Abstract
Purpose
To investigate the effectiveness of dysphagia screening and subsequent swallowing rehabilitation in elderly stroke patients with malnutrition risk.
Patients and Methods
Based on the Chinese Stroke Center Alliance (CSCA) from August 1, 2015 to July 21, 2019, we compared the in-hospital adverse outcomes among stroke patients (including ischemic stroke, intracranial hemorrhage, and subarachnoid hemorrhage) over 70 years old with and without dysphagia screening. The primary outcome was in-hospital all-cause mortality. Secondary outcomes were the composite endpoint of discharge against medical advice (DAMA) or in-hospital death.
Results
Among 365,530 stroke patients ≥ 70 years old with malnutrition risk in the CSCA, documented dysphagia screening was performed for 288,764 (79.0%) participants. Of these, 41,482 (14.37%) patients had dysphagia, and 33,548 (80.87%) patients received swallowing rehabilitation. A total of 1,694 (0.46%) patients experienced in-hospital death. After adjustment for traditional risk factors, dysphagia screening was associated with a low risk of all-cause mortality in stroke patients [adjusted odds ratio (aOR): 0.75, 95% confidence interval (CI):0.65–0.87]. Compared to patients with dysphagia who did not receive swallowing rehabilitation, patients reveiving swallowing rehabilitation had a reduced risk of in-hospital death (aOR:0.39, 95% CI: 0.33–0.46). Additionally, dysphagia screening had a lower risk for the composite endpoint of DAMA or in-hospital death (aOR:0.83,95% CI: 0.80–0.87), as did subsequent swallowing rehabilitation (aOR:0.43,95% CI: 0.40–0.47). Similar results were observed in the sensitivity analysis through inverse probability of treatment weighting, propensity score matching, and excluding patients without National Institutes of Health Stroke Scale scores. A similar association was observed between dysphagia management and adverse clinical outcomes in ischemic stroke and intracranial hemorrhage patients.
Conclusion
Dysphagia screening and swallowing rehabilitation were associated with a reduced risk of in-hospital death and composite outcome of DAMA or in-hospital death for stroke patients with malnutrition risk. Future research should concentrate on improving the quality of medical care for dysphagia management to improve patients’ outcomes.
Introduction
China faces a great burden due to stroke. The mortality of cerebrovascular diseases in China was 149.49 per 100,000 in 2018.Citation1 Dysphagia is common among stroke survivors, affecting 27–64% of patients,Citation2,Citation3 while affecting 25–81% of survivors 70 years or older.Citation4 Dysphagia can increase the risk of malnutrition, mortality, and hospitalization complications.Citation2,Citation3,Citation5,Citation6 Dysphagia is a significant risk factor for malnutrition in stroke patients older than 70 years.Citation3,Citation6,Citation7 The nutrition screening 2002 (NRS2002) is recommended for hospital patients by the European Society of Parenteral and Enteral Nutrition (ESPEN)Citation8 and is suitable in screening malnutrition risk among Chinese geriatric inpatients older than 70 years.Citation9 According to NRS2002, stroke patients older than 70 years are defined as being at malnutrition risk.Citation8 Positive outcomes, including lower mortality, complications, and health-care costs, are common among hospitalized, older adult patients receiving enteral or oral nutrition.Citation10–Citation12 The prevalence of malnutrition risk assessed by NRS2002 among patients with acute ischemic stroke (AIS) at admission is approximately 45%.Citation13–Citation15 NRS2002 has a higher predictive power and can predict both short- and long-term outcomes for stroke patients.Citation13,Citation14 Dysphagia and malnutrition influence each other and are associated with adverse outcomes (ie, pneumonia, all-cause mortality).Citation2,Citation4,Citation15,Citation16 Therefore, increased attention should be paid to older adult stroke patients who are at malnutrition risk.
Multiple guidelines recommend early dysphagia screening before oral food or tablets given for stroke patients.Citation17–Citation20 Doctors and nurses can use some screening methods to diagnose the risk of dysphagia, such as the medical history, questionnaires, and swallowing tests.Citation4 The 10 mL water swallowing test and the Gugging Swallowing Screen (GUSS) can provide information regarding dysphagia to predict poor outcomes, including pneumonia, in-hospital death, and 3-month disability.Citation21 However, a systematic review revealed that there was insufficient randomized controlled trial (RCT) data to determine whether dysphagia screening can reduce poor outcomes.Citation22
Additionally, a meta-analysis demonstrated that swallowing therapy had no effect on case fatality but reduced the incidence of pneumonia.Citation2 However, other studies found that early dysphagia screening and intervention could reduce in-hospital death or hospital-associated pneumonia.Citation23,Citation24 Although guidelines strongly recommend dysphagia screening prior to oral food or medications, clinical evidence remains insufficient,Citation2,Citation22,Citation25 especially for older stroke patients who are at malnutrition risk.
Therefore, we evaluated the effectiveness of dysphagia screening and subsequent swallowing rehabilitation among older adults with stroke [including AIS, intracerebral hemorrhage (ICH), or subarachnoid hemorrhage (SAH)] based on the Chinese Stroke Center Alliance (CSCA).
Materials and Methods
Study Design
The study was based on the data derived from the CSCA and enrolled 1,006,798 patients with acute stroke/ transient ischemic attacks (TIA) from August 1, 2015, to July 21, 2019.Citation26,Citation27 The CSCA program was designed to develop stroke centers and treat patients in a manner consistent with accepted national guidelines. Patients aged ≥18 years and within 7 days of symptom onset were enrolled in the program. The CSCA was approved by the ethics committee of Beijing Tiantan Hospital (KY 2018–061-02). The study protocol conforms to the ethical guidelines of the Declaration of Helsinki. The data were collected and managed via a web-based tool. Participating hospitals in the CSCA collected data without the individual information and exemption from their Institutional Review Board.Citation26
Study Population
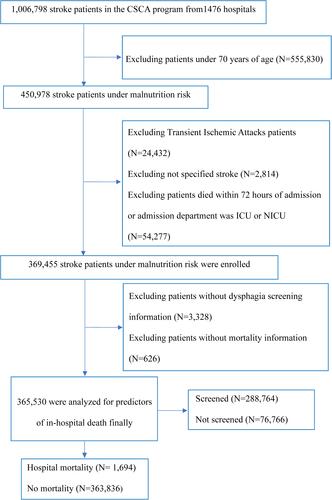
NRS2002 involves three factors: age, disease severity, and nutritional impairment. The NRS2002 score of participants with stroke and age ≥ 70 were assessed for 2 and 1, respectively. Patients with a score of NRS2002 ≥ 3 were at malnutrition risk. The present study included stroke patients ≥ 70 years old from the CSCA who were at risk of malnutrition based on the NRS2002.Citation8 Patients were excluded if they met the following criterion: diagnosed with TIA and unspecified stroke, stroke patients aged ≤ 70 years, patients who died within 72 hours, admission department was intensive care unit (ICU) or neurological intensive care unit (NICU), and missing data for dysphagia screening or mortality. Finally, a total of 365,530 stroke patients under malnutrition risk were included for analyses ().
Variables and Outcomes
Data were collected via the web-based patient data collection and management tool (Medicine Innovation Research Center, Beijing, China). Data were collected for patient demographics, insurance status, medical history, National Institutes of Health Stroke Scale (NIHSS) score on admission, and the hospital characteristics (geographic region, hospital grade). The body mass index (BMI) was calculated as weight [kg] divided by height squared [m2]. Dysphagia screening was defined as the patient's swallowing function as assessed by medical care personnel before any oral intake during hospitalization. The dysphagia screening tool following clinical guidelines mainly included the 10 mL water swallowing test, GUSS, acute stroke dysphagia screen, Eating Assessment Tool-10, Clinical Swallowing Function Assessment Form, and so on.Citation17–Citation20 Swallowing rehabilitation was provided by a professional physiatrician for swallowing function according to the condition of the patients. The manner of swallowing rehabilitation included acupuncture treatment, medication, neuromuscular electrical stimulation, pharyngeal electrical stimulation, transcranial direct current stimulation, etc.Citation26,Citation27
The primary outcome was in-hospital all-cause mortality. Secondary outcomes were the composite outcomes including death and discharge against medical advice (DAMA), and hospital-associated pneumonia. DAMA was defined as a patient leaving the hospital against the advice of their care provider. Hospital-associated pneumonia was diagnosed by the clinician through clinical symptoms, physical examination, and radiological or etiological evidence.Citation26,Citation27
Statistical Analysis
Continuous variables were described as mean ± standard deviation or median and interquartile range (IQR). Categorical variables were presented as absolute numbers with percentages. We compared the differences in the baseline characteristics between patients with and without dysphagia screening using the standardized difference. An absolute standardized difference (ASD) of >10% indicated significant differences in the variable between the two groups.Citation28
Multivariable logistic regression models were performed to determine the risk of dysphagia screening or swallowing rehabilitation for poor outcomes among stroke patients as odds ratios (OR) and 95% confidence intervals (CI). The age,; sex; initial NIHSS score; BMI; medical history, including stroke, hypertension, diabetes mellitus, coronary heart disease/myocardial infarction, dementia, heart failure, and atrial fibrillation; current smoking; alcoholism; medication history; and the hospital characteristics (geographic region, hospital grade) were adjusted in the multivariable models.
In the sensitivity analysis, the associations were further assessed using the inverse probability of treatment weighting and greedy, nearest-neighbor propensity score matching (PSM). Inverse probability of treatment weighting estimation was then defined as the inverse of the estimated propensity score for patients with dysphagia screening and the inverse of one minus the estimated propensity score for those without dysphagia screening.Citation29 Propensity scores were calculated for each patient based on a multivariable logistic regression model. This model included demographic variables (age, sex); inpatients’ medical insurance; stroke severity (NIHSS score) at admission; history of stroke, hypertension, diabetes mellitus, dyslipidemia, coronary heart disease/ myocardial infarction, dementia, heart failure, atrial fibrillation, carotid stenosis; current smoking, alcoholism; medication history of antiplatelet drugs, anticoagulant drugs, antihypertensive drugs, lipid-lowering drugs; and the hospital characteristics (geographic region, hospital grade). We also matched patients without and with dysphagia screening in a 1:4 ratio using the greedy, nearest-neighbor method without replacement, with a caliper of 0.01 of the propensity score.Citation30 Given that there were more missing values in the NIHSS score, we excluded patients without the NIHSS scores in a sensitivity analysis. Additionally, we evaluated the balance of covariates between groups in the matched samples and determined the risk of dysphagia screening or swallowing rehabilitation for the poor outcomes in patients with different types of stroke.
All tests were two-tailed with P-values <0.05 considered as statistically significant. All statistical analyses were performed using SAS version 9.4 statistical software (SAS Institute Inc., Cary, North Carolina, USA).
Results
Baseline Characteristics
According to the NSR2002 criterion, 450,978 (44.79%) stroke patients were ≥ 70 years old. A total of 365,530 patients were ultimately included in the study and 288,764 (79.0%) received dysphagia screening before oral food or tablets given were provided. Before PSM, patients who received dysphagia screening had a higher likelihood of mild to moderate stroke severity and a lower proportion of middle geographic region. There were no significant differences between the two groups in the demographic characteristics or medical history according to ASD. According to the inverse probability of treatment weighting, patients with and without dysphagia screening were similar with respect to age, sex, NIHSS score at admission, previous medical history, medication history, and hospital characteristics. After the greedy, nearest-neighbor PSM, baseline characteristics between 177,433 patients with dysphagia screening and 45,302 patients without dysphagia screening were well balanced ().
Table 1 Baseline Characteristics Before and After Inverse Probability of Treatment Weighted in Stroke Patient (with DS and Without DS)
Primary Outcome: In-hospital Death
A total of 1694 (0.46%) stroke patients died during hospitalization. Patients who died during hospitalization were significantly older and had higher NIHSS scores, and had a higher likelihood of previous medical history and dysphagia, whereas a lower proportion of dysphagia screening and swallowing rehabilitation than survivors (Table S1). After adjusting for age, sex, NIHSS score at admission, BMI, the medical history of stroke/TIA, hypertension, etc. medication history, and the hospital characteristics (grade and region), dysphagia screening was associated with a reduced risk of in-hospital death [adjusted OR (aOR): 0.75, 95% CI:0.65–0.87]. After adjusting for the same confounders, dysphagia was significantly associated with the occurrence of in-hospital death (aOR: 6.13, 95% CI: 5.18–7.27). Older age, severity of stroke (NIHSS score at admission), the medical history of stroke or TIA, diabetes mellitus, coronary heart disease/previous myocardial infarction, atrial fibrillation, heart failure, dementia and tertiary grade hospital were risk factors for all-cause mortality in stroke patients. Meanwhile, the associations were consistent after PSM and inverse probability of treatment weighting estimation ().
Table 2 Multivariable Analysis of Risk Factors Associated with Hospital Mortality in Stroke Patients
Among the 288,764 stroke patients with documented dysphagia screening, 41,482 (14.37%) patients had dysphagia, and 33,548 (80.87%) patients received swallowing rehabilitation (Table S2). Compared to patients with dysphagia but who did not receive swallowing rehabilitation, swallowing rehabilitation significantly reduced the risk of death (aOR: 0.39, 95% CI: 0.33–0.46) ().
Table 3 The Hospital Poor Outcomes in Stroke Patients with and without DS and Swallowing Rehabilitation
Secondary Outcomes: Composite Outcomes and In-hospital Pneumonia
A total of 19,909 (5.45%) deaths and DAMA occurred; the proportion of DAMA patients was 4.98% (18,215), and 51,649 (14.13%) patients were diagnosed with in-hospital pneumonia. After adjusting for the confounders, dysphagia screening prior to oral intake reduced the risk of the composite outcome, including DAMA and death (aOR: 0.83, 95CI: 0.80–0.87). However, dysphagia screening was associated with an increased risk for hospital-associated pneumonia (aOR: 1.54, 95CI: 1.49–1.59). Swallowing rehabilitation also reduced the risk of DAMA and death (aOR: 0.43, 95CI: 0.40–0.47) among stroke patients with dysphagia. Similar results were observed using propensity score approaches with inverse probability of treatment weighting and PSM ().
Sensitivity Analysis and Subgroup Analysis for the Association Between Dysphagia Management and Clinical Outcomes
We performed a sensitivity analysis for dysphagia management and clinical outcomes among stroke patients after excluding patients who lacked NIHSS scores. Dysphagia management including dysphagia screening and swallowing rehabilitation was also associated with a lower risk of in-hospital death and the composite outcome ().
Table 4 Hospital Poor Outcomes in Stroke Patients Excluded Missing of NIHSS Score with and without DS and Swallowing Rehabilitation
In the subgroup analysis, dysphagia screening (aOR: 0.74, 95% CI: 0.63–0.87) and swallowing rehabilitation (aOR: 0.40, 95% CI: 0.33–0.48) were also associated with a reduced risk of all-cause mortality among ischemic stroke patients. We also observed that dysphagia screening (aOR: 0.87, 95% CI: 0.83–0.91) and swallowing rehabilitation (aOR: 0.42, 95% CI: 0.39–0.45) reduced the risk of the composite outcome including DAMA and death for ischemic stroke patients (). A similar relationship was observed for intracranial hemorrhage but not subarachnoid hemorrhage stroke patients (Tables S3 and S4).
Table 5 The Hospital Poor Outcomes in Ischemic Stroke Patients with and without DS and Swallowing Rehabilitation
Discussion
In the present study, we investigated the association between dysphagia management and poor clinical outcomes among stroke patients at malnutrition risk based on the CSCA. For the 365,530 stroke patients enrolled in our study, documented dysphagia screening was performed for 288,764 (79.0%) patients; 41,482 (14.37%) patients had dysphagia, and 33,548 (80.87%) patients received swallowing rehabilitation. We found that the dysphagia status after dysphagia screening was an independent risk factor for in-hospital death. Dysphagia screening performed prior to oral intake and subsequent swallowing rehabilitation could reduce the risk of in-hospital death; and composite poor outcomes, including DAMA and death. Unexpectedly, we found that dysphagia screening and swallowing rehabilitation were associated with a higher likelihood of developing hospital-related pneumonia.
A total of 288,764 (79.0%) patients underwent dysphagia screening in our study, which is similar to that of approximately 80% reported in previous studies.Citation5,Citation31,Citation32 However, the performance of dysphagia screening was higher than that of 69.2% in the HeadPoST program conducted in China from March 2015 to November 2016.Citation31 The GWTG–Stroke program from 2003–2009 reported 68.9% of patients were documented to have been provided dysphagia screening.Citation33 The higher rate of dysphagia screening in our study relative to previous studies could be due to several reasons. The stroke patients enrolled in our study were ≥ 70 years old. Patients who received documented dysphagia screening tended to be older.Citation5,Citation31,Citation34 The older age was significantly associated with dysphagia screening (≥ 80 versus < 60 years, adjusted OR, 1.44; 95% CI: 1.18–1.75).Citation5 Moreover, with multiple national and international guidelines recommending dysphagia screening and management for stroke patients,Citation17–Citation20 clinicians and nurses may pay increased attention to dysphagia screening, especially for older adults or patients at malnutrition risk.Citation4,Citation6 Further, the quality of stroke care in China has improved in overall adherence to guideline-recommended performance measures, including dysphagia screening.Citation32 The patients in our study were from the CSCA program, which was designed to improve stroke care quality and outcomes. The CSCA have been implemented to promote the progress of stroke center construction and the standard of clinical practice in China.Citation26 Therefore, the performance of dysphagia screening in our study may have improved significantly in recent years.Citation27
We observed that dysphagia screening could reduce the risk of adverse in-hospital outcomes. Similar to our results, a cluster RCT revealed that stroke care pathways consisting of dysphagia screening could reduce the risk of all-cause mortality at 90-days (adjusted OR: 0.33; 95% CI: 0.12–0.90).Citation35 Early dysphagia screening and intervention could reduce hospital-associated death or pneumonia in some studies.Citation23,Citation24 Additionally, in the Quality in Acute Stroke Care (QASC) study, patients who received intervention for acute stroke (ie, fever, sugar, and swallowing management) were significantly less likely to be dependent or die (mRS ≥2) at 90 days than patients in the control group [236 (42%) vs 259 (58%), P=0.002], but this was not the case for all-cause mortality [21 (3.7%) vs 24 (5.3%), P=0.36].Citation36 Unexpectedly, we observed that dysphagia screening was associated with an increased risk of pneumonia. The GWTG–Stroke program also reported that dysphagia screening was associated with a higher OR for pneumonia.Citation33 However, we suggest that the causal relationships may be reversed. Firstly, stroke patients at higher risk of pneumonia may be more likely to receive dysphagia screening in clinical practice. Furthermore, patients with documented dysphagia screening were more likely to have a medical history (ie, atrial fibrillation, current smoking) that could increase the risk of pneumonia.Citation37 Meanwhile, our results demonstrate that the dysphagia status as a result of the dysphagia screening was also associated with a higher risk of in-hospital death (adjusted OR: 6.13, 95% CI: 5.18–7.27), which is consistent with other studies.Citation5,Citation23,Citation31
In the present study, we observed that subsequent swallowing rehabilitation had beneficial effects on all-cause mortality for patients with stroke (adjusted OR: 0.39, 95% CI: 0.33–0.46), AIS (adjusted OR: 0.40, 95% CI: 0.33–0.48) and intracranial hemorrhage (adjusted OR: 0.28, 95% CI: 0.20–0.39). Compared with conventional discharge, DAMA was likely to increase the risk of hospital readmission, and mortality.Citation38,Citation39 Swallowing rehabilitation also significantly decreased the risk of composite outcomes, including in-hospital death and DAMA in our study. Some meta-analyses showed that acupuncture may have beneficial effects on swallowing function and dependency, but no data were reported for mortality.Citation40,Citation41 However, another meta-analysis revealed that swallowing therapy did not affect case fatality (OR: 1.00, 95% CI: 0.66–1.52), but could reduce the incidence of pneumonia (OR: 0.36, 95% CI: 0.16–0.78).Citation2 Swallowing rehabilitation may decrease the risk of adverse outcomes, but the association was significant, such that we consider it may be overstating the effect. Firstly, the socioeconomic status and compliance of patients in undertaking swallowing rehabilitation may have been superior and, hence, improved treatment outcomes.Citation42 Further, the hospitals that provided swallowing rehabilitation may have adhered to evidence-based performance measures and improved multifaceted intervention quality, including intravenous recombinant tissue plasminogen activator (rt-PA), deep venous thrombosis prophylaxis, evidence-based medications after admission, and dysphagia management that prevented and reduced in-hospital and long-term mortality.Citation43
Dysphagia interventions involve behavioral therapy and rehabilitative methods, and behavioral approaches include modification of fluid and food consistencies.Citation4 Some high-quality RCTs report that dietary adjustments or nutritional support could reduce the risk of death. The FOOD trials showed that a supplemented diet reduced the absolute risk of death in stroke patients with dysphagia [7%, 95% CI: −1.4–2.7; P= 0.5)].Citation44 The Effect of early nutritional support on Frailty, Functional Outcomes, and Recovery of malnourished medical inpatients Trial revealed that assessing patients by NRS2002 could decrease the risk of a composite adverse clinical outcome defined as all-cause mortality, admission to intensive care, non-elective hospital readmission, major complications, and decline in functional status at 30 days (HR: 0.81, 95% CI: 0.68–0.97) and all-cause mortality (HR: 0.65, 95% CI: 0.48–0.88) within 30 days.Citation45 The abovementioned findings indicate the importance of performing dysphagia screening and management to reduce the risk of adverse outcomes, especially for stroke patients who are older or at malnutrition risk.
We acknowledge several limitations in our study. Firstly, there may have been heterogeneity in the type of dysphagia screening or swallowing rehabilitation among the multicenter hospitals. The detailed information was not collected on the heterogeneity for further analysis. Secondly, there may have been selection bias, as our study patients with stroke at malnutrition risk were screened based on age (≥ 70 years old), which meets two items of malnutrition risk defined by NRS-2002. Therefore, some patients who were < 70 years old but might be screened as at malnutrition risk according to other items in the NRS-2002 were not included in our study. However, several previous studies reported that the average age of stroke patients at malnutrition risk was ≥ 70 years.Citation13,Citation46 Positive outcomes were more likely among older patients ≥ 70 years old who received nutritional support.Citation10–Citation12 Therefore, we focused on this segment of patients at malnutrition risk in our study. Hence, caution should be taken when generalizing the findings to other populations at malnutrition risk. A major strength of our study is the large sample size of stroke patients at malnutrition risk from multicenter, and the main purpose was to provide evidence for reducing poor outcomes through dysphagia management among specific patients, specifically, older adults. In addition, the primary endpoint included in-hospital death and complication but not outcomes after discharge. Finally, some other potential confounding factors (ie, modified Rankin score at admission, activities of daily living) may have influenced the results. However, the quality of these related variables was not sufficient for inclusion in the analysis in our study. Further studies are needed to validate that dysphagia screening may reduce the risk of short- and long-term adverse outcomes and investigate its effect in a larger scope of populations at malnutrition risk.
Conclusion
Dysphagia screening and swallowing rehabilitation were associated with reducing the risk of death and the composite outcome of DAMA and in-hospital death among stroke patients. Future research should concentrate on improving the quality of medical care for dysphagia management to improve patients’ outcomes.
Abbreviations
AIS, acute ischemic stroke; ASD, absolute standardized difference; CI, confidence interval; CSCA, Chinese Stroke Center Alliance; DAMA, discharge against medical advice; IPTW, inverse probability of treatment weight; IQR, interquartile range; NIHSS, National Institutes of Health Stroke Scale; NRS 2002, nutrition screening 2002; PSM, propensity score matching; TIA, transient ischemic attacks.
Data Sharing Statement
The data are available to researchers on reasonable request for purpose of reproducing the results or replicating the procedure from the corresponding author.
Ethics Approval and Consent to Participate
The CSCA was approved by the ethics committee of Beijing Tiantan Hospital (KY 2018-061-02). The study protocol conforms to the ethical guidelines of the Declaration of Helsinki. The data was collected and managed via the web-based tool. Participating hospitals in CSCA collected data without the individual information and exemption from their Institutional Review Board.
Acknowledgments
We thank the CSCA collaborating centers, members, and volunteers for their hard work and efforts. We thank every participant who has contributed important and invaluable data to CSCA. We thank Prof. Haiqiang Qin for his constructive suggestions in revising the manuscript. We would like to thank Editage (www.editage.cn) for English language editing.
Disclosure
The authors report no conflicts of interest in this work.
Additional information
Funding
References
- Wang YJ, Li ZX, Gu HQ, et al. China Stroke Statistics 2019: a Report From the National Center for Healthcare Quality Management in Neurological Diseases, China National Clinical Research Center for Neurological Diseases, the Chinese Stroke Association, National Center for Chronic and Non-communicable Disease Control and Prevention, Chinese Center for Disease Control and Prevention and Institute for Global Neuroscience and Stroke Collaborations. Stroke Vasc Neurol. 2020;5(3):211–239. 10.1136/svn-2020-000457
- Bath PM, Lee HS, Everton LF Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10:CD000323. 10.1002/14651858.CD000323.pub3
- Zhang M, Li C, Zhang F, et al. Prevalence of Dysphagia in China: an epidemiological survey of 5943 participants. Dysphagia. 2020;36:339–350. 10.1007/s00455-020-10138-7
- Ortega O, Martin A, Clave P. Diagnosis and management of oropharyngeal dysphagia among older persons, state of the art. J Am Med Dir Assoc. 2017;18(7):576–582. 10.1016/j.jamda.2017.02.015
- Joundi RA, Martino R, Saposnik G, Giannakeas V, Fang J, Kapral MK Predictors and outcomes of dysphagia screening after acute ischemic stroke. Stroke. 2017;48(4):900–906. 10.1161/STROKEAHA.116.015332
- Blanar V, Hodl M, Lohrmann C, Amir Y, Eglseer D Dysphagia and factors associated with malnutrition risk: a 5-year multicentre study. J Adv Nurs. 2019;75(12):3566–3576. 10.1111/jan.14188
- Wang J, Luo B, Xie Y, Hu HY, Feng L, Li ZN Evaluation methods on the nutritional status of stroke patients. Eur Rev Med Pharmacol Sci. 2014;18(24):3902–3907.
- Kondrup J, Allison SP, Elia M, et al. ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–421. 10.1016/S0261-5614(03)00098-0
- Miao J-P, Quan X-Q, Zhang C-T, et al. Comparison of two malnutrition risk screening tools with nutritional biochemical parameters, BMI and length of stay in Chinese geriatric inpatients: a multicenter, cross-sectional study. BMJ Open. 2019;9(2):e022993. 10.1136/bmjopen-2018-022993
- Kondrup J Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–336. 10.1016/S0261-5614(02)00214-5
- Bouillanne O, Curis E, Hamon-Vilcot B, et al. Impact of protein pulse feeding on lean mass in malnourished and at-risk hospitalized elderly patients: a randomized controlled trial. Clin Nutr. 2013;32(2):186–192. 10.1016/j.clnu.2012.08.015
- Seguy D, Hubert H, Robert J, Meunier JP, Guerin O, Raynaud-Simon A Compliance to oral nutritional supplementation decreases the risk of hospitalisation in malnourished older adults without extra health care cost: prospective observational cohort study. Clin Nutr. 2020;39(6):1900–1907. 10.1016/j.clnu.2019.08.005
- Cai ZM, Wu YZ, Chen HM, et al. Being at risk of malnutrition predicts poor outcomes at 3 months in acute ischemic stroke patients. Eur J Clin Nutr. 2020;74(5):796–805. 10.1038/s41430-020-0605-8
- Zhang M, Ye S, Huang X, et al. Comparing the prognostic significance of nutritional screening tools and ESPEN-DCM on 3-month and 12-month outcomes in stroke patients. Clin Nutr. 2020;40(5):3346–3353. 10.1016/j.clnu.2020.11.001
- Aliasghari F, Izadi A, Khalili M, Farhoudi M, Ahmadiyan S, Deljavan R Impact of premorbid malnutrition and dysphagia on ischemic stroke outcome in elderly patients: a Community-Based Study. J Am Coll Nutr. 2019;38(4):318–326. 10.1080/07315724.2018.1510348
- Shimizu A, Maeda K, Koyanagi Y, Kayashita J, Fujishima I, Mori N The global leadership initiative on malnutrition-defined malnutrition predicts prognosis in persons with stroke-related Dysphagia. J Am Med Dir Assoc. 2019;20(12):1628–1633. 10.1016/j.jamda.2019.07.008
- Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019;50(12):e344–e418. 10.1161/STR.0000000000000211
- Burgos R, Breton I, Cereda E, et al. ESPEN guideline clinical nutrition in Neurology. Clin Nutr. 2018;37(1):354–396. 10.1016/j.clnu.2017.09.003
- Hebert D, Lindsay MP, McIntyre A, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11(4):459–484. 10.1177/1747493016643553
- Zhang T, Zhao J, Li X, et al. Chinese Stroke Association guidelines for clinical management of cerebrovascular disorders: executive summary and 2019 update of clinical management of stroke rehabilitation. Stroke Vasc Neurol. 2020;5(3):250–259. 10.1136/svn-2019-000321
- Lopes M, Freitas E, Oliveira M, et al. Impact of the systematic use of the Gugging Swallowing Screen in patients with acute ischaemic stroke. Eur J Neurol. 2019;26(5):722–726. 10.1111/ene.13825
- Smith EE, Kent DM, Bulsara KR, et al. Effect of dysphagia screening strategies on clinical outcomes after stroke: a systematic review for the 2018 guidelines for the early management of patients with acute ischemic stroke. Stroke. 2018;49(3):e123–e128. 10.1161/STR.0000000000000159
- Palli C, Fandler S, Doppelhofer K, et al. Early Dysphagia screening by trained nurses reduces pneumonia rate in stroke patients: a Clinical Intervention Study. Stroke. 2017;48(9):2583–2585. 10.1161/STROKEAHA.117.018157
- Titsworth WL, Abram J, Fullerton A, et al. Prospective quality initiative to maximize dysphagia screening reduces hospital-acquired pneumonia prevalence in patients with stroke. Stroke. 2013;44(11):3154–3160. 10.1161/STROKEAHA.111.000204
- Li Z, Pandian J, Sylaja PN, et al. Quality of care for ischemic stroke in China vs India: findings from national clinical registries. Neurology. 2018;91(14):e1348–e1354. 10.1212/WNL.0000000000006291
- Wang Y, Li Z, Wang Y, et al. Chinese Stroke Center Alliance: a national effort to improve healthcare quality for acute stroke and transient ischaemic attack: rationale, design and preliminary findings. Stroke Vasc Neurol. 2018;3(4):256–262. 10.1136/svn-2018-000154
- Gu HQ, Yang X, Wang CJ, et al. Clinical characteristics, management, and in-hospital outcomes in patients with stroke or transient ischemic attack in China. JAMA Netw Open. 2021;4(8):e2120745. 10.1001/jamanetworkopen.2021.20745
- Austin PC Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. 10.1002/sim.3697
- Brookhart MA, Wyss R, Layton JB, Sturmer T Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes. 2013;6(5):604–611. 10.1161/CIRCOUTCOMES.113.000359
- Benedetto U, Head SJ, Angelini GD, Blackstone EH Statistical primer: propensity score matching and its alternatives. Eur J Cardiothorac Surg. 2018;53(6):1112–1117. 10.1093/ejcts/ezy167
- Ouyang M, Boaden E, Arima H, et al. Dysphagia screening and risks of pneumonia and adverse outcomes after acute stroke: an international multicenter study. Int J Stroke. 2020;15(2):206–215. 10.1177/1747493019858778
- Li Z, Wang C, Zhao X, et al. Substantial progress yet significant opportunity for improvement in stroke care in China. Stroke. 2016;47(11):2843–2849. 10.1161/STROKEAHA.116.014143
- Masrur S, Smith EE, Saver JL, et al. Dysphagia screening and hospital-acquired pneumonia in patients with acute ischemic stroke: findings from Get with the Guidelines–Stroke. J Stroke Cerebrovasc Dis. 2013;22(8):e301–309. 10.1016/j.jstrokecerebrovasdis.2012.11.013
- Teuschl Y, Trapl M, Ratajczak P, Matz K, Dachenhausen A, Brainin M Systematic dysphagia screening and dietary modifications to reduce stroke-associated pneumonia rates in a stroke-unit. PLoS One. 2018;13(2):e0192142. 10.1371/journal.pone.0192142
- Rai N, Prasad K, Bhatia R, et al. Development and implementation of acute stroke care pathway in a tertiary care hospital in India: a cluster-randomized study. Neurol India. 2016;64 Suppl:S39–45. 10.4103/0028-3886.178038
- Middleton S, McElduff P, Ward J, et al. Implementation of evidence-based treatment protocols to manage fever, hyperglycaemia, and swallowing dysfunction in acute stroke (QASC): a cluster randomised controlled trial. Lancet. 2011;378(9804):1699–1706. 10.1016/S0140-6736(11)61485-2
- Kuo YW, Huang YC, Lee M, Lee TH, Lee JD Risk stratification model for post-stroke pneumonia in patients with acute ischemic stroke. Eur J Cardiovasc Nurs. 2020;19(6):513–520. 10.1177/1474515119889770
- Glasgow JM, Vaughn-Sarrazin M, Kaboli PJ Leaving against medical advice (AMA): risk of 30-day mortality and hospital readmission. J Gen Intern Med. 2010;25(9):926–929. 10.1007/s11606-010-1371-4
- Lin Z, Han H, Wu C, et al. Discharge against medical advice in acute ischemic stroke: the risk of 30-day unplanned readmission. J Gen Intern Med. 2021;36:1206–1213. 10.1007/s11606-020-06366-0
- Yang A, Wu HM, Tang JL, Xu L, Yang M, Liu GJ Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev. 2016(8):CD004131.
- Zhong LL, Zheng Y, Lau AY, et al. Would integrated Western and traditional Chinese medicine have more benefits for stroke rehabilitation? A systematic review and meta-analysis. Stroke Vasc Neurol. 2021. 7 77–85 10.1136/svn-2020-000781
- Pan Y, Chen R, Li Z, et al. Socioeconomic status and the quality of acute stroke care: the China National Stroke Registry. Stroke. 2016;47(11):2836–2842. 10.1161/STROKEAHA.116.013292
- Wang Y, Li Z, Zhao X, et al. Effect of a multifaceted quality improvement intervention on hospital personnel adherence to performance measures in patients with acute ischemic stroke in China: a Randomized Clinical Trial. JAMA. 2018;320(3):245–254. 10.1001/jama.2018.8802
- Collaboration TFT. Routine oral nutritional supplementation for stroke patients in hospital (FOOD): a multicentre randomised controlled trial. Lancet. 2005;365(9461):755–763.
- Schuetz P, Fehr R, Baechli V, et al. Individualised nutritional support in medical inpatients at nutritional risk: a randomised clinical trial. Lancet. 2019;393(10188):2312–2321. 10.1016/S0140-6736(18)32776-4
- Sremanakova J, Burden S, Kama Y, et al. An observational cohort study investigating risk of malnutrition using the malnutrition universal screening tool in patients with stroke. J Stroke Cerebrovasc Dis. 2019;28(12):104405. 10.1016/j.jstrokecerebrovasdis.2019.104405