Abstract
Introduction
As with several countries around the world, cesarean section rates are increasing also in Indonesia, raising issues of quality and cost-effectiveness of health care, especially with the shift from a fee-for-service to a prospective payment system. For hospital services to be effective (quality control) and efficient (cost control), clinical pathways are essential. However, no studies have been done to develop a clinical pathway for cesarean sections (CS) in the INA-CBG system that is both effective and efficient.
Objective
To develop clinical pathways for CS that are both effective and efficient by determining unit costs and tariffs for CS services, reviewing procedures and outcomes, and assessing performance efficiency and effectiveness.
Methods
Using a sample of 110 patients undergoing cesarean sections consecutively recruited in 11 hospitals of West Sumatra (6 public hospitals and 5 private institutions), this mixed (qualitative and quantitative) study aimed at developing clinical guidelines for childbirth delivery modes responding both to criteria of efficacy and efficiency.
Results
Of 110 patients, 50 patients (45%) had efficient CS, 85 patients (77%) had effective CS, and 40 patients (36.4%) had both effective and efficient CS. A comprehensive clinical pathway for CS procedure was created by investigating 40 patients who underwent effective and efficient CS using interviews, a Delphi study, and professional advice.
Discussion
Hospitals can adopt the effective and efficient clinical pathway for CS protocol to prevent cost-related losses (efficient) while retaining the quality of the service (effective).
Introduction
Cesarean section surgery is a surgical procedure to deliver a baby through an incision in the abdominal wall (laparotomy) and uterus (hysterotomy).(Adriaansz, 2017) It’s important to note that this definition excludes cases where the fetus is removed from the abdominal wall due to spontaneous tearing of the uterine wall (uterine rupture) or abdominal pregnancy.
The incidence of cesarean section (CS) experienced an increasing trend in various parts of the world, including Indonesia. In Indonesia, the CS rate increased from 12.9% in 2012 to 17% in 2017. According to the World Health Organization (WHO), the ideal CS rate is between 10% to 15% to avoid maternal deaths and improve maternal and neonatal outcomes.Citation1–3 However, some experts suggest that a more reasonable threshold of 19% may be appropriate as the previously recommended national target rates for CS deliveries may be too low.Citation4
In West Sumatra, the CS rate was 23.6% in 2018. This rate is much higher than the maximum standards set by WHO and expert recommendations in a recent study.Citation1–4 As a result, West Sumatra has become the fifth-ranked province with highest CS rate in Indonesia.Citation5,Citation6
The increasing CS incidence in Indonesia is not accompanied by an increase in the quality of hospital services and could be more efficient in terms of hospital costs. This is because the government has implemented a health financing system using a case-mix system called the Indonesia Case Based Groups (INA-CBG’s).Citation7 Under this system, both hospitals and the payers no longer break down bills based on the details of the services provided (fee for services), but only submit the patient’s discharge diagnosis and the CBG code (prospective payment system).Citation8 Unfortunately, many hospitals feel that the cost set by the Ministry of Health do not cover the actual costs incurred for the CS service package. As a result, they experience a negative difference or loss.Citation9
Clinical Pathway (CP) has long been recognized as a critical tool for achieving effectiveness and efficiency in hospital services.Citation10 In Lin’s 2021 study, it was found that implementing CP leads to a reduction in the Length of Stay (LOS) and hospital costs. Additionally, Rotter et al in 2021 also concluded that CP implementation can reduce the incidence of complications in hospitals, improve documentation, reduce readmissions, death, LOS, and hospital costs.Citation11,Citation12 CP is a map and model for clinical and non-clinical care perspectives and processes. This involves prioritizing existing guidelines and protocols, standards, and patient clinical outcomes. There are four main components of CP:Citation13
Timeline. Based on the type of case present, this could last days or even months.
Categories of action or treatment at each level and recommended local interventions.
Intermediate and long-term outcome criteria can be determined in advance.
Existing variants can be noted.
Until now, there has been no research on developing an efficient and effective clinical pathway for CS based on cost calculations and analysis of activity procedures within the INA-CBG’s system. Based on the description above, this research aims to develop an efficient and effective integrated clinical pathway for CS services through calculating unit costs and tariffs for CS services, reviewing procedures and outcomes, and evaluating performance efficiency and effectiveness in the INA-CBG’s system in West Sumatra.
Methods
This study was conducted in West Sumatra between August 2021 and April 2022. The study population consisted of 51 hospitals, categorized as Type B (with over 200 beds), Type C (with over 100 beds), and Type D (with over 50 beds). The study aimed to select 30% of hospitals from each category, resulting in 11 hospitals that provided CS services. In order to determine the necessary number of participants, the Lemeshow formula (1997) was employed, and it was found that 110 CS patients were needed to complete a questionnaire. Therefore, 10 patients were invited to participate from each hospital, resulting in a total of 110 patients. These patients were classified based on the type of CS services they received, which follows the American Society of Anesthesiologists (ASA) guidelines during the preoperative assessment. Mild CS were classified as ASA I–II, moderate CS as ASA III, and severe CS as ASA IV–V. To be eligible for the study, patients had to be registered with the national health insurance (BPJS) and willing to participate. Patients with severe complications were excluded from the study.
There are three stages of research activity. The first stage is calculating the unit cost of CS services and analyzing the efficiency of CS service performance. The second stage is to analyze the effectiveness of CS services. Stages 1–2 in this study are quantitative research, where the type of research is observational analytic.Citation14 The sample consisted of 110 patients who underwent CS services at 11 hospitals in West Sumatra. Sampling was done using non-probable sampling with a consecutive approach, meaning that every patient who comes and will have a CS is immediately recorded as a sample for observation. And so on until there are enough patients for each hospital.Citation14,Citation15
The total cost of CS services consists of direct costs and indirect costs, which are calculated using accounting data forms (direct costs form and indirect cost form).Citation16 Directs costs are related to health care delivered (in this case cesarean section), such as drugs, medical materials, and healthcare professionals’ services. On the other hand, indirect costs are Costs whose benefits are not a direct part of production, but are costs needed to support production units For instance, these could be costs associated with employee and general administration, such as finance, HR, and other non-production units.Citation17,Citation18 The direct costs are calculated using primary data obtained directly from all study participants through ‘direct cost forms’ and interviews, whereas the indirect costs are calculated using secondary data obtained from hospital records through “indirect cost forms” and interviews. The Activity-Based Costing (ABC) method is used to calculate indirect costs.Citation19
To evaluate the efficiency of CS services, the Break Even Point (BEP) method is used.Citation20 This involves comparing the results obtained from calculating the tariff for CS services with the tariff set by the government, as stated in Minister of Health RegulationCitation21 By comparing costs and revenues, we can identify a “loss area” (inefficient) and a “profit area” (efficient). The procedure is considered efficient if the CS service tariff is lower than the tariff policy (Government Tariff).
Analysis of the effectiveness of CS service performance was carried out by analyzing activity procedures and CS service outcome analysis.Citation22–24 Analysis of CS service activity procedures consists of 16 activities, starting from registration, initial assessment, laboratory, diagnostics, preoperative, medical procedures, anesthesia, intraoperative, infant procedures, postoperative, maternal care, child care, nutrition, sterilization, and pharmacy. Each procedure was analyzed using the Direct Observational of Procedural Skill (DOPS) form of the procedure steps for each activity.Citation25 Meanwhile, the outcome analysis for CS services was carried out by observing 3 types of outcomes, namely surgical pain, length of stay (LOS), and surgical site infection (SSI), in all patient samples. The procedure is said to be good (effective) if ≥ 80% of the steps are carried out,Citation26 no complications are found (SSI, surgical pain), and the LOS is according to the clinical pathway (3 days).Citation27
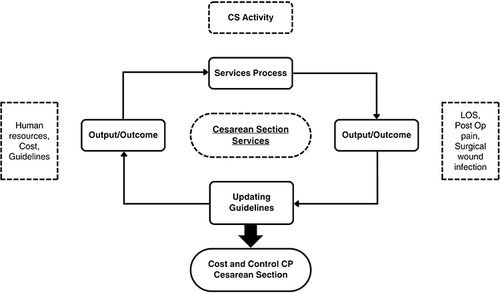
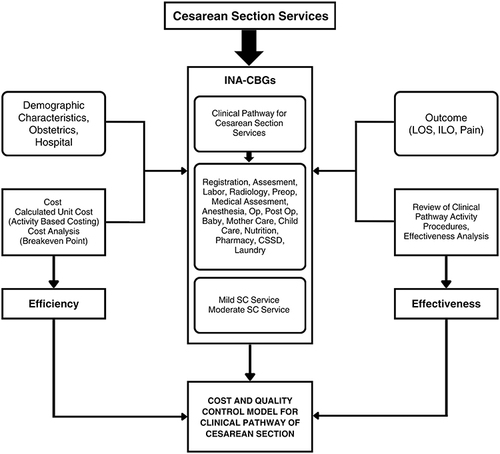
The third stage is making the initial product (prototype) in the form of a clinical pathway model framework for CS services that has been adjusted to the cost (efficiency) analysis and quality (effectiveness) analysis of all procedures (activities) for CS services. The prototype model was developed based on the Quality Care Framework Theory from Donabedian (1973), where the essence of the conceptual framework is to carry out continuous improvement efforts in the quality control cycle of cost control by looking at the aspects of structure, process, and output/outcome, as shown in .Citation10 This development research uses interviews, Delphi techniques, and clinical pathway guidelines to obtain a new prototype model, which will be validated again to obtain a new, permanent model. Qualitative research for design validation and model development was conducted in 4 class C hospitals, and 56 person as validators of each activity consist of 37 heads of installation, 6 staff, 1 General Practitioner, 8 Specialist, 3 pharmacists, 1 pharmacist assistant.Citation14,Citation15 This qualitative data collection was carried out by in-depth interviews, observation, document review, and focus group discussion (FGD). In collecting qualitative data, the researcher was assisted with recording equipment, a list of questions, notebooks, observation checklists, and document review checklists. The form of a clinical pathway model framework for CS is shown in .
Results
The study was carried out across 11 hospitals in West Sumatra Province, with 6 public hospitals (55%) and 5 private hospitals (45%) included. Out of all patients, 100 (90.9%) patients received mild CS services, while 10 (9.1%) patients received moderate CS. The majority of patients who underwent CS were from rural areas (57%). Almost half of the patients were between the ages of 30–39 (47.3%) and were housewives (79.1%). A large percentage of patients had primary education (Elementary school, Junior high school and senior high school) (79%) and earned below 1.5 million rupiahs (44.5%). Around 29% of patients had parity 1. The gestational age at the time of CS fell between 37–42 weeks for 85.5% of patients. Over half had a previously undergone a CS (60%), and had attended four ante-natal visits (61.8%). Fortunately, there were no reported surgical wound infections, and only a small percentage of patients (4.5%) reported experiencing surgical wound pain. Most patients (79%) were able to be discharged after only three days of stay (LOS), resulting in positive outcomes.
Hospital J has the highest direct cost of US$ 226.12, while Hospital A boasts the lowest direct cost of US$ 125.49. To calculate the unit cost, both direct and indirect costs are taken into consideration. The unit cost for mild CS services was lowest at hospital C (US$ 205.81), whereas it was highest for hospital D (US$ 754.29). In addition for moderate CS the lowest unit cost was for Hospital K (US$ 305.22) and highest for Hospital D (US$ 755.62). Please refer to for further details.
Table 1 Calculation of Costs and Tariffs for CS Services
In this study, 50 patients (45%) received CS services that were efficient, while 85 patients (77%) received services that were effective. These findings are presented in and , respectively. The study also discovered that 40 patients (36.4%) received CS services that were both effective and efficient, while 46 patients (41.8%) received services that were effective but not efficient. Please refer to
Table 2 Efficiency Distribution of CS Services According to Treatment Class
Table 3 Distribution of the Effectiveness of Cesarean Section Services by Class of Treatment
Table 4 Distribution Efficient and Effective, Efficient and Ineffective, Inefficient and Effective, and Inefficient and Ineffective of CS Services
This clinical pathway is a matrix consisting of several columns. The first column is the CS service activity. There are 14 activities ranging from registration to pharmaceutical activities. The second column describes activities and activity steps carried out in the context of CS services. The description of this activity is the result of observation and refers to the standards set by the hospital and existing regulations. The third column is the average time required for the activity or steps of the service activity (time spent), calculated in minutes. In the time column, the average number is obtained from the observations made by researchers in each CS service activity. The fourth column is when the activity description is carried out in the context of CS services, whether on the first day, second day or third day, according to predetermined standards. A checkmark in the day column indicates that predetermined standards are carried out. The fifth column is the variant column if an activity is not carried out by the existing document, and the reason is in the description column. The seventh column is the cost column, which is direct and indirect costs calculated in USD units. Regarding the cost column, it is divided into 2 columns, namely direct costs and indirect costs.
Discussion
The unit cost in this study results from the sum of direct and indirect costs.Citation28 The unit cost for CS varies from US$205.81 to a maximum of US$755.62, where the significant difference is due to the higher indirect costs at government hospitals compared to private hospitals. High direct and indirect costs are a barrier to utilizing maternity care, especially for many poor households.Citation29 Research in Ethiopia discovered that the hidden costs of CS were higher than other delivery modes for up to 28% of yearly family income in Ethiopia due to the complex procedures and more extended length of stay in the hospital.Citation30 A similar study estimated that 79% of households in Bangladesh did not have enough money to pay for delivery, and they had to borrow from friends and relatives.Citation31 Research in Cambodia found different things where the unit costs for government hospitals were lower than private hospitals.Citation32 CS service tariffs are calculated from the unit cost plus the tariff policy set by the hospital leadership. The tariff policy uses a target rate of return pricing, which is the setting of tariffs where the board of directors has determined the target profit amount.
The CS service tariffs are calculated based on unit cost and hospital tariff policy. The tariff policy uses target rate of return pricing to determine profit. Based on the findings of the study, 36% of patients received efficient and effective CS services that met established quality standards without incurring additional costs. However, this finding also revealed that the remaining CS services failed to adhere to cost control and quality control principles by less than 50%, indicating a need for improvement.
In this study, 16 activities procedure related to CS services were observed in 110 patients. The results showed that all procedures were implemented correctly in all cases. These findings indicate that the 11 hospitals which were part of the study provide high-quality services. This can be attributed to the fact that all of these hospitals have received approval from the Hospital Accreditation Committee (KARS) as a requirement for operating in conjunction with the National Health Insurance (BPJS).Citation33
The Integrated Clinical Pathways (ICP) for CS services in this study is a planning document structured as a map and model of a collection of clinical and non-clinical care activities from various CS service units in hospitals within the framework. Clinical pathways have several advantages and benefits, namely: improving medical services and patient-focused care because patients can participate in what is planned, being able to provide feedback about the results achieved, providing patient education and information about the care provided, facilitating collaboration in multidisciplinary teams in medical and nursing services.Citation11,Citation17 Furthermore, using ICP in the CS would minimize the length of stay in the hospital (LOS) and reduce hospital expenses.Citation34,Citation35
This model was developed based on the Quality Care Framework model from Donabedian (1973), where the essence of the conceptual framework is to carry out continuous improvement efforts of the quality control cycle of cost control by looking at the aspects of structure, process, and output/outcome.Citation10
The clinical pathway for CS services consists of three phases, namely the preoperative, intraoperative and postoperative. Refer to Supplementary Material 1 for further details. Preoperative consists of registration, initial assessment procedures and education (general practitioners, specialists, nurses and nutritionists), laboratory examination procedures, diagnostic examination procedures (USG, CTG, CT Scan), medical procedures and preoperative procedures. The intraoperative phase consists of anesthetic procedures, surgical procedures and the initial assessment and procedures for the baby. Postoperatively consists of postoperative care procedures, maternal care service procedures, child care service procedures and nutrition procedures (food services), as well as registration and discharge education.Citation36
In this study, researchers have developed a model in the form of an integrated clinical pathway. This model was developed from the results of cost analysis and activity procedure analysis in effective and efficient CS services, which were found in 40 cases of study subject patients. The workflow of mild CS services is the main part. Analyzed within the framework of management accounting and quality management. An overview of this model is as follows:
The main part of this model is the CS service activity procedure, carried out from the initial admission to the hospital until discharge.
There are 14 service activities, divided into 3 major groups: pre-operation, operation and post-operation.
Within the cost control framework, there is 1 module and 1 program, namely the indirect cost calculation module using the Activity Based Costing (ABC) method and the efficiency analysis program using the Break Even Point method.
Within the quality control framework, there is 1 program, namely the effectiveness analysis program, by analyzing the activity procedures and outcomes of CS services.
The output of all the modules and programs above, within the framework of the INA-CBG’s system of CS services and carried out in the hospital into a module called the module for quality control and cost control for CS services in hospitals.
Conclusion
The unit cost for mild CS services ranged from US$ 205.81 to US$755.62, while moderate CS services ranged from $305.22 to $755.62. The average cost of effective CS services is $249.14, with tariffs for mild services ranging from $246.97 to $754.29 and those for moderate services from $320.64 to $755.62.
Health care for cesarean section was efficient as well effective in approximately 36.4% patients. To ensure quality control and cost control for CS services, an Integrated Clinical Pathway model was obtained by combining quality as well as indirect cost control. This is recommended that hospitals follow the above Integrated Clinical Pathway to implement cost effective maternity health care, resilient to any changes in health care financing.
Abbreviations
4-D, define, design, develop, and dissemination; ABC, activity based costing; ASA, American society of anesthesiologists; ICP, integrated clinical pathway; INA-CBGs, Indonesia-case based groups.
Ethics Approval and Informed Consent
This study was carried out in accordance with the principles of the Helsinki Declaration. The Faculty of Medicine’s Research Ethics Committee at Andalas University in Padang, Indonesia, granted ethical approval for this study. (Approval number:1133/UN.16.2/KEP-FK/2021). Informed consent was obtained from all study participants.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Acknowledgments
The author would like to thank the Faculty of Medicine and the Faculty of Economics, Andalas University, which have provided facility support to carry out this research.
Data Sharing Statement
The data that support the study’s findings are accessible upon request from the corresponding author.
Additional information
Funding
References
- Indonesian Ministry of Health. Indonesia district health survey 2017: national population and family planning board statistics Indonesia; 2018.
- Santoso BI, Trisnantoro L, Hendra Y. Cesarean section tariff analysis based on Indonesian case base groups in cipto mangunkusumo hospital. Adv Sci Lett. 2017;23(4):3590–3593. doi:10.1166/asl.2017.9188
- Wang W. Costs-Effectiveness Analysis of Elective Cesarean Section Compared with Vaginal Delivery: A Prospective Cohort Study in a Hospital in León, Nicaragua. Uppsala University; 2016.
- Molina G, Weiser TG, Lipsitz SR, et al. Relationship between cesarean delivery rate and maternal and neonatal mortality. JAMA. 2015;314(21):2263. doi:10.1001/jama.2015.15553
- Indonesian Ministry of Health. Indonesian basic health research. Science. 2013;127:2013.
- Indonesian Ministry of Health. Indonesian basic health research; 2018:674.
- Aden J. Implementation of Cost Control and Quality Control of Health Services of Kutai Kartanegara Regional Health Insurance Programme at RSUD Parikesit Tenggarong. Gajah Mada Univ; 2012.
- Miller NH. Pricing health benefits: a cost-minimization approach. J Health Econ. 2005;24(5):931–949. doi:10.1016/j.jhealeco.2005.03.001
- Indonesian Ministry of Health. Regulation of Indonesian minister of health number 71 of 2013 concerning health services at the national health insurance; 2013.
- Donabedian A. The Definition of Quality and Approaches to Its Assessment. In: Explorations in Quality Assessment and Monitoring. Ann Arber, MI: Health Administration Press; 1980.
- Lin D, Zhang C, Shi H. Effects of clinical pathways on cesarean sections in china: length of stay and direct hospitalization cost based on meta-analysis of randomized controlled trials and controlled clinical trials. Int J Environ Res Public Health. 2021;18(11):1.
- Rotter T, Kinsman L, James E, et al. Clinical pathways: effects on professional practice, patient outcomes, length of stay and hospital costs. Cochrane Database Syst Rev. 2010;3:CD006632.
- Cunningham FG. Williams Obstetric. 25th ed. Mcgraww-Hill Education; 2018.
- Sugiyono. Qualitative and Quantitative Research Methods R&D. Bandung: Alfabeta; 2013.
- Sastroasmoro S, Ismael S. Dasar-dasar Metodologi Penelitian Klinis; 2016.
- Koss E, Lewis DA. Productivity or efficiency-measuring what we really want. Natl Productivity Rev. 1993;12(2):273–284. doi:10.1002/npr.4040120212
- Big dictionary of discussions Indonesian. Efficiency. Available from: https://kbbi.web.id/efficiency. Accessed May 20, 2024.
- Aljunid SM, Moshiri H, Ahmed Z. Measuring Hospital Efficiency Theory and Methods. Kuala Lumpur: Casemix Solutions; 2013.
- Roztocki N, Al E, Thomas RM, Needy KL. A procedure for smooth implementation of activity-based costing in small companies. Eng Manag J. 2015;16(4):19–27. doi:10.1080/10429247.2004.11415262
- McGee J. Break Event Analysis. Wiley Encycl Mangement; 2015.
- Indonesian Ministry of Health. Indonesia ministry of health regulation number 52 (2016) Indonesia case based groups (INA-CBGs) and non Indonesian case based, concerning health service tariff standards in the implementation of the health insurance program; 2016.
- Big Dictionary of Discussions Indonesian (KBBI). Effectiveness. Available from: https://kbbi.web.id/effectiveness. Accessed May 20, 2024.
- Gibson. Organisasi-Perilaku-Struktur-Proses. Jakarta: Erlangga; 2002.
- Moshiri H, Aljunid SM, Amin RM. Hospital efficiency: concept, measurement techniques and review of hospital efficiency studies. Malaysian J Public Heal Med. 2010;10(2):35–43.
- Naghma Naeem. Validity, reliability, feasibility, acceptability, and educational impact of direct observation of procedural skills. J Coll Physicians Surg Pakistan. 2013;23(1):77–82.
- Indonesian Ministry of Home Affair. Indonesian ministry of home affair regulation number 690.900.327 (1996) regarding guidelines for evaluating financial performances; 1996.
- Cegolon L, Mastrangelo G, Campbell OM, et al. Length of stay following cesarean sections: a population based study in the Friuli Venezia Giulia region (North-Eastern Italy), 2005–2015. PLoS One. 2019;14(2):e0210753. doi:10.1371/journal.pone.0210753
- Indonesian Hospital Association. Financial Management and Accounting for Indonesian Hospitals - Series 3: Accounting. Persi: Indonesian Hospital Association; 2018.
- Khan A, Zaman S. Costs of vaginal delivery and Caesarean section at a tertiary level public hospital in Islamabad, Pakistan. BMC Pregnancy Childbirth. 2010;10(1):2. doi:10.1186/1471-2393-10-2
- Merga M, Debela TF, Alaro T. Hidden costs of hospital-based delivery among women using public hospitals in Bale Zone, Southeast Ethiopia. J Prim Care Community Health. 2019;10:2150132719896447. doi:10.1177/2150132719896447
- Nahar S, Costello A. The hidden cost of free maternity care in Dhaka. Bangladesh Health Policy Plan. 1998;13(4):417–422. doi:10.1093/heapol/13.4.417
- Glaeser E, Jacobs B, Appelt B, et al. Costing of cesarean sections in a government and a non-governmental hospital in Cambodia-a prerequisite for efficient and fair comprehensive obstetric care. Int J Environ Res Public Health. 2020;17(21). doi:10.3390/ijerph17218085
- Hospital Accreditation Commission. List of accredited hospitals; 2022. Available from: https://kars.or.id/ws/view_hasil_akreditasi.php. Accessed May 20, 2024.
- Bin W, Di C, Hongwei Z, Huaxin S, Qi X. Influence of clinical pathways used the hospitals of Traditional Chinese Medicine on patients hospitalized with stroke: a systematic review and Meta-analysis. J Tradit Chin Med. 2017;37(2):159–164. doi:10.1016/S0254-6272(17)30039-0
- Saint S, Hofer TP, Rose JS, Kaufman SR, McMahon LFJ. Use of critical pathways to improve efficiency: a cautionary tale. Am J Manag Care. 2003;9(11):758–765.
- Hospital Accreditation Commission. Hospital Accreditation Instrument Accreditation Standard Version 2012. Jakarta: KARS; 2012.