?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
The present study aimed to estimate the cost of rheumatoid arthritis and its components in a university hospital-based health management organization in Argentina, during the prebiologic era.
Methods
A one-year (2002) observational prevalence, cost-of illness study of patients with rheumatoid arthritis from the societal perspective was performed in a hospital-based health management organization population. Direct medical costs were obtained using administrative databases. Direct nonmedical and indirect costs were obtained from a semistructured questionnaire. Indirect costs included work absenteeism, permanent work disability, and housework lost for housewives, using the human capital approach. Costs are expressed in 2002 US dollars per patient per year.
Results
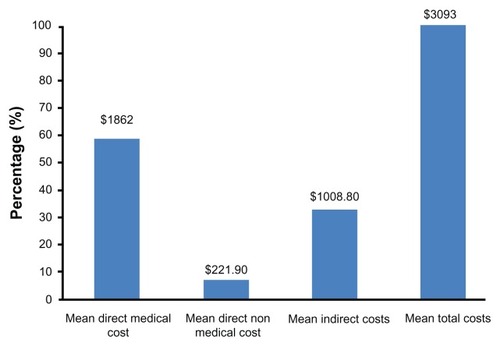
A total of 165 patients (84% females), of mean age 61 ± 15 years and with a mean disease duration of 8.5 ± 8.3 years were included. Mean total direct medical costs were US$1862 (95% confidence interval [CI] 828–2899). Mean direct nonmedical costs were US$222 (95% CI 149–294). Mean indirect costs were US$1008 (95% CI 606–1412). The annual mean total cost was US$3093 without biologics. Hospitalizations represented 73% of total direct medical costs while drugs and outpatient procedures represented 16% and 8% of total direct medical costs, respectively. Sixty percent of the total costs were related to direct medical costs, while indirect costs represented 33% of total costs.
Conclusion
In our population, annual mean total costs in the prebiologic therapy era were mainly driven by direct medical costs. Even without the use of biologic agents, rheumatoid arthritis represents an important burden for society in developing countries.
Introduction
Rheumatoid arthritis is a chronic systemic inflammatory disabling disorder affecting 0.2%–1% of the population worldwide. In Argentina, the prevalence of rheumatoid arthritis has been estimated to be 0.2%–0.94% in population-based studies.Citation1–Citation3 Rheumatoid arthritis imposes a considerable burden on society in terms of morbidity, long-term disability, and costs.Citation4,Citation5 The quantification of all costs associated with a particular disease are used as a proxy for the medical and economic burden that the disease places upon society.Citation5 Such studies are known as cost-of-illness studies or burden-of-illness studies.Citation5,Citation6
Burden-of-illness analysis, by assessing the use of health care resources and detailing the cost components involved, gives additional insight into the magnitude of the disease and its consequences.Citation7 On the other hand, burden-of-illness studies provide the bases for cost calculations in the cost-effectiveness analysis.Citation8 In the era prior to biologic treatments, direct medical costs of rheumatoid arthritis have been estimated at 5700–5800 US dollars per year in the US.Citation9 Drugs represented 8%–24% of direct medical costs, while hospital admission represented 60%–80%.Citation9
There is very scarce information on the burden of rheumatoid arthritis in developing countries, in particular for Latin America.Citation10–Citation13 Resource availability is limited in many sectors in Argentina, including the health care system. To optimize utilization of the scant resources available, it is essential to conduct systematic economic evaluations of health interventions, as well as to develop an awareness of how these costs break down and are utilized. To date, there have been no studies on resource allocation and the cost of rheumatoid arthritis from a societal perspective in Argentina. The objective of this study was to explore the burden of rheumatoid arthritis in a health management organization (HMO) in Argentina, including cost and components of costs from a societal perspective in the prebiologic era.
Materials and methods
We performed a one-year (2002) observational, retrospective, prevalence “bottom-up”, sum-all medical, cost-of-illness study from the societal point of view. All patients affiliated to the Hospital Italiano de Buenos Aires HMO (Plan de Salud) identified in an earlier prevalence studyCitation1 and fulfilling the inclusion criteria were included. All patients met the American College of Rheumatology 1987 revised criteria for the classification of rheumatoid arthritis.Citation14 Eligible patients had to fulfill the following criteria: age > 18 years; continuous affiliation with the Plan de Salud during 2002 (except for dropouts due to death). Ethical approval for this study was obtained from the hospital institutional review board.
Setting
The Plan de Salud is an HMO with its medical care based in a university hospital which is part of the private health insurance subsystem in Argentina. Argentina’s health system is divided into three major subsystems as follows.
Public subsystem
The public subsystem is open to the whole population but mainly used by those without voluntary or compulsory insurance (mainly unemployed or on the “black” labor market), representing around 40% of the total population.
Social security subsystem
The social security subsystem involves central agents of the health insurance system covering the population insured under a compulsory insurance system (income-related contributions by employers and employees), representing 52% of Argentina’s population. This subsystem includes the national social security institute for retirees and pensioners (PAMI) which is under a special regime, and covers 22.4% of the population under the compulsory insurance system, and its resources come from contributions from active and retired workers.
Private insurance or voluntary insurance subsystem
The third subsystem is the private insurance or voluntary insurance model containing the Plan de Salud, and covers around 7% of the higher-income population in Argentina. Patients voluntarily affiliate with the Plan de Salud and with a monthly prepaid system acquire full coverage for all medical events (including ambulatory and inpatient care), and 60% coverage for all prescribed medications. Since 1999, the Plan de Salud has had a problem-oriented electronic medical record system in which all medical encounters and diagnoses are registered. During the year 2002, Plan de Salud had around 70,000 affiliated adult members. Ninety percent of all Plan de Salud and its affiliates are individual bodies as opposed to institutional affiliations.
Data sources
Data for health care utilization and direct medical costs were obtained from the HMO administrative and medical databases. Clinical data were obtained from the first Rheumatology visit during year 2002. Clinical assessments included demographics and the Argentine validated version of the Health Assessment Questionnaire (HAQ) disability index.Citation15 Nonmedical direct costs (transportation) and indirect costs incurred in the previous 12 months were assessed by a semistructured cost questionnaire administered at the same visit.
Direct medical costs
All costs were included (sum-all medical).Citation6 Direct medical costs comprised the costs related to medications (including out-of-pocket payment for prescribed medications), laboratory tests and procedures, hospitalizations, medical and other allied health professional outpatient visits, and rehabilitation. Complementary practitioners, eg, chiropractors and acupuncturists, were not included. Direct medical costs and health care utilization were obtained from the HMO administrative database, and reflect charges to the HMO without adjustment, and are expressed in US dollars for the year 2002.
Direct nonmedical costs
Patients and family members and/or caregiver transportation costs were included and obtained from the cost questionnaire.
Indirect costs
Indirect costs included the cost estimates resulting from work absenteeism by patients and their family members, and the patient’s loss of productivity because of early retirement due to rheumatoid arthritis (permanent work disability). For those in the labor force (full-time and part-time) and family members, the human capital approachCitation16 was used, considering the average Argentine wage rate in the year 2002 (US$588 per month) to value the lost time. The following formula was used:
For those who were permanently disabled, implicit one-year income losses were calculated using average Argentine wage rates. For housewives, the replacement cost approach was used, ie, multiplying the number of self-reported days unable to attend to domestic duties by market values to perform equivalent duties at home ($1.79 US per hour × 8 hours a day). All these indirect cost data were obtained from the cost questionnaire.
Statistical analysis
Demographic and disease characteristics of the patients are presented using descriptive statistics. Health care utilization is presented as the mean ± standard deviation or median and interquartile range (IQR) according to variable distribution. Costs are presented as mean annual values per patient in 2002 US dollars without adjustment. Costs were also compared between patients according to disability status measured by HAQ (< or >0.8 as a dichotomous variable). Statistical analysis was performed using STATA statistical software, version 8.0 (Stata Corporation, College Station, TX).
Results
One hundred and sixty-five patients were included in this study. Patient demographics and work-related characteristics are summarized in . Mean age at study entry was 62 ± 15 years, and mean disease duration was 8.5 ± 8.3 years. All patients had full health care coverage because all were affiliated with the Plan de Salud. summarizes health care utilization during the study period. The annual incidence of hospitalizations was 254 per 1000 patients (95% confidence interval [CI] 128–381).
Table 1 Demographic and work-related characteristics of 165 patients with rheumatoid arthritis
Table 2 Utilization of health care resources
Direct medical costs
Four primary components of cost (hospitalization, drugs, medical and allied health professional visits, and outpatient procedures) are summarized in . Mean annual total direct medical cost was US$1862 ± US$6735 per patient (median 460; IQR 221–830). Hospitalizations represented 73% of total direct medical costs, while drugs and outpatient procedures represented 16% and 8% of total direct medical costs, respectively.
Table 3 Annual mean direct medical costs according to type
Direct nonmedical costs
Mean annual expenditure for transportation of patients and family members was US$221.9 ± US$315 (95% CI 149–294; median 107; IQR 17–343).
Indirect costs
Ninety patients completed the cost questionnaire. There were no differences in demographic characteristics between patients answering the questionnaire and the total study population with rheumatoid arthritis. shows the distribution of patients related to their work status. Forty-seven percent (95% CI 36–57) were working full-time and 18% (95% CI 11–28) were full-time housewives.
shows work absenteeism and indirect costs. Fifty-eight percent of workers reported at least one day of absenteeism because of their disease. Workers (full-time plus part-time) lost a mean of 17.6 ± 29.2 (median 12; IQR 0–12) days during the year because of the disease, and family members lost a mean of 4 ± 8.9 days per year for the same reason.
Table 4 Work absenteeism and indirect costs
Housewives were unable to attend their homes for a mean 8.8 ± 13.4 days during the year. Six patients (7%, four females and two males) retired at an early age (mean age of retirement 55 ± 10 years) because of permanent disability. The remaining patients (18%) were retired because of their age alone and were not currently working. Annual mean total indirect cost were US$1008 (95% CI 606–1412; median 353; IQR 0–859) per patient.
shows cost types according to disability status measured by HAQ in 132 patients in whom HAQ status was available. While direct medical costs were not significantly different in patients with lower or higher HAQ, indirect and total costs were significantly higher in patients with more disability (HAQ > 0.8).
Table 5 Median direct annual costs and total costs according to HAQ status
Total costs
shows the mean total cost and the distribution of its components. Mean annual total cost was US$3093 (95% CI 1581–4605) per patient. Sixty percent of total costs were related to direct medical costs, while indirect costs represented 33% of total costs.
Discussion
The results of this study indicate that the annual costs of rheumatoid arthritis in the Argentine population during the prebiologic therapy era were approximately 3000 US dollars per patient. Numerous studies exist on the costs of rheumatoid arthritis in many countries; however, there are few studies of costs for adults with rheumatoid arthritis in Latin America and other developing countries.Citation10–Citation13,Citation17 It is difficult to compare costs from different countries because of varying definitions of costs and sources of unit costs, as well as differing time periods and exchange rates.Citation17
Pugner et alCitation17 reviewed cost studies performed between 1978 and 1998 in the major Organization for Economic Cooperation and Development countries. They reported that the mean annual total cost of rheumatoid arthritis was $12,210 per patient, expressed in 1998 US dollars. A review by Cooper of 15 studiesCitation5 reported direct medical costs averaging US$5720 (1996 US dollars) and indirect costs of US$5822. These figures are higher than ours, and this could be explained by the fact that health care is less expensive in Argentina than in developed countries (a medical visit is paid in the US 825% more than in Argentina (at US$49.50Citation18 versus US$6, and a hand and wrist x-ray is paid 275% more in the US than in Argentina, at US$27.50Citation18 versus US$10).
On the other side, costs in our study were higher than those reported in other Latin American countries, such as BrazilCitation12,Citation13 and Colombia.Citation19,Citation20 Brazilian authors found a mean direct annual cost per patient of US$403.04 (2002),Citation13 which is lower than our mean of US$1862. One possible explanation is that they only considered costs related to rheumatoid arthritis, while we took into account all medical costs. Mean numbers of medical visits, diagnostic tests, and hospitalizations were lower in the Brazilian study than in ours. In the first Colombian study, the direct total cost was US$938 for the first year of disease after diagnosis (taking into account methotrexate as the first-choice treatment). Medications represented more than 50%, followed by the costs of diagnostic tests, while physician’s fees represented less than 6%.Citation19 In the other Colombian study, patients with mild and moderate disease (most of them without biologics) were US$1689, and US$1805, respectively.Citation19 In both studies, patients had early rheumatoid arthritis, where less costs are expected, in particular during the first year.Citation19,Citation20 In Mexico, the total annual medical costs were US$2339, and the main component was use of medication.Citation21
More meaningful perhaps than comparing costs between different countries is to look at percent contributions of the various components of costs. A prevalence estimate of the cost of disease can provide information regarding the categories of cost that can be targeted for economic savings. Between one quarter and one half of the costs of rheumatoid arthritis were direct medical costs, and hospitalization was the most important single factor in direct costs in the review by Pugner.Citation17 Summarizing 12 studies, the authors found that hospitalization accounted for a median of 47% (range 16%–67%) of direct costs, whereas medication accounted for a median 16%.Citation17 In the review by Cooper,Citation5 two of the four studies that estimated both direct and indirect costs reported direct costs to be the largest contributor to total cost (62%–74%)Citation22,Citation23 and two studies reported indirect costs to be approximately twice the direct costs.Citation24,Citation25 In that review, medication constituted 8%–24% of total medical costs and inpatient stays 17%–88%.Citation5
In our study, direct medical costs accounted for 60%, and indirect costs for 33% of total annual costs. Within the direct medical costs, hospitalizations accounted for 73% and drug costs for 16%. Thus, hospitalizations accounted for the largest proportion of costs, and represent the area with the largest potential for savings. Interestingly, while patients with more disability measured by HAQ had similar direct medical costs, they had higher indirect and total costs. This result probably reflects the higher work impairment in patients with more disability.
The cost of rheumatoid arthritis and the components thereof changed after the introduction of biologic agents. Direct medical costs became driven by drug costs, and drug costs were mainly driven by biologic therapy in the study by Michaud et al.Citation18 The mean total annual direct cost for patients receiving biologic agents was US$19,016 per year, while the cost for those not receiving biologic therapy was US$6164.Citation18 The high acquisition costs of new therapies are expected to be compensated by savings in employment productivity, given that maintaining people at work is the only way that such agents can be cost-effective.Citation26,Citation27
Our study has some inherent limitations. It was performed in an HMO which was part of the private insurance health care subsystem, including patients with higher incomes. Whether this population is representative of the whole Argentine population with rheumatoid arthritis and whether our estimates can be generalized further remains controversial. In a national study of patients with rheumatoid arthritis in Argentina, the patients included were similar to those with rheumatoid arthritis in the rest of the country in terms of demographics, disease activity, disability, and standard of care provided (unpublished data). The characteristics of the study population have an effect on cost estimates. In this sense, our population was similar to that reported in other studies.Citation5 Forty-eight percent of our patients were over 65 years of age and many of them were not working or retired. This might have underestimated the impact of temporary work disability, and underestimated indirect costs. The rate of permanent work disability in our study (7%) was lower than that reported in the review by Burton et alCitation27,Citation28 (20%–70%). A review of 12 cross-sectional studies from Europe and the US found that patients with rheumatoid arthritis had an increased risk of being without paid employment, with odds ratios between 1.2 and 3.4 compared with reference groups.Citation29 Restriction on employment occurred during the early phase of rheumatoid arthritis and varied between different studies.Citation29 Two years after diagnosis, disability benefits increased by up to 30% in some European countries.Citation29 An observational study in the US of work disability in subjects with rheumatoid arthritis found annualized incidence rates of 8.7% for stopping work and 4.0% for stopping and not resuming work over a period of 12.8 years.Citation30 These differences might be explained, at least in part, by the low disability compensation and retirement wages in our country, which discourage early retirement. The fact that our patients are from a high-income population had no effect on indirect costs because we used the average Argentine wage instead of actual salaries.
For direct medical costs, we included all medical costs, not just costs related to rheumatoid arthritis. This was a population of elderly patients, where some comorbidities are to be expected. We adopted this position because it is not always clear what costs should be attributed strictly to rheumatoid arthritis. Cardiovascular disease has been shown to be more frequent in patients with rheumatoid arthritis, and along with infections and gastrointestinal ulcers, could be considered consequences of rheumatoid arthritis.Citation31–Citation33 Lajas et alCitation34 found that only 10% of global health care costs were not related to rheumatoid arthritis. Although the calculation of incremental costs using a disease-free population is recommendedCitation5 to avoid the assumption that without the disease of interest a person would incur no cost-of-illness, these data are still relevant for decision-makers, government, and society as a whole.
We used charges rather than costs without adjustment. This could generate some differences when attempting to generalize results to other settings, because the amount billed and paid for a resource may very often be different from its actual cost. However, most studies use charges as proxies for costs, and figures obtained in this way might better reflect the disease burden for society. Finally, the study was performed in 2002, and its results might not exactly reflect the situation today. However, these are still valuable data on health service utilization and costs of patients treated with traditional disease-modifying antirheumatic drugs.
Despite these limitations, our study has the following merits. The study was done in a community-based rather than on a hospital-based population. This provides a more reliable estimate about the impact of rheumatoid arthritis in terms of restriction on activities and medical care utilization, and may be more realistic when generalizing to the overall disease population in our country. We measured real direct medical costs rather than estimating them from mean values, standard costs, or patient’s reported use of care, as have earlier studies,Citation5,Citation17 giving a more accurate estimate of health care utilization. Finally, we report not only costs, but also health care utilization, which might be more useful for international comparisons.
Our results are consistent with previous studies from other parts of the world. In developing countries, costs are still mainly driven by direct medical costs because they follow international values more closely than national wages. The high acquisition costs of new therapies at their international prices contrasting with the lower economic impact of maintaining employment makes these treatments in developing countries much less cost-effective than in developed countries, and this is a problem that all sectors involved will have to address.
Acknowledgment
The authors express their gratitude to Mould Joaquin and Tang Boxiong for their valuable comments on the manuscript.
Disclosure
The study was partially supported by an unrestricted educational grant from Pfizer SA.
References
- SorianoECarrioJSchpilbergMFigarSImamuraPCatoggioLIncidence and prevalence of rheumatoid arthritis in a health management organization in ArgentinaRheumatology200342Supp 1130
- SpindlerABellomioVBermanAPrevalence of rheumatoid arthritis in Tucuman, ArgentinaJ Rheumatol20022961166117012064829
- ScublinskyDVenarottiHCiteraGThe prevalence of rheumatoid arthritis in Argentina: a capture-recapture study in a city of Buenos Aires provinceJ Clin Rheumatol201016731732120859227
- KvienTKEpidemiology and burden of illness of rheumatoid arthritisPharmacoeconomics200422Suppl 211215157000
- CooperNJEconomic burden of rheumatoid arthritis: a systematic reviewRheumatology (Oxford)2000391283310662870
- AkobunduEJuJBlattLMullinsCDCost-of-illness studies: a review of current methodsPharmacoeconomics200624986989016942122
- Ben SedrineWRadicanLReginsterJYOn conducting burden-of-osteoporosis studies: a review of the core concepts and practical issues. A study carried out under the auspices of a WHO Collaborating CenterRheumatology (Oxford)200140171411157136
- BeresniakAGossecLGoupillePDirect cost-modeling of rheumatoid arthritis according to disease activity categories in FranceJ Rheumatol201138343944521123324
- YelinEHHenkeCJKramerJSNevittMCShearnMEpsteinWVA comparison of the treatment of rheumatoid arthritis in health maintenance organizations and fee-for-service practicesN Engl J Med1985312159629673974686
- OsiriMMaetzelATugwellPThe economic burden of rheumatoid arthritis in a developing nation: results from a one-year prospective cohort study in ThailandJ Rheumatol2007341576317183621
- AudisioMJStrusbergIOrellana BarreraSDSemester direct cost by rheumatoid arthritis in patients in a university hospitalRev Fac Cien Med Univ Nac Cordoba20036023541 Spanish14763431
- de AzevedoABFerrazMBCiconelliRMIndirect costs of rheumatoid arthritis in BrazilValue Health200811586987718489511
- ChermontGCKowalskiSCCiconelliRMFerrazMBResource utilization and the cost of rheumatoid arthritis in BrazilClin Exp Rheumatol2008261243118328143
- ArnettFCEdworthySMBlochDAThe American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritisArthritis Rheum19883133153243358796
- CiteraGArriolaMSMaldonado-CoccoJAValidation and crosscultural adaptation of an Argentine Spanish version of the Health Assessment Questionnaire disability indexJ Clin Rheumatol200410311011517043481
- RiceDPCost-of-illness studies: fact or fiction?Lancet19943448936151915207983947
- PugnerKMScottDIHolmesJWHiekeKThe costs of rheumatoid arthritis: an international long-term viewSemin Arthritis Rheum200029530532010805355
- MichaudKMesserJChoiHKWolfeFDirect medical costs and their predictors in patients with rheumatoid arthritis: a three-year study of 7,527 patientsArthritis Rheum200348102750276214558079
- Pineda-TamayoRArcilaGRestrepoPTabonGCamargoJFAnayaJMImpact of cardiovascular illness on hospitalization in patients with rheumatoid arthritisRevista Colombiana De Reumatología20041128996 Spanish
- MoraCGonzalesADiazJQuintanaGFinancial costs of early rheumatoid arthritis in the first year of medical attention: three clinical scenarios in a third-tier university hospital in ColombiaBiomédica20092914350 Spanish
- Mould QuevedoJPelaez BallestasIVazquez MelladoJSocietal costs of the most common inflammatory rheumatic diseases in Mexico from the patient’s perspectiveGac Med Mex20081443225231 Spanish18714591
- ClarkeAEZowallHLevintonCDirect and indirect medical costs incurred by Canadian patients with rheumatoid arthritis: a 12 year studyJ Rheumatol1997246105110609195508
- JonssonBRehnbergCBorgquistLLarssonSELocomotion status and costs in destructive rheumatoid arthritis. A comprehensive study of 82 patients from a population of 13,000Acta Orthop Scand19926322072121590060
- MeenanRFYelinEHHenkeCJCurtisDLEpsteinWVThe costs of rheumatoid arthritis. A patient-oriented study of chronic disease costsArthritis Rheum1978217827833100122
- StoneCEThe lifetime economic costs of rheumatoid arthritisJ Rheumatol19841168198276520836
- BrennanABansbackNReynoldsAConwayPModelling the cost-effectiveness of etanercept in adults with rheumatoid arthritis in the UKRheumatology (Oxford)2004431627212890861
- YelinEWork disability in rheumatic diseasesCurr Opin Rheumatol2007192919617278920
- BurtonWMorrisonAMacleanRRudermanESystematic review of studies of productivity loss due to rheumatoid arthritisOccup Med (Lond)2006561182716286432
- GeuskensGABurdorfAHazesJMConsequences of rheumatoid arthritis for performance of social roles – a literature reviewJ Rheumatol20073461248126017407220
- WolfeFAllaireSMichaudKThe prevalence and incidence of work disability in rheumatoid arthritis, and the effect of anti-tumor necrosis factor on work disabilityJ Rheumatol200734112211221717787043
- del RinconIDWilliamsKSternMPFreemanGLEscalanteAHigh incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factorsArthritis Rheum200144122737274511762933
- GonzalezAMaradit KremersHCrowsonCSDo cardiovascular risk factors confer the same risk for cardiovascular outcomes in patients with rheumatoid arthritis as in non-RA patients?Ann Rheum Dis2008671646917517756
- GoodsonNCoronary artery disease and rheumatoid arthritisCurr Opin Rheumatol200214211512011845015
- LajasCAbasoloLBellajdelBCosts and predictors of costs in rheumatoid arthritis: a prevalence-based studyArthritis Rheum2003491647012579595