Abstract
Background
Few investigations of successful long-term weight loss beyond two years have been conducted, and none has examined weight changes in medically underserved rural populations of older adults. The purpose of this study was to assess long-term weight loss maintenance 3.5 years after the completion of an initial six-month lifestyle intervention for obesity among women aged 50–75 years residing in rural communities.
Methods
One hundred and ten obese women with a mean (± standard deviation) age of 60.08 ± 6.17 years and mean body mass index of 36.76 ± 5.10 kg/m2 completed an in-person assessment during which their weight and adherence to behavioral weight management strategies were evaluated.
Results
Participants showed a mean weight reduction of 10.17% ± 5.0% during the initial six- month intervention and regained 6.95% ± 9.44% from the completion of treatment to follow-up assessment 3.5 years later. A substantial proportion of participants (41.80%) were able to maintain weight reductions of 5% or greater from baseline to follow-up. “Successful” participants (those who maintained losses of 5% or greater at follow-up) reported weighing themselves, self-monitoring their intake and calories, planning meals in advance, and choosing lower calorie foods with greater frequency than “unsuccessful” participants (those who lost less than 5%).
Conclusion
Collectively, these findings indicate that a large proportion of participants were able to maintain clinically significant weight losses for multiple years after treatment, and that self-monitoring was a key component of successful long-term weight management.
Introduction
Reviews suggest that participants in behavioral treatment programs for obesity typically regain most of their lost weight within five years, leading to the widely held belief that sustaining long-term weight losses is exceedingly rare.Citation1,Citation2 Although obese individuals face significant behavioral, environmental, and physiological challenges following treatment, a substantial proportion of participants do manage to maintain their weight losses in the long term. However, outcomes of behavioral interventions, which typically report average weight loss, often mask the fact that large subsets of participants in lifestyle intervention programs are successful at maintaining weight losses of at least 5%. Weight reductions of 5% or greater are considered to be clinically significant because research has demonstrated that losses of this magnitude are associated with measurable improvements in risk factors for cardiovascular disease.Citation1
Research in successful weight loss maintainers suggests that weight regain is due at least in part to failure to maintain key behavior changes (self-monitoring, high levels of daily physical activity, consumption of a low-calorie, low-fat diet).Citation3 Further, several years of sustained weight maintenance increases the probability of future weight maintenance. For example, studies of participants in the National Weight Control Registry indicate that weight regain among previously successful maintainers is associated with more recent losses (<2 years versus ≥2 years), decreases in energy expenditure, and increases in fat intake.Citation3 Once individuals have regained weight it is difficult for them to recover, since small weight regains typically lead to larger ones.Citation4
While extended-care programs delivered via face-to-face, telephone, or Internet counseling can improve weight loss maintenance,Citation5,Citation6 relatively few long-term follow-up studies of successful weight loss maintainers beyond two years have been conducted. Further, a major limitation in the field of weight maintenance is that most studies of extended-care programs for obesity are conducted in academic health science centers utilizing samples of predominantly Caucasian participants from urban and suburban settings.
To our knowledge, no studies have examined the behavioral factors associated with long-term weight loss maintenance in medically underserved rural populations of older adults. Significantly higher rates of obesity and chronic disease are observed among rural adults than among their urban counterparts, even after controlling for demographic and socioeconomic factors.Citation7,Citation8 However, most published studies of obesity treatment among rural populations are in the form of case reports or case-controlled studies as opposed to randomized controlled trials.Citation9–Citation11 The obesity interventions that have been conducted have yielded weight losses that are modest compared with the 8.5 kg losses commonly achieved in lifestyle programs of similar length and intensity. Citation12 Improving both short-term and long-term outcomes of behavioral interventions in rural residents, who comprise approximately 30% of the US population, is an important treatment priority.Citation13
The aim of the current study was to examine behavioral factors associated with successful long-term weight maintenance (3.5 years after treatment) among participants who completed an initial six-month lifestyle intervention for obesity delivered in rural settings. Following the intervention, participants were randomized to one of three year-long extended-care conditions (face-to-face counseling, telephone counseling, or mail-only contact) and assessed upon its completion (month 18). In the current study, we assessed participants 3.5 years after completing the initial intervention, and 2.5 years after the conclusion of the extended-care phase (month 48). Specifically, we compared “successful” weight maintainers (participants who lost more than 5% from baseline to long-term follow-up) with “unsuccessful” participants (those who either lost less than 5% or gained weight from baseline to long-term follow-up) with regard to their current use of behavioral weight management strategies, including self-monitoring, goal setting, and physical activity.
Materials and methods
Participants were 234 obese women of mean age 59.3 ± 6.2 (range 50–75) years, with a body mass index ≥30 kg/m2 (mean 36.8 ± 5.0 kg/m2) residing in rural and medically underserved counties who completed the TOURS (Treatment of Obesity in Underserved Rural Settings) study. During the initial six-month intervention, participants took part in 24 weekly group sessions, each lasting approximately 90 minutes. Treatment was delivered via Cooperative Extension Services by personnel with bachelor’s or master’s level education in family and consumer sciences, nutrition, psychology, exercise science, or a related field. The TOURS intervention was modeled in part on the Diabetes Prevention Program and emphasized behavioral skills (eg, goal setting, self-reinforcement, and stimulus control). Dietary goals included a reduction in energy intake by 500–1000 kcal/day (sufficient to produce a weight loss of 1–2 lb per week), reduction in total fats to 25%–30%, and reduction in protein to 15% of total caloric intake. Physical activity goals included the addition of 3000+ steps per day above baseline, or 30 minutes/day of walking, six days/week. Participants were provided with self-monitoring logs and were strongly encouraged to self-monitor their caloric intake and physical activity every day.
Following the initial six-month intervention, participants were randomized to one of three year-long extended-care programs (face-to-face counseling, telephone counseling, or mail-only contact). Participants assigned to the face-to-face counseling program continued to meet at the County Extension off ices for two group sessions per month; participants in the telephone counseling condition had two 10–15-minute telephone contacts with the interventionist per month; and participants assigned to the mail condition received biweekly newsletters containing information related to weight management. The treatment objectives for the extended-care phase included the maintenance of healthy eating behaviors and physical activity levels achieved during the initial intervention and continued reinforcement of behavioral weight management skills. A detailed description of the TOURS intervention has been published previously.Citation14
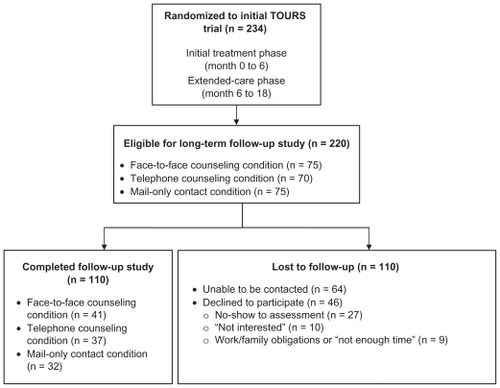
The original TOURS study ended after the year-long extended-care phase (month 6 to month 18) and participants received no treatment or contact from their interventionists from month 18 to month 48 (when the current follow-up assessment was conducted). Only participants who completed the initial six-month intervention and all three original study assessments at months 0, 6, and 18 (n = 220) were eligible for the current study assessment 3.5 years later (month 48). Participant flow throughout the trial is shown in . Participants’ weight and current use of weight management skills were assessed during a group assessment session held at their local Cooperative Extension office. Individuals wishing to partake in the study but unable to attend the group follow-up assessment had the opportunity to schedule an individual session at their convenience.
Figure 1 Flow diagram of participant involvement in follow-up study.
Body weight
Body weight, measured to the nearest 0.1 kg using a certified balanced beam scale, was the primary outcome of the current study. Participants were weighed during the initial intervention at months 0 and 6, following completion of extended-care at month 18, and again for the current study 3.5 years after treatment (month 48).
Behavioral weight management skills
Use of behavioral self-management skills relevant to weight loss were examined via the Weight Management Questionnaire, a 36-item measure that assessed adherence to changes in eating and exercise behaviors in the past month (Part I) and in the period since the weight management program ended (Part II) on a 1–6-point Likert-type scale. A similar measure was used in a previous weight maintenance study by Perri et al.Citation15 The Weight Management Questionnaire asked participants to rate their degree of adherence to key behavioral strategies for weight management and included questions related to self-weighing, self-monitoring (eg, “How often in the past month have you kept a food record of what you eat?” and “How often have you written down the number of minutes you’ve exercised?”), goal setting (eg, “How often have you kept a goal for the amount of calories you eat per day?” and “How often have you kept a goal for the grams of fat you eat per day?”), and stimulus control (eg, “How often have you tried to limit eating out at restaurants?” and “How often have you tried to avoid doing other activities such as watching TV while eating?”). Part II of the measure was divided into five subscales, ie, Record Keeping, Stimulus Control, Goal Setting, Planning Meals, and Mindful Eating. The Weight Management Questionnaire has demonstrated good internal reliability, α = 0.878 for the overall measure, α = 0.872 for Part I, and α = 0.870 for Part II.
Statistical analysis
For our preliminary analyses, Chi-square tests and t-tests were used to determine if there were any differences between participants who chose to take part in the current follow-up study and those who were eligible but did not participate. Repeated-measures analysis of variance were done to compare weight maintenance at month 48 among participants in the three extended-care conditions. A one-way analysis of variance was used to investigate the impact of the extended-care condition on maintenance at month 48. The t-tests were used to compare “successful” weight maintainers (those who maintained a body weight reduction ≥5% from baseline to month 48) and “unsuccessful” participants (those who maintained a body weight change <5% of baseline or gained weight) on Weight Management Questionnaire Part II subscales and individual items of the Weight Management Questionnaire from Part I. Participants who gained weight (n = 37) and those who lost <5% of their body weight (n = 27) were combined into one group, given that there were no significant differences in these subsets of participants with respect to frequency of weight maintenance behaviors.
Results
Participants
The participants were 110 women with a mean (± standard deviation) age of 60.08 ± 6.17 years and mean body mass index of 36.76 ± 5.10 kg/m2. The sample was comprised of Caucasian (79.1%), African-American (18.2%), and Hispanic/Latino (2.7%) participants. There were no significant differences between participants who did complete the study compared with those who did not with respect to age, ethnicity, education, baseline weight, or weight change during the initial or extended-care phases of the intervention (all Ps > 0.05).
Long-term weight maintenance
The 110 participants who completed the follow-up study had mean body weight reductions of 10.17% ± 5.0% during the initial six-month intervention. Participants regained a mean 1.73 ± 6.03 kg from month 6 to month 18, and regained an additional 4.10 ± 7.74 kg from month 18 to month 48 (a 6.95% ± 9.44% increase in body weight from month 6 to month 48). On average, participants maintained 4.08% body weight reductions from month 0 to month 48. Using ≥5% as a cutoff for successful maintenance, we found that 41.80% (n = 46) were able to maintain weight losses of 5% or greater from baseline to month 48.
Participants from each of the extended-care programs (face-to-face counseling condition [n = 41], telephone counseling condition [n = 37], and mail-only contact condition [n = 32]) were represented in the follow-up study. There were no significant differences in weight maintenance at month 48 among participants in the three extended-care conditions (P = 0.932, η2 = 0.001) or among participants in the active (face-to-face counseling and telephone counseling) versus the control (mail-only contact) extended-care conditions (P = 0.709, η2 = 0.001).
After identifying the participants who were successful at long-term weight maintenance, we next investigated what behaviors these individuals were engaging in compared with those who were unsuccessful. In the total period (3.5 years) since the end of the weight management program, successful participants (n = 46) reported engaging in Record Keeping (t[107], = 2.77, P = 0.007) and regular Self-Weighing (t[107] = 3.27, P = 0.001) with a significantly greater frequency than unsuccessful participants (n = 64). However, there were no significant differences between successful and unsuccessful participants with respect to the Stimulus Control (P = 0.107), Planning Meals (P = 0.232), or Mindful Eating (P = 0.193) subscales of the Weight Management Questionnaire. Differences between successful and unsuccessful participants on the Goal Setting subscale (P = 0.052) approached significance.
As shown in , examination of individual items from Part I of the Weight Management Questionnaire indicated that successful participants engaged in select behavioral strategies with greater frequency than unsuccessful participants in the past month, including self-monitoring of weight, food intake, and caloric intake, planning meals ahead of time, and choosing lower calorie options of particular foods (all Ps < 0.05). Differences between successful and unsuccessful participants with respect to self-monitoring of physical activity (minutes) approached significance (P = 0.059). There were no significant differences between successful and unsuccessful participants in terms of slowing the pace of eating, setting a goal for fruit and vegetable consumption, fat grams, or calories, increasing the intake of whole grains, avoiding eating in restaurants, eating breakfast, wearing a pedometer, avoiding eating while doing other activities (for example, watching television), eating smaller portions, avoiding eating late at night, or avoiding snack foods.
Table 1 Use of weight management strategies in past month among successful versus unsuccessful participants
Discussion
To our knowledge, this is the first study to examine successful long-term weight maintenance within a medically underserved rural population of older adults. The results indicate that participants achieved a mean 4.08% body weight reduction from month 0 to month 48, and 41.8% of individuals were able to maintain weight losses of at least 5% at follow-up. Weight changes of this magnitude are potentially sufficient to improve health and lower the risk of chronic disease, and compare favorably with results of previous studies assessing long-term weight maintenance.Citation1
Successful participants reported engaging in select behavioral self-management techniques at follow-up (self-monitoring of weight, intake, and calories, planning meals ahead of time, and choosing lower-calorie food options), with significantly greater frequency during the previous month than unsuccessful participants. Self-monitoring of physical activity approached significance. These results highlight the importance of self-monitoring (of weight, caloric intake, and physical activity) as an essential tool for weight loss and long-term maintenance, a conceptualization supported by an extensive body of research which suggests that self-monitoring is the core component of behavioral treatment.Citation16 The implications of these findings are two-fold, ie, participants should be encouraged to self-monitor their intake as often as possible, and interventionists should immediately address any obstacles to adherence, both to enhance weight loss in the short-term and establish a pattern of consistent self-monitoring that will ideally be sustained over time.
However, less is known about the specific degree of self-monitoring necessary to sustain treatment-induced weight losses. Successful participants consistently engaged in multiple forms of self-monitoring with greater frequency in the past month than unsuccessful participants, including self-weighing (10.76 versus 6.24 times), keeping a food record (7.09 versus 2.67 days), and self-monitoring their calories (5.04 versus 1.67 days). While this pattern of findings supports a “more is better” approach, the optimal frequency and comprehensiveness of self-monitoring necessary to achieve long-term weight maintenance remains unknown. For example, little is known about the impact of simplified methods of self-monitoring on long-term weight loss outcomes. Given that it is unlikely participants will continue to self-monitor indefinitely (particularly with respect to food intake), providing individuals with innovative and convenient tools to improve their adherence to self-monitoring in the long term is critical.Citation17
The role of frequent self-weighing has received considerable research attention in recent years.Citation18,Citation19 Although behavioral interventions typically advise weekly self-monitoring of weight, successful maintainers in the current study reported weighing themselves more regularly (an average of 2.69 times per week in the past month). Daily self-weighing provides individuals with regular, concrete feedback regarding their progress and ideally prompts corrective action. Recognizing small weight gains early on is key, given that small gains typically lead to larger ones.Citation4 Although regular self-weighing was associated with improved outcomes in the current study, its appropriateness as a treatment recommendation for all populations warrants further exploration.
Collectively, the findings from the current study and others suggest that certain key behaviors (self-monitoring of weight, food intake, and calories) are associated with successful weight maintenance, and that failure to sustain these behavioral changes likely contributes to weight regain.Citation20 Learning theory perspectives provide a useful framework from which to interpret these findings in relation to long-term weight maintenance.Citation21 The failure of some participants to maintain their treatment-induced weight losses may be due in part to the return of “old learning” (unhealthy eating habits and sedentary behavior) which resurfaces once the context under which new learning occurred is no longer in place (the weight management program). Discouraged by the realization that weight maintenance demands a high degree of vigilance, and faced with maintaining newly learned behaviors without the social support and built-in accountability of a weight management program, some participants may fail to adhere to their weight loss strategies.
It may be that successful weight maintainers prevent their “old learning” from returning once a weight loss program ends by utilizing self-monitoring as a cue, which heightens awareness of behavior and provides the opportunity for self-reinforcement. This theory would suggest that a “continuous care” approach involving periodic contact with a treatment provider is warranted.Citation22 However, the difficulty in developing a “continuous care” approach lies in adherence, since attendance at face-to-face sessions in multi-year programs diminishes over time and sustaining long-term interventions is costly. To this end, several recent maintenance trials have explored the effectiveness of telephone and Internet-based technologies which have the potential for wide dissemination at relatively low cost.Citation5,Citation6
There are some limitations to the current study. First, the percentage of eligible TOURS participants who completed the follow-up study was relatively low (50%). Of note, the majority of participants who did not complete the follow-up study were not able to be contacted by our staff (n = 64) and did not specifically decline to participate. Given that the original TOURS study was not designed with this multi-year follow-up assessment in mind, we were reliant upon the limited contact information collected at the month 18 assessment to locate participants. It is worth noting that this rate of participation (50%) is comparable with that of other long-term studies with 3–4-year follow-up. For example, in two recent studies with a similar follow-up time frame, the average attrition rates were 51.8% and 53.0%, respectively.Citation23,Citation24 Thus, this limitation is not unique to our study and is a common problem in long-term follow-up of behavioral interventions.
It is important to assess, to the extent possible, whether these findings are representative of all TOURS participants or reflect only the subset of participants who chose to complete the study. In order to examine this issue, comparisons of subjects who participated versus those who did not participate were conducted, examining a multitude of demographic and behavioral factors. Although no significant differences were detected, the possibility remains that the participants who completed the follow-up assessment may have been more successful at maintaining their weight losses, and that social desirability factors may have prevented some participants from completing the study. Additional limitations include the self-report nature of the follow-up assessment battery (which may be influenced by participants’ perceived performance in the intervention) and the possibility that factors not included in our assessment (for example, motivational factors, self-efficacy) may also play a role in long-term weight maintenance. Finally, further work is necessary in order to validate the Weight Management Questionnaire.
This investigation has a number of strengths. Although the prevalence of obesity and cardiovascular disease is significantly higher in rural than in urban communities, to our knowledge this study is the first to examine the behavioral strategies associated with successful long-term weight maintenance among older adults from medically underserved rural areas. Further, many long-term weight maintenance studies involve interventions with continued treatment until final follow-up; in contrast, the current study assessed participants 3.5 years following the cessation of initial treatment and assessed weight at multiple time points.Citation2 Finally, this study is one of few investigations overall to involve a multiple-year follow-up after initial behavioral weight loss treatment.
Collectively, our findings suggest that a substantial proportion of individuals are able to maintain clinically significant weight losses multiple years post-treatment. Self-monitoring (of weight, intake, and calories) appears to be a key component to successful long-term weight loss maintenance among rural populations of older adults, who exhibit higher rates of obesity and chronic disease than their urban counterparts. Future community-based research initiatives should target ways to enhance adherence to long-term self-monitoring in this population, ideally via technologies which have the potential for wide dissemination.
Acknowledgments
Funding for this study was provided in part by grant R18HL73526 from the National Heart, Lung and Blood Institute. Publication of this article was funded in part by the University of Florida Open-Access Publishing Fund.
Disclosure
The authors report no conflicts of interest in this work.
References
- Institute of MedicineWeighing the Options: Criteria for Evaluating Weight-Management ProgramsWashington, DCNational Academy Press1995
- PerriMGForeytJPAntonSDPrevention of weight regain after weight lossBrayGABouchardCHandbook of Obesity Treatment: Clinical Applications3rd edNew York, NYInforma Healthcare2008
- KlemMLWingRRMcGuireMTSeagleHMHillJOA descriptive study of individuals successful at long-term maintenance of substantial weight lossAm J Clin Nutr199767946
- WingRRPhelanSLong-term weight loss maintenanceAm J Clin Nutr20052222S225S16002825
- SvetkyLPStevensVJBrantleyPJComparison of strategies for sustaining weight loss: The Weight Loss Maintenance randomized controlled trialJAMA20082991139114818334689
- WingRRTateDFGorinAARaynorHAFavaJLA self-regulation program for maintenance of weight lossN Engl J Med20063551563157117035649
- JacksonJEDoescherMPJerantAFHartLGNational study of obesity prevalence and trends by type of rural countyJ Rural Health20052114014815859051
- EberhardtMIngramDMakucDUrban and Rural Health Chartbook. Health, United StatesHyattsville, MDNational Center for Health Statistics2001
- RobertsAAshleyGWhat are the characteristics of overweight and obese patients who achieve weight loss and what factors are most helpful: A quantitative and qualitative study of patients and interventions in a rural general practiceJ Hum Nutr Diet1999122027
- StampsPLCatinoDCFeolaACTreatment of obesity in three rural primary care practicesJ Fam Pract1983176296346619748
- Mayer-DavisEJD’AntonioAMSmithSMPounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communitiesAm J Public Health2004941736174215451743
- WingRRBehavioral weight controlWaddenTAStunkardAJHandbook of Obesity TreatmentNew York, NYGuilford Press2002
- United States Census Bureau2010American Community Survey 1-year estimates. B01003. Total population – universe: Total population Available from: http://quickfacts.census.gov/qfd/states/12/12107.htmlAccessed August 8, 2011
- PerriMGLimacherMCDurningPEExtended-care programs for weight management in rural communities: The Treatment of Obesity in Underserved Rural Settings (TOURS) randomized trialArch Intern Med20081682347235419029500
- PerriMGNezuAMMcKelveyWFShermerRLRenjilianDAViegenerBJRelapse prevention training and problem-solving therapy in the long-term management of obesityJ Consult Clin Psychol20016972272611550740
- BakerRCKirschenbaumDSSelf-monitoring may be necessary for successful weight controlBehav Ther199324377394
- YonBAJohnsonRKHarvey-BerinoLGoldBCHowardABPersonal digital assistants are comparable to traditional diaries for dietary self-monitoring during a weight loss programJ Behav Med20073016517517216341
- LevitskyDAGarayJNausbaumMNeighborsLDellavalleDMMonitoring weight daily blocks the freshman weight gain: A model for combating the epidemic of obesityInt J Obesity20063010031010
- LindeJAJefferyRWFrenchSAPronkNPBoyleRGSelf-weighing in weight gain prevention and weight loss trialsAnn Behav Med20053021021616336072
- McGuireMTWingRRKlemMLLangWHillJOWhat predicts weight regain among a group of successful losersJ Consult Clin Psychol19996717718510224727
- BoutonMEA learning theory perspective on lapse, relapse, and the maintenance of behavior changeHealth Psychol200219576310709948
- PerriMGNezuAMViegenerBJImproving the long-term management of obesity: theory, research and clinical guidelinesNew YorkWiley1992
- LantzHPeltonenMAgrenLTorgersonJSA dietary and behavioural programme for the treatment of obesity: A 4-year clinical trial and a long-term post-treatment follow-upJ Intern Med200325427227912930237
- MelinIReynisdottirSBerglundLZamfirMKarlstromBConservative treatment of obesity in an academic obesity unit: Long-term outcome and drop-outEat Weight Disord200611223016801742