Abstract
Background and aims
The total health care cost for human immunodeficiency virus (HIV) patients has constantly grown in recent years. To date, there is no information about how this trend will behave over the next few years. The aim of the present study is to define a pharmacoeconomic model for the forecast of the costs of a group of chronically treated patients followed over the period 2004–2009.
Methods
A pharmacoeconomics model was built to describe the probability of transition among different health states and to modify the therapy over time. A Markov model was applied to evaluate the temporal evolution of the average cost. The health care resources exploited during hospitalization were analyzed by using an “activity-based costing” method.
Results
The Markov model showed that the mean total cost, after an initial increase, tended to remain stable. A total of 20 clinical records were examined. The average daily cost for each patient was EUR 484.42, with a cost for admission of EUR 6781.88.
Conclusion
The treatment of HIV infection in compliance with the guidelines is also effective from the payer perspective, as it allows a good health condition to be maintained and reduces the need and the costs of hospitalizations.
Introduction
Out of the nearly 150,000 people who live with human immunodeficiency virus (HIV) infection in Italy, about 25,000 have full-blown disease. Although the epidemiologic trend of HIV infection shows a significant decrease, a small but constant number of new cases is diagnosed every year.Citation1
Since 1996, highly active antiretroviral therapy (HAART) has changed the clinical course of HIV infection, reducing the rate of disease progression, incidence of opportunistic infections, and mortality. This prolonged survival has turned HIV infection into a chronic disease. This change has caused a constant shift of the economic resources needed to treat HIV infection from the hospital to outpatient management. The economic impact of HIV infection is well acknowledged, and it mainly includes the use of health care services for the treatment of HIV infection, the treatment of acquired immunodeficiency syndrome (AIDS)-associated symptoms and opportunistic infections, and the indirect costs associated with morbidity and premature death of working-age patients.Citation2,Citation3
In Italy, inpatient and outpatient specialist services are funded according to a prospective per case payment system based on a regional fee plan. The reimbursement provided for outpatient activities is based on national price lists. Each region can choose whether to adopt the national rate of reimbursement or determine its own rate, as in the case of the Lombardy Regional Healthcare System (RHS). This is calculated taking into account the production costs (time and resources) and the strategic priorities of the Regional Social Services and Health Care Plan, which are updated yearly.Citation4
The amount to be paid by the RHS for hospital admissions is determined using the diagnosis-related group (DRG) system (International Classification of Diseases, Ninth Revision, Clinical Modification), introduced in Italy in 1995. A specific weight, which takes into account the composition of the procedures delivered by the providers, is assigned to each region and updated every year. Such weight is used to calculate the regional diagnosis-related group rate of reimbursement.
The Lombardy region is the most populated of the 20 Italian regions, with more than 15% of the whole Italian population, and has the highest prevalence of AIDS cases in Italy, which has a strong impact on the regional health care budget.
From 2001 to 2008, there have been more than 3500 new HIV cases diagnosed in Lombardy, with a high prevalence (70%) within males. The majority of patients were diagnosed with an advanced phase of the disease.Citation4 Recently, the health authorities of the Lombardy region organized a survey aimed at the characterization of the epidemiological features of new HIV cases. A total of 472 new HIV subjects have been identified showing a high prevalence of heterosexual exposure as a risk factor. These epidemiological data confirm that facing HIV remains a priority for health care organizations and that a specific strategy needs to be implemented.Citation2
In Lombardy, HAART therapies can be delivered only inside the hospitals. The provider is refunded with the same amount the RHS paid at the moment of the purchase of each drug. As also reported in international studies, this amount is generally lower than the market value.Citation4
Up to now, the Regional Healthcare Service has spent more than EUR 150,000,000 to provide HIV therapy, and this amount increases by about 10% every year. In Lombardy, the total number of treated patients increased by 32.1% between 2004 and 2009. The total expenditure for the management of these subjects increased from EUR 224,902,421 to EUR 255,946,864, mostly due to the cost of the drugs, which grew from EUR 107,185,600 to EUR 137,215,086 (data from the Regional Data Base: banca Dati assistito Regione Lombardia). Previous studies have investigated the determinants of costs, consistently finding a relationship between CD4 cell count and health care expenditures.Citation5
As a matter of fact, other clinical features such as HIV viral load and hepatitis C virus coinfection may be related to costs. Moreover, although it has been shown that the total health care cost for these patients has constantly grown, there is still no information about how this trend will behave in the upcoming years, in particular with regards to chronically treated patients, who are the majority in the treated population.Citation4
Since the expenditure for the care of patients with HIV AIDS has a relevant impact on the total health budget in Italy, and its trend is currently unknown, the present study was designed to define a pharmacoeconomic model to forecast the costs of a group of chronically treated patients followed over the period 2004–2009 at the Division of Infectious and Tropical Diseases of the IRCCS Policlinico San Matteo Foundation. Because the estimate of the real cost of hospital admission is currently not evaluated, an “activity-based costing” model was used to provide a trusted measure of resources employed in this setting. The combination of these data will supply a better resource allocation to the policymaker.
Methods
A pharmacoeconomic model, and in particular a Markov model (MM),Citation6 was implemented to forecast the total expenditure trend over the next 4 years. MMs are stochastic models, where the study of a system is based on the assessment of the state of the system at a specific time stamp and of the probability of transition to a new state in the future, such transition being dependent only on the values of the current state and not on the previous history of the system up to that point (Markov property).
The six health care states of the MM were defined based on CD4 count and HIV viral load, as detailed in . Such a model takes into account the probability of:
Table 1 Health state subdivision according to CD cell count and HIV-viral load
transition among different health states over time;
modification of the therapy due to virological failure or side effects; and
use of new generation and expensive drugs.
This model will enable the number of people who will be in a specific health status at a particular time to be determined. As the total health care costs increase with the progression of the disease, the probability for a patient to change his/her health status will influence the total cost of the patient group he/she belongs to, and consequently will be related to the definition of the total resources to be employed for the management of the patients.
This model has been implemented using TreeAge Pro Suite software (TreeAge Software, Inc, Williamstown, MA).
To build the model, an evaluation of the clinical records of the patients treated at the Division of Infectious and Tropical Diseases between 2004 and 2009 was carried out. For each patient, the following data were collected:
demographics, clinical events, antiretroviral therapy;
the total cost, calculated as a sum of:
○ antiretroviral drugs cost (number of boxes per month of treatment),
○ visits cost,
○ laboratory and instrumental examinations cost (according to the price list of RHS for Lombardy),
○ nonantiretroviral therapy cost (all the drugs prescribed to the patient and collected at any provider within the Lombardy region, such as hospitals and pharmacies),
○ hospital admissions cost (DRGs reimbursement).
Costs were discounted at 2009, considering the Italian inflation rates related to the average consumer prices. Cost analyses were performed considering both the evolution of the total costs and of each cost category between 2004 and 2009. The clinical data were then analyzed to identify patient characteristics which may be related to the costs in each year.
The cohort of HIV patients followed at the outpatients division of the Divisione di Malattie Infettive e Tropicali - Fondazione IRCCS Policlinico San Matteo, Pavia was analyzed separately.
Activity-based cost of HIV-related DRGs
The analysis of the resources exploited for the assistance of patients during hospitalization (eg, the actual amount of direct costs and the estimate of indirect costs) was carried out by a retrospective analysis of the clinical records of 20 cases. The “activity-based costing” method was used, which is an accounting method that analyzes the performance process by breaking it down into multiple activities and computing the final cost as the sum of the cost of each activity. The cost of health performances can be divided into all the components cooperating in the production process.
The methodology used in this case was as follows:
Modeling of the process of care, taking into account the sequence of diagnosis, therapy, and assistance given to the hospitalized patient
Identification of the matrix of performed activities, including the knowledge on the professional figures involved. The following activities were identified:
hospital admission (administrative, medical, and nursing)
hospital stay (medical and nursing activity during hospital stay, meal and laundry costs, diagnostic procedures – both laboratory and instrumental, health-and nonhealth-related equipment costs, external consultants)
hospital discharge (administrative, medical, and nursing)
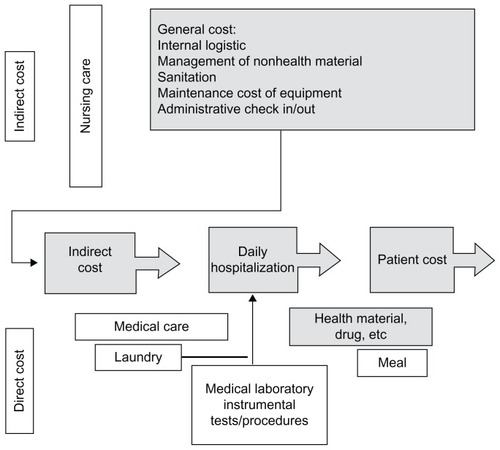
A scheme of the root used is shown in .
To quantify the cost of each activity, the following guidelines were used:
Medical and nursing assistance (whole staff cost per day of stay)
Direct cost of material and diagnostic procedures (cost/day or cost/activity – price list of RHS for Lombardy)
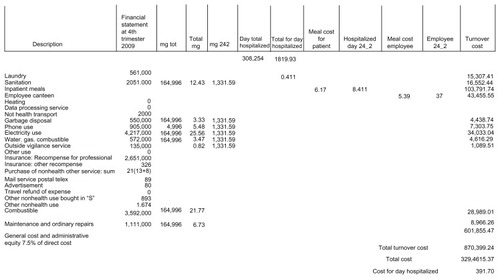
Indirect costs (calculated according to hospital cost driver, as summarized in ).
Results
Cost of antiretroviral therapy in the period 2004–2009
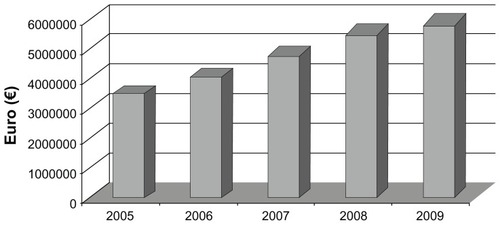
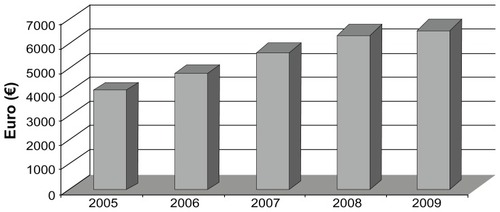
This analysis was carried out on the total cohort of patients followed at the authors’ department. During the monitored period, the total drug cost constantly increased both as a whole cost and as percentage trend. shows how the yearly incremental cost is about 17% for years 2005–2006, decreases to 5% for 2007–2008, and goes back to previous levels for 2008–2010. This trend is motivated by the increase in the number of treated patients (from 840 to 913 during the observation period) and by the use of more expensive drugs as suggested by the simultaneous growth of the average cost per patient ().
Analysis of a cohort of 200 patients
Demographics
A total of 200 subjects consecutively starting the follow-up period between 2004 and 2009 were considered for the analysis. summarizes the demographic features of the analyzed population. All patients received antiretroviral treatment during their follow-up.
Table 2 Demographic characteristics of patients analyzed by the Markov model (200 subjects)
Costs according to health state
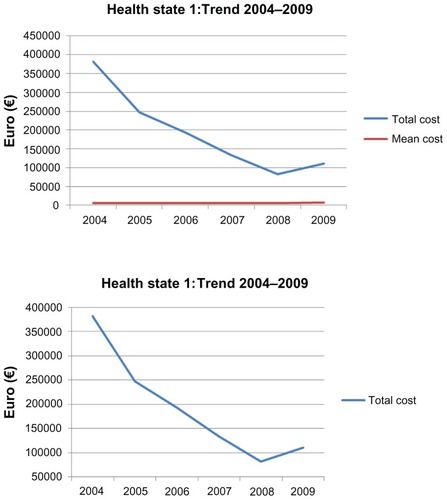
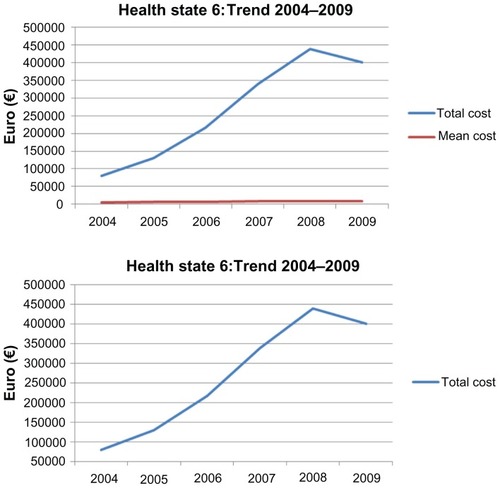
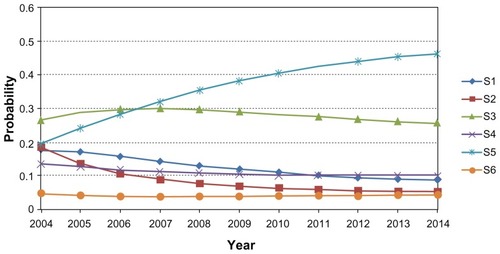
shows the distribution of the patients according to their health status. At the beginning of the observation period, the percentage of patients in state 1 was 37%, while in 2009 it dropped to 9%. At the same time, the percentage of patients in state 6 rose from 8% in 2004 to 27% in 2009, with an increase of 5% every year. reports the detailed costs related to the different considered categories, such as drugs, visits, and laboratory and instrumental tests. The total cost of each status and the average cost per patient are also reported. The transition of patients towards a better health status affects the overall cost distribution, while the average yearly cost per patient remains quite stable. The total cost of patients in state 1 decreased from EUR 328,171 (2004) to EUR 110,311 (2009), with an average cost per patient ranging from EUR 5164 (2004) to EUR 6489 (2009) (). With regards to state 6, its cost increases from EUR 80,099 in 2004 to EUR 400,374 in 2009. This is associated also with an increase in the average cost per patient, which rose from EUR 5340 to EUR 7554 ().
Table 3 Subdivision of patients according to health status
Table 4 Cost analysis for every health status, split by year
Analysis of the cost trend as forecasted by the MM
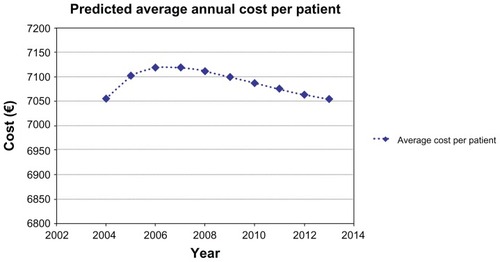
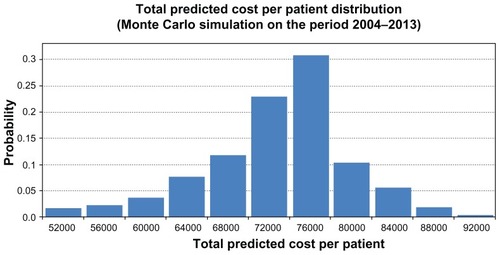
The analysis of the costs performed through an MM shows that patients have a high probability to move to a better health status along the period of observation (), while the average total cost, after an initial increase, tends to show a stable behavior (). This observation is confirmed also by a Monte Carlo simulation () showing that in a hypothetical cohort of 10,000 patients, the average cost per patient for the period 2004–2013 would range between EUR 72,000 and EUR 76,000, with a probability of more than 50% () (95% uncertainty limits, calculated by taking the 2.5th and 97.5th percentiles of the 10000 Monte Carlo simulations: [53568.17, 83865.63]).
Activity-based cost of HIV-related DRGs
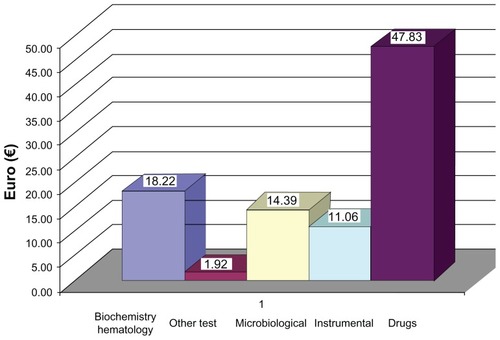
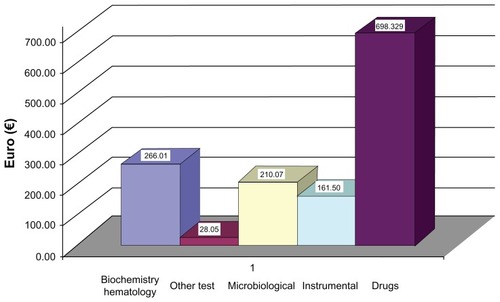
Twenty clinical records of patients admitted to hospital in the first 6 months of 2009, among those of the group analyzed by MM, have been examined, each one referring to a single hospital stay. The computation of the costs for every admission showed that the indirect costs and those related to hospital staff total EUR 391.70. shows the strategy used to evaluate the costs. Into this amount, the cost of administrative and general activities that account for the 7.5% of the total direct cost were also considered. The direct cost for each patient is computed as the sum of the costs for drugs, laboratory tests, and procedures. The cost of the drugs was assessed by multiplying the number of dispensed units (pills or vials) for each day of stay by the length of stay. The mean length of stay was 14 days. The average daily cost for each patient was EUR 485.12 (EUR 391.70 indirect cost + EUR 93.42 direct cost), with an average cost per admission of EUR 6792.88 ( and ).
Discussion
This retrospective study was designed to evaluate the temporal evolution of the resources used in HIV patient care. Since it is trivial that the increase in the number of treated patients should lead to an increase in the health care related costs, the authors herein tried to assess the costs of a cohort of chronically treated patients to forecast the amount of resources needed over the next few years to carry on their health assistance. This is particularly useful in a setting where the public RHS has to make a regular plan of the amount of future costs. It was found that the costs relating to the cohort of patients treated at the authors’ institution increased constantly over time. This is due to an increase in the number of treated patients and to the use of new and more expensive drugs. Focusing on a group of chronic patients treated for a long period of time, it was found that the costs remain substantially stable and will not show a significant growth in the future. Moreover, the patients are likely to show a transition toward a better health status. The advantages of the antiretroviral treatment are confirmed by the reduction of the hospitalization rate, shown by the decrease in the costs relating to the reimbursements for hospital admission. Also, it was also found that each day at the hospital costs about EUR 500. This amount exceeds the DRG reimbursement fee if the stay is longer than 13 days. Thus, hospitalization causes a resource use corresponding to that of a year of antiretroviral therapy.
The data in this study are consistent with those presented in other studies that demonstrate that antiretroviral therapy is cost-effective.Citation7 Schackman et al analyzed the composition of the total cost related to the treatment of HIV-positive patients in the United States. The main cost category was HAART, with a percentage impact of 73%, consistent with the findings of this present study. Fleishman et al,Citation8 who analyzed the costs of outpatient visits and inpatients activities in more than 13,000 HIV-infected adults between 2000 and 2002, found that the cost of inpatient activities decreased constantly during the period, whereas outpatient activities cost was more stable. Recently, a paper published by Rizzardini et alCitation9 showed findings similar to the present study where it was observed that an increase in HAART percentage impacts on the total cost. These authors demonstrate also that age, lower CD4 cell count, coinfection of hepatitis C virus and undetectable HIV-RNA are determinants of cost increase. These findings are very interesting, since they are related to an economic setting that is the same as that in the present study.
The present study has some limitations. First, it is a single-center study, and the results may be affected by local patient management and by the use of considered cost driver. Moreover, the number of patients is limited and cannot be considered representative of a wider sample. Finally, the different reimbursement systems within the National Health Service make the results of this study not directly comparable to those of other international studies.
Our findings should however address some indication to the payer. First, the treatment of patients in a stable clinical condition doesn’t show a trend leading to a significant increase. Second, also treating patients in an early stage of the disease allows them to be maintained in a good condition, reducing the need of hospitalization. Third, the hospital stay requires the use of massive economic resources, which increase with the length of hospitalization and exceed the reimbursement fee. Finally, the tendency to an improvement of the patients’ condition opens the way to a reduction of the nontangible costs related to HIV disease, such as productivity loss and the worsening of quality of life.
In conclusion, it can be stated that the treatment of HIV infection in compliance to the guidelines is effective also from the payer perspective, as it allows maintaining a good health condition and reducing the need and the costs of hospitalizations. This is particularly important where the resources appointed to the in-hospital care are planned to be reduced toward the use for home care strategies. Because the total expenditure for antiretroviral drugs in Italy follows only that for anticancer ones, the forecasting of how much the trend will increase is crucial to better allocate the financial resources needed to treat patients with this transmissible disease. Since the patients actually treated are in a stable condition, the focus of this study was on this category of subjects because they use the largest amount of resources. The finding of a stability of expenditure trend in these subjects, with a forecast extended until 2013, allows policymakers to plan a better allocation of health care resources, by putting new resources toward the treatment of newly diagnosed patients and new strategies of care, such as that of simplification of therapy, and, more importantly, to prevent the spread of the disease.
Disclosure
The authors report no conflicts of interest in this work.
References
- SuligoiBBorosSCamoniLLeporeD Available at: www.iss.it/binary/pres/cont/Rapporto_31_dicembre_2008.pdf
- CasariSSuligoiBCamoniLCaratteristiche comportamentali dei pazienti HIV+ di recente riscontro (Studio Nu.Di.H.) Simit 9° Congresso NazionaleNovember 24–27, 2010Rome, Italy
- SendiPPalmerAJGafniABattegayMHighly active antiretroviral therapy: pharmacoeconomic issues in the management of HIV infectionPharmacoeconomics200119770971311548908
- Regione Lombardia [homepage on the Internet]ALEE-AO – Atlante Lombardo Epidemiologico ed Economico dell’Attività Ospedaliera22012 [cited February 11, 2012]. Available from: http://www.aleeao.it/Accessed February 11, 2012
- MooreRDCost effectiveness of combination HIV therapy: 3 years laterPharmacoeconomics200017432533010947487
- SimpsonKNStrassburgerAJonesWJDietzBRajagopalanRComparison of Markov model and discrete-event simulation techniques for HIVPharmacoeconomics200927215916519254048
- SchackmanBRGeboKAWalenskyRPThe lifetime cost of current human immunodeficiency virus care in the United StatesMed Care20064499099717063130
- FleishmanJAGeboKAReillyEDHospital and outpatient health services utilization among HIV infected adults in care 2000–2002Med Care200543Suppl 91114011152
- RizzardiniGRestelliUBonfantiPThe cost of HIV disease in Northern Italy: the payer’s perspectiveJ Acquir Immune Defic Syndr20115721121721546850