Abstract
Purpose
This study aims to evaluate the cost-effectiveness of chin tuck against resistance (CTAR) for citizens suffering from dysphagia compared to the standard municipal treatment in Denmark.
Patients and Methods
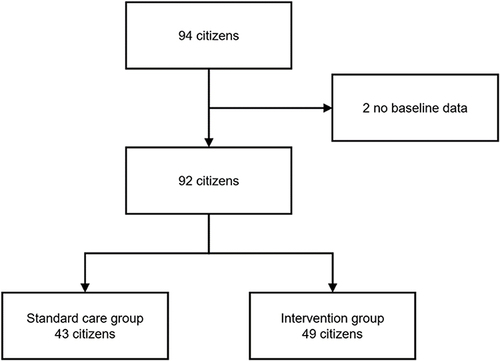
A cost-utility analysis, employing a municipal perspective, was conducted using cost data collected alongside clinical data of a randomized controlled trial evaluating the effect of CTAR training for citizens with dysphagia. The composition of the clinical randomized controlled trial, which included citizens with different diagnoses, means that participants had different disease courses. Ninety-two citizens from seven different Danish municipalities were enrolled, of whom 43 received standard care, and 49 received CTAR in addition to standard care. The effect outcome of the economic evaluation was quality-adjusted life years (QALY), estimated using the EQ-5D-5L questionnaire. Individual resource consumption of each citizen was determined based on the use of home care, home nursing care, physio- and occupational therapy, dietitian guidance, and hospital admissions. The incremental costs and QALYs between the intervention group (CTAR in addition to standard care) and standard care group were estimated using regression analysis, and sensitivity analyses were performed to investigate the robustness of the results.
Results
The base case analysis showed that the intervention group was dominant compared to the standard care group, with a decrease in incremental costs of £542.38 and an increase in incremental QALYs of 0.0118. All sensitivity analyses demonstrated similar findings as the base case analysis, supporting the robustness of the results.
Conclusion
This study found that the intervention group was the dominant alternative, hence being more effective and cost-saving, compared to the standard care group in a Danish municipality perspective with a three-month time horizon. This study adds to the scarce evidence on the cost-effectiveness of CTAR in a Danish clinical setting, but further studies should focus on estimating long-term cost-effectiveness.
Introduction
The swallowing disorder called dysphagia poses a physiological, social, and psychological burden for the individual and an increased financial cost for national health-care systems.Citation1,Citation2 International and Danish studies demonstrate that the hospital- and municipality costs of patients with dysphagia are significantly higher than those without dysphagia.Citation1,Citation3,Citation4 The increase in hospitalization and admission cost in dysphagia patients can be associated with increased length of stay, diagnostic testing, and additional treatment.Citation1 Moreover, dysphagia is associated with an overall increase in the cost of care, as health-care consumption of the individual is increased due to, among others, prolongation of hospital stay, discharge to nursing homes rather than the individual’s own home, comorbidities, additional treatments, and institutionalization of geriatric patients with dysphagia.Citation2,Citation3,Citation5–8
Self-reported prevalence of dysphagia ranges between 2.3% and 16% in the population, but the prevalence increases with age. The condition is more commonly seen in individuals aged 65 years and older, with a prevalence of 52.7% in elders living in nursing homes.Citation3,Citation5–7 Besides being a result of higher age, dysphagia can also occur due to disease and is seen in individuals with established dementia, stroke, cancer, and Parkinson’s disease.Citation2,Citation3,Citation5,Citation7,Citation9 Dysphagia is associated with lower respiratory infections, malnutrition, dehydration, frailty, pneumonia, increased admissions and re-admissions rates, reduced quality of life (QoL), and increased risk of mortality.Citation2,Citation3,Citation5,Citation7,Citation9–12 Moreover, dysphagia has been associated with poor functional capacity, multimorbidity, polymedication, and frailty.Citation5
Implementation of preventive strategies, including screening, nursing, and compensatory strategies, have been suggested to reduce health-related costs associated with dysphagia.Citation5,Citation7 Furthermore, intervention-based exercises improving the physiology of deglutition have proven beneficial and could potentially result in reduced health-related costs.Citation3,Citation5,Citation6,Citation13 It is reported that the rehabilitative exercise “chin tuck against resistance” (CTAR) increases swallowing function significantly through its impact on the suprahyoid muscles and improves psychological state in patients with neurological diseases.Citation14–16
To our knowledge, cost-effectiveness analyses have yet to be made to analyze whether CTAR is a cost-effective strategy. In Denmark, the focus on dysphagia has gone from being centralized in hospitals to an increased focus on dysphagia in municipalities as well.Citation4 The municipalities have an incentive for preventive- and rehabilitative initiatives, as they co-finance the consumption of regional health-care services, such as hospital care and other specialist care, by approximately 17%.Citation17 Hence, prevention of admissions, re-admissions, and a reduced need for hospital care could pose a financial incitement for the municipalities. Moreover, as citizens become more self-reliant, it could be speculated that their needs for municipal home care will also be reduced.
This study aims to evaluate the cost-effectiveness of CTAR for citizens suffering from dysphagia compared to standard municipal treatment. The study will be conducted as a cost-utility analysis (CUA) from a Danish municipal perspective.
Materials and Methods
CUA was conducted with cost data collected alongside clinical data from a randomized controlled trial (RCT) evaluating the effect of CTAR training for citizens with dysphagia.Citation18 The RCT was conducted from March 2019 to October 2020 and included citizens from seven Danish municipalities (Hjørring, Frederikshavn, Jammerbugt, Kolding, Tønder, Brøndby, and Odense). Citizens who fulfilled the inclusion criteria of ≥18 years and were diagnosed with dysphagia, confirmed by volume viscosity swallow test (V–VST), the Minimal Eating Observation form – version II (MEOF-II), and understood and gave informed consent were included. Exclusion criteria comprised severe dementia or other cognitive impairments, citizens in the palliative stage, and citizens with feeding tubes. When participants had signed an informed consent, the occupational therapist (OT) randomized them 1:1 to either standard care or the intervention group (CTAR in addition to standard care), using the Research Electronic Data Capture (REDCap), hosted at the North Denmark Region.Citation19,Citation20 REDCap is a secure, web-based software platform that supports data capture for research studies.
The standard care group consisted of two visits from an OT and a dietitian to educate about dysphagia, optimal sitting position, viscosities, and calorie-and protein intake. The intervention group was offered standard care, plus an intervention consisting of CTAR. The intervention group received a visit twice a week for 6 weeks from an OT who introduced participants to CTAR and ensured the exercise was performed correctly. They were instructed to perform CTAR three times a day for 6 weeks.Citation18
Data Collection
The economic evaluation followed the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) guideline for conducting health economic evaluations alongside clinical trialsCitation21 and the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) for economic evaluations.Citation22 The time horizon for the analysis was restricted to 3 months, and a Danish municipality perspective was applied. The perspective included costs accumulated within the municipality sector and the municipal co-financing of regional health-care costs, including hospital admissions and outpatient visits.
Cost Accumulation and Resource Consumption
All costs are reported as British Pounds (£) at 2020 value. Costs were inflated by the Danish consumer price indexCitation23 and converted from Danish Krones (DKK) to British Pounds (£) (exchange rate used from The Bank of England on 22 September 2022: £1 = 8.5309 DKK).Citation24 The collection of costs was differentiated into municipal and regional resource consumption. Municipal resource consumption was collected for each citizen using local registers and consisted of home care, home nursing care, physio- and occupational therapy, and dietitian guidance. The hourly consumption related to the elements of municipal services was identified for each citizen via registration in the municipality. Data were extracted via the Danish Civil Registration System (CPR). A national average hourly wage rate was utilized for municipal consumption to value the resource consumption of each citizen.Citation25 For the valuation of regional resource consumption, consisting of costs related to hospitalizations, relevant Diagnosis-Related Groups (DRG) tariffs were assigned based on information on the length of stay and diagnosis. DRG tariffs are used to reimburse Danish hospitals and reflect the average costs for treating patients with similar diagnoses and courses of treatment at a Danish hospital.Citation26,Citation27 Table S1 provides an overview of the applied DRG tariffs.
Due to the perspective of the analysis, only the amount related to the municipal co-financing was included, corresponding to 17% of the DRG tariff. Furthermore, a cost for the training ball used for the CTAR exercise program was included in the total cost estimate for the intervention group. The protocol-driven costs, such as training the OTs in using the questionnaires for outcome measurement, were not included.
Measurement of Health Outcomes
The health outcome of this economic evaluation was quality-adjusted life years (QALY), which was estimated using the EQ-5D-5L questionnaire,Citation28 a generic questionnaire consisting of five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression).
The EQ-5D-5L was completed at baseline and 3 months for both groups and at 6 weeks for the intervention group. Estimations of HRQoL were converted into EQ-5D-5L index scores using Danish societal weights.Citation29 Citizens dying during the study received an EQ-5D-5L index score of zero. For each of them, QALYs were calculated by assuming linear interpolation between the two measurements of HRQoL at baseline and 3 months.
Additional data on health outcomes were also collected for both groups at baseline and 3 months, and at 6 weeks for the intervention group, eg the V–VST and the MEOF-II to assess dysphagia, and the Dysphagia Handicap Index (DHI-DK) and Barthel 20 index to assess QoL and functional capacity. Demographic data on age, height, weight, and housing were collected at inclusion for everyone. Data was collected by OTs in the municipalities and entered in REDCap.
Data Analysis
The analysis is based on the intention-to-treat principle. Missing data were assumed to be missing at random (MAR), and multiple imputation was applied.Citation30 A description of the applied imputation model is available in the Supplementary Material Table S2.
For descriptive analysis, data were reported as means and standard deviations (SD), and mean differences between the intervention group and standard care group were presented as raw, unadjusted differences. Student’s t-test evaluated P-values for between-group differences for continuous variables and Pearson’s X2 evaluated for binary variables. A p-value < 0.05 indicates a statistically significant difference between groups, and all significance tests were two-tailed.
The estimates of incremental costs and QALYs between the intervention group and standard care group were based on a generalized linear model (GLM) with a robust variance estimator. The QALY and cost estimates were adjusted for baseline HRQoL, as the citizens’ HRQoL at follow-up, as well as their resource use during the follow-up period, are believed to be highly correlated to their HRQoL at baseline. Adjustment for baseline utility is especially important in case of baseline between-group imbalance, and failure to do so may bias the result.Citation31 All statistical analyses were performed in Stata, version 17.0 (STATA Corporation, College Station, USA).
Sensitivity analyses were performed to investigate the robustness of the base case analysis. The sensitivity analyses were composed of three scenario analyses presented in the following.
Scenario 1: As a base case analysis but excluding citizens with more than 7 days of hospitalization. Citizens in intervention groups with hospitalizations longer than 7 days could not receive the training program, and citizens with prolonged hospitalizations could potentially drive the costs of the intervention.
Scenario 2: As a base case analysis, but with the inclusion of the EQ-5D-5L measurement in the intervention group at 6 weeks. To include the temporary increase in HRQoL obtained directly after the training programme.
Scenario 3: As the base case analysis but only conducted on complete cases.
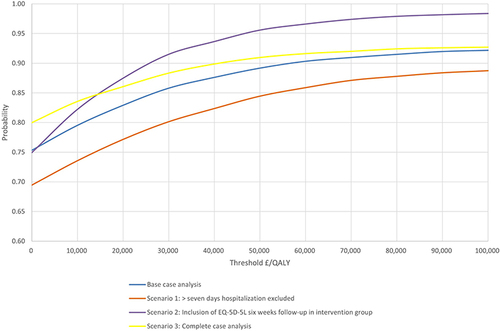
All analyses were subject to probabilistic sensitivity analysis (PSA) by drawing 10,000 trial simulations. Correlated draws were obtained using the variance-covariance matrices from the GLM models and Cholesky’s decomposition. The results for all analyses were visualized in a cost-effectiveness plane and using cost-effectiveness acceptability curves.
Results
In total, 94 citizens were enrolled in the trial. Two citizens were excluded due to missing data on their dysphagia diagnosis, leaving 92 citizens to be included in the analysis (). Of the 92 citizens, 12 was lost to follow-up (intervention group = 6, standard care group = 6). Of the remaining 80 citizens, three died during the study (intervention group = 2, standard care group = 1) and received an EQ-5D-5L index score of zero.
At baseline, statistically significant between-group differences were detected for total score on EQ-5D-5L scores (p=0.016) and DHI-DK scores (p=0.003) ().
Table 1 Baseline Characteristics of Citizens in Standard Care Group and Intervention Group. Data are Reported as Mean (Standard Deviation) Unless Otherwise Noted
presents the mean value of the measured health outcomes at different time points: baseline, 6 weeks (only intervention group), and 3 months (both the intervention group and standard care group). The presented values are the non-imputed and unadjusted values. A significant difference was detected between the measurement at baseline of EQ-5D-5L and DHI-DK, but no difference at 3-month follow-ups.
Table 2 Non-Imputed and Unadjusted Values of the Health Outcomes per Citizen in the Intervention Group and Standard Care Group
In , the resource consumption and the applied unit costs are presented. The results in the table present the unadjusted differences in resource consumption between the intervention group and standard care group. Based on the results, it is evident that the intervention group had a slightly lower utilization of homecare services but an increased use of nursing and occupational therapy compared to the standard care group. Additionally, the intervention group had higher costs associated with hospitalization compared to the standard care group.
Table 3 Non-Imputed and Unadjusted Mean Resource Use per Citizen for the Intervention Group and Standard Care Group Over 3 Months Follow-Up and Applied Unit Costs
The results from the base case analysis and the sensitivity analyses are presented in . The base case analysis showed that the intervention group is dominant compared to the standard care group, with a decrease in incremental costs of £542.38 and an increase in incremental QALYs of 0.0118. Similar results are shown in scenarios 1, 2, and 3 from the sensitivity analyses. The results are illustrated in an incremental cost-effectiveness plane (). The probability that the base case and each of the sensitivity analyses are cost-effective at varying willingness-to-pay thresholds is illustrated in a cost-effectiveness acceptability curve ().
Table 4 Results of Intervention Group Compared to Control Group
Figure 2 Incremental cost-effectiveness plane with the indication of the base case and sensitivity analyses and scatter plot of the probabilistic sensitivity analysis of the base case. The line across the plot indicates a cost-effectiveness threshold of £20,000 per quality-adjusted life-year (QALY).
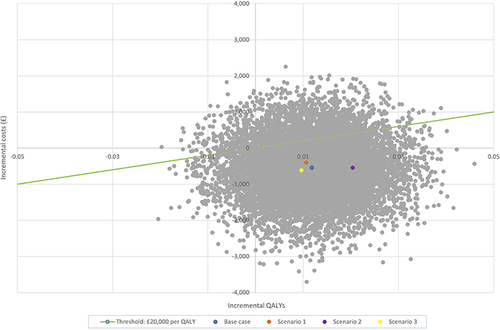
Figure 3 Cost-effectiveness acceptability curve. The probability that the base case and each of the sensitivity analyses are cost-effective at varying willingness-to-pay thresholds. The blue line represents the base case analysis, the Orange scenario 1, the purple scenario 2, and the yellow scenario three, respectively.
Discussion
The main finding of this study indicated that the use of CTAR for citizens suffering from dysphagia compared to standard municipal treatment is dominant, meaning that CTAR is both more effective and less costly. All sensitivity analyses applied to test the robustness of the analysis showed similar results as the base case analysis.
As demonstrated in , the EQ-5D-5L utility value at 3 months was lower in the intervention group than in the standard care group (0.584 vs 0.597), indicating a lower HRQoL at that time point. However, it is important to consider the large difference in EQ-5D-5L utility value at baseline, where the intervention group scored significantly lower than the standard care group (0.465 vs 0.620).
When looking at the HRQoL development in the two groups, an increase is seen from baseline to follow-up in the intervention group compared to a decrease in the standard care group. Furthermore, it should be noticed that an increase from baseline to 6 weeks, and a decrease from 6 weeks to 3 months, are seen in the intervention group (not measured in standard care). The reason for the increase and decrease is unknown but could be related to a potential decrease in compliance following the discontinuation of the visits from an OT, as it is known that the effect of training subsides sometime after the training effort ceases.Citation32
The strengths of the current study include the use of data from different municipalities across Denmark. The inclusion of seven different municipalities, which differ in geographical location and size, strengthens the generalizability of the results. Hereby, it could be expected that the study population is representative of citizens with dysphagia in Denmark, as the study sample included individuals with different underlying causes of dysphagia and thereby disease courses.Citation18 Furthermore, the study population included citizens with different co-morbidities and was not limited to citizens or patients with a specific disease (eg, stroke, cancer, and Alzheimer’s). A limitation to the study design and the inclusion of citizens in the RCT entails excluding citizens with a feeding tube, which can bring an element of bias as more severe cases of dysphagia are excluded. Moreover, the citizens in the intervention group had more time and supervision with clinicians, which can introduce a risk of placebo effect. The RCT employed as a vehicle in the current study uses the common standard municipal treatment in the standard care group. Hereby, the relevance of the results is enhanced, as the intervention is compared to current practice.Citation18
Furthermore, a micro-costing approach was utilized in the estimation of municipal resource consumption, resulting in a more detailed evaluation of the individual citizen’s resource consumption. The costs related to hospital admissions were, however, estimated utilizing a gross-costing approach. By usage of Interactive DRG (a virtual tool for identification of the specific DRG group a specific citizen registration belongs to)Citation33 and information about citizens’ hospital admissions provided by the municipalities, each admission was valuated.
As the DRG groups were based on information on hospitalization from the municipality, no knowledge of other diagnoses was included in the estimation of the DRG group. This could under- or overestimate the costs related to hospitalizations. However, this is consistently estimated in both groups.
The perspective for this CUA consisted of a municipal perspective. A narrow perspective could lead to missing relevant costs, eg, change in resource consumption at the general practitioner. Furthermore, the choice of a time horizon of 3 months could result in missing relevant long-term consequences. Both factors could affect the results, and future research should focus on investigating the cost-effectiveness of CTAR from a broader perspective and longer time horizon.
As stated, the RCT did not collect similar measurements for citizens receiving standard care at 6 weeks follow-up, as was collected for the intervention group.Citation18 This limitation in data collection may entail that it cannot be ruled out whether there was a derived effect of inclusion in the study, meaning that an increased effect could also be seen for citizens receiving standard care at 6-week follow-up. As a result hereof, and to make a conservative estimate, the effect at 6 weeks follow-up for the intervention group was not included in the base-case analysis.
It has not been possible to find any other studies investigating the cost-effectiveness of CTAR in individuals with dysphagia. Thus, it has not been possible to directly compare the results of this study with others investigating the same. However, the effect of CTAR in individuals with dysphagia has been assessed. Different studies have demonstrated that the use of CTAR improves the swallowing function significantly and leads to an improvement in the participants’ self-reported depression.Citation14–16 Though improvements in swallowing function have been seen in the aforementioned studies, they did not report on whether this continued to be present at a potential follow-up at a later point in time. Moreover, the studies did not assess the citizens’ HRQoL by use of EQ-5D-5L, as did the current study. It can be speculated whether the results of Yoon et al.Citation16 Sze et alCitation15 and Gao et alCitation14 can be compared with the results of the current study, or not.
Conclusion
This study found that CTAR in addition to standard care was the dominant alternative compared to standard care with the application of a Danish municipality perspective and a three-month time-horizon. Similar results are demonstrated in the sensitivity analyses. This study adds to the scarce evidence on cost-effectiveness of CTAR; however, future research should focus on estimating the long-term cost-effectiveness of CTAR from a broader perspective.
Data Sharing Statement
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
The study complies with the Declaration of Helsinki and was approved by the regional ethics committee of Northern Denmark (N-20180061), registered at the Danish Data Protection Authority (2008-58-0028) and ClinicalTrials.gov (NCT04402307). All participants in the study signed informed consent prior to participation. A collaboration agreement was made with all participating municipalities.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be
accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The authors thank all participating municipalities and citizens.
Additional information
Funding
References
- Patel DA, Krishnaswami S, Steger E, et al. Economic and survival burden of dysphagia among inpatients in the United States. Dis Esophagus. 2018;31(1):1–7. doi:10.1093/dote/dox131
- Christmas C, Rogus-Pulia N. Swallowing disorders in the older population. J Am Geriatr Soc. 2019;67(12):2643–2649. doi:10.1111/jgs.16137
- Lancaster J. Dysphagia: its nature, assessment and management. Br J Community Nurs. 2015;2015:S28–32. doi:10.12968/bjcn.2015.20.Sup6a.S28
- Westmark S, Melgaard D, Rethmeier LO, Ehlers LH. The cost of dysphagia in geriatric patients. Clinicoecon Outcomes Res. 2018;10:321–326. doi:10.2147/CEOR.S165713
- Baijens LW, Clavé P, Cras P, et al. European society for swallowing disorders - European Union geriatric medicine society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging. 2016;11:1403–1428. doi:10.2147/CIA.S107750
- Starmer HM, Riley LH, Hillel AT, Akst LM, Best SRA, Gourin CG. Dysphagia, short-term outcomes, and cost of care after anterior cervical disc surgery. Dysphagia. 2014;29(1):68–77. doi:10.1007/s00455-013-9482-9
- Rommel N, Hamdy S. Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol. 2016;13(1):49–59. doi:10.1038/nrgastro.2015.199
- Melgaard D, Rodrigo-Domingo M, Mørch MM. The prevalence of oropharyngeal dysphagia in acute geriatric patients. Geriatrics. 2018;3(2):15. doi:10.3390/geriatrics3020015
- Panebianco M, Marchese-Ragona R, Masiero S, Restivo DA. Dysphagia in neurological diseases: a literature review. Neurol Sci. 2020;41(11):3067–3073. doi:10.1007/s10072-020-04495-2
- Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–146. doi:10.1007/s00455-001-0113-5
- Bendsen BB, Jensen D, Westmark S, Krarup AL, Riis J, Melgaard D. The quality of life in citizens with oropharyngeal dysphagia-A cross-sectional study. J Clin Med. 2022;11(14):4212. doi:10.3390/jcm11144212
- Melgaard D, Baandrup U, Bøgsted M, Bendtsen MD, Hansen T. The prevalence of oropharyngeal dysphagia in Danish patients hospitalised with community-acquired pneumonia. Dysphagia. 2017;32(3):383–392. doi:10.1007/s00455-016-9765-z
- Park JS, Hwang NK. Chin tuck against resistance exercise for dysphagia rehabilitation: a systematic review. J Oral Rehabil. 2021;48(8):968–977. doi:10.1111/joor.13181
- Gao J, Zhang HJ. Effects of chin tuck against resistance exercise versus Shaker exercise on dysphagia and psychological state after cerebral infarction. Eur J Phys Rehabil Med. 2017;53(3):426–432. doi:10.23736/S1973-9087.16.04346-X
- Sze WP, Yoon WL, Escoffier N, Rickard Liow SJ. Evaluating the training effects of two swallowing rehabilitation therapies using surface electromyography--chin tuck against resistance (CTAR) Exercise and the Shaker Exercise. Dysphagia. 2016;31(2):195–205. doi:10.1007/s00455-015-9678-2
- Yoon WL, Khoo JKP, Rickard Liow SJ. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a Shaker-type exercise. Dysphagia. 2014;29(2):243–248. doi:10.1007/s00455-013-9502-9
- The Danish ministry of health. Available from: https://sum.dk/english. Accessed May 12, 2023.
- Jensen D, Bendsen BB, Westmark S, et al. Effect of chin tuck against resistance exercise in citizens with oropharyngeal dysphagia—a randomised controlled study. Geriatrics. 2022;7(6):129. doi:10.3390/geriatrics7060129
- Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi:10.1016/j.jbi.2019.103208
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
- Ramsey SD, Willke RJ, Glick H, et al. Cost-effectiveness analysis alongside clinical trials II-An ISPOR good research practices task force report. Value Health. 2015;18(2):161–172. doi:10.1016/j.jval.2015.02.001
- Husereau D, Drummond M, Augustovski F, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 Explanation and Elaboration: a Report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25(1):10–31. doi:10.1016/j.jval.2021.10.008
- Statistics Denmark. StatBank Denmark. Economy. Price index. Consumer price index. PRIS8: Consumer price index, annual average. Available from: https://www.statbank.dk/statbank5a/default.asp?w=1098. Accessed May 12, 2023.
- Bank of England. Statistics. Exchange rates; 2022. Available from: https://www.bankofengland.co.uk/. Accessed September 22, 2022.
- Statistics Denmark. StatBank Denmark. Labour and income. Income and earnings. Pay level. LONS20. Available from: https://statistikbanken.dk/statbank5a/default.asp?w=1536. Accessed May 12, 2023.
- The Danish Health Data Authority. DRG tariffs 2019. Tariff system guidelines 2019. Available from: https://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering/takster-drg/takster-2019. Accessed May 19, 2023.
- The Danish Health Data Authority. DRG tariffs 2020. Tariff system guidelines 2020. Available from: https://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering/takster-drg/takster-2020/. Accessed May 19, 2023.
- EuroQol Research Foundation. EQ-5D-5L User Guide; 2019. Available from: https://euroqol.org/publications/user-guides. Accessed May 12, 2023.
- Jensen CE, Sørensen SS, Gudex C, Jensen MB, Pedersen KM, Ehlers LH. The Danish EQ-5D-5L value set: a hybrid model using cTTO and DCE Data. Appl Health Econ Health Policy. 2021;19(4):579–591. doi:10.1007/s40258-021-00639-3
- Faria R, Gomes M, Epstein D, White IR. A guide to handling missing data in cost-effectiveness analysis conducted within randomised controlled trials. Pharmacoeconomics. 2014;32(12):1157–1170. doi:10.1007/s40273-014-0193-3
- Manca A, Hawkins N, Sculpher MJ. Estimating mean QALYs in trial-based cost-effectiveness analysis: the importance of controlling for baseline utility. Health Econ. 2005;14(5):487–496. doi:10.1002/hec.944
- Borde R, Hortobágyi T, Granacher U. Dose-response relationships of resistance training in healthy old adults: a systematic review and meta-analysis. Sports Med. 2015;45(12):1693–1720. doi:10.1007/s40279-015-0385-9
- The Danish Health Data Authority. Interaktiv DRG [Interactive DRG. Available from: https://sundhedsdatastyrelsen.dk/da/afregning-og-finansiering/gruppering-drg/interaktiv-drg]. Accessed May 12, 2023.