTaylorCR308-nm excimer laser for the treatment of psoriasis: a dose-response studyArch Dermatol2000136561962410815855
- FeldmanSRMellenBGHousmanTSEfficacy of the 308-nm excimer laser for treatment of psoriasis: results of a multicenter studyJ Am Acad Dermatol200246690090612063488
- MafongEAFriedmanPMKauvarANBernsteinLJAlexiades-ArmenakasMGeronemusRGTreatment of inverse psoriasis with the 308 nm excimer laserDermatol Surg200228653053212081686
- TrehanMTaylorCRHigh-dose 308-nm excimer laser for the treatment of psoriasisJ Am Acad Dermatol200246573273712004316
- SpencerJMNossaRAjmeriJTreatment of vitiligo with the 308-nm excimer laser: a pilot studyJ Am Acad Dermatol200246572773112004315
- SunYWuYXiaoBTreatment of 308-nm excimer laser on vitiligo: a systemic review of randomized controlled trialsJ Dermatolog Treat201517
- MehrabanSFeilyA308nm excimer laser in dermatologyJ Lasers Med Sci20145181225606333

