Abstract
Maintaining or improving quality of life (QoL) is a key outcome of clinical interventions in older people. Fear of falling (FoF) is associated with activity restriction as well as with poorer physical and cognitive functions and may be an important contributor to a diminished QoL. The objectives of this systematic review were to determine i) the effect of FoF on QoL in older people, ii) whether the association between these two constructs depends on the use of specific conceptualizations and measurement instruments, and iii) the role of fall events as mediating factor in this relationship. Four electronic databases (PubMed, EMBASE, CINAHL, and Cochrane Library) were searched from their inceptions to February 2018. Thirty mostly cross-sectional studies in nearly 30.000 people (weighted mean age 75.6 years (SD =6.1); 73% women) were included. FoF was associated with QoL in most studies, and this association appeared to be independent of the conceptualization of FoF. Moreover, this relationship was independent of falls people experienced which seemed to have a lower impact. FoF should be considered not only as by-product of falls and targeted interventions in parts different from those to reduce falls are likely required. Studies are needed showing that reducing FoF will lead to increased QoL.
Introduction
Falls in older adults are frequent events with severe consequences for the individual and high associated costs for the health care systems. Apart from physical injury, such as bone fractures and traumatic brain injuries, psychological consequences such as fear associated with falls might be just as detrimental for the individual in the long term. Together they may lead to disability, need for care, and loss of independence, greatly affecting one’s quality of life (QoL). A great variability in the prevalence of fear of falling (FoF) has been reported, ranging from 3% to as high as 92% of the community-dwelling elderly fallers.Citation1,Citation2 First reported as fear-related “post-fall syndrome” affecting about one-third of older people admitted to hospital after a fall,Citation3 today, this fear is no longer considered a “post-fall syndrome”. It has been shown that in more than 50% of the people with no prior fall experience, FoF exists.Citation2,Citation4–Citation7 Conceptually, there are two different approaches to define and operationalize FoF. First, there is the definition focusing on the fear itself by measuring the fearful anticipation of future falls, for instance by using one-item questions (“At the present time, are you very fearful, somewhat fearful, or not fearful that you may fall?”). The second definition relates to Bandura’s theory of self-efficacyCitation8 and measures the construct of fall-related efficacy, which is the (loss of) confidence in one’s abilities during certain tasks of daily life. Examples for instruments to assess fall-related efficacy are the Fall-Efficacy Scale (FES) by TinettiCitation9 and the Activities-specific Balance Confidence Scale by Powell & Myers.Citation10 FoF is associated with poorer performance in physical, mobility, and cognitive tests.Citation11,Citation12 One major consequence of this fear is the subsequent restriction of activities leading into a downward spiral of inactivity, deconditioning, loss of confidence, and further increased fall risk.Citation13,Citation14 Hence, it is not surprising that FoF has been found to be associated with frailty in older adults.Citation15 The restriction of activities caused by fear-avoidance behavior also affects participation in social activities, a factor underlying reduced QoL.Citation16,Citation17
Quality of life is a broad, subjective, and complex construct that depends on cultural and social circumstances. Gerok and Brandstädter describe QoL and a long life without severe functional limitations as the key components of successful aging.Citation18 Changes in physical, mental, and functional dimensions during the aging process caused by illness, multimorbidity, and cognitive impairments affect QoL as do significant life transitions, such as retirement and the loss of important life partners.Citation19 Thus, the construct of QoL consists of physical, social, and emotional dimensionsCitation19,Citation20 and includes the satisfaction of basic needs as well as the sensation of happiness and fulfillment.Citation21 Strongly related to the construct of QoL and mostly used in research is the construct of health-related quality of life (HRQoL). As for QoL, there is no universal definition of HRQoL.Citation22 Similarly to QoL, it is a multidimensional concept that focuses on the impact health has on QoL, based on the individual’s perception of well-being and functioning.Citation20,Citation22–Citation24 In this article, we will refer to both concepts as QoL.
According to the World Health Organization, in addition to an increased lifespan, the main goal of health care is to ensure “adding life to years”Citation25 in recognition of the significance of high QoL for people. Although underlying medical conditions and functional performance need to be targeted, patient-reported outcomes, such as QoL are more and more important in health care systems that move beyond survival.Citation26 Thus, in older people with multiple chronic conditions and functional limitations, main aim should be maintaining or improving QoL.Citation27,Citation28 The demographics worldwide are changing rapidly toward aging societies. Therefore, the problem of FoF and falls and their impact on QoL is going to increase. However, to our knowledge, there has been no systematic analysis of the influence of FoF on QoL, including the clinically relevant issues addressed above (conceptualizations and measurement instruments for FoF/QoL and the mediating effect of actual fall events). We, therefore, conducted a systematic literature review to determine the impact of FoF on QoL. Specifically, we attempted to answer the following questions: 1) What is the effect of FoF on QoL? 2) Does the association depend on the operationalization of FoF or QoL? 3) Is there a mediating effect of falls on the effect of FoF on QoL?
Methods
Literature search strategy
Four electronic databases (PubMed, EMBASE, CINAHL, Cochrane Library) were searched for articles published from their inceptions to 12th of February 2018, with an initial search on 21 May 2015 and an update in February 2018. We applied a combined search of Medical Subject Headings (MeSH) and keywords related to fear (“fear of falling”, anxiety, “self-efficacy”, “self efficacy”, “self confidence”, “falls-efficacy”, “falls efficacy”, “balance confidence”, “fall-related efficacy”, “activity restriction”), older age (Aged, “older adults”, “older persons”, elderly, senior*), and QoL (“quality of life”, QoL, HRQoL, “well-being”). If possible (PubMed, EMBASE, CINAHL), the search was limited to English language only. The Cochrane database was limited to “Trials”. PubMed and CINAHL searches were further specified by excluding articles with diseases/medical conditions specified in the title (eg, Parkinson’s Disease, stroke) and those that stated “review” or “randomized controlled” in the title field. Reference lists of included studies and review articles were also searched for relevant articles.
Eligibility criteria
Articles were included when they reported on studies fulfilling the following criteria: i) cohort, cross-sectional (including baseline data from intervention studies) or case–control study design; ii) minumum age of participants 60 years or mean age 65 years and older; iii) included measures of FoF and QoL which were put into relation to each other. Studies were excluded if they investigated disease-specific populations and were not published peer-reviewed articles (no abstracts or theses) in languages other than English.
Screening process, data extraction, and risk assessment
In a first step, the initial screening of titles and abstracts was performed. Subsequently, the assessment for eligibility of retrieved full texts was conducted. A standardized, pre-piloted form was used to extract data from included studies. Extracted information included: study design; sample size; sample characteristics (age, gender, ethnicity, setting, health (conditions, co-morbidity, medications), falls, use of walking aids); instrument for assessing FoF; instrument for assessing QoL; prevalence/incidence of FoF; association between FoF and QoL. The ‘Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies’ was used to critically appraise the risk of bias of included studies.Citation29 Fourteen items were rated as ‘yes’, ‘no’, or 'other' (cannot be determined, not applicable, not reported) with no use of an overall score. All above-mentioned processes were done independently by two reviewers. Any disagreement was solved through discussion with a third reviewer.
Due to the large heterogeneity of instruments used for both constructs and differences in investigated populations we refrained from performing meta-analysis.
Results
Description of included studies
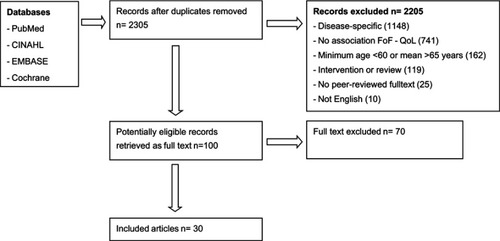
Thirty articles were included in this systematic review. describes the process of identification of included studies. A variety of study designs were applied, including cross-sectional studies, cohort studies, and pre-post group design studies. However, for the purpose of this review, all but one studyCitation30 used a cross-sectional design. Overall, 29,029 individuals were included with sample sizes ranging widely between 32Citation31 and 11,802 participants.Citation32
Figure 1 Flowchart of study selection process.
displays the characteristics of included studies. Most participants resided in the community. Exceptions were few studies recruiting participants from nursing homes,Citation33–Citation35 retirement villages/senior housing,Citation4,Citation36 emergency department,Citation37 and day services.Citation38
Table 1 Sample sizes, age ranges, mean age (standard deviations), population characteristics, measurements, and main results of fear of falling and quality of life of the included studies
Apart from one study that included people from 58 to 96 years (mean age 78),Citation39 all studies had participants’ minimum ages of 60 years. Thirteen publications included only participants of 65 years and olderCitation15,Citation30,Citation31,Citation37,Citation40–Citation48 and 6 studies only adults above 70 years.Citation32,Citation33,Citation35,Citation49–Citation51 Overall, the weighted mean age of 25 studies reporting on this outcome was 75.6 years (SD =6.1 (22 studies)).
The overall weighed proportion of women was 73%, ranging from 40% to 84%. Four studies exclusively recruited women.Citation30,Citation32,Citation35,Citation50
Study populations consisted of numerous cultures from all inhabited continents and 16 countries, ie, Nigeria,Citation40 Brasil,Citation48 Canada,Citation30,Citation36 USA,Citation4,Citation15,Citation39,Citation49,Citation52 China/HK,Citation34,Citation47 Iran,Citation53 Japan,Citation35,Citation38 Taiwan,Citation41–Citation44,Citation46 Thailand,Citation54 Vietnam,Citation55 New Zealand/Australia,Citation51 Finland,Citation50 Germany,Citation33,Citation43 Greece,Citation56 Turkey,Citation31,Citation37 and UK.Citation32,Citation45,Citation57
Health status of participants differed significantly across studies, from healthy to functionally impaired and frail covering a wide spectrum of fall risk. Generally, participants did not suffer from degenerative diseases and were cognitively functioning on a sufficient level. Need of walking aids was used as marker for function that was reported by a majority of studies and ranged from 0%Citation53 to 79%.Citation33 Falls during the past year, when reported, ranged from 12.4%Citation15 to 100%.Citation50 Several studies reported on previous fracturesCitation32,Citation33,Citation35,Citation48 ranging from 3.9% to 68%.
Measurement instruments for FoF and QoL
Most studies utilized standard FoF questionnaires related to self-efficacy including the FES and its variations (FES-I and MFES, translations)Citation3,Citation4,Citation37,Citation40,Citation43,Citation44,Citation47,Citation48,Citation50–Citation53,Citation55,Citation56 and the ABC scale.Citation30,Citation57 The SAFE, measuring the activity restrictions due to FoF was used in three studies.Citation4,Citation34,Citation49 Nine studies identified FoF with a single question;Citation15,Citation31,Citation32,Citation38,Citation39,Citation41,Citation42,Citation46,Citation54 however, response options partially differed (dichotomized, 3-, 4-, 6-level scale). One study applied three questionnaires for different aspects of FoF (consequences of falling: CONSq; falls-efficacy measures – concern and fear about falling: CAFlik, balance confidence: CONbal).Citation45 Another study developed an instrument that used ratings by nursing staff in combination with a newly developed QoL questionnaire in people with FoF consisting of three subscales, one of them being “fear of falling”.Citation33
The evaluation of the participants’ QoL was also administered by a wide range of standard instruments, the SF-36,Citation4,Citation38,Citation40–Citation42,Citation46,Citation51,Citation53,Citation56 SF-12,Citation43,Citation49 SF-8,Citation35 EQ-5D,Citation30,Citation32,Citation44 WHOQOL–BREF,Citation31 modified WHOQOL-OLD,Citation54 Short Happiness and Affect Research Protocol (SHARP),Citation36 LEIPAD,Citation50 WHO (Five) Well-Being Index (WHO-5),Citation50 Social Production Function Instrument (SPF-IL),Citation52 Nottingham Health Profile (NHP),Citation33,Citation37 Philadelphia Geriatric Morale Scale (PGMS),Citation45 and Chinese Personal Wellbeing Index (CPWI).Citation47 Eight studies used single questions related to self-rated health (SRH) status using a visual analog scaleCitation57 or graded response options with dichotomized,Citation15 three,Citation48 four,Citation39 and five categories.Citation34,Citation46,Citation52,Citation55
Methodological quality assessment
The methodological quality of included studies was largely homogeneous (). With the exception of one study,Citation54 the population was clearly defined. However, in only half of the studies, the participation rate was clearly 50% or above, potentially affecting generalizability of results. For the questions of interest, all but one study were of cross-sectional design.Citation30 However, also in the study by Davis et al, no temporal relationship between falls-related self-efficacy and QoL was investigated and thus forbidding any cause–effect relationship.Citation30 Except for few studies for which scoring, or test–retest reliability were unclear, all studies used valid and reliable instruments for FoF and QoL. For the mediating effect of actual fall events on the relationship between FoF and QoL, none of the studies included exclusively these three measures and models were adjusted for different variables, mostly related to demographics and health. Small sample sizes likely impacted on the results in several studies. This was also due to most studies having had other primary objectives than the current review. None of the studies reported on blinding of outcome assessors for relevant outcomes.
Table 2 Rating of methodological quality of included studies using the ‘Quality assessment tool for observational cohort and cross-sectional studies’Citation29
Prevalence/incidence of fear of falling
From 30 articles, several did not provide data on prevalence, incidence, or point estimates with spread measures of FoF for their respective study samples.Citation4,Citation34,Citation43,Citation45 Prevalence rates of remaining studies varied widely likely due to differences in sample characteristics and measurement properties (scoring, number of categories, wording). Participants without mobility restrictions or increased fall risk had the lowest FoF prevalence (<30%).Citation15,Citation39,Citation40,Citation57 Higher prevalence rates of FoF were found in frail populations,Citation38 increased with the number of experienced falls,Citation36,Citation50,Citation57 was higher in people at increased risk of hip fracturesCitation32 or in those with previous fall-related fractures,Citation48 in individuals with chronic musculoskeletal painCitation57 and in people requiring walking aids for ambulation.Citation4,Citation39,Citation53,Citation57 Several studies reported higher levels of FoF in women.Citation4,Citation36,Citation38,Citation39,Citation41,Citation46–Citation48,Citation53,Citation55
What is the effect of FoF on QoL?
Better QoL was consistently associated with lower levels of FoF. Comparison of means/ranks showed that people with less FoF rated their QoL better.Citation31,Citation36,Citation41,Citation42,Citation46,Citation47,Citation49,Citation52,Citation57 When using multiple categories for FoF, this seems to be a linear relationship with higher levels of FoF being associated with poorer scores on QoL.Citation15,Citation32,Citation38,Citation48,Citation50,Citation52,Citation57 Several studies reported moderate to strong correlations between FoF and QoL (r=−0.47 to −0.80).Citation30,Citation37,Citation43,Citation45,Citation51,Citation52,Citation55 The relationship between FoF and QoL appears to be stronger for the physical than for the mental components of QoL. Comparing sub-scales of the SF-36 and its modified versions, highest correlations were observed for the physical function domain.Citation4,Citation35,Citation40,Citation53,Citation56 Beside the physical function domain, also other physical domains such as bodily pain,Citation15,Citation35,Citation40,Citation46,Citation56 general health perceptions,Citation4,Citation15,Citation40,Citation46,Citation56 and physical role functioningCitation15,Citation35,Citation46,Citation56 were associated with FoF. Exceptions were studies that found similar associations with the mental health domain.Citation46,Citation56 One study demonstrated a moderate correlation between the social role functioning domain and FoF, measured with FES and SAFE in residents of public senior housing communities.Citation4
Regression analyses showed that FoF is an independent predictor for QoL.Citation15,Citation30,Citation32,Citation39,Citation41,Citation44,Citation46–Citation48,Citation50–Citation52 Again, this relationship was stronger for the physical components of QoL.Citation4,Citation35,Citation40,Citation44,Citation50 Stretton and colleaguesCitation51 reported that the MFES was the single highest contributor to SF-36 physical component summary score and the physical function domain in frail older adults. Moreover, FoF and QoL appeared to be more important for predicting each other than other basic variables such as age, gender, previous falls, and comorbidity.Citation4,Citation40,Citation46,Citation48,Citation51 In contrast, Valentine and colleaguesCitation45 using structural equation modeling found no direct effect of balance confidence or self-efficacy on the relationship between postural instability and QoL in a geriatric rehabilitation setting; however, they found a relationship between QoL and general anxiety. Yodmai and colleaguesCitation54 found no associations between FoF and QoL scales, but low-level FoF during use of public transport was linked to better QoL.
Hsu et alCitation43 demonstrated a mediating effect of physical activity (PA) participation and the self-concept of health and physical independence on the relationship between FOF and QoL with lower PA levels being associated with higher FoF and reduced QoL in two independent samples in Germany and Taiwan.
Does the association depend on the operationalization of FoF or QoL?
The relevance of FoF for QoL appeared to be independent of the FoF instruments used as evidenced by the consistent results of the association across studies that administered different instruments. Few studies administered more than one instrument related to the FoF construct. The SAFE explained a comparable amount of variance in QoL (SF-36, 1-item question SRH) as the FES and a single question measurement of FoF (four levels).Citation4 Contrary, Valentine et al applied the Caflik as a measure for fear of falling and the Confbal for balance confidence and both tools were parts of different paths in structural equation models.Citation45
Most studies administered the SF-36, an abbreviated version of this instrument, SRH questions or the EQ-5D to assess QoL and nearly in all of these studies a significant association was demonstrated. The WHOQOL-BREFCitation31 and mod WHOQOL-OLD,Citation54 administered each in one study, did not show an overall association with FoF in Asian samples, although latter found a reduced level of QoL during public transport use and FoF. The use of the PGMS also demonstrated no association with FoF.Citation45 Two studies administered more than one instrument of QoL. Tiernan et alCitation52 found in multivariate logistic regression analyses that FoF (adapted FES) was a significant contributor to SRH and well-being (SPF-IL). However, the amount of variance explained was larger for SRH.Citation52 Another study found that older women with a falls history who were moderately or highly concerned about falls (FES-I) reported poorer QoL (LEIPAD) and well-being (WHO-5) than those with low levels of concern.Citation50 Due to the very wide confidence intervals, a direct comparison could not be done.
Is there a mediating effect of falls on the association between FoF and QoL?
To explore the potential mediating effect of actual fall events on the association of FoF and QoL, we looked at studies that used multivariate modeling and included all three variables. Several studies found FoF and falls to be independent predictors of QoL.Citation4,Citation15,Citation39 Findings in studies with community-dwelling older people, including those from large epidemiological studies, however, indicated that FoF was a significant risk factor for reduced QoL after controlling for falls or fall-related injuries with little or no mediation from actual falls.Citation32,Citation41,Citation44,Citation52 Iglesias and colleagues found that the main burden of QoL loss was FoF which was consistently associated with this outcome in three large datasets, while falls and fractures had much smaller effect sizes, with fall events being non-significant in two of these three studies.Citation32 Similarly, Tiernan et al found that when including falls-efficacy and falls into the modeling process, latter added very little to the relationship with SRH beyond that explained by falls-efficacy.Citation52 Contrary, FoF and falls were maintained independent predictors for well-being.Citation52 Finally, Lin and colleagues demonstrated that among other factors, FoF was an independent predictor for overall QoL while fall events were not in community-dwelling elderly with functional limitations.Citation44 Regarding individual domains of QoL these authors found both, FoF and falls were associated with self-care but only FoF was linked to mobility.Citation44 In another study, fall history and FoF were associated with the physical function component of the SF-36 but only FoF was also associated with the mental function component.Citation41
Two of the identified studies were conducted in institutionalized settings.Citation35,Citation45 Kato found no mediating influence of falls on the relationship between falls-efficacy and the physical function component of the SF-8 in female nursing home residents.Citation35 The study by Valentine and colleagues using structural equation modeling found no direct or indirect effect of falls, balance confidence, and falls-efficacy on the relationship between instability and QoL.Citation45
Discussion
This systematic review aimed at determining the impact of FoF on QoL in older adults and the effect of actual fall events on this relationship. We found that FoF was consistently and strongly associated with QoL and this association appeared to be independent of the conceptualizations of FoF and QoL. Moreover, this relationship is independent of falls people experienced which seem to have a lower impact.
What is the effect of FoF on QoL?
Our results demonstrate a robust association of lower levels of FoF and higher perceived QoL. In multivariate analyses of single studies, FoF remained an independent predictor of QoL. Furthermore, the relationship appears to be more important than other basic variables such as age and gender.Citation4,Citation51
Fear is an important emotional trait that evolved and triggers innate responses important for survival and one of these fears is the fear of heights or depth which may lead to a fall with serious if not fatal consequences.Citation58 How the concept of FoF in older adults fits in this context is less well established. But it seems that fearful individuals elicit postural responses in everyday activities that younger fearful people demonstrate when exposed to heights >3 m.Citation59 Thus, emotion and balance control are associated with each other and more fearful people seem to learn associations between specifically related tasks and an avoidance response.Citation60 While an activity avoidance may protect from dangerous situations and can already be observed in infants,Citation61 it may be maladaptive if it exceeds a certain level, and thereby, the fear becomes debilitating, initiating a vicious cycle of activity reduction and physical and mental decline.Citation62 In line with this, Hsu et alCitation43 found a mediating effect of PA on the relationship between FoF and QoL.
While fear itself is a psychological construct, highest correlations were found not for mental but for physical components of QoL.Citation4,Citation33,Citation35,Citation46,Citation49,Citation52 Particularly strong associations with FoF were found for physical function, general health perceptions, bodily pain status, vitality, physical role functioning, and physical mobility,Citation4,Citation15,Citation33,Citation35,Citation40,Citation56 indicating that physical components of health are key determinants for high QoL. This is confirmed by findings that QoL is lower in people with medical conditions that affect physical functioning, including multimorbid and frail individualsCitation63 while FoF is increased in physically frail older adults.Citation64
It seems that the association between these physical limitations and FoF is in parts due to restricting activity participation and subsequent negative consequences. Similarly, one study in people with chronic musculoskeletal pain found that activity restriction due to FoF was associated with sedentary behavior.Citation65 Howland and colleagues found the influence of FOF on activity restriction to be independent after controlling for other factors such as age, sex, pain, self-rated health, previous falls, medications, and the use of walking aids.Citation39 This finding supports other results which stated that FOF is a significant predictor of activity restriction and that individuals being fearful were distinguished from those that additionally restricted their activities.Citation14,Citation66
Findings also indicate that activity restriction is related not only to physical functioning but also to psychological issues, such as depression.Citation67,Citation68 Individual studies found associations between mental health, social functioning and QoL,Citation4,Citation56 emphasizing that QoL is a complex multifactorial construct. This association may be linked to a maladaptive degree of activity restriction too. Fear only has positive effects as long as social and physical mobility is not decreased.Citation69 Also, less social interaction, participation and becoming homebound can cause not only physical but also mental problems, resulting in reduced levels of QoL.Citation70
The limitation of physical functions and reduction of social activities can lead to mental problems such as depression and loss of self-confidence. Self-critical thinking, low functional performance, and limited personal and social activities are risk or exacerbating factors for depressive symptoms in older people.Citation71 Taking the physical and mental components together, activity restriction in older people can lead to deconditioning, depression, social isolation and thus reduced QoL.Citation72 Hence, activity restriction appears to be an important link between FoF and QoL. Today it remains unclear, when and how individuals decide to avoid certain activities. A small qualitative study in people with FoF found that some individuals’ QoL were not affected by their FoF while in others it led to restrictions of activities.Citation73 It seems that this complex process involves physical and cognitive functions, rating one’s own risk and subsequent risk-taking behavior and is influenced by personality traits (especially introversion/extroversion), depressive symptoms among other factors.Citation36,Citation74–Citation76 Anxious people may overestimate their actual risk of falling and subsequently avoid activities.Citation74
Evidence suggests a direct link of FoF related measures on physical performance, such as balance and gait.Citation77 Thus, QoL likely is also diminished by reduced physical functioning not related to activity restriction. In addition, recent fall experience has been associated with post-traumatic stress disorder in older people.Citation78 Also, anxiety has been associated with chronic stress and the perseverative cognitive representation leads to elevated stress levels.Citation79 As people are permanently concerned about falling, inflammation levels may be increased affecting one’s physical and mental health.Citation80–Citation82 To our knowledge, no study has been published on this topic with regard to FoF but it might be another path how QoL is reduced by FoF.
Does the association depend on the operationalization of FoF or QoL?
No obvious systematic difference on the relationship of FoF and QoL in dependence of measurement method of FoF was found. A lower degree of FoF was consistently associated with better perceived QoL, independent of the instrument used for FoF and QoL. The majority of studies administered measures for falls-efficacy, the SAFE or 1-item questions for FoF and versions of the MOS questionnaire or 1-item SRH questions for QoL. Administering more than one instrument led to results pointing into the same direction,Citation39,Citation50,Citation52,Citation53 indicating that the underlying association was similar. Psychometric properties of multi-item generic measures of QoL and FoF measures have been questioned,Citation83,Citation84 but most of the ones used in the analyses were judged to be valid, internally consistent and reliable. Some QoL instruments were not associated with FoF but were each only administered in one study (WHOQOL-BREF,Citation31 mod WHOQOL-OLD,Citation54 PGMSCitation45). This may be caused by the different operationalization of QoL or sample characteristics and more studies are needed to draw firm conclusions.
While direct measurement of FoF and instruments of falls-efficacy were used, the latter construct has been criticized, as it is possible that people are confident of their abilities to engage in activities but may still be fearful of having a fall.Citation69 Similarly, Hadjistavropoulos, Delbaere, and Fitzgerald argue that these constructs are not be used interchangeably as often done.Citation77 Supporting this, the study by Valentine found no association between the constructs of self-efficacy, FoF and QoL using structural equation modeling.Citation45 However, these authors applied different (newly developed) instruments that require further external validation. The authors point out that FoF in older adults is a multifactorial construct that is related to postural stability and lesser to general anxiety.Citation45 Future studies of sufficient size are needed to determine the more complex relationships between concepts involved. There is limited evidence that suggests a difference in people that are concerned about falling and those that additionally restrict their activities.Citation14 These groups are likely affected differently in their QoL. This relationship requires further investigation.
There is a need for further validation of FoF instruments potentially conceptualizing different constructs. For instance, brain networks including sub-cortical (low road) and higher cortical centers (high road) have been described as pathways in the processing of fear.Citation85 However, sufficient data to show in how far FoF is associated to these are lacking.
Is there a mediating effect of falls on the association between FoF and QoL?
The majority of studies that included actual fall events as variable in the association between FoF or QoL found both, FoF and falls to be independent predictor of QoL or QoL and falls for FoF. All three concepts have been shown to be influenced not only by each other but also by multiple other factors. The fact that non-fallers may also be concerned about falls also indicates the independence of these measures.Citation2 Falls and FoF independently predict each other and individuals, who have one of them, also have an increased risk to develop the other outcome.Citation86 It has been shown that this fear declines linearly over time and becomes non-significant after two to three years without falling.Citation87 However, it appears that in about 60% of the individuals FoF is persistent, with previous falls and female gender being independent risk factors.Citation88 This may indicate different coping strategies that lead to the misperception of fall risk in some individualsCitation74 and may further confirm the detrimental effect of persistent cognitions. Apart from being independent predictors of QoL, samples without heightened fall risk (eg, use of mobility aids, falls in the recent past) had the lowest levels of FoF. Higher prevalence of FoF was found in study populations with poorer general condition, with higher proportions of frail people or with heightened fall risk. Mentioned attributes were already identified as risk factors for FoF in a literature review.Citation2 This demonstrates that FoF and falls also share some variance.
However, some studies demonstrated that fall events played no or a minor role in the association of FoF and QoL.Citation32,Citation35,Citation41,Citation44,Citation52 FoF is associated with psychological factors (eg, depression) and physical function which in turn are known risk factors for falls in the elderly.Citation89 Murphy, Dubin, & Gill demonstrated that falls were only associated with FoF when other predisposing factors were present.Citation90 It may be that instead of a direct relationship of falls, other with falls associated factors mediate the relationship between FoF and QoL, such as functional performance measures (instability, mobility).Citation44,Citation45 Recently, the simplistic vicious cycle in which fear leads to restriction of activities, deconditioning and increased risk of falls has been questioned.Citation77 An alternative model in which FoF affects falls-efficacy which in turn affects balance performance negatively leading to an increased fall risk has been proposed.Citation77 However, the multiple causes of falls are still not untangled and quite likely both paths play a role in the genesis of falls. In addition, it has been demonstrated that the level of PA mediates the relationship between FoF and outdoor falls.Citation13 Low PA levels could be a proxy for activity restriction. As most studies did not obtain this measure, current evidence might underestimate the direct impact of fall-related activity restriction on the association between FoF and QoL. Future studies are required to determine more complex and accurate cause–effect models.
Clinical implications
Findings of this review demonstrate the importance of FoF on QoL and thus on the subjectively perceived well-being of an individual. Hence, the identification of individuals at risk and the subsequent intervention to reduce FoF are important to increase QoL in older people. FoF and associated factors are modifiable risk factors and should be targeted in clinical interventions to improve QoL as important patient-centered outcome. The relationship between FoF and QoL appears to be partially mediated by physical and cognitive functioning and by higher levels of PA. Increased PA levels and in particular structured exercise have been linked to improve physicalCitation91 and cognitive functioning,Citation92 reduced levels of FoF,Citation93 and increased QoL.Citation94
Also, cognitive-behavioral interventions that can be administered at home and aim at cognitive re-structuring to instill adaptive and realistic views are effective in reducing FoF and related activity restriction in older adults,Citation95 partially mediated by psychosocial factors such as control beliefs, self-efficacy, and outcome expectations.Citation96
Limitations of the review
We acknowledge several limitations of this review. First, only English language and full articles were included. Therefore, it is possible that relevant studies not fulfilling these criteria were excluded. Second, some articles were excluded due to populations with specific diseases. While included studies often did not exclude individuals with specific conditions or multimorbidity, the generalizability of results may be limited. Third, different scales and instruments were used to conceptualize the constructs of FoF and QoL. Although these might not measure exactly the same, our results were quite similar and did not appear to be influenced by the underlying differences. Finally, we did not investigate the effect of specific or non-specific interventions on the relationship between FoF and QoL. To our knowledge, there has been no systematic review published on this topic.
Conclusions
Findings of this systematic review demonstrate the importance of fear of falling on quality of life in older individuals which is independent of fall events and appears to be more important than actual falls. This association also seems to be independent of different conceptualizations of FoF. Clinically, this implies FoF should be considered not only as by-product of falls and requires targeted interventions, different from those aiming to reduce falls. More research is needed to prospectively investigate the cause–effect relationship of FoF, falls and QoL, determine the validity of different constructs involved, and to investigate whether specific activities are linked stronger to QoL than others.
Disclosure
The authors report no conflicts of interest in this work.
References
- Aoyagi K, Ross PD, Davis JW, Wasnich RD, Hayashi T, Takemoto T-I. Falls among community-dwelling elderly in Japan. J Bone Miner Res. 1998;13(9):1468–1474. doi:10.1359/jbmr.1998.13.9.14689738520
- Scheffer AC, Schuurmans MJ, van Dijk N, van der Hooft T, de Rooij SE. Fear of falling: measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37(1):19–24. doi:10.1093/ageing/afm16918194967
- Murphy J, Isaacs B. The post-fall syndrome. A study of 36 elderly patients. Gerontology. 1982;28(4):265–270. doi:10.1159/0002125437117852
- Lachman ME, Howland J, Tennstedt S, Jette A, Assmann S, Peterson EW. Fear of falling and activity restriction: the survey of activities and fear of falling in the elderly (SAFE). J Gerontol B Psychol Sci Soc Sci. 1998;53(1):P43–50. doi:10.1093/geronb/53B.1.P439469171
- Lawrence RH, Tennstedt SL, Kasten LE, Shih J, Howland J, Jette AM. Intensity and correlates of fear of falling and hurting oneself in the next year: baseline findings from a Roybal center fear of falling intervention. J Aging Health. 1998;10(3):267–286. doi:10.1177/08982643980100030110342933
- Legters K. Fear of falling. Phys Ther. 2002;82(3):264–272.11869155
- Myers AM, Powell LE, Maki BE, Holliday PJ, Brawley LR, Sherk W. Psychological indicators of balance confidence: relationship to actual and perceived abilities. J Gerontol A Biol Sci Med Sci. 1996;51(1):M37–43. doi:10.1093/gerona/51A.1.M378548512
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi:10.1037/0033-295X.84.2.191847061
- Tinetti ME, Richman D, Powell L. Falls efficacy as a measure of fear of falling. J Gerontol. 1990;45(6):P239–243.2229948
- Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50a(1):M28–34.7814786
- Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ. Fear of falling and restriction of mobility in elderly fallers. Age Ageing. 1997;26(3):189–193. doi:10.1093/ageing/26.3.1899223714
- Donoghue OA, Cronin H, Savva GM, O’Regan C, Kenny RA. Effects of fear of falling and activity restriction on normal and dual task walking in community dwelling older adults. Gait Posture. 2013;38(1):120–124. doi:10.1016/j.gaitpost.2012.10.02323200462
- Wijlhuizen GJ, de Jong R, Hopman-Rock M. Older persons afraid of falling reduce physical activity to prevent outdoor falls. Prev Med. 2007;44(3):260–264. doi:10.1016/j.ypmed.2006.11.00317184828
- Murphy SL, Williams CS, Gill TM. Characteristics associated with fear of falling and activity restriction in community-living older persons. J Am Geriatr Soc. 2002;50(3):516–520.11943049
- Arfken CL, Lach HW, Birge SJ, Miller JP. The prevalence and correlates of fear of falling in elderly persons living in the community. Am J Public Health. 1994;84(4):565–570.8154557
- Elliott MS, Barris R. Occupational role performance and life satisfaction in elderly persons. Occup Ther J Res. 1987;7(4):215–224. doi:10.1177/153944928700700403
- Levasseur M, Desrosiers J, Noreau L. Is social participation associated with quality of life of older adults with physical disabilities? Disabil Rehabil. 2004;26(20):1206–1213. doi:10.1080/0963828041233127037115371021
- Gerok W, Brandstädter J. Normales, krankhaftes und optimales altern: variations- und Modifikationsspielräume In: Baltes PB, Mittelstraß J, Staudinger UM, editors. Alter und Altern: Ein interdisziplinärer Studientext zur Gerontologie. Berlin: de Gruyter; 1994:356–386.
- Halvorsrud L, Kalfoss M. The conceptualization and measurement of quality of life in older adults: a review of empirical studies published during 1994–2006. Eur J Ageing. 2007;4(4):229–246. doi:10.1007/s10433-007-0063-328794792
- Bowling A. Measuring Disease, second edition. Philadelphia: Open University Press; 2001.
- Noro A, Aro S. Health-related quality of life among the least dependent institutional elderly compared with the non-institutional elderly population. Qual Life Res. 1996;5(3):355–366. doi:10.1007/BF04339208763804
- Bakas T, McLennon SM, Carpenter JS, et al. Systematic review of health-related quality of life models. Health Qual Life Outcomes. 2012;10(1):134. doi:10.1186/1477-7525-10-13423158687
- Romero M, Vivas-Consuelo D, Alvis-Guzman N. Is Health Related Quality of Life (HRQoL) a valid indicator for health systems evaluation? SpringerPlus. 2013;2(1):664. doi:10.1186/2193-1801-2-66424353981
- de Wit M, Hajos T. Health-related quality of life In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. New York: Springer New York; 2013:929–931.
- Organization WH. Good Health Adds Life to Years: Global Brief for World Health Day 2012. Geneva: WHO; 2012.
- Deshpande PR, Rajan S, Sudeepthi BL, Abdul Nazir CP. Patient-reported outcomes: A new era in clinical research. Perspect Clin Res. 2011;2(4):137–144. doi:10.4103/2229-3485.8687922145124
- NICE. Multimorbidity: clinical assessment and management. NICE guideline [NG56]; 2016 Available from: https://www.nice.org.uk/guidance/ng56/resources/multimorbidity-clinical-assessment-and-management-pdf-1837516654789. Accessed November 28, 2018.
- Yarnall AJ, Sayer AA, Clegg A, Rockwood K, Parker S, Hindle JV. New horizons in multimorbidity in older adults. Age Ageing. 2017;46(6):882–888. doi:10.1093/ageing/afx15028985248
- National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Bethesda: National Institutes of Health, Department of Health and Human Services; 2014.
- Davis JC, Marra CA, Liu-Ambrose TY. Falls-related self-efficacy is independently associated with quality-adjusted life years in older women. Age Ageing. 2011;40(3):340–346. doi:10.1093/ageing/afr01921436152
- Basalan IF, Atay E. How effective are exercise recommendations supported by written and visual materials in elderly people? Turk Geriatri Dergisi. 2014;17(4):410–416.
- Iglesias CP, Manca A, Torgerson DJ. The health-related quality of life and cost implications of falls in elderly women. Osteoporos Int. 2009;20(6):869–878. doi:10.1007/s00198-008-0753-518846400
- Warnke A, Meyer G, Bott U, Mühlhauser I, Validation of a quality of life questionnaire measuring the subjective fear of falling in nursing home residents. Z Gerontol Geriatr. 2004;37(6):459–466. Available from: http://onlinelibrary.wiley.com/o/cochrane/clcentral/articles/419/CN-00511419/frame.html. doi:10.1007/s00391-004-0214-515614598
- Yeung FKC, Chou KL, Wong ECH. Characteristics associated with fear of falling in Hong Kong Chinese elderly residing in care and attention homes. Clin Gerontol. 2006;29(3):83–98. doi:10.1300/J018v29n03_07
- Kato C, Ida K, Kawamura M, et al. Relation of falls efficacy scale (FES) to quality of life among nursing home female residents with comparatively intact cognitive function in Japan. Nagoya J Med Sci. 2008;70(1–2):19–27.18807292
- Kloseck M, Hobson S, Crilly R, Vandervoort A, Ward-Griffin C. The influence of personality on falling and engagement in daily activities by community-dwelling older adults. Phys Occup Ther Geriatr. 2007;26(1):1–17. doi:10.1080/J148v26n01_01
- Cinarli T, Koc Z. Fear and risk of falling, activities of daily living, and quality of life: assessment when older adults receive emergency department care. Nurs Res. 2017;66(4):330–335. doi:10.1097/NNR.000000000000022728654570
- Suzuki M, Ohyama N, Yamada K, Kanamori M. The relationship between fear of falling, activities of daily living and quality of life among elderly individuals. Nurs Health Sci. 2002;4(4):155–161. doi:10.1046/j.1442-2018.2002.00123.x12406202
- Howland J, Peterson EW, Levin WC, Fried L, Pordon D, Bak S. Fear of falling among the community-dwelling elderly. J Aging Health. 1993;5(2):229–243. doi:10.1177/08982643930050020510125446
- Akosile CO, Anukam GO, Johnson OE, et al. Fear of falling and quality of life of apparently-healthy elderly individuals from a nigerian population. J Cross Cult Gerontol. 2014;29(2):201–209. doi:10.1007/s10823-014-9228-724710949
- Chang N, Chi L, Yang N, Chou P. The impact of falls and fear of falling on health-related quality of life in Taiwanese elderly. J Community Health Nurs. 2010;27(2):84–95. doi:10.1080/0737001100370495820437289
- Chang N, Yang N, Chou P. Incidence, risk factors and consequences of falling injuries among the community-dwelling elderly in Shihpai, Taiwan. Aging Clin Exp Res. 2010;22(1):70–77. doi:10.1007/BF332481819934620
- Hsu Y, Alfermann D, Lu FJH, Lin LL. Pathways from fear of falling to quality of life: the mediating effect of the self-concept of health and physical independence. Aging Ment Health. 2013;17(7):816–822. doi:10.1080/13607863.2013.80539823767870
- Lin SI, Chang KC, Lee HC, Yang YC, Tsauo JY. Problems and fall risk determinants of quality of life in older adults with increased risk of falling. Geriatr Gerontol Int. 2015;15(5):579–587. doi:10.1111/ggi.1232025109554
- Valentine JD, Simpson J, Worsfold C, Fisher K. A structural equation modelling approach to the complex path from postural stability to morale in elderly people with fear of falling. Disabil Rehabil. 2011;33(4):352–359. doi:10.3109/09638288.2010.49157520533873
- Chang HT, Chen HC, Chou P. Factors associated with fear of falling among community-dwelling older adults in the Shih-Pai study in Taiwan. PLoS One. 2016;11(3):e0150612. doi:10.1371/journal.pone.015061226933882
- Liu JY. Fear of falling in robust community-dwelling older people: results of a cross-sectional study. J Clin Nurs. 2015;24(3–4):393–405. doi:10.1111/jocn.2015.24.issue-3pt424787119
- Malini FM, Lourenco RA, Lopes CS. Prevalence of fear of falling in older adults, and its associations with clinical, functional and psychosocial factors: the frailty in Brazilian older people-Rio de Janeiro study. Geriatr Gerontol Int. 2016;16(3):336–344. doi:10.1111/ggi.1247725869919
- Li F, Fisher KJ, Harmer P, McAuley E, Wilson NL. Fear of falling in elderly persons: association with falls, functional ability, and quality of life. J Gerontol B Psychol Sci Soc Sci. 2003;58(5):P283–290. doi:10.1093/geronb/58.5.P28314507935
- Patil R, Uusi-Rasi K, Kannus P, Karinkanta S, Sievanen H. Concern about falling in older women with a history of falls: associations with health, functional ability, physical activity and quality of life. Gerontology. 2014;60(1):22–30. doi:10.1159/00035433524107382
- Stretton CM, Latham NK, Carter KN, Lee AC, Anderson CS. Determinants of physical health in frail older people: the importance of self-efficacy. Clin Rehabil. 2006;20(4):357–366. doi:10.1191/0269215506cr946oa16719034
- Tiernan C, Lysack C, Neufeld S, Goldberg A, Lichtenberg PA. Falls efficacy and self-rated health in older African American adults. Arch Gerontol Geriatr. 2014;58(1):88–94. doi:10.1016/j.archger.2013.08.00524063870
- Baharlouei H, Salavati M, Akhbari B, Mosallanezhad Z, Mazaheri M, Negahban H. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) using self-report and interview-based questionnaires among Persian-speaking elderly adults. Arch Gerontol Geriatr. 2013;57(3):339–344. doi:10.1016/j.archger.2013.06.00523830993
- Yodmai K, Phummarak S, Sirisuth JC, Kumar R, Somrongthong R. Quality of life and fear of falling among an aging population in semi rural, Thailand. J Ayub Med Coll Abbottabad. 2015;27(4):771–774.27004319
- Hoang OT, Jullamate P, Piphatvanitcha N, Rosenberg E. Factors related to fear of falling among community-dwelling older adults. J Clin Nurs. 2017;26(1–2):68–76. doi:10.1111/jocn.1333727723217
- Billis E, Strimpakos N, Kapreli E, et al. Cross-cultural validation of the Falls Efficacy Scale International (FES-I) in Greek community-dwelling older adults. Disabil Rehabil. 2011;33(19–20):1776–1784. doi:10.3109/09638288.2010.54693721219254
- Stubbs B, Schofield P, Patchay S, Leveille S. Musculoskeletal pain characteristics associated with lower balance confidence in community-dwelling older adults. Physiother. 2016;102(2):152–158. doi:10.1016/j.physio.2015.03.3721
- Ohman A, Mineka S. Fears, phobias, and preparedness: toward an evolved module of fear and fear learning. Psychol Rev. 2001;108(3):483–522. doi:10.1037/0033-295X.108.3.48311488376
- Davis JR, Campbell AD, Adkin AL, Carpenter MG. The relationship between fear of falling and human postural control. Gait Posture. 2009;29(2):275–279. doi:10.1016/j.gaitpost.2008.09.00618963992
- Tinetti ME, Powell L. Fear of falling and low self-efficacy: a case of dependence in elderly persons. J Gerontol. 1993;48:Spec No:35–38. doi:10.1093/geronj/48.Special_Issue.35
- Gibson EJ, Walk RD. The “visual cliff.”. Sci Am. 1960;202(4):64–71. doi:10.1038/scientificamerican0460-6413827949
- Cumming RG, Salkeld G, Thomas M, Szonyi G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J Gerontol A Biol Sci Med Sci. 2000;55(5):M299–305. doi:10.1093/gerona/55.5.M29910819321
- Li CI, Lin CH, Lin WY, et al. Successful aging defined by health-related quality of life and its determinants in community-dwelling elders. BMC Public Health. 2014;14:1013. doi:10.1186/1471-2458-14-101325263664
- Esbri-Victor M, Huedo-Rodenas I, Lopez-Utiel M, et al. Frailty and fear of falling: the FISTAC study. J Frailty Aging. 2017;6(3):136–140.28721429
- Stubbs B, Patchay S, Soundy A, Schofield P. The avoidance of activities due to fear of falling contributes to sedentary behavior among community-dwelling older adults with chronic musculoskeletal pain: a multisite observational study. Pain Med. 2014;15(11):1861–1871. doi:10.1111/pme.1257025224385
- Fletcher PC, Guthrie DM, Berg K, Hirdes JP. Risk factors for restriction in activity associated with fear of falling among seniors within the community. J Patient Saf. 2010;6(3):187–191. doi:10.1097/PTS.0b013e3181f1251c21491793
- Boltz M, Resnick B, Capezuti E, Shuluk J. Activity restriction vs. self-direction: hospitalised older adults’ response to fear of falling. Int J Older People Nurs. 2014;9(1):44–53. doi:10.1111/opn.2014.9.issue-123295109
- Mausbach BT, Chattillion EA, Moore RC, Roepke SK, Depp CA, Roesch S. Activity restriction and depression in medical patients and their caregivers: a meta analysis. Clin Psychol Rev. 2011;31(6):900–908. doi:10.1016/j.cpr.2011.04.00421600868
- Jung D. Fear of falling in older adults: comprehensive review. Asian Nurs Res (Korean Soc Nurs Sci). 2008;2(4):214–222. doi:10.1016/S1976-1317(09)60003-725029959
- Painter JA, Allison L, Dhingra P, Daughtery J, Cogdill K, Trujillo LG. Fear of falling and its relationship with anxiety, depression, and activity engagement among community-dwelling older adults. Am J Occup Ther. 2012;66(2):169–176. doi:10.5014/ajot.2012.00253522394526
- Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. 2009;5:363–389. doi:10.1146/annurev.clinpsy.032408.15362119327033
- Vlaeyen JW, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85(3):317–332. doi:10.1016/S0304-3959(99)00242-010781906
- Tischler L, Hobson S. Fear of falling: a qualitative study among community-dwelling older adults. Phys Occup Ther Geriatr. 2005;23(4):37–53. doi:10.1080/J148v23n04_03
- Delbaere K, Close JC, Brodaty H, Sachdev P, Lord SR. Determinants of disparities between perceived and physiological risk of falling among elderly people: cohort study. BMJ. 2010;341:c4165. doi:10.1136/bmj.c416520724399
- Butler AA, Lord SR, Taylor JL, Fitzpatrick RC. Ability versus hazard: risk-taking and falls in older people. J Gerontol A Biol Sci Med Sci. 2015;70(5):628–634. doi:10.1093/gerona/glu20125387729
- Butler AA, Lord SR, Fitzpatrick RC. Perceptions of speed and risk: experimental studies of road crossing by older people. PLoS One. 2016;11(4):e0152617. doi:10.1371/journal.pone.015261727054918
- Hadjistavropoulos T, Delbaere K, Fitzgerald TD. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J Aging Health. 2011;23(1):3–23. doi:10.1177/089826431037803920852012
- Bloch F. Literature review and meta-analysis of risk factors for delayed post-traumatic stress disorder in older adults after a fall. Int J Geriatr Psychiatry. 2017;32(2):136–140. doi:10.1002/gps.v32.227723122
- Brosschot JF. Markers of chronic stress: prolonged physiological activation and (un)conscious perseverative cognition. Neurosci Biobehav Rev. 2010;35(1):46–50. doi:10.1016/j.neubiorev.2010.01.00420096302
- Vogelzangs N, Beekman ATF, de Jonge P, Penninx BWJH. Anxiety disorders and inflammation in a large adult cohort. Transl Psychiatry. 2013;3(4):e249. doi:10.1038/tp.2013.2723612048
- Miller GE, Blackwell E. Turning up the heat:inflammation as a mechanism linking chronic stress, depression, and heart disease. Curr Dir Psychol Sci. 2006;15(6):269–272. doi:10.1111/j.1467-8721.2006.00450.x
- Korte SM. Corticosteroids in relation to fear, anxiety and psychopathology. Neurosci Behav Rev. 2001;25(2):117–142. doi:10.1016/S0149-7634(01)00002-1
- Haywood KL, Garratt AM, Fitzpatrick R. Quality of life in older people: a structured review of generic self-assessed health instruments. Qual Life Res. 2005;14(7):1651–1668. doi:10.1007/s11136-005-1743-016119178
- Denkinger MD, Lukas A, Nikolaus T, Hauer K. Factors associated with fear of falling and associated activity restriction in community-dwelling older adults: a systematic review. Am J Geriatr Psychiatry. 2015;23(1):72–86. doi:10.1016/j.jagp.2014.03.00224745560
- LeDoux JE. The Emotional Brain: The Mysterious Underpinnings of Emotional Life. New York: Simon & Schuster; 1996.
- Friedman SM, Munoz B, West SK, Rubin GS, Fried LP. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatr Soc. 2002;50(8):1329–1335.12164987
- Jang SN, Cho SI, Oh SW, Lee ES, Baik HW. Time since falling and fear of falling among community-dwelling elderly. Int Psychogeriatr. 2007;19(6):1072–1083. doi:10.1017/S104161020600480717288637
- Oh-Park M, Xue X, Holtzer R, Verghese J. Transient versus persistent fear of falling in community-dwelling older adults: incidence and risk factors. J Am Geriatr Soc. 2011;59(7):1225–1231. doi:10.1111/j.1532-5415.2011.03475.x21718266
- Deandrea S, Lucenteforte E, Bravi F, Foschi R, La Vecchia C, Negri E. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21(5):658–668. doi:10.1097/EDE.0b013e3181e9edc420585256
- Murphy SL, Dubin JA, Gill TM. The development of fear of falling among community-living older women: predisposing factors and subsequent fall events. J Gerontol A Biol Sci Med Sci. 2003;58(10):M943–947. doi:10.1093/gerona/58.10.M94314570863
- Steib S, Schoene D, Pfeifer K. Dose-response relationship of resistance training in older adults: a meta-analysis. Med Sci Sports Exerc. 2010;42(5):902–914. doi:10.1249/MSS.0b013e3181c3446519996996
- Kelly ME, Loughrey D, Lawlor BA, Robertson IH, Walsh C, Brennan S. The impact of exercise on the cognitive functioning of healthy older adults: a systematic review and meta-analysis. Ageing Res Rev. 2014;16:12–31. doi:10.1016/j.arr.2014.05.00224862109
- Kendrick D, Kumar A, Carpenter H, et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst Rev. 2014;(11):CD009848.25432016
- Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56(suppl_2):23–35.11730235
- Dorresteijn TA, Zijlstra GA, Ambergen AW, Delbaere K, Vlaeyen JW, Kempen GI. Effectiveness of a home-based cognitive behavioral program to manage concerns about falls in community-dwelling, frail older people: results of a randomized controlled trial. BMC Geriatr. 2016;16:2. doi:10.1186/s12877-015-0177-y26739339
- Zijlstra GA, van Haastregt JC, van Eijk JT, de Witte LP, Ambergen T, Kempen GI. Mediating effects of psychosocial factors on concerns about falling and daily activity in a multicomponent cognitive behavioral group intervention. Aging Ment Health. 2011;15(1):68–77. doi:10.1080/13607863.2010.50105420924813
