 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Inpatient geriatric falls are a frequent complication of hospital care that results in significant morbidity and mortality.
Objective
Evaluate factors associated with falls in geriatric inpatients after implementation of the fall prevention program.
Methods
Prospective observational study comprised of 788 consecutive patients aged 79.5±7.6 years ( ± standard deviation) (66% women and 34% men) admitted to the subacute geriatric ward. Comprehensive geriatric assessment (including Mini-Mental State Examination, Barthel Index of Activities of Daily Living, and modified Get-up and Go Test) was performed. Confusion Assessment Method was used for diagnosis of delirium. Patients were categorized into low, moderate, or high fall risk groups after clinical and functional assessment.
Results
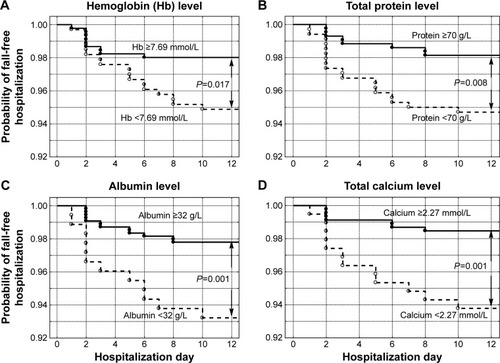
About 15.9%, 21.1%, and 63.1% of participants were classified into low, moderate, and high fall risk groups, respectively. Twenty-seven falls were recorded in 26 patients. Increased fall probability was associated with age ≥76 years (P<0.001), body mass index (BMI) <23.5 (P=0.007), Mini-Mental State Examination <20 (P=0.004), Barthel Index <65 (P=0.002), hemoglobin <7.69 mmol/L (P=0.017), serum protein <70 g/L (P=0.008), albumin <32 g/L (P=0.001), and calcium level <2.27 mmol/L. Four independent factors associated with fall risk were included in the multivariate logistic regression model: delirium (odds ratio [OR] =7.33; 95% confidence interval [95% CI] =2.76–19.49; P<0.001), history of falls (OR =2.55; 95% CI =1.05–6.19; P=0.039), age (OR =1.14; 95% CI =1.05–1.23; P=0.001), and BMI (OR =0.91; 95% CI =0.83–0.99; P=0.034).
Conclusion
Delirium, history of falls, and advanced age seem to be the primary risk factors for geriatric falls in the context of a hospital fall prevention program. Higher BMI appears to be associated with protection against inpatient geriatric falls.
Introduction
Inpatient geriatric falls are a frequent complication of hospital care that results in significant morbidity and mortality, including serious injuries, prolonged hospitalization, increased hospital financial liability, decreased quality of life, and increased risk for placement in nursing homes.Citation1–Citation6 Prevention strategies and interventions that have been implemented at the hospital and hospital ward level have been shown by others to reduce the number of fall incidents.Citation7,Citation8 Multiple fall risk factors have been identified in community-dwelling elderly, among them specific medical conditions,Citation9–Citation12 balance and gait disorders, history of falls, visual impairment, advanced age, female sex, polypharmacy, pain, cognitive decline, and environmental factors.Citation13,Citation14 Certain medications have also been shown to be associated with increased fall risk in community-based elderly, including antiarrhythmics, nonselective β-blockers, benzodiazepines, and antidepressants.Citation15 Specifically in hospitalized patients, alterations in consciousness, inattention,Citation16 confusion,Citation17 anemia, osteoporosis, and a history of fallsCitation3 as well as specific medications, including benzodiazepines, haloperidol, tricyclic antidepressants,Citation17 zolpidem, and calcium channel antagonists,Citation18 were identified as fall risk factors. The STRATIFY scale was found to be the best tool for assessing the risk of falls for hospitalized acutely ill adults.Citation19 However, no screening tool has shown sufficient prognostic accuracy to be recommended for predicting falls among newly admitted acute care hospital patients aged 65 years or older.Citation20,Citation21
In 2013, a standard operational program for fall and delirium prevention was implemented in the Department of Geriatrics at University Hospital Number 7 SUM, Katowice, Poland, a subacute geriatric ward at a multiprofile university hospital. For the purposes of the program, fall was defined as a sudden, uncontrolled body transition caused by loss of body balance control or body support instability. In addition to inpatient geriatric fall prevention strategies described by others,Citation1 this program classifies patients at admission according to three levels of geriatric fall risk: low, moderate, and high (). The assessment includes clinical and functional evaluation made by the department team. Initial fall risk classification is modified if patient status changes significantly during hospitalization. On the basis of a comprehensive geriatric assessment, an individualized multifactorial approach to reduce patient fall risk is applied. Patient ambulation is restricted based on patient fall risk assessment: moderate-risk patients are instructed to request staff assistance before ambulating between dusk and dawn, while high fall risk patients are instructed to request staff assistance before ambulating at all times. These restrictions are accompanied by an individualized rehabilitation program for each patient, directed at early mobilization and maintenance of mobility. Patients with cognitive impairment are provided with increased nursing surveillance. The program requires the documentation and analysis of all patient fall data irrespective of fall complications. The study was designed to analyze geriatric falls in hospitalized patients after implementation of a fall prevention program.
Table 1 Components of the fall prevention program implemented in the Department of Geriatrics at University Hospital Number 7 SUM, Katowice, Poland
Patients and methods
Participants
This prospective observational study comprised of 788 consecutive patients aged 79.5±7.6 years ( ± standard deviation) within a range of 60–100 years, among whom 66% were women and 34% were men. Participants were admitted to the Department of Geriatrics at University Hospital Number 7 SUM Uppersilesian Medical Center in Katowice, Poland, a subacute geriatric ward at a multiprofile university hospital, between June 2013 and June 2014.
Measurements
Patients were evaluated by taking comprehensive general history (including fall history and balance disorders) and by performing a physical examination (postural balance and gait assessment), geriatric functional assessment, blood work (), electrocardiogram, abdominal ultrasound, and chest X-ray. BIS_cr equationCitation22 was used to estimate glomerular filtration rate. This method is recommended in very elderly persons if cystatin C is not available.Citation23 Modified Get-up and Go TestCitation24 (scored from 0 to 10 with lower values suggesting increased ambulatory disability) was used to evaluate patient fall risk. The test consists of five exercises: 1) rise from a hard chair with backrest, 2) stand for 5 seconds, 3) walk a distance of 3 m at normal speed, 4) execute a 180° turn and return to the chair, and 5) sit down in the chair. Each of the tasks is scored either 2 points (normal, confident, self-reliant performance), 1 point (mildly to moderately abnormal performance – use of orthopedic devices or any deviation from a confident, normal, but self-reliant, performance), or 0 points (severely abnormal – need for staff assistance or inability of self-reliant performance of the exercise). Tinetti Performance-Oriented Mobility AssessmentCitation25 was also applied in a limited number of cases to assess risk of falls (scored from 0 to 28 with lower values indicating higher fall risk). Mini-Mental State Examination (MMSE)Citation26 was used to assess global cognitive performance. Geriatric Depression Scale–Short Form was used to screen for depression.Citation27 Barthel Index of Activities of Daily Living (Barthel Index)Citation28 and Lawton Instrumental Activities of Daily Living Scale (IADL)Citation29 were used to determine functional status. MMSE scores range from 0 to 30, Barthel Index from 0 to 100, and IADL from 9 to 27; higher scores indicate better functional status. Geriatric Depression Scale–Short Form scores range from 0 to 15, with higher scores indicating higher depression probability. Confusion Assessment Method for diagnosis of deliriumCitation30 was applied. Dementia was diagnosed according to recommendations from the National Institute on Aging-Alzheimer’s Association.Citation31 Pain intensity was assessed with the Visual Analog ScaleCitation32,Citation33 scored from 0 to 10, or with Doloplus-2 scaleCitation34,Citation35 based on the behavioral–observational method and scored from 0 to 30 points (with higher scores indicating more severe pain) in patients who were unable to report pain intensity because of cognitive impairment. To harmonize both pain scales, Doloplus-2 values were divided by a factor of 3 and pain intensity was scored from 0 to 10 in each patient. Body mass index (BMI) was calculated in all subjects. On the basis of clinical and functional assessment, patients were categorized into low, moderate, and high fall risk groups ().
Table 2 Demographic, clinical, and functional differences between patients who experienced falls during hospitalization (group F) as compared with patients who did not (group C)
Data collection
Data was collected by three research nurses and entered into predefined forms.
Statistical analysis
Data were analyzed using STATISTICA version 10 (StatSoft, Inc., Tulsa, OK, USA). Chi-square test, V-square test, and Fisher’s exact test were used for categorical variables, and the nonparametric Mann–Whitney U-test for quantitative variables was used to compare patients who experienced a fall during hospitalization with those who did not. Probability density analysis was used to calculate fall probability with regard to hospitalization day and time. Multivariate binary logistic regression was performed to assess factors predictive of falls. Variables were adjusted for clinical, functional, and laboratory factors. Multivariate analysis with backward elimination included variables that yielded P-values of 0.1 or lower in the initial univariate analysis (). The Kaplan–Meier method was used to estimate probability of fall-free hospitalization in subgroups of patients with respect to select variables, while differences between these subgroups were assessed with the Wilcoxon–Gehan method. Variables were tested to define the value corresponding with the lowest P level. P-values <0.05 were considered statistically significant.
Table 3 Variables that yield P-values of 0.1 or lower in the initial univariate logistic regression analysis of factors predictive of falls
Ethics
The study protocol was registered with the Bioethical Committee of the Medical University of Silesia in Katowice, Poland. The committee determined that “the study is characterized by record review and in the context of law is not a medical experiment and does not require assessment by the bioethical committee” (Letter KNW/0022/KB/78/I/13). On the basis of this decision, study participant written informed consent was not required for our study nor was separate patient consent required for our statistical analysis or research since patient data are not disclosed outside internal hospital ward staff.
Results
On the basis of assessment at admission, 15.9%, 21.1%, and 63.1% of study participants were classified into low, moderate, and high fall risk groups, respectively. Twenty-seven falls were registered in 26 patients; three falls in the low-risk group of 125 patients (11.5% of patients who fell), three falls in the moderate-risk group of 166 patients (11.5%), and 20 falls in the high-risk group of 497 patients (76.9%). No fall was complicated by serious injury or decline in functional status. Increased hospital fall activity occurred on day 2 of hospitalization, with day 0 taken as day of admission (). We observed a 24-hour biphasic pattern of increased falls with a minor spike between 04:00 and 05:00 and a major spike in the evening, about 21:00 (). Among other demographics, laboratory, and clinical factors, patients with dementia, treated with neuroleptics before and during hospitalization, as well as patients with lower cognitive and functional status tended to be associated with increased falls (). Increased fall probability was associated with age ≥76 years (P<0.001), BMI <23.5 (P=0.007), MMSE <20 (P=0.004), and Barthel Index <65 (P=0.002; ), as well as with hemoglobin level <7.69 mmol/L (P=0.017), serum protein level <70 g/L (P=0.008), albumin level <32 g/L (P=0.001), and calcium level <2.27 mmol/L (P=0.001) (). Four independent factors associated with risk of fall were included in the multivariate logistic regression model: delirium occurrence at the ward (odds ratio [OR] =7.33; 95% confidence interval [CI] =2.76–19.49; P<0.001), history of falls (OR =2.55; 95% CI =1.05–6.19; P=0.039), age (OR =1.14; 95% CI =1.05–1.23; P=0.001), and BMI (OR =0.91; 95% CI =0.83–0.99; P=0.034).
Figure 1 Fall probability of geriatric inpatients who experienced a fall incident during hospitalization in relation to hospitalization day.
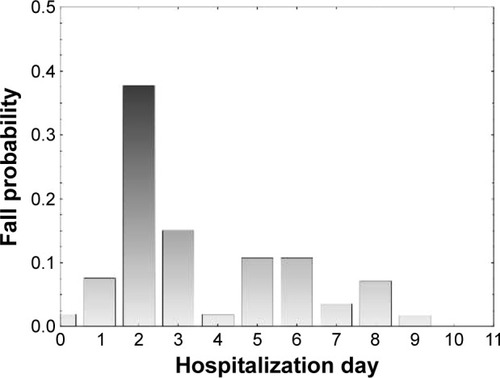
Figure 2 Fall probability of geriatric inpatients who experienced a fall incident during hospitalization in relation to the time of day.
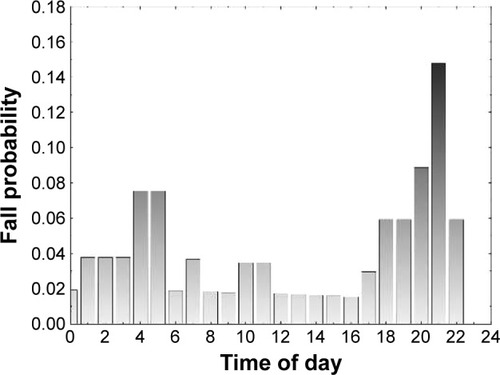
Figure 3 Probability of fall-free hospitalization according to (A) age <76 years compared to older age, (B) BMI ≥23.5 compared to lower values, (C) MMSE scores ≥20 compared to lower values, and (D) Barthel Index of Activities of Daily Living (BI) ≥65 compared to lower values.
Abbreviations: BMI, body mass index; MMSE, Mini-Mental State Examination.
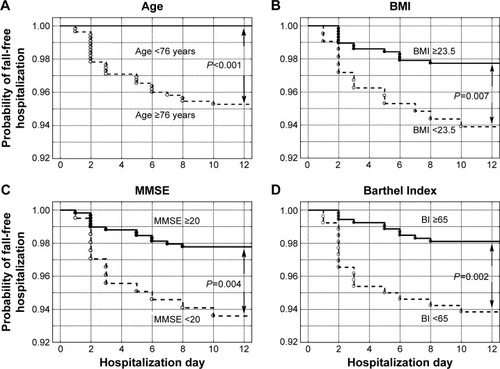
Figure 4 Probability of fall-free hospitalization according to (A) hemoglobin level ≥7.69 mmol/L compared to lower values, (B) serum total protein level ≥70 g/L compared to lower values, (C) serum albumin level ≥32 g/L compared to lower values, and (D) serum total calcium level ≥2.27 mmol/L compared to lower values.
Discussion
As is the case for many geriatric syndromes, fall prevention in the hospital or health care facility setting requires multifactorial risk assessment and interventions tailored to specific patient needs.Citation36 Fall risk factors in the elderly may differ depending on local environmental conditions. Despite numerous studies, no well-defined and highly effective fall prevention program for the elder-care setting has been described. Therefore, it seems reasonable to compare results from different centers. We examined fall incidence and related risk factors in geriatric ward patients after implementation of a staff-developed fall prevention program in 2013. A significant proportion of our patients were identified during screening as being at moderate or high fall risk, which is consistent with other similar studies.Citation20,Citation21 This suggests high sensitivity but low specificity and obviates the need for better fall prediction tools for assessing geriatric patients admitted to the acute care hospital wards. Serious injury or decline in functional status was not observed as a consequence of the 27 recorded falls that 26 patients experienced during the study period. Notably, we observed an increased fall probability on the second day of patient hospitalization during evening hours. This observation, of particular practical significance, is most likely multifactorial and complex. Loss of visual perception during periods between dusk and dawn may have a magnified effect in persons with impaired senses, including geriatric patients. This explanation would seem to be supported by studies associating lighting and perceptual cues in older adults with risk of falls.Citation37 Evening or nocturnal psychomotor agitation (sundown syndrome) is a common phenomenon in patients with cognitive impairment, which may result in failure to adhere to ambulatory restrictions and result in increased tendency toward falls.Citation38 In the literature, data on 24-hour fall patterns in the hospital setting are inconsistent.Citation39 Among demographic and clinical characteristics of patients who experienced falls, advanced age, history of falls, dementia, and poor functional state were, as it would be expected from other studies,Citation36 factors predictive of falls. Lower BMI appeared to be another risk factor in our study group. Coutinho et alCitation40 showed that BMI ≤20, cognitive impairment, previous stroke, and lack of urine control were associated with increased incidence of severe fall-related fractures in 250 hospitalized patients matched with 250 community controls. O’Neil et alCitation17 found association between low BMI (≤18.5) and increased risk of hospital falls. Decreased body mass may be related to frailty, a syndrome prevalent in geriatric inpatients,Citation41 associated with increased fall risk.Citation42 Both low and very high BMI are associated with increased prevalence of frailty.Citation43 However, some observations indicate that obesity may be protective against falling in community-dwelling older adults.Citation44 Delirium appears to be the greatest risk factor for falls in our cohort of inpatients. Delirium-related cognitive deterioration combined with psychomotor agitation acutely impairs both patient compliance and secure mobility.Citation45,Citation46 Other studies demonstrated that agitation was associated with falls in patients residing in elder-care units.Citation47,Citation48 Delirium has also been associated with previous falls both in acute general medicine patientsCitation49 as well as in geriatric ward patients.Citation50 A history of falls has been recognized as predictive of future falls during hospitalization.Citation51
Implementation of a geriatric fall prevention program in the hospital setting presents unique challenges for medical professionals. Particular care must be taken to address fall interventions that may also inadvertently complicate comorbid conditions. Specifically, restricting patient-independent ambulation during hospitalization in moderate- and high-risk patients may decrease overall ambulation during hospitalization in these patients and increase the probability of delirium. Additional concerns with restriction of independent ambulation include strain on limited staff time, eliciting or enhancing a fear of falling among a susceptible population,Citation52 or even the implication of loss of independence.Citation36 A critical compensatory intervention in this respect is a comprehensive individualized rehabilitation program directed toward early mobilization and maintenance of mobility for prevention of both falls and their risk factors, including delirium.Citation1,Citation45 Given the morbidity and mortality associated with hospital falls, clinicians have been working toward the goal of decreasing hospital falls to the point of “never-events”.Citation53 In this respect, temporary limits on patient-independent ambulation during hospitalization seem reasonable.
The main limitation of our study was the lack of fall risk comparison before and after program implementation. Our fall prevention program assessed all patients admitted to the ward and documented all patient falls irrespective of fall complications. Since fall data before program implementation were incomplete, we were unable to assess the effectiveness of the program interventions. Nevertheless, it appears that an effective fall prophylaxis program requires implementation of evidence-based as well as common-sense interventions and counseling strategies.
Conclusion
Delirium, history of falls, and advanced age seem to be the primary risk factors for geriatric falls in the context of a hospital fall prevention program. Higher BMI appears to be associated with protection against inpatient geriatric falls.
Funding
This project was funded by Medical University of Silesia grants to statutory work (contracts KNW-1-029/K/4/0) and graduate student research agreement (KNW-2/035/D/4/N).
Disclosure
The authors report no conflicts of interests in this work.
References
- InouyeSKBrownCJTinettiMEMedicare nonpayment, hospital falls, and unintended consequencesN Engl J Med20093602390239319494213
- CameronIDGillespieLDRobertsonMCInterventions for preventing falls in older people in care facilities and hospitalsCochrane Database Syst Rev201212CD00546523235623
- al TehewyMMAminGENassarNWA study of rate and predictors of fall among elderly patients in a university hospitalJ Patient Saf20151121021425010190
- AndersonDCPostlerTSDamTTEpidemiology of hospital system patient falls: a retrospective analysisAm J Med Qual Epub482015
- BasicDHartwellTJFalls in hospital and new placement in a nursing home among older people hospitalized with acute illnessClin Interv Aging2015101637164326508846
- TwibellRSSielaDSproatTCoersGPerceptions related to falls and fall prevention among hospitalized adultsAm J Crit Care201524e78e8526330442
- OliverDConnellyJBVictorCRStrategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analysesBMJ20073348217158580
- QuigleyPABarnettSDBulatTFriedmanYReducing falls and fall-related injuries in medical-surgical units: one-year multihospital falls collaborativeJ Nurs Care Qual20163113914526323049
- RudzińskaMBukowczanSStożekJCauses and consequences of falls in Parkinson disease patients in a prospective studyNeurol Neurochir Pol20134742343024166563
- LeeKPresslerSJTitlerMFalls in patients with heart failure: a systematic reviewJ Cardiovasc Nurs Epub9292015
- MinetLRPetersonEvon KochLYtterbergCOccurrence and predictors of falls in people with stroke: six-year prospective studyStroke2015462688269026243230
- MamotoKInuiKOkanoTIncidence rate of falls and its risk factors in patients with rheumatoid arthritis compared to controls: four years of the TOMORROW studyMod Rheumatol Epub542016
- AmbroseAFPaulGHausdorffJMRisk factors for falls among older adults: a review of the literatureMaturitas201375516123523272
- MunchTHarrisonSLBarrett-ConnorEPain and falls and fractures in community-dwelling older menAge Ageing20154497397926396181
- HamACSwartKMEnnemanAWMedication-related fall incidents in an older, ambulant population: the B-PROOF studyDrugs Aging20143191792725398701
- DohertyKArchambaultEKellyBRudolphJLDelirium markers in older fallers: a case-control studyClin Interv Aging201492013201825473272
- O’NeilCAKraussMJBettaleJMedications and patient characteristics associated with falling in the hospitalJ Patient Saf Epub3162015
- KozonoAIsamiKShiotaKRelationship of prescribed drugs with the risk of fall in inpatientsYakugaku Zasshi201613676977627150933
- Aranda-GallardoMMorales-AsencioJMCanca-SanchezJCInstruments for assessing the risk of falls in acute hospitalized patients: a systematic review and meta-analysisBMC Health Serv Res20131312223547708
- MatareseMIvzikuDBartolozziFPireddaMDe MarinisMGSystematic review of fall risk screening tools for older patients in acute hospitalsJ Adv Nurs2015711198120925287867
- LattMDLohKFGeLHepworthAThe validity of three fall risk screening tools in an acute geriatric inpatient populationAustralas J Ageing Epub3152016
- SchaeffnerESEbertNDelanayePTwo novel equations to estimate kidney function in persons aged 70 years or olderAnn Intern Med201215747148123027318
- LopesMBAraújoLQPassosMTEstimation of glomerular filtration rate from serum creatinine and cystatin C in octogenarians and nonagenariansBMC Nephrol20131426524295505
- MathiasSNayakUSIsaacsBBalance in elderly patients: the “get-up and go” testArch Phys Med Rehabil1986673873893487300
- TinettiMEPerformance-oriented assessment of mobility problems in elderly patientsJ Am Geriatr Soc1986341191263944402
- FolsteinMFFolsteinSEMcHughPRMini-mental state: a practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res1975121891981202204
- SheikhJIYesavageJAGeriatric Depression Scale (GDS): recent evidence and development of a shorter versionClin Gerontol19865165173
- MahoneyFIBarthelDWFunctional evaluation: the Barthel IndexMd State Med J1965145661
- LawtonMPBrodyEMAssessment of older people: self-maintaining and instrumental activities of daily livingGerontologist196991791865349366
- InouyeSKvan DyckCHAlessiCAClarifying confusion: the confusion assessment method. A new method for detection of deliriumAnn Intern Med19901139419482240918
- McKhannGMKnopmanDSChertkowHThe diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s diseaseAlzheimers Dement2011726326921514250
- JoyceCRZutshiDWHrubesVMasonRMComparison of fixed interval and visual analogue scales for rating chronic painEur J Clin Pharmacol197584154201233242
- HjermstadMJFayersPMHaugenDFStudies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature reviewJ Pain Symptom Manage2011411073109321621130
- WaryBDoloplus-2, a scale for pain measurementSoins Gerontol201119252710745928
- Lefebvre-ChapiroSThe Doloplus-2 scale – evaluating pain in the elderlyEur J Palliat Care20018191194
- National Institute for Health and Care ExcellenceFalls. Assessment and prevention of falls in older people. Issued: June 2013NICE guidance number guidance.nice.org.uk/CG161 Available from: www.nice.org.uk/guidance/CG161Accessed March 6, 2016
- FigueiroMGPlitnickBReaMSGrasLZReaMSLighting and perceptual cues: effects on gait measures of older adults at high and low risk for fallsBMC Geriatr2011114921864387
- KhachiyantsNTrinkleDSonSJKimKYSundown syndrome in persons with dementia: an updatePsychiatry Investig20118275287
- López-SotoPJManfrediniRSmolenskyMHRodríguez-BorregoMA24-hour pattern of falls in hospitalized and long-term care institutionalized elderly persons: a systematic review of the published literatureChronobiol Int20153254855625471448
- CoutinhoES1FletcherABlochKVRodriguesLCRisk factors for falls with severe fracture in elderly people living in a middle-income country: a case control studyBMC Geriatr200882118727832
- BieniekJWilczyńskiKSzewieczekJFried frailty phenotype assessment components as applied to geriatric inpatientsClin Interv Aging20161145345927217729
- KojimaGKendrickDSkeltonDAMorrisRWGawlerSIliffeSFrailty predicts short-term incidence of future falls among British community-dwelling older people: a prospective cohort study nested within a randomised controlled trialBMC Geriatr20151515526625940
- HubbardRELangIALlewellynDJRockwoodKFrailty, body mass index, and abdominal obesity in older peopleJ Gerontol A Biol Sci Med Sci20106537738119942592
- SheehanKJO’ConnellMDCunninghamCCrosbyLKennyRAThe relationship between increased body mass index and frailty on falls in community dwelling older adultsBMC Geriatr20131313224313947
- FlahertyJHDeliriumSinclairAJMorleyJEVellasBPathy’s Principles and Practive of Geriatric Medicine25th edChichester, UKWilley-Blackwell2012837850
- InouyeSKWestendorpRGJSaczynskiJSDelirium in elderly peopleLancet201438391192223992774
- OliverDBrittonMSeedPMartinFCHopperAHDevelopment and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studiesBMJ1997315104910539366729
- HendrichALBenderPSNyhuisAValidation of the Hendrich II fall risk model: a large concurrent case/control study of hospitalized patientsAppl Nurs Res20031692112624858
- PendleburySTLovettNGSmithSCObservational, longitudinal study of delirium in consecutive unselected acute medical admissions: age-specific rates and associated factors, mortality and re-admissionBMJ Open20155e007808
- OtrembaIWilczyńskiKSzewieczekJDelirium in the geriatric unit: proton-pump inhibitors and other risk factorsClin Interv Aging20161139740527103793
- AmbroseAFPaulGHausdorffJMRisk factors for falls among older adults: a review of the literatureMaturitas201375516123523272
- FletcherPCHirdesJPRestriction in activity associated with fear of falling among community-based seniors using home care servicesAge Ageing20043327327915082433
- WatersTMDanielsMJBazzoliGJEffect of medicare’s nonpayment for hospital-acquired conditions: lessons for future policyJAMA Intern Med201517534735425559166
