Abstract
Objective
Secukinumab, a fully human monoclonal IgG1 antibody that selectively neutralizes the proinflammatory cytokine IL-17A, has been approved in Europe in 2015 for the treatment of adult patients with moderate-to-severe plaque psoriasis, psoriatic arthritis (PsA), and ankylosing spondylitis (AS). This analysis assessed the budget impact of introduction of secukinumab to the Italian market for all three indications from the perspective of the Italian National Health Service.
Materials and methods
A cross-indication budget impact model was developed and included biologic-treated adult patients diagnosed with psoriasis, PsA, and AS. The analyses were conducted over a 3-year time horizon and included direct costs (drug therapy costs, administration costs, diseases-related costs, and adverse events costs). Model input parameters (epidemiology, market share projections, resource use, and costs) were obtained from the published literature and other Italian sources. The robustness of the results was tested via one-way sensitivity analyses: secukinumab cost, secukinumab market share, intravenous administration costs, and adverse events costs were varied by ±10%.
Results
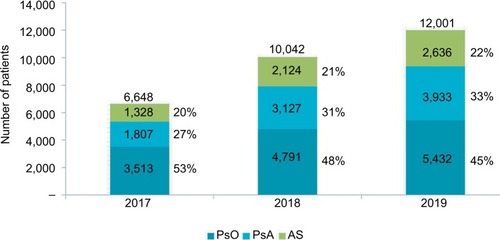
The total patient population for secukinumab over the 3-year timeframe was projected to be 6,648 in the first year, increasing to 12,001 in the third year, for all three indications combined (psoriasis, PsA, and AS). Compared to a scenario without secukinumab in the market, the introduction of secukinumab in the market for the treatment of psoriasis, PsA, and AS showed a cumulative 3-year incremental budget impact of −5%, corresponding to savings of €66.1 million and per patient savings of about €1,855. The majority of the cost savings came from the adoption of secukinumab in AS (58%), followed by PsA (29%) and psoriasis (13%). Sensitivity analyses confirmed the robustness of the results.
Conclusion
Results from this cross-indication budget impact model show that secukinumab is a cost-saving option for the treatment of PsA, AS, and psoriasis patients in Italy.
Introduction
Psoriasis, psoriatic arthritis (PsA), and ankylosing spondylitis (AS) are chronic, immune-mediated, inflammatory diseases associated with various comorbidities and worsening health-related quality of life (QoL).Citation1–Citation6 They are all generally chronic lifelong diseases having alternating flare-ups and periods of remission, resulting in reduced patients’ physical and psychological well-being, reduced work productivity, and higher health care costs in the longer term.Citation7,Citation8
Among these three diseases, psoriasis is the most common condition, which is estimated to affect between 0.7% and 2.9% of the population in Europe.Citation9 It primarily manifests on the skin, resulting in plaques on the elbows, knees, or scalp, which may extend to other areas of the body.Citation5,Citation10,Citation11 PsA and AS are part of spondyloarthritis (SpA), which are enthesitis driven, lifelong, painful, and debilitating immune-mediated inflammatory diseases affecting the joints and/or spine that can lead to irreversible structural bone damage caused by years of inflammation.Citation6,Citation12–Citation15 The prevalence of PsA in the general population has been reported to range from 0.01% in AsiaCitation16 to 0.67% in Norway,Citation17 while the prevalence of AS ranges from 0.1% to 1.4% globally.Citation18
Psoriasis is associated with significant clinical and emotional morbidity, impacting patients’ work and social lives and reduces the QoL.Citation19 Moreover, psoriasis is linked to other health conditions, such as diabetes, heart disease, and depression,Citation20 further impacting the QoL of patients. Patients with PsA and AS experience pain, loss of physical function, and difficulty in performing activities of daily living, including the ability to work.Citation6 Different studies have reported significant economic burden of psoriasis, PsA, and AS in different countries,Citation21–Citation26 including Italy.Citation27,Citation28 The economic and humanistic burden of SpA is closely connected to the functional status in PsA and AS patients, and it is increased by the fact that SpA usually occurs in active young adults.Citation7,Citation29–Citation33 According to a survey performed in 17 out of the 20 regions in Italy, sponsored by the National Association of Rheumatic Patients, half of the patients with SpA reported disability and one third felt that their condition limited their career progression and personal development.Citation34
Early efficacious treatments targeting inflammation control, prevention of comorbidities and complications, and function and social participation normalization are important in psoriasis, PsA, and AS management.Citation35,Citation36 The initial treatment for mild psoriasis includes topical steroids and phototherapy, whereas the initial treatment for moderate-to-severe psoriasis includes phototherapy and conventional systemic therapy, alone or in combination.Citation37 In the past decade, the development of several drugs, biologics, and non-biologics has substantially improved the outcomes of patients with moderate-to-severe psoriasis.Citation38 These include tumor necrosis factor (TNF)-α inhibitors (adalimumab, etanercept, certolizumab, golimumab, and infliximab), interleukin (IL)-12 and 23 inhibitor (ustekinumab), and IL-17A inhibitors (secukinumab and ixekizumab). In addition, among non-biologics, apremilast improves the outcomes (see for a list of currently approved and reimbursed treatments in Italy for each indication).Citation37,Citation39 Conventional pharmacologic treatment options for PsA and AS include nonsteroidal anti-inflammatory drugs as the first-line treatment.Citation40–Citation43 For PsA, conventional synthetic disease-modifying antirheumatic drugs are also used.Citation40,Citation41 Biologics are currently used for PsA and AS patients inadequately controlled by conventional treatments mentioned above/previously.
Table 1 Approved indications and currently approved and reimbursed treatments for secukinumab in Italy, along with their posology
Secukinumab, a recombinant fully human monoclonal IgG1 antibody that selectively neutralizes the proinflammatory cytokine IL-17A constitutes an alternative and efficacious mechanism of action for the treatment of these immune-mediated inflammatory diseases.Citation44 In 2015, secukinumab received market authorization in Europe for the treatment of adult patients with moderate-to-severe plaque psoriasis (300 mg), active PsA (150/300 mg), and active AS (150 mg), offering a new treatment option for these diseases and being the first non-TNF biologic for AS.Citation44 Indeed, secukinumab is currently the only non-TNF biologic that is approved in all three indications. Ixekizumab, an IgG4 monoclonal antibody L-17A inhibitor, has been recently authorized for use in adults with active PsA in addition to moderate-to-severe plaque psoriasis patients.Citation45
Secukinumab has been shown to have significant efficacy in the treatment of moderate-to-severe psoriasis,Citation46 PsA,Citation47 and AS,Citation48 demonstrating a rapid onset of action and sustained responses with a consistent safety profile, according to the results of several phase three clinical trials both vs placebo and comparators.Citation46–Citation54 In addition to its clinical value, secukinumab has been reported as a dominant or cost-effective treatment option compared to other biologics in multiple economic evaluations for the three indications.Citation55–Citation59 However secukinumab, being a biologic drug, is a costly treatment option and, in a context of limited resources, it is necessary to evaluate sustainability of its use.
This analysis aimed to estimate the budget impact of the introduction of secukinumab to the Italian market for the three indications (psoriasis, PsA and AS) over a 3-year time horizon from the perspective of Italian National Health Service (INHS).
Materials and methods
A cross-indication budget impact analysis (BIA) was developed by means of a dynamic simulation model in Microsoft Excel®. The model evaluated the budgetary impact of introducing secukinumab into the current approved and reimbursed treatments for moderate-to-severe psoriasis, active PsA, and active AS in Italy. The analysis was carried out from the perspective of the INHS over a 3-year timeframe. The model was populated with data available from literature and market research; therefore, no institutional review board or ethics committee approval was required. Model inputs included epidemiology data, current and future market share projections for treatments, data on resource use and on the following cost items (expressed in 2017 euros): drug therapy costs, administration costs, disease-related costs (resource use and associated costs), and adverse event (AE)-related costs.
Modeling framework
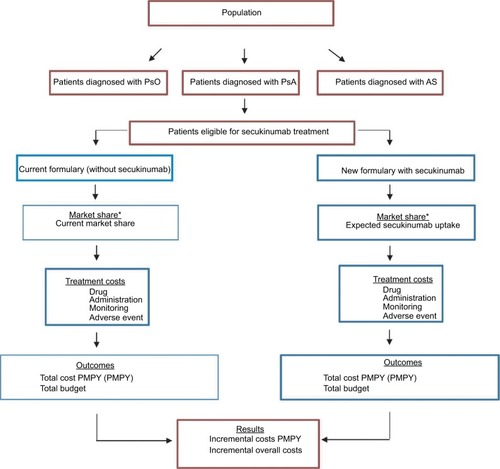
The budget impact model compared two different scenarios: 1) without secukinumab introduction (where secukinumab is not available as an alternative biologic treatment for psoriasis, PsA, and AS patients and 2) with the introduction of secukinumab (where secukinumab is available as an alternative biologic treatment for psoriasis, PsA, and AS patients, and secukinumab market share changes over time. The model compares the costs of the current and expected psoriasis, PsA, and AS treatment options over 3 years. The treatment regimens that were modeled included market shares of approved treatments including biosimilars (etanercept and infliximab biosimilars) and expected market shares after introduction of secukinumab to the market. For each licensed treatment, the indication-specific posology was taken from the summary of product characteristics from the European Medicines Agency (see ).
For each disease, BIA was conducted for the first 3 years after secukinumab introduction. The total annual cost was obtained for each scenario, and the budget impact was estimated as the difference between the two scenarios, without and with secukinumab introduction into the Italian market, for the eligible population. Results are presented for all three indications combined and for each of the indications taken individually. The modeling framework and methods are consistent with the recommendations made by the International Society for Pharmacoeconomics and Outcomes Research’s Task Force on Good Research Practices and are presented in .Citation60,Citation61
Figure 1 Model structure.
Abbreviations: AS, ankylosing spondylitis; BIA, budget impact analysis; ISTAT, Italian National Statistical Institute; PMPY, per Member per Year; PsA, psoriatic arthritis; PsO, psoriasis.
Model input data
Patient population and market shares
The size of initial population was based on national epidemiological data derived from Italian National Statistical Institute. Adult patients (aged ≥18 years) diagnosed with psoriasis, PsA, and AS and currently treated with a biologic treatment were included in the BIA. The number of current psoriasis, PsA, and AS patients treated with different biologic drugs was obtained from the market share data.Citation62 The model also accounted for the incidence and new treatment starters for each indication. In order to estimate the number of patients treated over 3 years, yearly future growth rates of 17%, 10%, and 12% for psoriasis, PsA, and AS, respectively, were used on the basis of market research findings. shows the input data on eligible population and market growth. Based on dynamic market research, 30% of patients were assumed as biologic-naïve patients.Citation62 Detailed psoriasis, PsA, and AS population projections for both scenarios (with and without secukinumab) over the 3 years and the respective changing market share for all treatments are shown in –.
Table 2 Model input data on population
Costs
Only direct costs of the treatments were considered, including drugs costs, administration costs associated with intravenous (IV) infusions, disease-related costs (resource use and associated costs: non-biologic drugs, physician visits, emergency room visits, phototherapy), and AE costs.
Drugs costs
Drug acquisition costs were derived from official national price lists, and ex-factory prices were used (with −5%, −5% mandatory rebates). Induction and maintenance periods for each drug were taken into account in calculating drug costs. For the doses and administration schedules, summary of product characteristics was used. shows the doses and cost per dose for the biologic treatments as well as apremilast, and concomitant non-biologic treatments. For infliximab, the dose of drug to be administered is established on the basis of the patient’s weight, and in our analysis it was obtained by considering the mean patients’ weight in the three indications (88.54 kg for psoriasis, 87.11 kg for PsA, and 81.57 kg for AS)
Table 3 Doses and cost per dose for the biologic treatments as well as apremilast, and concomitant non-biologic treatments
No additional administration costs were considered for subcutaneous treatments, while for IV treatment (infliximab and its biosimilar), estimated administration cost per infusion was about €291 (discounted in 2017).Citation63,Citation64
Resource use and associated costs
To estimate the resource use impact for each indication, the proportion of patients requiring health care interventions along with the frequency were obtained. To estimate these costs, the unit costs were multiplied by the frequency and proportion of patients. Unit costs for each included item are available in .
AE costs
AEs such as serious infections, non-melanoma skin cancer (NMSC), and malignancies other than NMSC were considered by individual event rates (see ). Costs per event, obtained from National Diagnosis-Related Group tariffs (DRG 89, 284, 414), were €3,185, €773, and €2,194 for serious infections, NMSC, and malignancy other than NMSC, respectively.Citation65
Sensitivity and scenario analyses
To assess the robustness of results, a one-way sensitivity analysis was performed by changing the following parameters by ±10%: secukinumab cost, secukinumab market share, IV administration costs, and AE costs. Moreover, in order to quantify the impact of a larger uptake of secukinumab in PsA and AS biologic-naïve patients, we carried out a scenario with twice as many PsA and AS biologic-naïve patients starting with secukinumab (60% compared to 30% in base case).
Results
Patients on secukinumab
Combining all three indications (psoriasis, PsA, and AS), the total patient population in Italy treated with secukinumab over the 3-year timeframe was projected to be 6,648 in the first year, 10,042 in the second year, and 12,001 in the third year. Results are shown in detail in .
Budget impact analysis
Overall population
The introduction of secukinumab in Italy in psoriasis, PsA, and AS indications (all three combined) resulted in cumulative savings of 5% over the 3-year period, compared to the scenario without secukinumab in market (). This corresponds to per patient savings of about €1,855 and overall population savings of €66.1 million over the 3 years. The major proportion of cost savings was contributed by the adoption of secukinumab in AS (58%), followed by PsA (29%) and psoriasis (13%).
Table 4 Budget impact results in the overall population (psoriasis, PsA, AS)
Psoriasis
The introduction of secukinumab for moderate–severe plaque psoriasis treatment resulted in savings of 1% in the first year and 2% for the second and third year, compared to the scenario without secukinumab in market (). These correspond to savings of €1.9 million in the first year and savings increase in the following years, with €2.9 million and €3.5 million in the second and third years, respectively. The cumulative budget impact of introducing secukinumab is estimated to yield savings of €8.3 million over the 3-year period (). The cost savings per patient was €132 in the first year, €238 in the third year, and the cumulative result per patient was €568 over 3 years.
Table 5 Budget impact results in psoriasis, PsA and AS populations
Psoriatic arthritis
The introduction of secukinumab for the treatment of PsA reveals savings of 2% in the first year, 4% in the second year, and 5% in the third year, compared to the scenario without secukinumab in market. These correspond to savings of €4.1 million in the first year and savings increase in the following years, with €7 million and €8.2 million in the second and third years, respectively. The cumulative budget impact of introducing secukinumab is estimated to yield savings of €19.3 million over the 3-year period (). Cost savings per patient were €329 in the first year, increasing to €645 in the third year with the cumulative per patient savings of €1,527 over 3 years.
Ankylosing spondylitis
The introduction of secukinumab for treatment of AS reveals savings of 8% in the first year, 13% in the second year, and 16% in the third year, compared to the scenario without secukinumab in market. These correspond to savings of €8.4 million in the first year and savings increase in the following years, with €13.4 million and €16.7 million in the second and third years, respectively. The cumulative budget impact of introducing secukinumab is estimated to yield savings of €38.5 million over the 3-year period (). Per patient cost results showed savings of €1,010 in the first year, which increased to €1,968 in the third year with the cumulative per patient savings of €4,568 over 3 years.
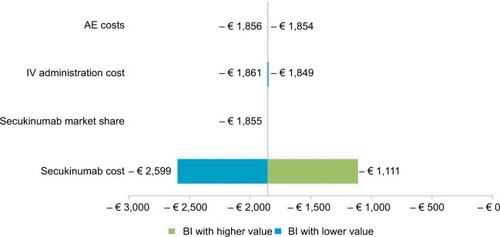
Sensitivity and scenario analyses
In , a tornado diagram shows one-way sensitivity analysis results for the overall population scenario (com bining patients with all three indications). This analysis demonstrated that budget impact results were most sensitive to change in secukinumab cost and the cost of secukinumab was the main cost driver in the analysis.
Figure 3 Tornado diagram for the sensitivity analysis results: ±10% variation of parameters in the overall per member BI scenario.
Abbreviations: AE, adverse event; BI: budget impact; IV, intravenous.
To assess the impact of a potential growth of biologic-naïve patients, twice the number of secukinumab AS and PsA biologic-naïve patients was assumed compared to that in base case scenario (in base case, 30% of PsA and AS eligible patients were biologic-naïve). With regard to combined PsA and AS population, the increase in biologic-naïve patients resulted in incremental cumulative savings of about €27.7 million over 3 years against base case scenario (€93.8 vs €66.1 million), as shown in .
Table 6 BIA results: base case vs twice PsA and AS biologic-naïve patients starting with secukinumab (150 mg secukinumab uptake)
The increase of PsA biologic-naïve population led to incremental cumulative savings of €16.2 million over the 3 years against base case scenario (€35.5 vs €19.3 million). Therefore, the market share assumed for secukinumab changed from 14.4%, 24.7%, and 30.9% in base case to 18.7%, 32.1%, and 40.2% in the first, second, and third year, respectively. With regard to AS population, the increase in biologic-naïve patients resulted in incremental cumulative savings of €11.5 million over the 3 years against base case scenario (€50 vs €38.5 million). In this case, market share for secukinumab 150 mg changed from 15.9%, 25.2%, and 31.1% in base case to 20.6%, 32.8%, and 40.5% in the first, second, and third year, respectively.
Discussion
This analysis demonstrated considerable cost savings for INHS with the introduction of secukinumab in the market for the treatment of moderate-to-severe plaque psoriasis, PsA, and AS. Considering total direct medical costs from the INHS perspective, cumulative savings resulted to about €66.1 million after 3 years of secukinumab introduction. The highest savings were observed in AS patients (€38.5 million), followed by PsA (€19.3 million) and psoriasis (€8.3 million) patients. Within a fixed health care budget, such savings with the introduction of secukinumab could allow treatment of more patients with psoriasis, PsA, and AS in Italy. Potentially with these aforementioned savings, approximately an additional 5,925 patients (230 for psoriasis, 392 for PsA, and 5,302 for AS) could be treated. Sensitivity analyses confirmed the base case findings in most cases, and secukinumab cost was found to be the main cost driver in the analysis. As revealed in alternative scenario analysis, the savings could potentially increase if secukinumab would be used more in biologic-naïve AS and PsA patients, thus providing a better cost-saving treatment. In view of the strong clinical and comparative evidence provided by several randomized controlled trials supporting the efficacy and safety of secukinumab for psoriasis, PsA, and AS treatment,Citation46,Citation48–Citation54,Citation66–Citation69 this analysis showed the budget impact of the introduction of secukinumab from the INHS perspective.
The budget impact model results presented in this analysis were consistent with other recent studies available in literature from different countries. Duteil et alCitation70 assessed the budget impact of the introduction of secukinumab for patients with moderate-to-severe psoriasis, AS, and PsA in France. This analysis demonstrated that secukinumab utilization led to savings of €83.6 million over a 6-year time period. Halliday et alCitation71 estimated the budget impact of introduction of secukinumab in the UK in patients with AS. The cumulative budget savings over a 5-year period were estimated to be €49.2 million.
There are few limitations of this analysis. Outcomes of the analysis are based on population and market share projections. Some input data were not available to Italian context, and when not available, data from other countries or assumptions were entered into the model. Furthermore, there could be a limit in the identification of the target population, as the model has considered separately the psoriasis, PsA, and AS populations, and there is lack of studies able to provide information regarding patients on treatment with simultaneous presence of these diseases.
The BIA, according to the INHS perspective, included only direct costs. In view of the huge impact on work productivity of these diseases, potential savings could be higher if we had included indirect costs as well. Therefore, it would be interesting to plan further analyses taking into account total costs to define the composition of direct and indirect costs and the real burden on patients and the Italian society. Although the robustness of results was confirmed by sensitivity analysis, real-world evidence could further confirm our assumptions and results in future.
In conclusion, this analysis demonstrated that secukinumab is a cost-saving option for INHS when introduced for psoriasis, PsA, and AS treatment, particularly cost-savings was the highest in AS and PsA patients.
Authors contributions
SMJ and PG designed the original model framework. SDM adapted the model to the Italian perspective. GLC reviewed and validated the model adaptation and wrote the manuscript. CM supported the model adaptation and in writing the manuscript. MN interpreted the data and decided on manuscript content and structure. GMB supervised the project and helped in writing the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank Alessandro Roccia from Novartis Pharma Italy, Martina Oselin and M Chiara Valentino from S.A.V.E. Research Center, and Niraj Modi from Novartis Healthcare Private Limited, Hyderabad for editorial writing support. This analysis was funded by Novartis Pharma S.p.A., Origgio, Italy.
Supplementary materials
Table S1 PsO population without and with secukinumab over a 3-year horizon and respective change in market share for treatments
Table S2 PsA population without and with secukinumab over a 3-year horizon and respective change in market share for treatments
Table S3 AS population without and with secukinumab over a 3-year horizon and respective change in market share for treatments
Table S4 Resource use and costs associated with PsO, PsA, and AS treatment
Table S5 Annual rates of adverse events associated with PsO, PsA, and AS treatment
References
- Italian National Formulary 2015 (physician visit)2015 Available from: www.mattoni.salute.gov.it/mattoni/documenti/11_Valutazi-one_costi_dell_emergenza.pdf (ER visit)Accessed March 25, 2018
- De CompadriPKolevaDI costi della psoriasis vulgaris nei pazienti sottoposti a terapia sistemica: una rassegna della letteratura e una stima preliminare di costo in Italia [The costs of psoriasis vulgaris in patients receiving systemic therapy: a review of the literature and a preliminary cost estimate in Italy]Quaderni di farmaco economia20086715
- National Clinical Guideline CentreNational Institute for Health and Clinical Excellence: GuidancePsoriasis: Assessment and Management of PsoriasisLondonRoyal College of Physicians (UK)2012
- GreenbergJDPalmerJBLiYHerreraVTsangYLiaoMHealthcare resource use and direct costs in patients with ankylosing spondylitis and psoriatic arthritis in a large US cohortJ Rheumatol2016431889626628601
- McInnesIBMeasePJKirkhamBSecukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, Phase 3 trialLancet201538699991137114626135703
- BaetenDSieperJBraunJSecukinumab, an interleukin-17A inhibitor, in ankylosing spondylitisN Engl J Med2015373262534254826699169
- van de KerkhofPCGriffithsCEReichKSecukinumab long-term safety experience: a pooled analysis of 10 Phase II and III clinical studies in patients with moderate to severe plaque psoriasisJ Am Acad Dermatol20167518398.e8427180926
- BurmesterGRPanaccioneRGordonKBMcIlraithMJLacerdaAPAdalimumab: long-term safety in 23 458 patients from global clinical trials in rheumatoid arthritis, juvenile idiopathic arthritis, ankylosing spondylitis, psoriatic arthritis, psoriasis and Crohn’s diseaseAnn Rheum Dis201372451752422562972
- MeasePJFleischmannRDeodharAAEffect of certolizumab pegol on signs and symptoms in patients with psoriatic arthritis: 24-week results of a Phase 3 double-blind randomised placebo-controlled study (RAPID-PsA)Ann Rheum Dis2014731485523942868
- LandeweRBraunJDeodharAEfficacy of certolizumab pegol on signs and symptoms of axial spondyloarthritis including ankylosing spondylitis: 24-week results of a double-blind randomised placebo-controlled Phase 3 studyAnn Rheum Dis2014731394724013647
- SterryWOrtonneJPKirkhamBComparison of two etanercept regimens for treatment of psoriasis and psoriatic arthritis: PRESTA randomised double blind multicentre trialBMJ2010340c14720124563
- BraunJvan der Horst-BruinsmaIEHuangFClinical efficacy and safety of etanercept versus sulfasalazine in patients with ankylosing spondylitis: a randomized, double-blind trialArthritis Rheum20116361543155121630245
- KavanaughAvan der HeijdeDMcInnesIBGolimumab in psoriatic arthritis: one-year clinical efficacy, radiographic, and safety results from a Phase III, randomized, placebo-controlled trialArthritis Rheum20126482504251722378566
- BraunJDeodharAInmanRDGolimumab administered subcutaneously every 4 weeks in ankylosing spondylitis: 104-week results of the GO-RAISE studyAnn Rheum Dis201271566166722012970
- RitchlinCRahmanPKavanaughAEfficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the Phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trialAnn Rheum Dis201473699099924482301
- ToriiHNakagawaHJapanese Infliximab Study investigatorsInflix-imab monotherapy in Japanese patients with moderate-to-severe plaque psoriasis and psoriatic arthritis. A randomized, double-blind, placebo-controlled multicenter trialJ Dermatol Sci2010591404920547039
- BraunJDeodharADijkmansBEfficacy and safety of infliximab in patients with ankylosing spondylitis over a two-year periodArthritis Rheum20085991270127818759257
- KavanaughAMeasePJGomez-ReinoJJTreatment of psoriatic arthritis in a Phase 3 randomised, placebo-controlled trial with apremilast, an oral phosphodiesterase 4 inhibitorAnn Rheum Dis20147361020102624595547
- MeasePJMcInnesIBKirkhamBSecukinumab inhibition of interleukin-17A in patients with psoriatic arthritisN Engl J Med2015373141329133926422723
Disclosure
GLC, GMB, CM, and SDM are employees of S.A.V.E. S.r.l and consultants for Novartis. SMJ is an employee and shareholder of Novartis Pharma AG, Basel, Switzerland. PG is an employee of Novartis Product Life Cycle Services-NBS, Novartis Healthcare Private Limited, Hyderabad, India. MN is an employee of Novartis Pharma, Origgio, Italy. The authors report no other conflicts of interest in this work.
References
- de KorteJMombersFMCBosJDSprangersMAGQuality of life in patients with psoriasis: a systematic literature reviewJ Investig Dermatol Symp Proc200492140147
- SwHHoltEWHusniMEQureshiAAWillingness-to-pay stated preferences for 8 health-related quality-of-life domains in psoriatic arthritis: a pilot studySemin Arthritis Rheum201039538439719095293
- HustedJAThavaneswaranAChandranVGladmanDDIncremental effects of comorbidity on quality of life in patients with psoriatic arthritisJ Rheumatol20134081349135623772076
- GratacósJDaudénEGómez-ReinoJMorenoJCCasado MiguelÁngelRodríguez-ValverdeVHealth-related quality of life in psoriatic arthritis patients in SpainReumatol Clín2014101253124099960
- BoehnckeW-HSchönMPPsoriasisLancet2015386999798399426025581
- GargNvan den BoschFDeodharAThe concept of spondyloarthritis: Where are we now?Best Pract Res Clin Rheumatol201428566367225488776
- HuscherDMerkesdalSThieleKCost of illness in rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis and systemic lupus erythematosus in GermanyAnn Rheum Dis20066591175118316540552
- FrankeLCAmentAJvan de LaarMABoonenASeverensJLCost-of-illness of rheumatoid arthritis and ankylosing spondylitisClin Exp Rheumatol2009274 Suppl 55S11812319822057
- ParisiRSymmonsDPMGriffithsCEMAshcroftDMGlobal epidemiology of psoriasis: a systematic review of incidence and prevalenceJ Invest Dermatol2013133237738523014338
- GudjonssonJEJohnstonASigmundsdottirHValdimarssonHImmunopathogenic mechanisms in psoriasisClin Exp Immunol200413511814678257
- FarleyEMenterAPsoriasis: comorbidities and associationsG Ital Dermatol Venereol2011146191521317853
- MeasePJArmstrongAWManaging patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasisDrugs201474442344124566842
- SalvadoriniGBandinelliFdelle SedieAAnkylosing spondylitis: how diagnostic and therapeutic delay have changed over the last six decadesClin Exp Rheumatol201230456156522510360
- RudwaleitMHaibelHBaraliakosXThe early disease stage in axial spondylarthritis: Results from the German spondyloarthritis inception cohortArthritis Rheumatol2009603717727
- SchettGLoriesRJD’AgostinoM-AEnthesitis: from pathophysiology to treatmentNat Rev Rheumatol2017131273174129158573
- ZengQChenRDarmawanJRheumatic diseases in ChinaArthritis Res Ther2008101R1718237382
- HoffMGulatiAMRomundstadPRKavanaughAHaugebergGPrevalence and incidence rates of psoriatic arthritis in central Norway: data from the Nord-Trøndelag Health Study (HUNT)Ann Rheum Dis2015741606423962458
- AkkocNAre spondyloarthropathies as common as rheumatoid arthritis worldwide? A reviewCurr Rheumatol Rep200810537137818817640
- HazardECherrySBLallaDWoolleyJMWilfehrtHChiouCFClinical and economic burden of psoriasisManag Care Interface20061942026
- MdefspdeOliveiraBdeoRochaDuarteGVPsoriasis: classical and emerging comorbiditiesAn Bras Dermatol201590192025672294
- GhatnekarOLjungbergAWirestrandLESvenssonACosts and quality of life for psoriatic patients at different degrees of severity in southern Sweden – a cross-sectional studyEur J Dermatol201222223824522361745
- BergerKEhlkenBKuglandBAugustinMCost-of-illness in patients with moderate and severe chronic psoriasis vulgaris in GermanyJ Dtsch Dermatol Ges20053751151815967010
- LevyARDavieAMBrazierNCEconomic burden of moderate to severe plaque psoriasis in CanadaInt J Dermatol201251121432144023171010
- PooleCDLebmeierMAraRRafiaRCurrieCJEstimation of health care costs as a function of disease severity in people with psoriatic arthritis in the UKRheumatology201049101949195620581376
- BoonenADirect costs of ankylosing spondylitis and its determinants: an analysis among three European countriesAnn Rheum Dis200362873274012860728
- KobeltGAndlin-SobockiPMaksymowychWPCosts and quality of life of patients with ankylosing spondylitis in CanadaJ Rheumatol200633228929516465660
- ColomboGModerate and severe plaque psoriasis: cost-of-illness study in ItalyTher Clin Risk Manag20084255956818728854
- OlivieriIde PortuSSalvaraniCThe psoriatic arthritis cost evaluation study: a cost-of-illness study on tumour necrosis factor inhibitors in psoriatic arthritis patients with inadequate response to conventional therapyRheumatology200847111664167018725374
- ConaghanPAltenRStrandVThe relationship between physical functioning and work for people with psoriatic arthritis: results from a large real-world study in 16 countries [Abstract 1712]Arthritis Rheumatol201668Suppl 10
- CortesiPAScaloneLD’AngiolellaLSystematic literature review on economic implications and pharmacoeconomic issues of psoriatic arthritisClin Exp Rheumatol2012304 Suppl 73S12613123072771
- AltobelliEMaccaroneMPetrocelliRAnalysis of health care and actual needs of patients with psoriasis: a survey on the Italian populationBMC Public Health2007715917448249
- Burgos-PolRMartínez-SesmeroJMVentura-CerdáJMElíasICalotoMTCasadoMÁ. The cost of psoriasis and psoriatic arthritis in 5 European countries: a systematic reviewActas Dermosifiliogr2016107757759027316590
- WilliamsEMWalkerRJFaithTEgedeLEThe impact of arthritis and joint pain on individual healthcare expenditures: findings from the Medical Expenditure Panel Survey (MEPS), 2011Arthritis Res Ther20171913828245879
- RamondaRMarchesoniACarlettoAPatient-reported impact of spondyloarthritis on work disability and working life: the ATLANTIS surveyArthritis Res Ther20161817827037139
- SmolenJSSchölsMBraunJTreating axial spondyloarthritis and peripheral spondyloarthritis, especially psoriatic arthritis, to target: 2017 update of recommendations by an international task forceAnn Rheum Dis201877131728684559
- AvedeCarvalhoRomitiRCdasSouzaPsoriasis comorbidities: complications and benefits of immunobiological treatmentAn Bras Dermatol201691678178928099601
- MrowietzUImplementing treatment goals for successful long-term management of psoriasisJ Eur Acad Dermatol Venereol201226Suppl 3122022356631
- NorlinJMSteen CarlssonKPerssonUSchmitt-EgenolfMSwitch to biological agent in psoriasis significantly improved clinical and patient-reported outcomes in real-world practiceDermatology2012225432633223328678
- SmithCHJabbar-LopezZKYiuZZBritish Association of Dermatologists guidelines for biologic therapy for psoriasis 2017Br J Dermatol2017177362863628513835
- GossecLSmolenJSRamiroSEuropean League Against Rheumatism (EULAR) recommendations for the management of psoriatic arthritis with pharmacological therapies: 2015 updateAnn Rheum Dis201675349951026644232
- CoatesLCKavanaughAMeasePJGroup for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 treatment recommendations for psoriatic arthritisArthritis Rheumatol20166851060107126749174
- WardMMDeodharAAklEAAmerican College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network 2015 recommendations for the treatment of ankylosing spondylitis and nonradiographic axial spondyloarthritisArthritis Rheumatol201668228229826401991
- van der HeijdeDRamiroSLandewéR2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritisAnn Rheum Dis201776697899128087505
- Cosentyx Summary of Product Characteristics Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/003729/WC500183132.pdfAccessed March 25, 2018
- Taltz – update from EMA regarding adoptation of new indication for Taltz2017 Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Summary_for_the_public/human/003729/WC500183132.pdfAccessed March 25, 2018
- LangleyRGElewskiBELebwohlMSecukinumab in plaque psoriasis – results of two Phase 3 trialsN Engl J Med Overseas Ed20143714326338
- MeasePJMcinnesIBKirkhamBSecukinumab Inhibition of Interleukin-17A in Patients with Psoriatic ArthritisN Engl J Med Overseas Ed20153731413291339
- BaetenDSieperJBraunJSecukinumab, an interleukin-17A inhibitor, in ankylosing spondylitisN Engl J Med Overseas Ed20153732625342548
- ThaçiDBlauveltAReichKSecukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trialJ Am Acad Dermatol201573340040926092291
- StrandVMeasePGossecLSecukinumab improves patient-reported outcomes in subjects with active psoriatic arthritis: results from a randomised Phase III trial (FUTURE 1)Ann Rheum Dis201776120320727169431
- McinnesIBMeasePJKirkhamBSecukinumab, a human anti-interleukin-17A monoclonal antibody, in patients with psoriatic arthritis (FUTURE 2): a randomised, double-blind, placebo-controlled, Phase 3 trialLancet201538699991137114626135703
- McinnesIBMeasePJRitchlinCTSecukinumab sustains improvement in signs and symptoms of psoriatic arthritis: 2 year results from the Phase 3 FUTURE 2 studyRheumatology201756111993200328968735
- DeodharAADougadosMBaetenDLEffect of secukinumab on patient-reported outcomes in patients with active ankylosing spondylitis: a Phase III randomized trial (MEASURE 1)Arthritis Rheumatol201668122901291027390130
- SieperJDeodharAMarzo-OrtegaHSecukinumab efficacy in anti-TNF-naive and anti-TNF-experienced subjects with active ankylosing spondylitis: results from the MEASURE 2 studyAnn Rheum Dis201776357159227582421
- PuigLNotarioJJiménez-MoralesASecukinumab is the most efficient treatment for achieving clear skin in psoriatic patients: a cost-consequence study from the Spanish National Health ServiceJ Dermatolog Treat201728762363028784002
- GoereeRChiva-RazaviSGundaPCost-effectiveness analysis of secukinumab for the treatment of active psoriatic arthritis: a Canadian perspectiveJ Med Econ201821216317328945143
- D’AusilioAAielloADanielFGrahamCRocciaAToumiMA cost-effectiveness analysis of secukinumab 300 mg vs current therapies for the treatment of moderate to severe plaque psoriasis in ItalyValue Health2015187A424
- LeeAGregoryVGuQBeckerDLBarbeauMCost-effectiveness of secukinumab compared to current treatments for the treatment of moderate to severe plaque psoriasis in CanadaValue Health2015183A182
- Costa-ScharplatzMLangAGustavssonAFasthACost-effectiveness of secukinumab compared to ustekinumab in patients with psoriasis from a Swedish health care perspectiveValue Health2015187A422
- MauskopfJASullivanSDAnnemansLPrinciples of good practice for budget impact analysis: report of the ISPOR Task Force on good research practices – budget impact analysisValue Health200710533634717888098
- SullivanSDMauskopfJAAugustovskiFBudget impact analysis – principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task ForceValue Health201417151424438712
- IMS Health Data ProcessingNovartis2016
- FavalliEGMarchesoniAColomboGLSinigagliaLPattern of use, economic burden and vial optimization of infliximab for rheumatoid arthritis in ItalyClin Exp Rheumatol2008261455118328146
- De CompadriPKolevaDI costi della psoriasis vulgaris nei pazienti sottoposti a terapia sistemica: una rassegna della letteratura e una stima preliminare di costo in Italia [The costs of psoriasis vulgaris in patients receiving systemic therapy: a review of the literature and a preliminary cost estimate in Italy]Quaderni di farmaco economia20086715
- Ministry of Health Tariffs of acute hospital care services [DRG tariffs]Official Journal of the Italian Republic. Series N.23; Supplement 8 of 28 January 2013 Available from: http://www.salute.gov.it/portale/temi/p2_6.jsp?lingua=italiano&id=1349&area=ricoveriOspedalieri&menu=sistemaAccessed March 25, 2018
- NashPMcinnesIMeasePSecukinumab for the treatment of psoriatic arthritis: comparative effectiveness versus adalimumab using a matching-adjusted indirect comparisonArthritis Rheumatol201668Suppl 10
- McinnesIBNashPRitchlinCTHU0437 secukinumab for the treatment of psoriatic arthritis: comparative effectiveness results versus licensed biologics and apremilast from a network meta-analysisAnn Rheum Dis201675Suppl 234834925433020
- HaweEVickersADMallyaUGMcBrideDWCapkun-NiggliGOlsonMSecukinumab 300 mg demonstrates highest probability of efficacy than other biologics in psoriasis: indirect comparisonPaper presented as a poster at the 23rd European Academy of Dermatology and Venereology CongressOctoberAmsterdam, the Netherlands2014
- BaetenDMeasePStrandVSAT0390 secukinumab for the treatment of ankylosing spondylitis: comparative effectiveness results versus currently licensed biologics from a network meta-analysisAnn Rheum Dis201675Suppl 2809810
- DuteilERachdiLCariouCBudget impact analysis of secukinumab in moderate to severe plaque psoriaris, ankylosing spondylitis and psoriatic arthritis In FranceValue in Health2016197A458
- HallidayAHackingVJuglSMBudget impact of secukinumab for ankylosing spondylitis in the UKValue in Health2016197A535
- Italian Republic Official Gazette Available from: http://www.gazzettauf-ficiale.it/ricerca/atto/serie_generale/originario?reset=true&normativi=falseAccessed March 25, 2018
- SaracenoRMannheimerRChimentiSRegional distribution of psoriasis in ItalyJ Eur Acad Dermatol Venereol200822332432918269600
- KhalidJMGlobeGFoxKMChauDMaguireAChiouC-FTreatment and referral patterns for psoriasis in United Kingdom primary care: a retrospective cohort studyBMC Dermatol2013131923957883
- de AngelisRSalaffiFGrassiWPrevalence of spondyloarthropathies in an Italian population sample: a regional community-based studyScand J Rheumatol2007361142117454930