Abstract
Background
Achalasia is a primary esophageal motility disorder of unknown etiology associated with abnormalities in peristalsis and lower esophageal sphincter relaxation. The disease is incurable; however, definitive treatment procedures like pneumatic dilation (PD)/balloon dilation and laparoscopic esophageal myotomy (LEM) are performed to relieve dysphagia and related symptoms. Currently, there is paucity of data comparing the outcomes of these procedures. The aim of this meta-analysis is to compare the short- and long-term success rates of PD and LEM.
Methods
A thorough systematic search of PubMed, Scopus, clinicaltrials.gov, and Cochrane library was conducted for randomized controlled trials (RCTs) comparing the outcomes of PD versus LEM in the treatment of achalasia. The Mantel-Haenszel method and random effect model were used to analyze the data. RCTs with outcome data at 3-month, 1-year, and 5-year intervals were analyzed.
Results
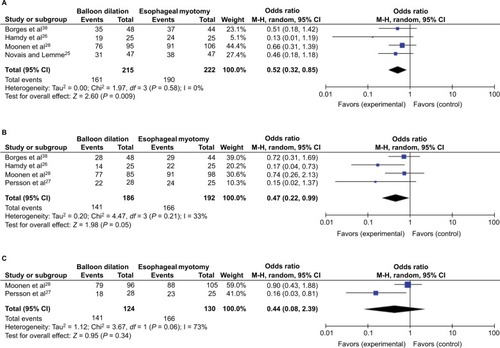
A total of 437,378 and 254 patients at 3-month, 1-year, and 5-year intervals were analyzed for outcome data. At 3 months and 1 year, PD was not as effective as LEM (odds ratio [OR]: 0.50; confidence interval [CI] 0.31–0.82; P = 0.009 and OR: 0.47; CI 0.22–0.99; P = 0.21) but at 5 years, one procedure was non-inferior to the other (OR: 0.62; 0.33–1.19; P = 0.34).
Conclusion
PD was as effective as LEM in relieving symptoms of achalasia in the long-term.
Introduction
Achalasia is an incurable primary progressive motility disorder of the esophagus where inhibitory ganglionic cells in the myenteric plexus of the lower esophageal sphincter (LES) are irreversibly lost. This leads to impaired relaxation of the LES after swallowing, causing functional obstruction.Citation1–Citation6 The most common symptoms of achalasia are dysphagia, heartburn, regurgitation, aspiration, and weight loss leading to impaired quality of life.Citation7–Citation9 This clinical diagnosis is enhanced by barium swallow studies and endoscopy, and confirmed by manometry.Citation10 Although there is no curative treatment of achalasia, various therapies have been tried in the past without much success.Citation10–Citation15 New options for achalasia peroral endoscopic myotomy (POEM), self-expanding metal stents, endoscopic sclerotherapy have shown promising results but there are only a few prospective observational studies to support their efficacy.Citation15–Citation23 Current standard of care for achalasia includes forceful pneumatic dilation/balloon dilatation (PD/BD) and laparoscopic (Heller’s) esophageal myotomy (LEM) with or without an anti-reflux procedure.Citation15 There are some randomized controlled trials (RCTs) comparing the success rate (improvement of dysphagia) of these procedures at short-term follow-up,Citation8,Citation24–Citation26 but there are only 3 RCTs comparing the long-term outcomes at 5 years published till date.Citation27–Citation29 Although there are systematic reviews and meta-analyses on prospective studies and non-RCTs,Citation30 there is only one meta-analysis of RCTs comparing the outcomes of these two procedures in the short-term.Citation31 Herein, we analyzed the published RCTs to study the short- and long-term success rates of these procedures in order to shed light on this controversial issue.
Methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis statement for reporting meta-analysis and systemic reviewsCitation32 as recommended by the Cochrane Collaboration was used for this meta-analysis (). A comprehensive electronic literature search was conducted for all the clinical trials on treatment of esophageal achalasia between the years 2000 and 2016 on PubMed, Embase, Scopus, Cochrane Library, clinicaltrials.gov, Ovid Medline, and Google scholar using the all-field “Achalasia, Esophageal”, all-fields “Balloon dilation” or “Pneumatic dilation, and all-fields “Myotomy” or “ Laparoscopic Heller’s Myotomy” or “Laparoscopic esophageal myotomy”; all three search headings were connected with Boolean operator “AND”. The eligibility criteria for the included studies relied on previously published guidelines for systematic reviews and were based on the PICO framework: P (Population: patients with idiopathic primary achalasia diagnosed with the help of clinical, endoscopic and manometric, and radiographic evidence), I (Intervention: repeated BD/PD), C (Comparative intervention/control group: LEM/Heller’s myotomy), and O (Outcomes: improvement in dysphagia score). Only RCTs published in English were included. Patients were randomly assigned to PD or LEM group. Studies with at-least 3-month follow-up were included. Two reviewers (RB and SU) independently assessed the eligibility and validity of each study. Any disagreements were resolved with discussion with the third and fourth authors (JK and SKS). The fifth, sixth, and seventh authors (TSM, BKG, and GB) evaluated the quality of the studies independently and any disagreement was resolved via discussions among all the reviewers, ultimately reaching to an agreement by consensus. This search parameter yielded 393 articles. Case reports, retrospective studies, letters, comments, and studies without the availability of the data were excluded. Only human studies were included. A total of 5 RCTs met the aforementioned criteria. Quality of the included studies was assessed with the Delphi Consensus criteria for RCTs ().Citation33
Figure 1 PRISMA statement of the study.
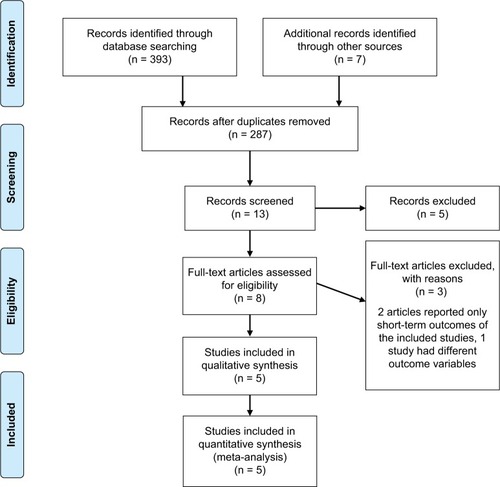
Table 1 Results of quality assessment by Delphi consensus criteria
From all the selected studies, we extracted the baseline study details (): total number of patient enrolled, number of patients in each arm, mean age, sex ratio, inclusion and exclusion criteria, procedure detail ( and ), randomization process, definition of success or failure, adverse events, and quality of life score. Success rate was measured at 3 months, 1 year, and 5 years. The outcomes were calculated with RevMan, version 5.2 for Windows (Cochrane Collaboration, Oxford, UK). Analysis was performed by Mantel-Haenszel test. Odds ratio (OR) was calculated using confidence interval (CI) of 95%. Heterogeneity was calculated using I2. A randomized model was used because of the low heterogeneity from the low number of studies. A P-value of <0.05 was considered significant. The primary analysis focused on symptom resolution as the outcome of interest. This was based on various dysphagia scores in each study. Success rate was evaluated by using improvement validated tools like Watson dysphagia scoreCitation34 by Persson et al,Citation27 Eckardt scoreCitation35 by Moonen et al,Citation28 Demeester’s grading of dysphagiaCitation5 by Hamdy et al,Citation26 and Vantrappen and Hellemans scoreCitation36 by Borges et alCitation37 and Novais and LemmeCitation25 ().
Table 2 Baseline characteristics and results of the included studies
Table 3 Pneumatic dilation/balloon dilation procedure of included studies
Table 4 Laparoscopic surgical procedure of included studies
Table 5 Outcome measure or primary endpoint for included studies
Results
A total of 437 patients at 3-month interval, 378 patients at 1-year interval, and 254 patients at 5-year interval were analyzed for success rate of the procedure, namely the improvement in the dysphagia score. At 3 months, success rate was significantly lower in patients with BD (OR: 0.50; CI 0.31–0.82; P = 0.02). At 1 year, success rate was still significantly lower in BD (OR: 0.47; CI 0.22–0.99; P = 0.99) but nearing non-inferior levels. At 5 years, BD was non-inferior to myotomy (OR: 62; CI 0.33–1.19; P = 0.15) (). In an RCT, not included in our study, by Chrystoja et al,Citation29 no significant difference was found in the improvement of achalasia severity questionnaire at 1 year (score difference: 7.3; CI −4.7 to 19.3; P = 0.23 at 1 year) and 5 years (score difference: 0.5; CI −13.5 to 14.4; P = 0.95).
Discussion
Achalasia is a primary motor disorder of the esophagus that is chronic and incurable. Although LEM and PD are the mainstays of treatment, the best modality remains controversial.Citation4 Both treatment approaches carry a variable risk of recurrence of symptoms, perforation, and gastrointestinal reflux.Citation38 Therefore, it is imperative to identify the best method for the short- and long-term symptom relief with due consideration of complications. Our study compared the short- and long-term outcomes of the two procedures based on symptom relief at 3 different intervals. Our analysis shows that LEM is better at 3 months and at 1 year (with increasing confidence interval), while PD becomes non-inferior to LEM at 5 years. These results indicate that both treatment approaches lead to comparable outcomes in the long run.
In contrast to LEM, one major advantage of PD is that it can be performed safely in the outpatient setting without need for general anesthesia. However, more patients in single PD group require re-intervention compared to those treated with LEM.Citation39 Although the remission rate is higher with graded dilation approach,Citation40–Citation43 it is associated with higher rates of perforation and complex surgeryCitation44 LEM, on the other hand, has the major risk of mucosal tear, and leads to abdominal wall trauma requiring longer recovery time.
In a meta-analysis by Yaghoobi et al,Citation31 LEM provided greater relief of symptoms compared to graded dilation. The main limitation of the study was the lack of long-term follow-up and a small number of included studies. The network meta-analysis by Schoenberg et alCitation45 corroborated these findings. The study did not include long-term follow-up and included indirect comparison. In another meta-analysis by Campos et al,Citation30 LEM was found to be more effective and long lasting compared to BD or botulin toxin injection. However, the complication rate was higher in the surgical group due to the invasiveness of the procedure. In this regard, PD was deemed more suited for frail patients who are poor surgical candidates, or for those patients who fail surgery. However, the results of these studies have to be interpreted with caution as these studies often use variable and subjective definitions of success rate. Furthermore, some of the studies included in the analysis used data from single dilations, while it is well known that it is a multistage procedure with graded dilation.Citation46 In lieu of the largest RCT, the European Achalasia Trial,Citation28 the present meta-analysis is the only one of its kind to include this in the analysis.
The other consideration for this study is the evolving technique of the procedure. The technique of dilation has evolved from rigid dilators to hydrostatic balloon. This allows achievement of maximum controlled volume with low pressure, which improves efficacy and prevents perforation.Citation47 The hypothesis that BD causes the disruption of muscular layer has been challenged by the study by Borhan-Manesh et al.Citation48 The finding shows that PD works by circumferential stretching of the LES. This has resulted in modification of the current method of dilation by slowing the rate of inflation, leading to increased remission rate of BD. POEM is a newer technique that is being used to perform myotomy of the LES. Long-term data from RCTs comparing POEM with conventional treatment methods are lacking. This procedure is still evolving and its role in management of achalasia is not clearly outlined.Citation49 Further studies comparing conventional treatment with POEM with a longer follow-up will be needed for change in practice. Thus, PD or LEM continues to remain the standard of care for achalasia with comparable outcome in the long-term.
Conclusion
Taken together, the data presented here provide evidence that both treatments have similar success rate at 5 years. So, eligible patients should be given the option of PD or LEM at this time.
Disclosure
The authors report no conflicts of interest in this work.
References
- GockelIMüllerMSchumacherJAchalasia–a disease of unknown cause that is often diagnosed too lateDtsch Arztebl Int20121091220921422532812
- RollGRRablCCiovicaRPeevaSCamposGMA controversy that has been tough to swallow: is the treatment of achalasia now digested?J Gastrointest Surg201014Suppl 1S33S4519760373
- ChuahSKHsuPIWuKLWuDCTaiWCChangchienCS2011 update on esophageal achalasiaWorld J Gastroenterol201218141573157822529685
- RichterJEAchalasia – an updateJ Neurogastroenterol Motil201016323224220680161
- VaeziMFPandolfinoJEVelaMFACG clinical guideline: diagnosis and management of achalasiaAm J Gastroenterol2013108812381249 quiz 125023877351
- ParkWVaeziMFEtiology and pathogenesis of achalasia: the current understandingAm J Gastroenterol200510061404141415929777
- ChanSMChiuPWWuJCLaparoscopic Heller’s cardiomyotomy achieved lesser recurrent dysphagia with better quality of life when compared with endoscopic balloon dilatation for treatment of achalasiaDis Esophagus201326323123622624653
- KosticSKjellinARuthMPneumatic dilatation or laparoscopic cardiomyotomy in the management of newly diagnosed idiopathic achalasia. Results of a randomized controlled trialWorld J Surg200731347047817308851
- MarlaisMFishmanJFellJRawatDHaddadMReduced health-related quality of life in children with achalasiaArch Dis Child201095Suppl 1A53
- MoonenAJBoeckxstaensGEManagement of achalasiaGastroenterol Clin North Am2013421455523452630
- MikaeliJFazelAMontazeriGYaghoobiMMalekzadehRRandomized controlled trial comparing botulinum toxin injection to pneumatic dilatation for the treatment of achalasiaAliment Pharmacol Ther20011591389139611552910
- BansalRNostrantTTScheimanJMIntrasphincteric botulinum toxin versus pneumatic balloon dilation for treatment of primary achalasiaJ Clin Gastroenterol200336320921412590230
- ZaninottoGAnneseVCostantiniMRandomized controlled trial of botulinum toxin versus laparoscopic Heller myotomy for esophageal achalasiaAnn Surg2004239336437015075653
- BeckWCSharpKWAchalasiaSurg Clin North Am20119151031103721889028
- KrillJTNaikRDVaeziMFClinical management of achalasia: current state of the artClin Exp Gastroenterol20169718227110134
- ZhaoJGLiYDChengYSLong-term safety and outcome of a temporary self-expanding metallic stent for achalasia: a prospective study with a 13-year single-center experienceEur Radiol20091981973198019296113
- ChengYSMaFLiYDTemporary self-expanding metallic stents for achalasia: a prospective study with a long-term follow-upWorld J Gastroenterol201016405111511720976849
- InoueHMinamiHKobayashiYPeroral endoscopic myotomy (POEM) for esophageal achalasiaEndoscopy201042426527120354937
- von RentelnDInoueHMinamiHPeroral endoscopic myotomy for the treatment of achalasia: a prospective single center studyAm J Gastroenterol2012107341141722068665
- BhayaniNHKurianAADunstCMSharataAMRiederESwanstromLLA comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasiaAnn Surg201425961098110324169175
- LiYDTangGYChengYSChenNWChenWXZhaoJG13-Year follow-up of a prospective comparison of the long-term clinical efficacy of temporary self-expanding metallic stents and pneumatic dilatation for the treatment of achalasia in 120 patientsAJR Am J Roentgenol201019561429143721098206
- MoretóMOjembarrenaEBarturenACasadoITreatment of achalasia by injection of sclerosant substances: a long-term reportDig Dis Sci201358378879623179151
- NiknamRMikaeliJFazlollahiNEthanolamine oleate as a novel therapy is effective in resistant idiopathic achalasiaDis Esophagus201427761161623927485
- BoeckxstaensGEAnneseVdes VarannesSBEuropean Achalasia Trial InvestigatorsPneumatic dilation versus laparoscopic Heller’s myotomy for idiopathic achalasiaN Engl J Med2011364191807181621561346
- NovaisPALemmeEM24-h pH monitoring patterns and clinical response after achalasia treatment with pneumatic dilation or laparoscopic Heller myotomyAliment Pharmacol Ther201032101257126520955445
- HamdyEEl NakeebAEl HanfyEComparative study between laparoscopic Heller myotomy versus pneumatic dilatation for treatment of early achalasia: a prospective randomized studyJ Laparoendosc Adv Surg Tech A201525646046425951417
- PerssonJJohnssonEKosticSLundellLSmedhUTreatment of achalasia with laparoscopic myotomy or pneumatic dilatation: long-term results of a prospective, randomized studyWorld J Surg201539371372025409838
- MoonenAAnneseVBelmansALong-term results of the European achalasia trial: a multicentre randomised controlled trial comparing pneumatic dilation versus laparoscopic Heller myotomyGut201665573273926614104
- ChrystojaCCDarlingGEDiamantNEAchalasia-specific quality of life after pneumatic dilation or laparoscopic Heller myotomy with partial fundoplication: a multicenter, randomized clinical trialAm J Gastroenterol2016111111536154527619832
- CamposGMVittinghoffERablCEndoscopic and surgical treatments for achalasia: a systematic review and meta-analysisAnn Surg20092491455719106675
- YaghoobiMMayrandSMartelMRoshan-AfsharIBijarchiRBarkunALaparoscopic Heller’s myotomy versus pneumatic dilation in the treatment of idiopathic achalasia: a meta-analysis of randomized, controlled trialsGastrointest Endosc201378346847523684149
- BellerEMGlasziouPPAltmanDGPRISMA for Abstracts GroupPRISMA for Abstracts: reporting systematic reviews in journal and conference abstractsPLoS Med2013104e100141923585737
- VerhagenAPde VetHCde BieRAThe Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensusJ Clin Epidemiol199851121235124110086815
- ClarkAGRogersKMDependence upon bile volume of the biliary excretion of bromocresol green and amaranth in the anaesthetized ratAust J Biol Sci19752843393511191126
- EckardtVFStaufBBernhardGChest pain in achalasia: patient characteristics and clinical courseGastroenterology199911661300130410348812
- VantrappenGHellemansJTreatment of achalasia and related motor disordersGastroenterology19807911441546991359
- BorgesAALemmeEMAbrahaoLJJrPneumatic dilation versus laparoscopic Heller myotomy for the treatment of achalasia: variables related to a good responseDis Esophagus2014271182323551592
- LakeJMWongRKReview article: the management of achalasia – a comparison of different treatment modalitiesAliment Pharmacol Ther200624690991816948803
- LopushinskySRUrbachDRPneumatic dilatation and surgical myotomy for achalasiaJAMA2006296182227223317090769
- WestRLHirschDPBartelsmanJFLong term results of pneumatic dilation in achalasia followed for more than 5 yearsAm J Gastroenterol20029761346135112094848
- ZerbibFThétiotVRichyFBenajahDAMessageLLamouliatteHRepeated pneumatic dilations as long-term maintenance therapy for esophageal achalasiaAm J Gastroenterol2006101469269716635216
- BraviINicitaMTDucaPA pneumatic dilation strategy in achalasia: prospective outcome and effects on oesophageal motor function in the long termAliment Pharmacol Ther201031665866520003094
- HulselmansMVanuytselTDegreefTLong-term outcome of pneumatic dilation in the treatment of achalasiaClin Gastroenterol Hepatol201081303519782766
- MorinoMRebecchiFFestaVGarroneCPreoperative pneumatic dilatation represents a risk factor for laparoscopic Heller myotomySurg Endosc19971143593619094277
- SchoenbergMBMarxSKerstenJFLaparoscopic Heller myotomy versus endoscopic balloon dilatation for the treatment of achalasia: a network meta-analysisAnn Surg2013258694395224220600
- MoonenABoeckxstaensGFinding the right treatment for achalasia treatment: risks, efficacy, complicationsCurr Treat Options Gastroenterol201614442042827687234
- JacobsJRichterJEOpening the bird’s beak: tips and tricks for effective pneumatic dilation for achalasiaAm J Gastroenterol2016111215715826856752
- Borhan-ManeshFKavianiMJTaghaviARThe efficacy of balloon dilation in achalasia is the result of stretching of the lower esophageal sphincter, not muscular disruptionDis Esophagus201629326226625765473
- YounYHMinamiHChiuPWParkHPeroral endoscopic myotomy for treating achalasia and esophageal motility disordersJ Neurogastroenterol Motil2016221142426717928