Abstract
Here, we report a case of a middle-aged woman presenting with severe, long-standing, hyperkeratotic plaques of the lower extremities unrelieved by over-the-counter medications. Initial history and clinical findings were suggestive of an inherited ichthyosis. Ichthyoses are genetic disorders characterized by dry scaly skin and altered skin-barrier function. A diagnosis of ichthyosis vulgaris was confirmed by histopathology. Etiology, prevalence, and treatment options are discussed.
Introduction
Inherited ichthyoses are a diverse group of genetic disorders characterized by dry, scaly skin; hyperkeratosis; and altered skin-barrier function. While these disorders of cutaneous keratinization are multifaceted and varying in etiology, disruption in the stratum corneum with generalized scaling is common to all.Citation1–Citation4 Although not entirely known how each diverse genetic process of the ichthyoses could lead to a similar phenotype, a weakened epidermal barrier allowing for inflammation and subsequent hyperproliferation of the skin is hypothesized.Citation1–Citation4
Various ichthyoses can be differentiated from one another through history, clinical exam, histopathological analysis, electron microscopy, and genetics. Determining the inheritance pattern is an important part of the family history; this information is helpful in both formulating the differential diagnosis as well as in understanding the variable expressivity and severity of the disorder.Citation1,Citation3,Citation4 It is also important to know: if the ichthyosis is congenital or was acquired later in adulthood; whether there is a presence or absence of erythroderma; and the features and specific appearance of the scale, as well as any other systemic manifestations of the disease.Citation1,Citation3,Citation4 Although histopathological analysis can be useful to differentiate some of the ichthyoses, such as epidermolytic hyperkeratosis, other ichthyoses may not be able to be distinguished from one another via this manner alone.Citation1,Citation3,Citation4
Ichthyosis vulgaris (IV), the most frequently occurring ichthyosis, is caused by mutations in the filaggrin gene (FLG).Citation1,Citation3–Citation13 Typical hallmarks of IV, which encompass a wide clinical spectrum, include visible scaling and dryness that spares flexural surfaces, hyperlinearity of palms and soles, and strong predisposition for allergic disease comorbidities.Citation1,Citation3–Citation11 Prevalence estimates for IV range from 4.0% to 7.7% in Europeans and 2.29% to 3.00% in Asians; observations of FLG mutations in darkly pigmented populations are low.Citation4,Citation5,Citation12,Citation13
Case report
A 57-year-old female with new-onset dyspnea was evaluated for severely hyperkeratotic skin of bilateral lower extremities ( and ). The lesions were reported as beginning during childhood, initially on the feet and progressing proximally to the level of the knee. The lesions, which were occasionally pruritic, had worsened over the prior 14 years and were not relieved by over-the-counter medications. Family history was significant for several generations of males and females with similar appearing skin as well as many unaffected family members. Our patient indicated improvement in symptoms when living in warmer, more humid environments with worsening of symptoms while living at more northern latitudes.
Discussion
IV, a genetically transmitted, autosomal semi- dominant disorder, exhibits varying penetrance of FLG mutations.Citation4,Citation6,Citation8,Citation13–Citation19 Individuals heterozygous for the FLG mutation often have a less severe form of the disease than those homozygous for the mutation.Citation4,Citation7,Citation8,Citation10,Citation14–Citation19 FLG encodes for a protein called profilaggrin, which functions as a precursor to filaggrin (or filament-aggregating protein).Citation7 Profilaggrin is stored in the granular layer of the epidermis as the major component of keratohyalin granules.Citation3,Citation4,Citation7,Citation15 Profilaggrin is cleaved into multiple filaggrin peptides that aggregate the keratin filaments. These keratin filament complexes are then cross-linked to the cell envelope and are important in maintaining the compact layer of skin and serving as a natural moisturizer.Citation3–Citation5,Citation6,Citation8,Citation16–Citation19
It has long been established that IV is associated with a decreased and even absent number of keratohyalin granules due to the deficiency of filaggrin proteins.Citation4,Citation7,Citation15 A compensatory epidermal hyperplasia with inflammation, abnormal desquamation, and hyperkeratosis results in an impaired epidermal barrier, water loss, and dehydration.Citation1,Citation9,Citation16,Citation20 Chemicals and allergens are more prone to cross the impaired barrier, leading to sensitization and an increased propensity for inflammatory skin conditions.Citation1,Citation4,Citation21–Citation23
IV is usually not clinically present at birth and may have a variety of presentations later in life. With inherited IV, symptoms usually begin before age 1 year and alternate between exacerbation and remission. With milder presentations, patients present with flaky white scaling patches, often on extremities and extensor surfaces, typically sparing the flexural and more hydrated areas of the body.Citation3,Citation4,Citation15 More severe cases of IV are rare and may show an increased hyperkeratosis of the palmoplantar skin with fissures forming on the heels of the feet.Citation1,Citation4,Citation15 The flaking scales may be pronounced over the head, trunk, face, and extremities. Intertriginous areas of the body (armpits, groin, etc), are usually spared.Citation1,Citation4,Citation15
Increased humidity explains the seasonal variation seen in IV. Symptoms often improve in the summer months and worsen in the cold and dry winter months, when the decreasing humidity further breaks down the residual filaggrin left in the skin.Citation1,Citation4,Citation15 IV is frequently associated with the atopic triad of atopic dermatitis, hay fever, and asthma as well as with keratosis pilaris.Citation4–Citation7,Citation11,Citation16,Citation18,Citation19 It is hypothesized that the epidermal barrier abnormality continually exposes the body to pathogens and allergens, ultimately resulting in a T-helper 2 immunophenotype consistent with atopy.Citation4
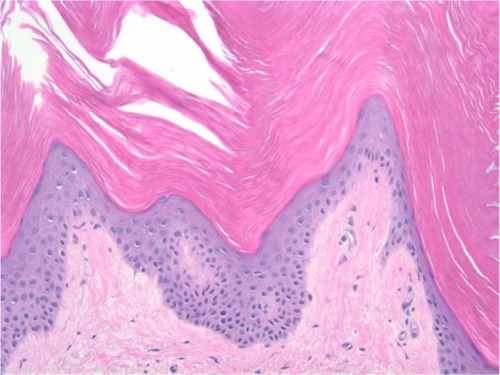
Histopathologically, IV demonstrates orthohyperkerato-sis, diminished to absent stratum granulosum, and decreased or absent keratohyalin granules on electron microscopy.Citation1,Citation4 In patients heterozygous for the gene mutation, the keratohyalin granules may be present but appear small.Citation3 Decreased or absent filaggrin on immunohistochemistry is characteristic as well.Citation1,Citation4
A histopathological analysis was done from a 4 mm punch biopsy of the right lower leg of our patient. Findings revealed orthohyperkeratosis with a markedly reduced stratum granulosum, consistent with IV. shows the histopathology of the punch biopsy specimen.
In this case, the severity of the IV was hypothesized to be related to her obesity and chronic lymphedema. Obesity is associated with mild chronic inflammation as well as impaired lymphatic drainage due to tissue compression.Citation24–Citation27 Lymphedema, the result of an inability of the lymphatic vasculature to remove fluid and lipids, leads to their accumulation in interstitial spaces.Citation24–Citation32 Recent reports also note fibrotic changes in the extracellular matrix of adipose tissue decrease lymphatic clearance of inflammatory macromolecules from interstitial spaces.Citation26,Citation27
While lymphedema begins as spongy swelling, the chronic recurring inflammation induces an infiltrate of fibroblasts and keratinocytes thus transforming the epidermal layer leading to its subsequent thickening.Citation28–Citation32 Over time, the limb with untreated lymphedema gains a brawny and indurated texture and histopathologically reveals hyperkeratosis and papillomatosis.Citation28–Citation32 Lymphedema-induced hyperkeratosis superimposed on the epidermal thickening associated with IV likely played a role in the exaggerated presentation in this case.
Treatment of IV is similar to that of many of the other ichthyoses and is symptomatic, complex, and dynamic.Citation9,Citation20–Citation23,Citation33 Primary treatments are topical moisturizers and medications designed to reduce scaling, support skin-barrier function, reduce water loss, and decrease symptoms. Lessening the scale, providing hydration, and moisturization can be accomplished with emollients, humectants, bathing immediately followed with moisturizers, keratolytic agents, and topical retinoids.Citation20,Citation21 Management of bacterial skin infections, most commonly staphylococcal or streptococcal in origin, is done with topical mupirocin or bacitracin.Citation21,Citation23 On the horizon, researchers are attempting to use genetic pharmacology to increase the body’s own production of normal filaggrin.Citation4,Citation15
For this patient, first-line treatment for IV was begun using topical 0.1% tretinoin and 40% urea cream. At follow-up, warm bath soaks prior to medication application was added to the regimen to enhance absorption. At the present time, marked objective clinical improvement, as well as subjective patient satisfaction with treatment, is noted. She continues to be followed in the dermatology clinic.
Conclusion
Our patient presented with an extreme presentation of a common disease. Based upon the history, IV was considered. However, the severity of the clinical presentation of hyperkeratosis strongly suggested an alternative diagnosis. This case is a helpful reminder that IV is the most common inherited ichthyosis, and therefore should be a diagnostic consideration in even extreme and atypical presentations.
Acknowledgments
Special thanks to the Department of Dermatology at West Virginia University School of Medicine, Morgantown, WV, for providing medical student opportunity for case study research. Manuscript editing assistance was provided by Susan B Leight, EdD, FNP-BC, FAANP, Director, School of Nursing, West Virginia Wesleyan College. The authors advise that the West Virginia University Ethics Committee/Institutional Review Board does not require patient approval for case reports.
Disclosure
The authors report no conflicts of interest in this work.
References
- BologniaJLJorizzoJLSchafferJVDermatology3rd edPhiladelphia, PAElsevier Saunders2012
- StyperekARRiceZPKamalpourLAnnual direct and indirect health costs of the congenital ichthyosesPediatr Dermatol201027432533520553402
- WolffKGoldsmithLAKatzSIGilchrestBAPallerASLeffellDJFitzpatrick’s Dermatology in General Medicine7th edNew York, NYMcGraw Hill2008
- ThyssenJPGodoy-GijonEEliasPMIchthyosis vulgaris: the filaggrin mutation diseaseBr J Dermatol201316861155116623301728
- LiMChengRShiMAnalyses of FLG mutation frequency and filaggrin expression in isolated ichthyosis vulgaris (IV) and atopic dermatitis-associated IVBr J Dermatol201316861335133823290076
- WellsRSKerrCBClinical features of autosomal dominant and sex-linked ichthyosis in an English populationBMJ19661549394795020790920
- LiuPYangQWangXIdentification of a genetic locus for ichthyosis vulgaris on chromosome 10q22.3–q24.2J Invest Dermatol200812861418142218079749
- SandilandsATerron-KwiatkowskiAHullPRComprehensive analysis of the gene encoding filaggrin uncovers prevalent and rare mutations in ichthyosis vulgaris and atopic eczemaNat Genet200739565065417417636
- BellewSDel RossoJQOvercoming the Barrier Treatment of Ichthyosis: A Combination-therapy ApproachJ Clin Aesthetic Dermatol2010374953
- Perusquίa-OrtizAMOjiVSauerlandMCComplete filaggrin deficiency in ichthyosis vulgaris is associated with only moderate changes in epidermal permeability barrier function profileJ Eur Acad Dermatol Venereol201327121552155823297869
- DreyfusIBourratEMaruaniAFactors associated with impaired quality of life in adult patients suffering from ichthyosisActa Derm Venereol201494334434624158261
- DreyfusIPauwelsCBourratEBurden of inherited ichthyosis: a French national surveyActa Derm Venereol201595332632825510955
- Esparza-GordilloJMatanovicAMarenholzIMaternal filaggrin mutations increase the risk of atopic dermatitis in children: an effect independent of mutation inheritancePLoS Genet2015113116
- MendesMSAquinoTAde Padua LimaAKouzakSSTakanoGHMosaic epidermolytic ichthyosis – case reportAn Bras Dermatol2013886 Suppl 111611924346896
- BrownSJMcLeanWHOne remarkable molecule: filaggrinJ Invest Dermatol20121323 Pt 275176222158554
- AkiyamaMFLG mutations in ichthyosis vulgaris and atopic eczema: spectrum of mutations and population geneticsBr J Dermatol2010162347247719958351
- ZhangXLiuSChenXNovel and recurrent mutations in the filaggrin gene in Chinese patients with ichthyosis vulgarisBr J Dermatol20101631636920222934
- NomuraTAkiyamaMSandilandsAPrevalent and rare mutations in the gene encoding filaggrin in Japanese patients with ichthyosis vulgaris and atopic dermatitisJ Invest Dermatol200912951302130519037238
- WingeMCGHoppeTBerneBFilaggrin genotype determines functional and molecular alterations in skin of patients with atopic dermatitis and ichthyosis vulgarisPLoS One2011612e2825422164253
- Blanchet-BardonCTadiniGMachado MatosMDelarueAAssociation of glycerol and paraffin in the treatment of ichthyosis in children: an international, multicentric, randomized, controlled, double-blind studyJ Eur Acad Dermatol Venereol20122681014101922118417
- FleckmanPNewellBDvan SteenselMAYansACTopical treatment of ichthyosesDermatol Ther2013261162523384017
- BodemerCBourratEMazereeuw-HautierJShort- and medium-term efficacy of specific hydrotherapy in inherited ichthyosisBr J Dermatol201116551087109421729027
- ChanAGodoy-GijonENuno-GonzalezACellular basis of secondary infections and impaired desquamation in certain inherited ichthyosesJAMA Dermatol2015151328529225565224
- DivyashreeRANaveenKNPaiVVAthanikarSBGuptaGCutaneous manifestations of obesity among dermatology patients in a tertiary care centerIndian J Dermatol Venereol Leprol201480327824823419
- GreeneAKGrantFDSlavinSALower-extremity lymphedema and elevated body-mass indexN Engl J Med2012366222136213722646649
- WeitmanESAschenSZFarias-EisnerObesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodesPLoS One201388e7070323950984
- ArngrimNSimonsenLHolstJJBülowJReduced adipose tissue lymphatic drainage of macromolecules in obese subjects: a possible link between obesity and local tissue inflammation?Int J Obes (Lond)201337574875022751255
- ScheinfeldNSObesity and dermatologyClin Dermatol200422430330915475230
- BozaJCTrindadeENPeruzzoJSachettLRechLCestariTFSkin manifestations of obesity: a comparative studyJ Eur Acad Dermatol Venereol201226101220122321929550
- LuSTranTAJonesDMLocalized lymphedema (elephantiasis): a case series and review of the literatureJ Cutan Pathol200936412018564285
- KabaHBakarYOzdemirOçSertelSComplex Decongestive Physiotherapy Treats Skin Changes like Hyperkeratosis Caused by LymphedemaCase Rep Dermatol Med2012201241642123259083
- LinnittNComplex skin changes in chronic oedemasBr J Community Nurs2007124S10S1517505345
- NayakSAcharjyaBMohantyPIchthyosis hystrixIndian Dermatol Online J201341474923440302