Abstract
Purpose
Macular hole (MH) is part of a group of age-related degenerative diseases characterized by pathology of vitreomacular interface. Similarly, neovascular age-related macular degeneration (nAMD) affects older patients and is a leading cause of irreversible visual loss. The purpose of this case series is to describe the development of full-thickness MH in patients with nAMD, following antivascular endothelial growth factor (anti-VEGF) treatment.
Methods
Participants in this case series were four patients with nAMD, who received anti-VEGF injections with variable therapeutic response to treatment. Patients were examined at baseline (when AMD was diagnosed) and monthly thereafter. The examination included visual acuity measurement, slit-lamp biomicroscopy, and optical coherence tomography.
Results
All patients were found to develop full-thickness MH within 1–4 months after the last anti-VEGF injection, even in the absence of pre-existing vitreomacular interface abnormalities in some cases. The median number of injections before the MH formation was 3.
Conclusion
MH formation may represent an adverse effect of anti-VEGF treatment in patients with nAMD and could be also coexisting pathology with nAMD in older individuals.
Introduction
Age-related macular degeneration (AMD) is the leading cause of irreversible visual loss in elderly population in the developed world and its prevalence increases with age, ranging from 0.2% (for people aged 55–64 years) to 13% (for those older than 85 years).Citation1–Citation3 Neovascular AMD (nAMD) can lead to visual impairment due to the development of choroidal neovascularization (CNV), and its prevalence is estimated to be 0.17%–5.8%.Citation1,Citation3 Vascular endothelial growth factor (VEGF) is the main angiogenic factor involved in the pathogenesis of nAMD.Citation4 Therefore, over the last two decades, intravitreal anti-VEGF agents are considered the standard of care in nAMD, aiming to block CNV activity and consequently prevent vision loss and improve vision in some cases.Citation5 Specifically, the two FDA-approved anti-VEGF agents for nAMD are ranibizumab (Lucentis®; Novartis, Basel, Switzerland), a recombinant antigen-binding fragment that neutralizes all isoforms of VEGF-A,Citation6 and aflibercept (Eylea; Bayer Healthcare, Berlin, Germany), which is a recombinant fusion protein consisting of human VEGF receptor extracellular domains from receptors 1 and 2 (VEGFR1 and VEGFR2) fused to the Fc domain of the human IgG backbone and also binded to all isomers of the VEGF-A family, VEGF-B, and placental growth factor.Citation7
A small number of ocular adverse events (<1%) have been reported after administration of anti-VEGF injections across large clinical trials, including endophthalmitis, rhegmatogenous retinal detachment, retinal tear, retinal pigment epithelium tear, traumatic cataract, vitreous hemorrhage, and uveitis.Citation5,Citation8 In addition, full-thickness macular hole (FTMH) formation following anti-VEGF treatment for nAMD has sparsely been reported in the literature, mainly as isolated case reports and mostly in the presence of vitreomacular traction disease.Citation9–Citation15 In light of the above, the purpose of this case series is to describe the development of FTMH in patients with nAMD, following anti-VEGF injections with variable therapeutic responses to treatment, even in the absence of pre-existing vitreomacular interface abnormalities.
Methods
Participants in this retrospective case series were four patients with nAMD, who developed FTMH after intravitreal anti-VEGF injections. Written informed consent was obtained by all participants for participation in this study and publication of the associated images. This study was in accordance with the Tenets of Helsinki Declaration and was approved by the Institutional Review Board of Korgialeneio Benakeio, Hellenic Red Cross Hospital, Athens, Greece. Exclusion criteria were any of the following: CMV of any cause except nAMD, previous FTMH, vitreomacular traction, uveitis, diabetic retinopathy, glaucoma, or retinal vein occlusion.
At baseline, all patients underwent best-corrected visual acuity (BCVA) measurement by means of Snellen charts, ophthalmic examination including slit-lamp biomicroscopy, and using optical coherence tomography (OCT). Time domain (Stratus 3000; Zeiss, Germany) or spectral domain OCT (Heidelberg Spectralis; Heidelberg Engineering, Heidelberg, Germany) were used. Fluorescein angiography (FA) was performed to confirm diagnosis and to exclude other causes of CNV.
All patients received at least one intravitreal injection of either 0.5 mg ranibizumab or 2.0 mg aflibercept. All the injections were performed under standard sterile conditions. Topical antibiotics were administered to all patients four times a day for 1 day before and for 5 days after the injection. Patients were examined monthly thereafter. At each visit, complete eye examination was performed, including BCVA measurement, fundoscopy, and OCT. FA was performed only at the examiner’s discretion and not at every postinjection evaluation.
Results
The patients’ characteristics are shown in . Of the four patients, two were males and two were females. The mean age of patients was 63.5±4.5 years. All patients presented active CNV with subretinal fluid and pigment epithelium detachment (PED). One patient had posterior vitreous detachment (PVD), and in three patients no PVD was present. Two patients had epiretinal membrane (ERM). At baseline, the mean BCVA was 0.4±0.16 decimal (about 6/12 Snellen). Three patients received ranibizumab and one aflibercept intravitreal injections. All patients developed FTMH about 1–4 months after the last intravitreal injection. Median number of intravitreal injection before developing FTMH was 3. The mean BCVA at the time of FTMH presence was counting fingers in all patients. and showed two indicative cases of our study and their progression over time. No other ocular side effects were found, such as endophthalmitis, inflammation, infection, increased intraocular pressure, retinal tear, or detachment.
Table 1 Demographic and clinical characteristics of our study sample
Figure 1 66-old-male patient with age-related macular degeneration, who developed full thickness macular hole after ranibizumab injections.
Notes: (A) Color fundus photo in a 66-year-old male patient, demonstrating a pigment epithelium detachment at the fovea surrounded by drusen and few retinal haemorrhages in his right eye; (B) early-phase and (C) late-phase fluorescein angiography of the same patient, showing an active choroidal neovascularization; (D) optical coherence tomography, showing subretinal fluid, pigment epithelium detachment, and retinal pigment epithelium changes, as well as disruption in ellipsoid zone; (E) optical coherence tomography after two ranibizumab injection, showing regression of subretinal fluid; (F) optical coherence tomography 2 months after the last ranibizumab injection, showing full-thickness macular hole; (G) optical coherence tomography 4 months later, showing the development of disciform scar underneath the macular hole, extending beyond the hole’s edges.
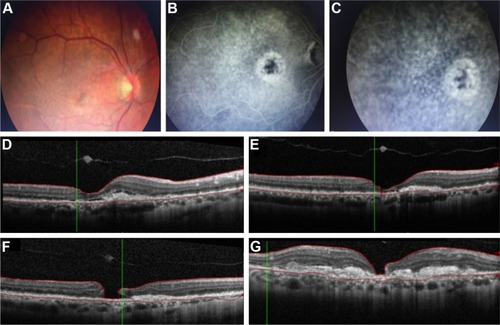
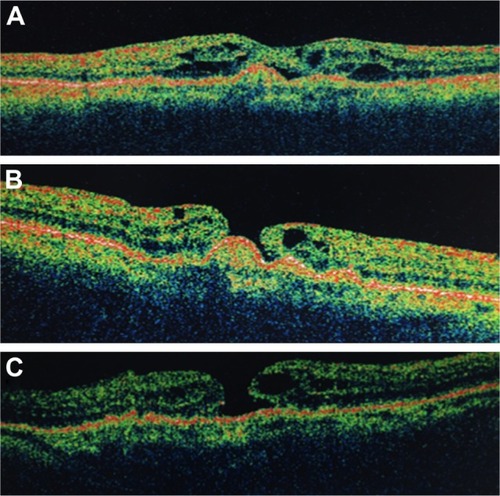
Figure 2 57-year-old female patient who developed full thickness macular hole after ranibizumab injections for age-related macular degeneration.
Discussion
According to a recent classification of the vitreoretinal interface disorders, FTMH is an anatomic defect in the fovea featuring interruption of all neural retinal layers from the internal limiting membrane to the retinal pigment epithelium.Citation16 GassCitation17 hypothesized that idiopathic FTMH formation occurred due to focal tangential traction on the fovea, following contraction of the prefoveal vitreous cortex. In addition, Gaudric et alCitation18 demonstrated with OCT that vitreous traction on the fovea may be oblique, whereas Tanner et alCitation19 suggested that initiation of MH formation may be attributed to an anteroposterior vitreofoveal traction documented by OCT imaging. Therefore, both tangential and oblique/anterior–posterior transvitreal traction have been implicated in the development of idiopathic FTMH.
The role of abnormal vitreomacular interface in AMD has previously been reported and vitreomacular adhesion, as well as vitreomacular traction has been implicated as potential risk factors for the development of exudative AMD.Citation20,Citation21 On the contrary, PVD seemed to have a prophylactic effect on AMD formation.Citation22 Furthermore, since currently anti-VEGF agents are the treatment of choice for nAMD, it has been reported that vitreoretinal traction, if present, could antagonize the effect of anti-VEGF treatment and cause pharmacological resistance in patients with nAMD.Citation23 However, anti-VEGF intravitreal injections can induce PVD in patients with nAMD. Specifically, it has been reported that 24% of patients receiving intravitreal injections for exudative maculopathies, such as nAMD, develop PVD over a mean 11.1-week follow-up period and PVD incidence correlates with increasing age.Citation24
FTMH formation following intravitreal anti-VEGF treatment for nAMD has been previously reported in the literature but was mainly based on isolated case reports.Citation9–Citation15 In all reported cases, vitreomacular interaction forces following intravitreal injections have been speculated to be closely linked to the formation of the MH. Several potential mechanisms have been implicated to explain this process. Induction of vitreous incarceration following anti-VEGF injections could enhance vitreoretinal traction and subsequently FTMH development.Citation13 Chemical compounds induced to the vitreous cavity and structural modification of vitreous body following anti-VEGF therapy could also lead to incomplete PVD, vitreomacular traction, and FTMH formation.Citation14,Citation15 Grigoropoulos et al hypothesized that intravitreal injections can increase the vitreomacular traction due to globe deformation during needle insertion and vitreous incarceration at the insertion site following treatment. This was proposed to cause vitreous syneresis and increase vitreofoveal traction leading to incomplete PVD and thus, resulting in focal sites of traction on the retinal surface and in FTMH formation.Citation25 Moreover, the anti-VEGF agent per se may have caused the MH by modulating the activity of the CNV and inducing contraction of the vascular membrane, leading to exacerbation of tangential traction on the overlying retina.Citation10
It has also been reported that the presence of PED in nAMD could be a predisposing factor for MH formation following anti-VEGF treatment. Changes in PED height and size, as a response to anti-VEGF treatment, could enhance the tractional forces exerted on the vitreoretinal interface leading to MH formation.Citation20 It is worthy to mention that all cases in our series had PED, but no retinal pigment epithelium tear developed following anti-VEGF treatment and prior to MH formation.
In our cases, two patients had only PED and the formation of FTMH in the absence of vitreoretinal interface abnormalities could be attributed to other predisposing factors, such as biochemical or cellular elements, rather than simple mechanical vitreofoveal traction, as previously reported. In the other two cases, a FTMH developed in the presence of a PED, which coexisted with ERM. In fact, a lamellar MH developed initially, which eventually led to a FTMH formation. Evolution of a lamellar MH to a FTMH could either be the natural course of the disease or could be attributed to the progression of nAMD, even in the absence of further anti-VEGF treatment.
Conclusion
Taking into account the prevalence of wet AMD as previously reported and the large number of patients treated with anti-VEGF injections, more attention should be paid on the possible changes of vitreomacular interface and PVD following anti-VEGF injections. If such a relationship exists, then there is a potential risk for MH formation following anti-VEGF treatment. If this risk does exist, it does not outweigh the well-established benefits of anti-VEGF therapy for nAMD. On the other hand, both FTMH and nAMD are age-related conditions with similar prevalence, which increases with age. Therefore, they may represent only coexisting pathologies in the older population and not an adverse effect to anti-VEGF treatment that eventually interact with each other.
Acknowledgments
This study was presented as a poster at the Controversies in Ophthalmology congress in March 2017, Lisbon.
Disclosure
The authors report no conflicts of interest in this work.
References
- KleinRPetoTBirdAVannewkirkMRThe epidemiology of age- related macular degenerationAm J Ophthalmol2004137348649515013873
- WongWLSuXLiXGlobal prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysisLancet Glob Health201422e106e11625104651
- SmithWAssinkJKleinRRisk factors for age-related macular degeneration: pooled findings from three continentsOphthalmology2001108469770411297486
- AdamisAPShimaDTThe role of vascular endothelial growth factor in ocular health and diseaseRetina200525211111815689799
- SolomonSDLindsleyKVedulaSSKrzystolikMGHawkinsBSAnti-vascular endothelial growth factor for neovascular age-related macular degenerationCochrane Database Syst Rev20148CD005139
- RosenfeldPJBrownDMHeierJSRanibizumab for neovascular age-related macular degenerationN Engl J Med2006355141419143117021318
- HeierJSBrownDMChongVVIEW 1 and VIEW 2 Study GroupsIntravitreal aflibercept (VEGF trap-eye) in wet age-related macular degenerationOphthalmology2012119122537254823084240
- DaySAcquahKMruthyunjayaPGrossmanDSLeePPSloanFAOcular complications after anti-vascular endothelial growth factor therapy in Medicare patients with age-related macular degenerationAm J Ophthalmol2011152226627221664593
- OshimaYApteRSNakaoSYoshidaSIshibashiTFull thickness macular hole case after intravitreal aflibercept treatmentBMC Ophthalmol2015153025881212
- MukherjeeCMitraAKumarNAElsherbinySLipPLMacular hole formation after intravitreal ranibizumab injection in wet age-related macular degenerationOpen Ophthalmol J2015917718026962382
- RegatieriCVDukerJSBilateral macular hole after anti-vascular endothelial growth factor therapy in a patient with exudative age-related macular degenerationRetin Cases Brief Rep20126112512825390731
- ClemensCRHolzFGMeyerCHMacular hole formation in the presence of a pigment epithelial detachment after three consecutive intravitreal antivascular endothelial growth factor injectionsJ Ocul Pharmacol Ther201026329729920565318
- QuerquesGSouiedEHSoubraneGMacular hole following intravitreal ranibizumab injection for choroidal neovascular membrane caused by age-related macular degenerationActa Ophthalmol2009872235237
- MoisseievEGoldsteinMLoewensteinAMoisseievJMacular hole following intravitreal bevacizumab injection in choroidal neovascularization caused by age-related macular degenerationCase Rep Ophthalmol201011364121369348
- RaijiVREliottDSaddaSRMacular hole overlying pigment epithelial detachment after intravitreal injection with ranibizumabRetin Cases Brief Rep201371919425390533
- DukerJSKaiserPKBinderSThe International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular holeOphthalmology2013120122611261924053995
- GassJDIdiopathic senile macular holes: its early stages and pathogenesisRetina2003236 Suppl629639
- GaudricAHaouchineBMassinPPaquesMBlainPErginayAMacular hole formation: new data provided by optical coherence tomographyArch Ophthalmol1999117674475110369584
- TannerVChauhanDSJacksonTLWilliamsonTHOptical coherence tomography of the vitreoretinal interface in macular hole formationBr J Ophthalmol20018591092109711520763
- MojanaFChengLBartschDUThe role of abnormal vitreomacular adhesion in age-related macular degeneration: spectral optical coherence tomography and surgical resultsAm J Ophthalmol2008146221822718538742
- SchulzeSHoerleSMennelSKrollPVitreomacular traction and exudative age-related macular degenerationActa Ophthalmol200886547048118537930
- KrebsIBrannathWGlittenbergCZeilerFSebagJBinderSPosterior vitreomacular adhesion: a potential risk factor for exudative age-related macular degeneration?Am J Ophthalmol2007144574174617884003
- VelosoCEKanadaniTMPereiraFBNehemyMBVitreomacular interface after anti-vascular endothelial growth factor injections in neovascular age-related macular degenerationOphthalmology201512281569157226038338
- GeckUPustollaNBarakiHAtiliAFeltgenNHoeraufHPosterior vitreous detachment following intravitreal drug injectionGraefes Arch Clin Exp Ophthalmol201325171691169523381655
- GrigoropoulosVEmfietzoglouJNikolaidisPTheodossiadisGTheodossiadisPFull-thickness macular hole after intravitreal injection of ranibizumab in a patient with retinal pigment epithelium detachment and tearEur J Ophthalmol201020246947220037902
