Abstract
Purpose
To assess the factors involved in oral intake discontinuation in elderly patients with recurrent aspiration pneumonia.
Patients and methods
This study included patients with pneumonia who were treated at Jichi Medical University Hospital between 2007 and 2013, at Toyooka Public Hospital between 2011 and 2013 and at Yuzawa Community Medical Center between 2010 and 2012. We consecutively enrolled patients with aspiration pneumonia. The primary study point was oral intake discontinuation after the initiation of oral intake during hospitalization in cases of recurrent aspiration. Various parameters were recorded at admission, at the initiation of intake, and during hospitalization; these parameters were statistically evaluated.
Results
A total of 390 patients were assigned to either a “no reaspiration of intake” group (n=310) or a “reaspiration of intake” group (n=80), depending on whether intake was discontinued owing to aspiration during hospitalization. At admission, the following items significantly differed between the groups: level of consciousness, respiratory rate, oxygen saturation, CURB-65 score, extent of infiltration/opacity on chest radiography, albumin levels, blood urea nitrogen levels, and application of swallowing function assessment. At the initiation of intake, level of consciousness, pulse rate, and albumin levels significantly differed between the groups. The following items did not significantly differ between groups: systolic blood pressure, pulse rate, C-reactive protein, bacteremia, use of ventilator at admission, oxygen administration, respiratory rate, and systolic blood pressure at initiation of intake. Multivariate analysis revealed that application of swallowing function assessment, level of consciousness at the initiation of intake, and extent of infiltration/opacity on chest radiography were significant predictive variables for discontinuation of intake.
Conclusion
A low level of consciousness at the initiation of intake and a greater extent of infiltration/opacity on chest radiography and the application of a swallowing function are important factors. These factors may be helpful to determine a suitable timing for resumption of oral intake.
Introduction
Owing to the rapidly aging society in Japan, the number of deaths due to pneumonia has been constantly increasing. Recent statistics showed that pneumonia is the third most common cause of death, after malignant neoplasms and heart diseases, and has recently overtaken cerebrovascular diseases.Citation1 Over 120,000 patients (approximately 100 in a population of 100,000) are known to die from pneumonia annually, and this mortality rate is expected to increase further. The rate of death from pneumonia is higher in Japan than in other developed countries, many of which have mortality rates of less than 50 per 100,000 people. In contrast, the age-adjusted mortality rate of pneumonia is over 2,000 per 100,000 people in sub-Saharan Africa and in Southern Asia.Citation2
In particular, aspiration pneumonia is common among cases of pneumonia in the elderly and accounts for one-third of patients hospitalized with pneumonia aged 50–59 years, 50% of those hospitalized with pneumonia aged 60–69 years, and 80.1% of those hospitalized with pneumonia aged >70 years.Citation3 One report indicated that aspiration pneumonia is the strongest predictor of 30-day mortality in patients with pneumonia.Citation4 Thus, the treatment and prevention of aspiration pneumonia are critical to the medical treatment of pneumonia.
In patients with aspiration pneumonia, the method for ensuring oral intake is vital in terms of quality of life and prevention of recurrence. Studies have been published on the significance of antimicrobial agent selection, swallowing assessment, oral care, rehabilitation, and vaccination with a pneumococcal vaccine in cases of aspiration pneumonia.Citation5–Citation10
A recent study showed that aspiration pneumonia the strongest predictor of 30-day mortality among patients with pneumonia.Citation11 This study was based on the Diagnosis Procedure Combination database, which is a national Japanese database of administrative claims and discharge abstracts. However, the Diagnosis Procedure Combination database lacks detailed information regarding swallowing function, as well as the general patient’s status at the time of the initiation of oral intake. Hence, the predictive factors for the discontinuation of oral intake in elderly cases of recurrent aspiration pneumonia remain unclear. To our knowledge, no other study on these predictive factors has been conducted so far.
A previous study from our group showed that 63.7% of physicians made patients fast temporarily for the treatment of aspiration pneumonia.Citation12 In addition, when making decisions regarding oral intake resumption after aspiration pneumonia, more than 80% of clinicians responding to questionnaire answered either “Strongly agree” or “Agree” to the importance of the following items: level of consciousness, oxygen saturation (SpO2), the discretion of the attending physician, body temperature, whether swallowing function testing had been performed, mental state, respiratory rate, visual impression, pneumonia severity, performance status, the opinion of a nonphysician health care provider, administration of oxygen, the patient’s request, and the family’s request.Citation13 However, there is no evidence whether the respondent physicians’ opinions are clinically appropriate for preventing either a reduction in swallowing ability or a recurrence of aspiration pneumonia.
In the present study, we aimed to assess the factors involved in the discontinuation of oral intake in elderly patients with recurrent aspiration pneumonia in order to determine an appropriate timing for the resumption of oral intake.
Patients and methods
Study design
This was a retrospective cohort study. The study was approved by the Ethics Committee for Epidemiologic Research at Jichi Medical University. Owing to the retrospective nature of the study, the need for written informed consent was waived.
Study setting and population
We included patients with pneumonia who were hospitalized at the Division of General Internal Medicine, Jichi Medical University Hospital, Tochigi, Japan, between 2007 and 2013; at the Department of General Medicine, Toyooka Public Hospital, Hyogo, Japan, between 2011 and 2013 and at the Department of Community and Family Medicine, Yuzawa Community Medical Center, Niigata, Japan, between 2010 and 2012. Among these patients, those with aspiration pneumonia (International Classification of Diseases-10 code, J69) were consecutively enrolled. These patients did not have nasogastric or gastrostomy tube feeding or parenteral nutrition. Aspiration pneumonia was defined, in accordance with the consensus of the Japanese Respiratory Society,Citation5,Citation14 as pneumonia that developed in patients with proven or highly suspicious dysphagia or aspiration at follow-up. Dysphagia or aspiration dates were taken from families, a meal assistant before admission, or clinical course after admission. We included patients who had not discontinued eating at the time of admission to the hospital and those who never discontinued eating. We excluded patients who did not receive any oral intake until death or during the study period. We also excluded patients who required nasogastric or gastrostomy tube feeding or parenteral nutrition before admission.
Measurement items
The primary study point was the discontinuation of oral intake due to recurrent aspiration after the initiation of oral intake during the hospitalization course. Even a single episode of discontinuation was considered as discontinuation of oral intake. Oral intake was defined as an oral diet without nasogastric or gastrostomy tube feeding and without parenteral nutrition.
We measured the following items at admission: age, sex, comorbidities (tumor of the head and neck, history of gastroesophageal surgery, cerebral nerve disease, chronic lower respiratory disease, and diabetes mellitus), level of consciousness (Glasgow Coma Scale),Citation15 respiratory rate, SpO2, blood pressure, pulse rate, and body temperature. We also assessed the extent of infiltration/opacity on each patient’s chest radiography as well as each patient’s white blood cell count, serum albumin levels, blood urea nitrogen (BUN) levels, C-reactive protein levels, presence of bacteremia, and use of a ventilator. Each patient’s Eastern Cooperative Oncology Group performance status (PS; a PS score of 3 or 4 diagnostically indicates nursing- and health care-associated pneumonia)Citation5 was determined, and speech therapists tested swallowing function using a repetitive saliva swallowing test, a modified water swallow test, a food test, or a fiberoptic endoscopic evaluation of swallowing.Citation5,Citation6 In addition, each patient’s CURB-65 score was evaluated. This score is a measure of severity for community-acquired pneumonia that reflects confusion, BUN levels, respiratory rate, blood pressure, and age over 65 years.Citation16 Further information about CURB-65 can be found in and .
If a medical physician believed that a patient had normal swallowing function, then swallowing function was not assessed by a speech therapist. In these cases, physicians relied on information from the patients’ families and on dysphagia screenings by nurses. If a medical physician suspected that a patient had poor swallowing function, then a speech therapist assessed swallowing function, as described earlier. Accordingly, the application of a swallowing function assessment indicated a more severe case of dysphagia. The swallowing function testing was the same across all the three hospitals.
At the initiation of oral intake, we recorded the following items: period from admission to the initiation of intake, level of consciousness (Glasgow Coma Scale), respiratory rate, oxygen administration, blood pressure, pulse rate, body temperature, white blood cell count, serum albumin levels, BUN levels, and C-reactive protein levels. In addition, we assessed any discontinuation of oral intake in cases of recurrent aspiration after the initiation of oral intake during the hospitalization course, when even a single episode of discontinuation was considered as discontinuation of oral intake. We also assessed duration of hospitalization and in-hospital death.
Statistical analysis
According to the need for the discontinuation (temporary termination) of oral intake due to reaspiration during the hospitalization course, each subject was assigned to either a “no reaspiration of intake” or a “reaspiration of intake” group. T-tests were used to compare numerical variables, while chi-square tests were used to compare categorical variables. In addition, we performed multiple logistic regression analysis (simultaneous regression) using presence or absence of discontinuation of intake due to reaspiration following the initiation of oral intake as the dependent variable. Variables with P-values less than 0.05 and those that were previously reported to be associated with aspiration pneumonia were included in the multivariate analysis. We used IBM Statistical Package for the Social Sciences (SPSS) for Windows version 22.0 (IBM Inc., Armonk, NY, USA) for the analyses. P-values less than 0.05 were considered to be statistically significant.
Results
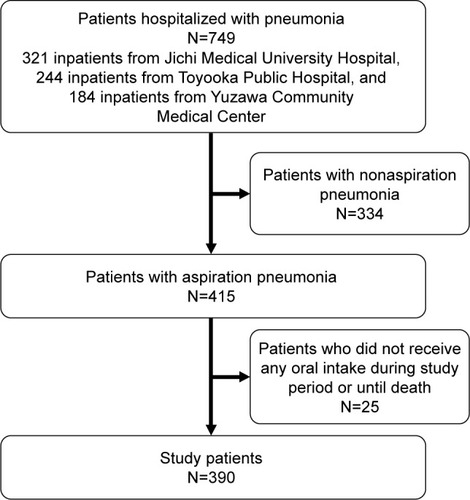
shows a flowchart of patient enrollment. Of a total of 749 inpatients with pneumonia, 415 were diagnosed with aspiration pneumonia. At Jichi Medical University Hospital, 151 of the 321 inpatients with pneumonia were diagnosed with aspiration pneumonia. At Toyooka Public Hospital, 111 of the 244 inpatients with pneumonia were diagnosed with aspiration pneumonia. At Yuzawa Community Medical Center, 130 of the 184 inpatients with pneumonia were diagnosed with aspiration pneumonia. Twenty-five patients who were unable to receive oral intake were excluded because they were discharged or died, and hence a total of 390 patients were included in this study (242 men and 148 women). The mean age of the patients was 79.3±13.1 years (range 22–102 years). Among the enrolled subjects, intake was discontinued in 80 patients owing to aspiration after the initiation of intake during the hospitalization course, and 42 patients died during the hospitalization course.
shows a comparison of several parameters between the groups with and without discontinuation of intake due to aspiration after the initiation of oral intake. These parameters include the period from admission to initiation of intake, the application of a swallowing function assessment, the duration of hospitalization, and the number of in-hospital deaths, among others.
Table 1 Comparisons of items at admission and during the hospital course between groups with and without discontinuation of intake due to reaspiration
Age, sex, PS score, and bacteremia rate did not differ significantly between the groups. However, a significant difference was observed for the following items: level of consciousness, respiratory rate, SpO2, CURB-65 score, extent of infiltration/opacity in more than two-thirds of the unilateral lung on chest radiography, white blood cell count, albumin levels, and BUN levels at admission, and the application of a swallowing function assessment. In the “reaspiration of intake” group, both the period from admission to intake and the duration of hospitalization were significantly longer in the “reaspiration of intake” group. In 19 of the 23 patients who died in the “reaspiration of intake” group, the cause of death was aspiration-related disease, whereas in the case of all patients who died in the “no reaspiration of intake” group, the cause of death was aspiration-related disease. In the “reaspiration of intake” group, only 36 of 80 patients were able to resume oral intake prior to discharge.
shows comparisons of several factors at the initiation of intake between the groups with and without the discontinuation of intake due to aspiration at the time of the initiation of oral intake. A significant difference in level of consciousness, pulse rate, and albumin levels was observed at the initiation of intake between the groups.
Table 2 Comparisons of items at the initiation of intake between the groups with and without discontinuation of intake due to reaspiration
The items found to be statistically significant from and were further analyzed using the multiple logistic regression analysis. For this analysis, the presence or absence of discontinuation of intake due to aspiration after the initiation of oral intake was the dependent variable (). Duration of hospitalization and in-hospital death rates were excluded as these were the outcomes. The odds ratios of the application of swallowing function assessment, level of consciousness at the initiation of intake, and extent of infiltration/opacity in more than two-thirds of the unilateral lung on chest radiography were 5.2, 3.2, and 2.3, respectively. Thus, these three items appear to be significant explanatory variables.
Table 3 Multiple logistic regression analysis results: the discontinuation of intake due to aspiration after the initiation of intake was used as the dependent variable
Discussion
In the present study, we investigated the factors involved in the discontinuation of oral intake in recurrent aspiration after the resumption of oral intake in hospitalized patients with aspiration pneumonia. Multiple logistic regression analysis indicated that the application of swallowing function assessment, a low level of consciousness at the initiation of intake, and extent of infiltration/opacity in more than two-thirds of the unilateral lung on chest radiography were significant predictors of discontinuation of oral intake.
Swallowing function is one of the criteria considered by physicians when resuming oral intake in aspiration pneumonia patients who have undergone short-term fasting.Citation13 In the present study, the discontinuation of intake due to aspiration after the initiation of oral intake was more frequent in cases where the swallowing function was assessed by speech therapists compared with cases where swallowing function was not assessed. The assessment of swallowing function has been shown to be useful to determine the resumption of oral intake after contracting respiratory disease or cerebrovascular disease;Citation6,Citation17,Citation18 hence, the application of swallowing function assessment is important. However, only one or two speech therapists were present at each of the participating hospitals for this study, and this number was not sufficient to effectively carry out the swallow function tests for all patients. Therefore, if the medical physician believed that the patient had normal swallowing function, then the swallowing function was not assessed by a speech therapist. In these cases, physicians relied on information from the patients’ families and on dysphagia screenings by nurses. However, if the medical physician suspected that a patient had poor swallowing function, then swallowing function was assessed by a speech therapist. To our knowledge, no study has indicated that patients who undergo a swallowing function test developed recurrent aspiration more frequently compared with patients who do not undergo a swallowing function test in aspiration pneumonia. All patients in the present study had developed aspiration pneumonia. In cases where swallowing function was measured, physicians could make an informed decision and were more likely to discontinue oral feeding. In contrast, in cases where swallowing function was not assessed, physicians relied on several judgments, including subjective assessments such as the opinion of the patient and family. Even if patients at high risk for aspiration passed the swallowing function test, they had a high likelihood of developing recurrent aspiration. If a medical physician believes that a patient with aspiration pneumonia has normal swallowing function or does not have a high risk for aspiration, then a swallowing function test may not be needed. In such cases, it is possible that patients can resume oral intake. Unfortunately, fluids related to clinical feeding exams might lead to higher false-negative and false-positive results. Fiberoptic endoscopic evaluation of swallowing is therefore a better diagnostic test for evaluating swallowing, but was performed in only some of the cases in this study.
One study reported that the ability of a patient to follow instructions at the resumption of oral intake is predictive of capacity for receiving oral intake after discharge.Citation16 Hence, the level of consciousness is an important factor for observing not only the severity, but also the progress, of pneumonia. Patients should reach a level of consciousness that allows them to follow the instructions of speech therapists or caretakers during meal assistance prior to the resumption of oral intake. The period from admission to intake and the duration of hospitalization were significantly longer, and the in-hospital death rate was significantly higher in the “reaspiration of intake” group compared with the “no reaspiration of intake” group. In fact, in 19 of the 23 patients who died in the “reaspiration of intake” group, the cause of death was aspiration-related disease, whereas in the case of all the patients who died in the “no reaspiration of intake” group the cause of death was aspiration-related disease. Moreover, in the “reaspiration of intake” group, 36 of 80 patients achieved total oral intake prior to discharge. We believe that the duration of hospitalization was longer in the “reaspiration of intake” group as a result of the need to rehabilitate swallowing function and to develop an established method for nutrient intake, such as oral feeding, tube feeding, or intravenous nutrition. The disturbance of consciousness of elderly patients with pneumonia is caused not only by the severity of the pneumonia but also by the severity of background dementia. In the present study, we did not distinguish between cases of severe dementia or other neurological disorders and cases of pneumonia as causes of consciousness disturbance. Nevertheless, consciousness disturbance caused by severe dementia or other neurological disorders would lead to a high risk for aspiration.Citation19
The guidelines for nursing- and health care-associated pneumoniaCitation5 and hospital-acquired pneumoniaCitation20 published by the Japanese Respiratory Society indicate that the extent of infiltration/opacity on chest radiography represents the severity of pneumonia. Moreover, the extent of infiltration/opacity on chest radiography may represent not only the spread of bacterial infection but also the degree and extent of aspiration. In addition, an infiltrative shadow may indicate the presence of complicated heart failure in aspiration pneumonia. Hence, the extent of infiltration/opacity on chest radiography should be carefully considered as a factor in recurrent aspiration after the resumption of oral intake and as a representation of the severity of aspiration pneumonia.
In the present study, several parameters were found to be significantly different between study groups following univariate analysis, but many of these were not significant variables when applying multiple logistic regression analysis. Certain guidelines indicate that the respiratory rate, SpO2, BUN levels, and age are indices for pneumonia severity.Citation5,Citation16 Furthermore, a previous studyCitation13 using questionnaires found that physicians consider several criteria when deciding whether to resume oral intake. These criteria included level of consciousness, SpO2, body temperature, swallowing function test results, and respiratory rate. However, we found that, of these items, only level of consciousness and swallowing function test results were involved in the discontinuation of oral intake in recurrent aspiration after the resumption of oral intake in hospitalized patients with aspiration pneumonia. The CURB-65 scoring method relies on BUN levels, respiratory rate, and age >65 years, all of which were not found to be significant factors. Hence, the CURB-65 score was not involved in the discontinuation of oral intake.
Limitations
The present study has several limitations. First, this study is retrospective in nature. In addition, in this analysis, the mean age of the subjects was 79.3±13.1 years, 65.6% of the subjects had a PS score of 3 or greater, and the mortality rate was 11.2%, which suggests that the subjects of this study were elderly with a low PS score and high mortality. Hence, the risk for recurrent aspiration would be expected to be high in our study population. We found that only the application of a swallowing function assessment, level of consciousness at the initiation of intake, and extent of infiltration/opacity on chest radiography were associated with recurrent aspiration after the resumption of oral intake. However, a group of patients with a lower risk for recurrent aspiration may exhibit other factors involved in recurrent aspiration.
Conclusion
This study showed that a low level of consciousness at the initiation of intake, extent of infiltration/opacity on chest radiography, and the application of a swallowing function assessment in patients suspected to have poor swallowing function by a medical physician are associated with the discontinuation of oral intake in recurrent aspiration after the resumption of oral intake. These factors may be helpful to determine a suitable timing for resumption of oral intake. Future prospective studies with a larger study population are needed to confirm our results.
Author contributions
TK conceived the study concept and design, analyzed and interpreted the data, and coordinated and drafted the manuscript. Taro T and MO conceived the study concept and design, drafted the manuscript, and corrected and restructured the manuscript. KK, Ayako K, YU, Takeshi T, YY, YH, and Akihito K participated in the recruitment of subjects and acquisition of data. All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Acknowledgments
This study was supported by a grant-in-aid for scientific research from the Japan Society for the Promotion of Science in Tokyo, Japan (grant number 25860507).
Supplementary materials
Table S1 CURB-65 score offers a simple clinical prediction rule based on the five clinical features of confusion, urea, respiratory rate, blood pressure, and age as a practical means of stratifying patients with community-acquired pneumonia into low, intermediate, and high mortality risk groups
Table S2 Risk of mortality at 30 days
Reference
- LimWSvan der EerdenMMLaingRDefining community acquired pneumonia severity on presentation to hospital: an international derivation and validation studyThorax20035837738212728155
Disclosure
The authors report no conflicts of interest in this work.
References
- Ministry of Health Labour Welfare: vital statistics 2015 Summary of Vital StatisticsTrends in leading causes of death Available from: http://www.mhlw.go.jp/english/database/db-hw/populate/index.htmlAccessed October 30, 2016
- World Health Organization (WHO)Disease and Injury Country EstimatesGenevaWHO2004 Available from: http://www.who.int/healthinfo/global_burden_disease/gbddeathdalycountryestimates2004.xlsAccessed October 30, 2016
- TeramotoSFukuchiYSasakiHSatoKSekizawaKMatsuseTJapanese Study Group on Aspiration Pulmonary DiseaseHigh incidence of aspiration pneumonia in community- and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in JapanJ Am Geriatr Soc20085657757918315680
- KomiyaKIshiiHUmekiKImpact of aspiration pneumonia in patients with community-acquired pneumonia and healthcare-associated pneumonia: a multicenter retrospective cohort studyRespirology20131851452123231701
- KohnoSImamuraYShindoYClinical practice guidelines for nursing- and healthcare-associated pneumonia (NHCAP) [complete translation]Respir Investig201351103126
- TeramotoSMatsuseTFukuchiYOuchiYSimple two-step swallowing provocation test for elderly patients with aspiration pneumoniaLancet19993531243
- YamayaMYanaiMOhruiTAraiHSasakiHInterventions to prevent pneumonia among older adultsJ Am Geriatr Soc200149859011207848
- YamamotoMEffectiveness of dysphagia therapy in patients with disuse syndrome, and factors influencing its effectivenessJpn J Logop Phoniatr200849713
- EbiharaTEbiharaSYamazakiMAsadaMYamandaSAraiHIntensive stepwise method for oral intake using a combination of transient receptor potential stimulation and olfactory stimulation inhibits the incidence of pneumonia in dysphagic older adultsJ Am Geriatr Soc20105819619820122066
- MaruyamaTTaguchiONiedermanMSEfficacy of 23-valent pneumococcal vaccine in preventing pneumonia and improving survival in nursing home residents: double blind, randomised and placebo controlled trialBMJ2010340c100420211953
- MomosakiRYasunagaHMatsuiHHoriguchiHFushimiKAboMPredictive factors for oral intake after aspiration pneumonia in older adultsGeriatr Gerontol Int20161655656025953259
- KenzakaTKosamiKMatsuokaYNodaAKumabeAThe difference between ideal and actual fasting duration in the treatment of patients with aspiration pneumonia: a nationwide survey of clinicians in JapanTohoku J Exp Med2016240322723327885198
- KenzakaTKumabeAKosamiKPhysicians’ opinions regarding the criteria for resuming oral intake after aspiration pneumonia: a questionnaire survey and cluster analysis of hospitals across JapanGeriatr Gerontol Int Epub5102016
- Japanese Respiratory SocietyAspiration pneumoniaRespirology200914S59S6419857224
- TeasdaleGJennettBAssessment of coma and impaired consciousness. A practical scaleLancet1974281844136544
- LimWSvan der EerdenMMLaingRDefining community acquired pneumonia severity on presentation to hospital: an international derivation and validation studyThorax20035837738212728155
- TakayanagiHEndoTNakayamaTKatoTDysphagia screening on resumption of oral intake in inpatients predictive factor for the resumption of oral intakeNihon Jibiinkoka Gakkai Kaiho2013116695702 Japanese23865295
- CraryMAMannGDGroherMEInitial psychometric assessment of a functional oral intake scale for dysphagia in stroke patientsArch Phys Med Rehabil2005861516152016084801
- MitchellSLTenoJMKielyDKThe clinical course of advanced dementiaN Engl J Med20093611529153819828530
- SekiMWatanabeAMikasaKKadotaJKohnoSRevision of the severity rating and classification of hospital-acquired pneumonia in the Japanese Respiratory Society guidelinesRespirology20081388088518657061