Abstract
Purpose
Dislocation is an important complication that increases the mortality, morbidity, and postoperative care following bipolar hemiarthroplasty. It is thought that the transtrochanteric approach that enables access to the femoral neck directly from the fracture line at the coronal plane of the greater trochanter without opening the posterior and anterior capsules could reduce the risk of dislocation. Additionally, it is argued that preservation of the external rotators could also be advantageous for patient rehabilitation and muscle strength. The aim of this study is to compare the effectiveness of the standard posterolateral approach and transtrochanteric approach performed from the fracture line, primarily the rate of dislocation, in osteoporotic Evans Type IV–V unstable intertrochanteric fractures on which bipolar hemiarthroplasty was performed.
Patients and method
One hundred and twelve patients had Type IV–V fracture according to Evans classification and underwent hemiarthroplasty were enrolled in the study. Patients operated using the posterolateral approach, that is, Group 1 (n=48), and patients operated using the transtrochanteric (transfracture) approach, that is, Group 2 (n=64), were compared in terms of dislocation, surgical duration, amount of blood transfusion, infection, mortality, and trochanteric nonunion. Factors that could affect the development of dislocation from the patient, surgery, and implant were also analyzed.
Results
It was found that the rate of dislocation was statistically significantly higher in Group 1 in comparison to Group 2 (P<0.05). It was also observed that the surgical duration was statistically significantly shorter in Group 2 (P<0.05). It was found that the presence of a cognitive disorder, trochanteric nonunion, and use of posterolateral surgical approach resulted in a statistically significant increase in the rate of dislocation (P<0.05).
Conclusion
Transtrochanteric (transfracture) approach is an effective method for minimizing possible complications following hemiarthroplasty, especially dislocation.
Introduction
Pertrochanteric fracture is an important entity that causes high mortality and morbidity, with the 1-year mortality rate being 30% in elderly individuals.Citation1–Citation3 These fractures constitute 45% of all hip fractures.Citation1,Citation4
Although the accepted primary treatment for stable hip fractures is osteosynthesis, one-third of the fractures in this region are constituted by unstable fractures.Citation1,Citation5 Internal fixation methods are associated with high complication rates in the elderly patient population, especially in case of unstable fractures.Citation6–Citation8 The observed complications and long-term bed rest that may be necessary following internal fixation further increase the risk of deep vein thrombosis, which is already high, and the complications associated with it.Citation9 In the light of this information, bipolar hemiarthroplasty can be the preferred primary treatment option for osteoporotic unstable hip fractures (Evans Types IV and V) in elderly patients.
One of the most common complications that increase mortality following bipolar hemiarthroplasty in elderly patients is dislocation.Citation10 Various studies have reported dislocation rates ranging from 1% to 22%.Citation11 It is asserted in many studies that the rate of dislocation is associated with the employed surgical approach. It is argued that the rate of dislocation is higher in the classical posterolateral approach in which the posterior capsule and external rotators are incised at the hip joint that tends to exhibit posterior dislocation. It was also demonstrated that the dislocation risk could be decreased by repairing posterior structures.Citation12,Citation13
In 2008, Bombaci defined the transtrochanteric approach that enables access to the femoral neck directly from the fracture line at the coronal plane of the greater trochanter without opening the posterior and anterior capsules.Citation14 In this approach, the operation is distant from the sciatic nerve, which is at risk in the posterior approach, and it is thought that the risk of dislocation could be theoretically reduced as the capsules and external rotators are preserved as compared to the classical posterior approach. Additionally, it is argued that preservation of the external rotators could also provide advantage for patient rehabilitation and muscle strength. However, there are no comparative studies on this subject in the literature.
In this study, our aim was to compare the effectiveness of the standard posterolateral approach with that of the transtrochanteric approach performed from the fracture line, and primarily the rate of dislocation, in osteoporotic Evans Type IV–V unstable intertrochanteric fractures on which bipolar hemiarthroplasty was performed.
Patients and methods
This retrospective comparative study was approved by the Institutional Review Board (IRB) of our hospital (Yenimahalle Hospital IRB no: 2018/60). Since the study was retrospective, informed consent by patients and providers was not required. The collection of medical records complies with patient data confidentiality and the Declaration of Helsinki. Two hundred sixty-four hip fractures operated between 2014 and 2017 at our clinic were retrospectively screened in this study. Among these fractures, 112 patients who had Type IV–V fractures according to Evans classification and underwent hemiarthroplasty were enrolled in the study. Patients operated in our clinic using the classical posterolateral approach before June 2015 constituted Group 1 (n=48), and those operated in our clinic using the transtrochanteric (transfracture) approach that was included in practice after June 2015 constituted Group 2 (n=64). All surgeries were performed by two surgeons with equal experience and seniority. Among the patients included in the study, 72 were implanted using cemented bipolar hemiarthroplasty purchased from Bi-Metric stem (Biomet, Sylvania, OH, USA), whereas 40 patients were implanted using uncemented modular bipolar hemiarthroplasty after evaluation according to patients’ cortical index (T2 Hip Prosthesis; Tipsan, Bornova/İzmir, Turkey). Mean age of the patients in groups 1 and 2 was 86.5±6.5 and 87.1±5.7 years, respectively. Thirty-one (64.6%) patients in Group 1 and 47 (73.4%) patients in Group 2 were female. Demographic characteristics and morbidities of patients, such as body mass index, status according to American Society of Anesthesiologists (ASA) classification, and presence of a cognitive disorder diagnosed by a neurologist at preoperative evaluation or obtained from patient records, as well as the distribution thereof by groups are provided in .
Table 1 Distribution of the demographic and clinical characteristics of the patients included in the study by groups and statistical analysis of the differences between the two groups
Patient records of the subjects who participated in the study were reviewed, and postoperative amount of blood transfusion, surgical duration, early mortalities, and time from admission to the hospital until surgery were recorded. Patient follow-up records were reviewed in order to investigate and analyze the complications such as mortality, infection, and dislocation for comparison between the two groups. Rate of dislocation was compared between the two groups, in addition to the analysis of factors such as bipolar head size that could affect dislocation.
Patients who were given an ASA score of 4 by the anesthesiology clinic, patients with pathologic fractures or multiple trauma, patients diagnosed with advanced Alzheimer’s disease, patients with inadequate outpatient follow-up, non-compliant patients, and patients with noncompliant relatives were not included in any group of this study.
Surgical technique
Posterolateral approach
Patients included in Group 1 were placed in the lateral decubitus position. Following a posterolateral skin incision and moving past the tensor fascia lata, the gluteus maximus was split along its proximal fibers. Then, the external rotators were separated at the point of attachment to the trochanter moving along the posterior aspect of the joint and a T-shaped incision was made on the capsule in order to excise the fractured femoral head. Following femur preparation in internal rotation, femoral stem was placed cemented or uncemented depending on the technique. Fixation of the fractured fragment in the greater trochanter was performed using trochanteric grip and cable. External rotators and capsule were sutured back to the trochanter and repaired.
Transtrochanteric (transfracture) approach
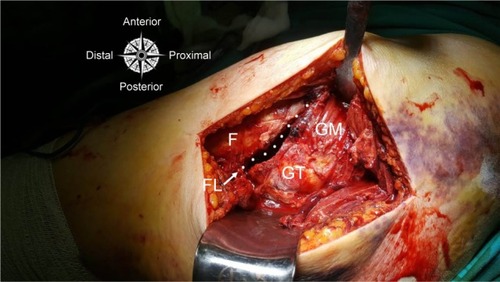
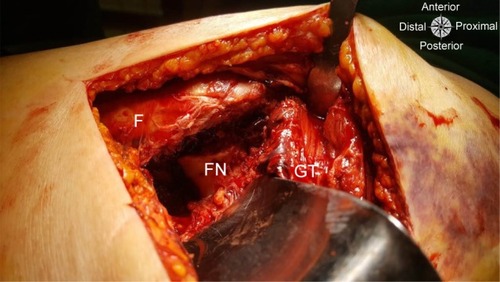
Patients included in Group 2 were subjected to the same stages with a posterolateral skin incision. Then, the fracture line at the coronal plane of the trochanter was split in order to expose the femoral neck without moving past the external rotators and capsule ( and ). The femoral head was excised with a superior incision of 1–2 cm. The same method was used for femoral stem implantation and fixation of the trochanter fracture.
Statistical analysis
SPSS 17.0 software package was used for the statistical analysis of data. Categorical measurements were given as numbers and percentage values, whereas continuous measurements were given as mean and SD values (median and minimum–maximum when necessary). Chi-squared test or Fisher’s test was used for comparing the categorical variables. Distributions were analyzed on comparing continuous variables between the groups, wherein Student’s t-test was used for variables that had a parametric distribution and Mann–Whitney U test for variables that did not have a parametric distribution. Independent risk factors that affect the formation of dislocation were determined using logistic regression analysis. Statistical significance level was accepted as 0.05 for all tests.
Results
According to the statistical comparison of the groups, it was found that the rate of dislocation was statistically significantly higher in Group 1 compared to Group 2 (P<0.05). Comparison of all the studied parameters is provided in detail in . Comparison of the patients in groups 1 and 2 in terms of demographic and clinical characteristics revealed that the only nonhomogenous distribution resulted in a statistical difference (P<0.05) in terms of the follow-up period (from the date of surgery to the date of collection of data for the study), as shown in .
Table 2 Comparison of the two surgical techniques
Analysis of other factors that could affect the formation of dislocation is provided in . It was found that the presence of a cognitive disorder, trochanteric nonunion, and use of posterolateral surgical approach resulted in a statistically significant increase in the rate of dislocation (P<0.05). No statistically significant difference was found related to fixation method (Bi-Metric cemented prosthesis vs T2 uncemented prosthesis) in terms of dislocation rate (P=0.743). Independent risk factors that could affect the formation of dislocation were investigated using logistic regression analysis (). Parameters that showed significant results in the univariate analysis were added to the model. Independent risk factors that affect the formation of dislocation in a patient were identified. It was found that the presence of a cognitive disorder, trochanteric nonunion, and use of posterolateral surgical approach increased the risk of developing dislocation in a patient (P<0.05).
Table 4 Logistic regression analysis
Table 3 Analysis of other factors that affect the formation of dislocation
Discussion
This study has shown that the transtrochanteric approach that could be performed from the fracture line at the trochanter without incision of the external rotators and capsule in osteoporotic Evans IV–V fractures in elderly patients was more effective in preventing dislocation, which is an important problem that increases morbidity in bipolar hemiarthroplasty, in comparison to the standard posterior approach. Analysis concerning incidence of dislocations revealed that the difference between the two groups was statistically significant (P<0.05).
This approach enables reducing the risk of dislocation as well as decreasing the amount of bleeding since external rotators and capsule are not incised. Although the mean amount of blood transfusion for patients in Group 2 after the operation was lower in comparison to the standard posterolateral approach, the difference between the two approaches was not statistically significant. Moreover, the surgery is performed at a distance from the sciatic nerve, which is under risk in the posterior approach. Another potential advantage of this approach is that concerning nonunion, which is a significant problem in the fixation of the trochanter; a better union can be provided without disrupting the vascular support of the fragment since posterior vascular structures are preserved. It is thought that preservation of the external rotators could also be advantageous for patient rehabilitation and muscle strength.
According to the literature, apart from the surgical approach, there are many factors (time to surgery, gender, mental status of the patient, fixation method, etc) that have an impact on the risk of dislocation following bipolar hemiarthroplasty.Citation15–Citation23 The relationship between fixation method, bipolar head size, mental status of the patients, gender, time until surgery, and dislocation was also analyzed irrespective of the surgical approach. Many studies have reported that there is no difference between the fixation methods (cemented vs uncemented) in terms of dislocation.Citation16–Citation18 The results of this study were similar to the data in the literature in that there was no statistically significant difference between cemented and uncemented fixation in terms of dislocation (P=0.743). It is argued that using larger femoral head significantly reduces the risk of dislocation in total hip arthroplasty.Citation19 Although theoretically a lower rate of dislocation is expected as the “jumping distance” would increase when using large bipolar heads, the number of comparative studies on this subject is very limited. However, it is asserted that the use of smaller heads as a result of a faulty measurement of the excised head size could be associated with early acetabular degradation and protrusion. In our study, there was no statistically significant difference in terms of the head size used in patients who experienced and did not experience dislocation (P=0.978). However, it would be more meaningful to evaluate these patients by measuring the excised head or conducting contralateral measurements. Madanat et alCitation20 and Salem et alCitation21 have shown in their studies that there was a direct correlation between time from admission to the hospital until surgery and dislocation. These studies reported that exceeding 24 and 48 hours could increase the risk of dislocation. In our study, there was no relationship between increase in this time period and the rate of dislocation (P=0.320). However, it was understood that among the patients operated at our clinic, the number of those operated within 48 hours upon admission to the hospital was very low.
It was demonstrated that factors related to the patient, such as cognitive status and gender, had an effect on the rate of dislocation. In a study by Abram and Murray, it was found that the rate of dislocation was higher in females and patients with a cognitive disorder; however, the difference was not statistically significant.Citation22 Ninh et al showed that there was a strong correlation between dislocation and the mental status of patients.Citation23 The same study also revealed that male gender had a higher risk of dislocation. In our study, it was found that the rate of dislocation was statistically significantly higher in patients with a cognitive disorder (P<0.05). The number of patients diagnosed with Parkinson’s disease was not sufficient to conduct a statistical analysis. No difference was found in the statistical analysis in terms of gender (P=0.733).
It is observed that dislocation generally develops within the first year, as indicated in the literature. However, the weakness of this study in terms of investigating long-term complications was that the mean follow-up periods were different between the two groups. Another weakness of this study was that measurement was not possible from the obtained radiographs to analyze the patient-related factors that could affect the development of dislocation, such as acetabular coverage and offset, and therefore it was not included in the study. Another limitation of this study is that the study design is retrospective. There is a need for prospective randomized comparative studies comparing hip approaches. The fact that it is the first study to compare quite a new approach that can be used in the prevention of dislocation, which is a significant problem in elderly individuals, with a standard approach and investigate the other factors that may affect dislocation can be considered as the strength of this study.
There are many studies investigating the effect of surgical approach on the rate of dislocation following hemiarthroplasty. According to an extensive meta-analysis and registry data, it is asserted that the rate of dislocation is higher in the posterior approach as compared to the anterolateral approach.Citation24,Citation25 Transtrochanteric approach in primary total hip arthroplasty was first described by Charnley,Citation26 followed by the description of Bombaci for the first time in hemiarthroplasty for intertrochanteric fractures involving access from the trochanteric fracture line.Citation14 Limited case series have shown that successful outcomes could be achieved by using this new approach in fractures of the hip area.Citation27,Citation28 However, there are no comparative and detailed studies concerning this approach. This study has shown that the rate of dislocation in transtrochanteric approach performed from the fracture line was lower in comparison to the standard posterior approach, wherein factors that could affect the rate of dislocation were also analyzed.
Conclusion
The use of transtrochanteric (transfracture) surgical approach performed from the fracture line by preserving anterior and posterior structures in suitable patients is effective in minimizing possible complications following hemiarthroplasty, especially dislocation.
Disclosure
The authors report no conflicts of interest in this work.
References
- HassankhaniEGOmidi-KashaniFHajitaghiHHassankhaniGGHow to treat the complex unstable intertrochanteric fractures in elderly patients? DHS or arthroplastyArch Bone Jt Surg20142317417925386578
- AbrahamsenBvan StaaTArielyROlsonMCooperCExcess mortality following hip fracture: a systematic epidemiological reviewOsteoporos Int200920101633165019421703
- PanulaJPihlajamäkiHMattilaVMMortality and cause of death in hip fracture patients aged 65 or older: a population-based studyBMC Musculoskelet Disord201112110521599967
- AbdelkhalekMAliAMAbdelwahabMCemented bipolar hemiarthroplasty with a cerclage cable technique for unstable intertrochanteric hip fractures in elderly patientsEur J Orthop Surg Traumatol201323444344823412149
- GrimsrudCMonzonRJRichmanJRiesMDCemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fracturesJ Arthroplasty200520333734315809952
- MaindsCCNewmanRJImplant failures in patients with proximal fractures of the femur treated with a sliding screw deviceInjury1989202981002592088
- BarriosCBroströmLAStarkAWalheimGHealing complications after internal fixation of trochanteric hip fractures: the prognostic value of osteoporosisJ Orthop Trauma1993754384428229380
- SheikhISIntertrochanteric femur fracture in elderly treated with bipolar vs DHS – a prospective studyJournal of Medical Thesis2014224549
- RaePJHodgkinsonJPMeadowsTHDaviesDRHargadonEJTreatment of displaced subcapital fractures with the Charnley–Hastings hemiarthroplastyJ Bone Joint Surg Br198971-B3478482
- PetersenMBJørgensenHLHansenKDuusBRFactors affecting postoperative mortality of patients with displaced femoral neck fractureInjury200637870571116765352
- BhandariMDevereauxPJSwiontkowskiMFInternal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysisJ Bone Joint Surg Am200385-A91673168112954824
- KoCKLawSWChiuKHEnhanced soft tissue repair using locking loop stitch after posterior approach for hip hemiarthroplastyJ Arthroplasty200116220721111222895
- MacaulayWColacchioNDFinkLAModified enhanced posterior soft tissue repair results in a negligible dislocation rate after hip resurfacingOper Tech Orthop2009193163168
- BombaciHTranstrochanteric approach in intertrochanteric femur fracturesJ Trauma20086551171117318753984
- JonesCBriffaNJacobJHargroveRThe dislocated hip hemiarthroplasty: current concepts of etiological factors and managementOpen Orthop J201711Suppl–7, M41200121229290857
- LangsletEFrihagenFOplandVMadsenJENordslettenLFigvedWCemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trialClin Orthop Relat Res201447241291129924081667
- DeangelisJPAdemiAStaffILewisCGCemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-upJ Orthop Trauma201226313514022198652
- FigvedWOplandVFrihagenFJervidaloTMadsenJENordslettenLCemented versus uncemented hemiarthroplasty for displaced femoral neck fracturesClin Orthop Relat Res200946792426243519130162
- HowieDWHolubowyczOTMiddletonRLarge Articulation Study GroupLarge femoral heads decrease the incidence of dislocation after total hip arthroplasty: a randomized controlled trialJ Bone Joint Surg Am201294121095110222717828
- MadanatRMäkinenTJOvaskaMTSoivaMVahlbergTHaapalaJDislocation of hip hemiarthroplasty following posterolateral surgical approach: a nested case–control studyInt Orthop201236593594021931967
- SalemKMIShannakOAScammellBEMoranCGPredictors and outcomes of treatment in hip hemiarthroplasty dislocationAnn R Coll Surg Engl201496644645125198977
- AbramSGMurrayJBOutcomes of 807 Thompson hip hemiarthroplasty procedures and the effect of surgical approach on dislocation ratesInjury20154661013101725704140
- NinhCCSethiAHatahetMLesCMorandiMVaidyaRHip dislocation after modular unipolar hemiarthroplastyJ Arthroplasty200924576877418555648
- VarleyJParkerMJStability of hip hemiarthroplastiesInt Orthop200428527427715316673
- RogmarkCFenstadAMLeonardssonOPosterior approach and uncemented stems increases the risk of reoperation after hemiarthroplasties in elderly hip fracture patientsActa Orthop2014851182524460108
- CharnleyJLow Friction Arthroplasty of the Hip Theory and PracticeBerlin, Heidelberg, New YorkSpringer1979
- PatilARole of cemented bipolar hemiarthroplasty for comminuted inter-trochanteric femur fracture in elderly osteoporotic patients through a modified transtrochanteric approach – “SION Hospital Modification”IOSR-JDMS2013944047
- PradeepCAnujAAbhishekGTreatment of comminuted unstable inter-trochanteric fracture in elderly patients with cemented bipolar prosthesisIndian J Orthop Surg201514255260