Abstract
Background
Social vulnerability occurs when individuals have been relatively disadvantaged by the social determinants of health. Complex interventions that reduce social vulnerability have the potential to improve health in older adults but robust evidence is lacking.
Objective
To identify, appraise and synthesize evidence on the effectiveness of complex interventions targeting reduction in social vulnerability for improving health related outcomes (mortality, function, cognition, subjective health and healthcare use) in older adults living in the community.
Methods
A mixed methods systematic review was conducted. Five databases and targeted grey literature were searched for primary studies of all study types according to predetermined criteria. Data were extracted from each distinct intervention and quality was assessed using the Mixed Methods Appraisal Tool. Effectiveness data were synthesized using vote counting by direction of effect, combining p values and Albatross plots.
Results
Across 38 included studies, there were 34 distinct interventions categorized as strengthening social supports and communities, helping older adults and their caregivers navigate health and social services, enhancing neighbourhood and built environments, promoting education and providing economic stability. There was evidence to support positive influences on function, cognition, subjective health, and reduced hospital utilization. The evidence was mixed for non-hospital healthcare utilization and insufficient to determine effect on mortality.
Conclusion
Despite high heterogeneity and varying quality of studies, attention to reducing an older adult’s social vulnerability assists in improving older adults’ health.
Background
What is Social Vulnerability
When two older adults have the same medical conditions and the same degree of frailty, the difference between living independently in the community with supports and requiring admission to a hospital or long-term care facility can be explained by social circumstances. Social vulnerability (SV) is defined as the degree to which a person’s overall social circumstances leave them susceptible to further insults (ie health or socially related adverse events).Citation1
Social vulnerability occurs when individuals have been relatively disadvantaged by the broader conditions in which they were born, lived, worked and aged; also known as the social determinants of health.Citation2 Socially vulnerable individuals have variable presentations. For example, an older woman living below the poverty line in a racialized neighbourhood may be vulnerable due to economic and housing reasons but has a robust social network of friends and family. Another example of social vulnerability is the reclusive and wealthy older man who has no one to call in the event of a natural disaster. The commonality is the inability to respond in times of crises due to a social reason (ie poverty or isolation) rather than a health-related reason. Unequal determinants directly impact individuals, but arise from complex political, social and economic structures. For this reason, the social determinants of health (SDOH) and social vulnerability are often conceptualized through ecological models.Citation3–Citation5
How SV Influences Health & How Reducing SV Might Work
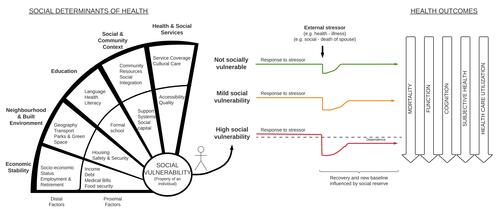
The link between SDOH and health is well documented, accounting for 30–55% of adverse health outcomes globally, such as mortality from chronic diseases.Citation6 The construct of social vulnerability as the manifestation of poor social determinants in an individual is less prominent; nonetheless, being socially vulnerable has been associated with greater mortality,Citation5,Citation7–Citation10 risk of cognitive declineCitation11 and disability,Citation9 and likelihood of long-term care admission.Citation12 Social divergence theory suggests socioeconomic disparities accumulate with time, resulting in worse health inequities in older age, which are compounded by shrinking social circles due to infirmity and death of friends and family members.Citation13 shows the associations between SDOH, SV and health outcomes and helps to explain how interventions reducing social vulnerability through the SDOH might work.
Why It is Important to Do This Review
Studying social vulnerability is challenging as complex interrelated pathways by which upstream social factors influence health to do not allow for hypothesis testing through traditional research methods. Moreover, since multicomponent intervention studies rarely distinguish the social components of the intervention, there is little evidence suggesting what can be done to reduce health inequities through the addition of social programs in real life situations. As social determinants research “for the most part exists outside the literature concerned with effectiveness of interventions”,Citation14 especially in non-hospitalized populations,Citation15,Citation16 this is one gap this review will try to address. To our knowledge, no previous systematic review has attempted to collate and evaluate complex interventions based on a strong social intervention component in older adults. Additionally, for older adults with multiple medical conditions, it is nearly impossible to separate out those who are purely frail from those who are purely socially vulnerable. By accepting that multiple things can go wrong simultaneously in an individual, interventions aimed at social vulnerability cannot ignore medical frailty and vice versa; to do so would continue to fractionate research areas, moving away from treating individuals holistically. Instead, the lens used here to study social interventions within complex interventions accounts for the broader context where older adults would presumably receive both medical and social supports. Combined with a systematic mixed-methods literature review methodology, the authors attempt to answer the broad research question: is there evidence to support the notion that complex interventions targeting reduction in social vulnerability improve health outcomes for older adults living in the community?
Methods
Review Objectives
To identify, appraise and synthesize evidence on the effectiveness of complex interventions where a main component of the intervention targets reduction in social vulnerability for improving health related outcomes (mortality, function, cognition, subjective health and healthcare use) in older adults living in the community.
Study Design, Search Strategy & Selection Criteria
This systematic review employs a mixed methods approach to synthesizing complex interventions following PRISMA-CI guidelines.Citation17,Citation18 Five databases were searched for primary studies: Medline, Cochrane Library (CENTRAL), EPPI-Centre’s Trials Registrar of Promoting Health Interventions, Campbell Collaboration, and Social Sciences Citation Index. The search strategy in Medline was approved by a medical librarian using the Peer Review Electronic Search Strategies (PRESS) checklist,Citation19 then translated to the remaining databases (Supplement A provides the complete search strategy). The last search was conducted on May 18, 2021. Reference lists of included studies were also searched. Due to the nature of the interventions of interest, there was a concurrent search of grey literature to find interventions conducted by governments, non-profit or volunteer organizations.Citation20 This included a targeted website search of known national and international organizations who fund, implement or evaluate social interventions (Administration for Community Living, The Care Policy and Evaluation Centre, Government of Canada, HelpAge International, The International Federation on Ageing and the World Health Organization).
Inclusion criteria is fully described in using the PICOT approach. Quantitative, qualitative or mixed studies were included if they investigated complex interventions targeting reductions in social vulnerabilities through the SDOH in a community-dwelling older adult population, and evaluated a priori outcomes of mortality, function, cognition, self-assessed health, hospital use or other healthcare use (primary care visits to doctors or nurses). A common pitfall in complex intervention reviews is the ambiguity of included studies; hence Supplement A3 provides a full list of exclusion criteria with examples. Although closely related, this is not a review of interventions targeting only social isolation, physical fitness or falls prevention, which already have considerable literature bases and excellent systematic reviews.Citation21–Citation27 The search was limited to English studies from the last ten years, enabling the assessment of practices and challenges relevant in the current political and healthcare climate. This review looked exclusively at active interventions, hereby called social vulnerability interventions, rather than broad governmental policies influencing social vulnerability.
Table 1 Search Strategy: Inclusion Criteria, PICOT Format
Data Collection & Extraction
Citations were imported into EndNoteCitation31 for de-duplication and title and abstract screening. Then full texts were assessed for relevance to inclusion criteria and reasons for exclusions were recorded. Screening and extraction was conducted by the primary author (JM). Relevant data was collected using a piloted data extraction form (Supplement B) to collect information on: (1) general information, (2) study design (3) population (4) intervention details (5) results and outcomes (6) key author conclusions. Methodological quality was assessed using the Mixed Methods Appraisal Tool (MMAT).Citation32
Data Synthesis
Evidence was synthesized using an integrated and aggregated synthesis approach following the Joanna Briggs Institute recommendations.Citation33 Due to the heterogeneity of the studies’ interventions, populations and outcomes/measures, a meta-analysis was not possible as few studies reported sufficient data to calculate standardized effect sizes; nonetheless, three methods of quantitative synthesis were used to answer the primary objective: (1) all studies were synthesized using vote counting based on direction of effect,Citation34,Citation35 (2) for studies including a control group, p values were combined using Fisher’s method to answer the question: “is there evidence of a positive effect on outcome in at least one study” to demonstrate the intervention is beneficial compared to the control,Citation34 and (3) Albatross plots were constructed for studies with a control group and calculable mean differences, which uses 2 sided p values plotted against sample sizes to estimate a magnitude of intervention effect.Citation36 Full details and calculations are described in . Data extraction and synthesis was conducted by one author (JM). A second reviewer also extracted, assessed risk of bias and performed the quantitative data synthesis on a randomly sampled 25% of the included papers to check that the data extraction and synthesis was consistent (audit results also shown in Supplement D3 and E3). All analyses were conducted with RStudio and Excel.
Table 2 Methods of Quantitative Data Synthesis, organized by descending amount of information provided by synthesis method
Results
Results of Search
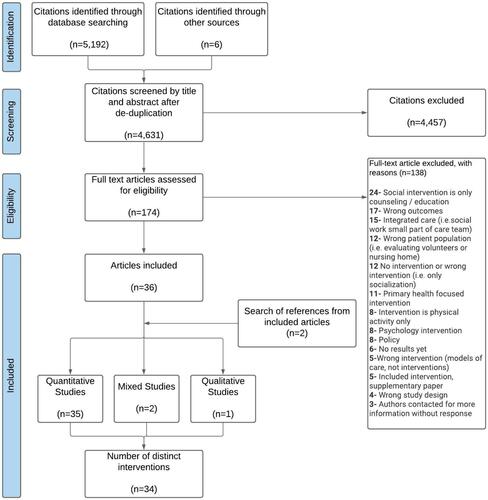
Of the 5918 citations retrieved, 567 were duplicates, 4457 were excluded after title and abstract screening, and 174 full text articles were obtained (see ). This review included a total of 38 studies, representing 34 distinct interventions. 52.9% of studies were conducted in the United States.
Description of Interventions
(with full details in Supplement C) summarizes the characteristics of each complex intervention and target population, grouped into five categories of reducing social vulnerability. On average, participants were 74.9 years old, 69.6% female and 50.2% lived alone. Social workers and nurses were the most prevalent trained professionals.
Table 3 Characteristics and Population of Interventions Included in Review, by Five Categories of Reducing Social Vulnerability
Lasting between 10 weeks to 3 years, there were 12 weekly or biweekly programs aimed at strengthening the social supports and communities where older adults live. Eight involved group activities in senior centers, community or public spacesCitation21,Citation38–Citation45 and 4 involved matched volunteers facilitating social activities.Citation46–Citation49 The interventions varied from organized group activitiesCitation38,Citation39,Citation41–Citation43,Citation45 to sessions promoting health literacy or knowledge of community assets.Citation21,Citation39,Citation43
Ranging from 4 to 52 weeks, some interventions helped older adults and their caregivers navigate health and social services. Navigators were community health workers or volunteers,Citation50–Citation52 social workersCitation53–Citation56 or consisted of multidisciplinary teams.Citation57–Citation63 All took place at home, but 4 were initiated during or shortly after a hospital admission.Citation50,Citation51,Citation54–Citation56 The Community Aging in Place: Advancing Better Living for Elders (CAPABLE) intervention (and its variations) is noteworthy as it is one of the few that has been implemented in multiple states and cities and has a large evidence base (five studies in 6 citations included for this review).Citation57–Citation62
Six interventions worked to enhance the neighbourhood or home built environment. Half provided social services, personalized care coordination, and environmental hazard reduction to affordable housing buildings.Citation64–Citation66 Two offered private home modifications for safetyCitation67,Citation68 and 1 provided accommodations for an adult in need by placing them in a home of an approved Shared Lives carer.Citation69
Two interventions provided financial assistance to older adults in the form of supplemental incomeCitation70,Citation71 or medication co-payment assistance,Citation72 both followed for 18 months. Three interventions mainly focused on education: 2 as college programs designed for seniorsCitation73,Citation74 and 1 for nutrition.Citation75
Description of Study Designs and Quality Assessment
Across all studies, 35 reported only quantitative outcomes, 2 studies used a mixed methodology and one study reported qualitative outcomes. Of the quantitative studies, 9 were randomized controlled trials (RCTs),Citation38–Citation40,Citation51,Citation58,Citation59,Citation61,Citation70,Citation75 7 were quasi-experimental studies or longitudinal cohort studies with a control group (hereafter called controlled before after (CBA)),Citation41,Citation43,Citation47,Citation62,Citation64,Citation67,Citation68 3 were retrospective cohort studies (RCS),Citation46,Citation54,Citation65 and 1 study conducted a cross-sectional survey (XCS).Citation69 The remaining quantitative studies did not have a control group. The mean and median sample sizes of all quantitative studies were 6908 and 242 participants, respectively, ranging from 12 to 172,965 participants. The largest studies were CBA or RCS in study design. Interviews were conducted with 6, 11 and 17 participants in the mixed methods or qualitative studies.
A summary of the individual MMAT scores per question and summary scores per study design are available in Supplement D. No patterns emerged when cross tabulating intervention category with study design. Overall, the quality of the included studies were poor or moderate, with only four studies matching all criteria and deemed high quality.Citation47,Citation54,Citation59,Citation69 Poor quality studies were not excluded from synthesis.
Effects of Interventions
Following quality appraisal, data was synthesized according to intervention category and outcome type (individual results in Supplement E). A visual summary of effect direction by vote counting of all included studies has been tabulated in . Across all studies, there was a positive direction of effect for function, cognition (borderline), subjective health and decreased hospital use. The sign test for the effect on non-hospital physician or nurse visits was 1, signalling interventions were equally likely to result in increased or decreased healthcare use.
Table 4 Summary of Direction of Health Impacts from Included Studies Using Vote Counting
Mortality
Only one study examined mortality as an outcome in relation to a social intervention. The Long Live the Elderly (LLE) study demonstrated a 13% reduction in mortality (p<0.001) during the summer of 2015 in urban areas with LLE compared to areas without the program, with indirect evidence to also suggest LLE attenuated the pre-existing association of higher mortality and lower socioeconomic status.Citation46
Function
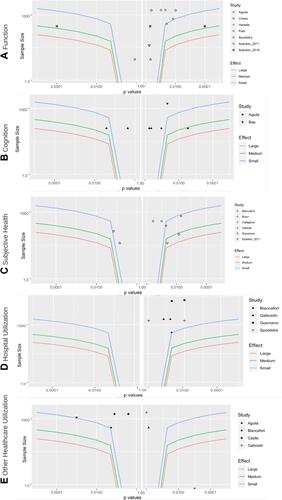
Of the 10 studies, 9 used a measure for ADLs or IADLs;Citation42,Citation43,Citation52,Citation57–Citation59,Citation61,Citation62,Citation67,Citation70 all but two had a positive direction of effect.Citation52,Citation59 Across 8 studies with a comparison group, the combined one-sided p value was <0.001, suggesting a positive effect on function favouring the intervention in at least one study. The studies reporting outcomes with calculable mean differences are visualized in with small estimated effect sizes (less than a 0.2 point difference in any measure used). The study of highest quality and design in this review examined the CAPABLE intervention. At its primary endpoint of 5 months, there was a medium improvement in the CAPABLE group’s ADL (aOR: 0.70, CI: 0.54–0.93, p=0.01) and IADL scores (aOR: 0.83, CI: 0.65–1.06, p=0.13) but not at 12 months (secondary endpoint).Citation59
Figure 3 Albatross plots depicting the association between interventions and five health outcomes (A – function, B – cognition, C – subjective health, D – hospital utilization, E – other healthcare utilization). Effect size contours represent mean differences of 0.2 (small), 0.5 (medium) and 0.8 (large). The left wings represent a negative association, the right wings represent a positive association and a p value of 1.00 represents a null effect.
Cognition
Five out of 6 studies demonstrated benefit on cognition as an outcome of interest.Citation41,Citation49,Citation55,Citation70,Citation74 Three of the interventions focused on strengthening social and community participation.Citation38,Citation41,Citation49 Of the studies with a control group, there was strong evidence of cognitive benefit in at least one study using eight distinct measures of cognition (p<0.001, 3 studies). One RCT reported mixed results with statistically significant benefits on spatial memory only out of 6 cognitive measures.Citation38 Another demonstrated improved verbal recall in the intervention group at 6 and 12 months.Citation70 The estimated effect sizes from the two RCTs are presented in .
Subjective Health
Subjective health (self-perceived or self-reported) or health related quality of life was the most commonly evaluated outcome in 18 studies;Citation21,Citation39,Citation40,Citation43–Citation45,Citation48,Citation49,Citation52,Citation55,Citation56,Citation60,Citation64,Citation66,Citation69,Citation72,Citation73,Citation75 but was also the outcome with the highest proportion of uncontrolled studies. Notably, at least half of all studies in each intervention category measured subjective health. Combining the p values from the controlled studies suggest we reject the null hypothesis of no benefit in any study (p<0.001, 7 studies). The Albatross plot is depicted in and the estimated average effect size ranges from a small to medium improvement in subjective health.
Hospital Utilization
ED visits or hospitalizations were assessed in 15 studies; 80% reported reduced hospital use.Citation39,Citation50,Citation52,Citation54–Citation56,Citation63–Citation66,Citation68,Citation72 Combining p values implies strong evidence (p<0.001, 8 studies) of positive effect on reducing hospital use but suggests any size of effect would be small.
Other Healthcare Utilization
Three studies reported increased primary care provider visitsCitation21,Citation64,Citation70 and two studies reported decreased visitsCitation55,Citation66 although the latter were both uncontrolled before after (UBA) studies of low quality. Within studies, this outcome varied as well; for example, in one study the intervention decreased physician visits but increased nursing visits.Citation39 The calculated combined p value of 4 controlled studies was 0.98 (accepting the null of no benefit of social interventions collectively on primary care provider visits), reflected in .
Discussion
Summary of Results
By counting direction of effect in all studies, the authors show there is a signal for effectiveness on function, subjective health and hospital utilization outcomes greater than chance alone for complex interventions with a main component of the intervention targeting social vulnerability. Then, combining p values of studies with a control group provided strong evidence (p<0.001) that at least one of the interventions improved function, cognition, subjective health and hospital utilization in a positive direction, although the effect sizes estimated with the Albatross plots were small (possible exception of a medium effect size for subjective health). There was an inadequate number of studies evaluating death as an outcome, but the sole study showed a statistically significant reduction in mortality. There is no evidence to suggest the interventions in this review had a consistent impact on primary care utilization. Although a positive effect was coded as a reduction in healthcare utilization, increasing physician and nursing visits can be seen as a good outcome in certain circumstances (ie for older adults in need but with reduced access) and should be considered in the interpretation of results. The complex interventions also demonstrated substantial variations in the program components, settings within the community and targeted older adult population. This review aligns with a recent systematic review and meta-analysis also addressing the gap between social interventions and measuring objective health outcomes, which concluded governmental social policies are an overall promising way to improve population health but noted that studies are often underpowered to detect a health effect, which offers an explanation for the small or null associations found by this review.Citation76
Strengths & Limitations
This review is novel in that it has attempted to describe, and synthesize, complex interventions where the common thread is a strong focus on social interventions. This review looks at effectiveness on objective health outcomes, as opposed to the more common health outcomes of self-perceived improvements, lifestyle changes or surrogate markers (ie increased physical activity);Citation15 albeit, the measured outcomes may not reflect those that are most valued by older adults. By including all types of studies, we are able to determine, in principle, that complex interventions focusing on reducing social vulnerability as a key intervention component does improve health outcomes. However, the choice to lump interventions instead of splitting the complex interventions means that the question of which type of intervention, for which populations, or which components of the intervention are most effective remains unanswerable. For example, Cappelli et al's recent review on social vulnerability suggested the quality of social relationship was a key factor in protecting older adults from functional decline.Citation77 Future research could answer this latter question using component network meta-analytic methods as recommended by the Cochrane Collaboration.
The biggest challenge of this review was managing the heterogeneity of the targeted populations, the SDOH addressed, and the measurement of health outcomes; hence synthesis via a meta-analysis was not feasible nor was answering questions of effect size and relative weights of each study according to quality. Generalizing across studies is also problematic given that 12 different countries and 34 distinct complex interventions, each with multiple components, are included in the findings. How much an intervention can impact is influenced by national or regional health and social policies. For example, the North American navigator interventions may not be as effective in Japan where older adults are automatically assessed for community resources under the national long-term care insurance scheme. Since the same intervention will have varied effects in different populations when the distributions of SDOH supports differ, there is a practical benefit of including all study types in this review, not only the ones with the best evidence or the most funding for a robust study design. Even if only RCTs were examined, the gold standard’s emphasis on “average effects” would not solve the problem of generalizability, nor would it help policymakers implement an intervention in their specific context. Said another way, the authors recognize that complexities create less definitive causal inferences which is a limitation of the review, but continue to search for methods to answer these types of questions without artificially fragmenting the duality of medical and social frailty.
The authors also recognize that this is a synthesis of social interventions that targeted reductions in social vulnerabilities through the social determinants. However, this is not the same as assuming the participants of the included studies were at the same level of baseline social vulnerability, which is another study limitation. A review of this nature, looking at interventions for a defined population with known social disadvantages would be a worthy endeavor.
While this review followed rigorous PRISMA-CI methodology, a single reviewer conducted the screening, data extraction and analysis as part of her doctoral studies. Ideally, a double screening and extraction approach would have been carried out to increase internal validity and reliability, and reduce the chance of random error or personal bias. However, since there was significant consultation between the authors to ensure adherence to the pre-established review protocol and to ensure consensus for any difficult screening questions, it is unlikely that double screening would change the overall findings of this paper.
Clinical, Research and Policy Relevance
Investing in social interventions to improve health has strong intuitive appeal, fundamentally based on the assumption that better population health requires interventions for socially vulnerable older adults. The question of how effective SV interventions may be remains difficult to answer with this review providing a small, but certain positive signal of effect among 34 complex interventions with a strong social focus. Furthermore, the findings of this review challenge researchers in this area to develop or revitalise research methodologies that can make cohesive sense of the heterogeneity of these studies, of the pragmatic nature of social interventions and of the wide variety populations. By providing evidence for the collective effectiveness and practicability of such interventions, there are implications for clinicians, policymakers and older adults themselves to implement and advocate for social interventions that will benefit their communities with objective health improvements as a motivator.
Conclusion
Attention to reducing an older adult’s social vulnerability may be helpful in accomplishing improvements to health. Complex interventions with a main component of the intervention targeting social vulnerability showed evidence of positive effects on function, cognition, subjective health and reduced hospital utilization. Moreover, this review demonstrates heterogeneity in intervention type and quality of studies and supports the need for more research in this area.
Abbreviations
aOR, adjusted odds ratio; CBA, controlled before & after study; CDC, Centers for Disease Control and Prevention; CI, confidence interval EPPI, Evidence for Policy and Practice Information and Co-ordination Centre; MMAT, Mixed Methods Appraisal Tool; OT, occupational therapist; PICOT population, intervention, comparison, outcome, type of study; PRESS, Peer Review Electronic Search Strategies; Q, qualitative; QoL, quality of life; RCS, retrospective controlled study; RCT, randomized controlled trial; RU, retrospective uncontrolled study; SDOH, social determinants of health; SV, social vulnerability; TRoPHI, Trials Registrar of Promoting Health Interventions; UBA, uncontrolled before after study; USA, United States of America; WHO, World Health Organization; XCS, cross-sectional controlled study; XUS, cross sectional uncontrolled study.
Author’s Information
This work is a modified and shortened version of the primary author’s comprehensive exams written as part of her doctoral program.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Acknowledgments
The authors would like to thank Dr. Judith Godin for her expertise in medical statistics and helping to write the code for Albatross plots in R and to Dr. Tyler Pitre for carrying out the data collection and analysis and audit of 25% of the studies. The authors would also like to thank Jackie Phinney from Dalhousie Medicine Libraries who aided in vetting the search strategy. MKA, KR and JCM are part of the Canadian Consortium on Neurodegeneration in Aging (CCNA) Team 14, which investigates how multi-morbidity, frailty and social context modify risk of dementia and patterns of disease expression.
Disclosure
KR is President and Chief Science Officer of DGI Clinical, which in the last five years has contracts with pharma and device manufacturers on individualized outcome measurement. In 2017 he attended an advisory board meeting with Lundbeck. Otherwise any personal fees are for invited guest lectures and academic symposia, received directly from event organizers, chiefly for presentations on frailty. He is Associate Director of the Canadian Consortium on Neurodegeneration in Aging, which is funded by the Canadian Institutes of Health Research, and with additional funding from the Alzheimer Society of Canada and several other charities, as well as, in its first phase (2013–2018), from Pfizer Canada and Sanofi Canada. He receives career support from the Dalhousie Medical Research Foundation as the Kathryn Allen Weldon Professor of Alzheimer Research, and research support from the Canadian Institutes of Health Research, the QEII Health Science Centre Foundation, the Capital Health Research Fund and the Fountain Family Innovation Fund of the QEII Health Science Centre Foundation. KR has asserted copyright of the Clinical Frailty Scale through Dalhousie University. Use is free for research, education or not-for-profit care (users are asked not to change it or charge for its use). MKA reports grants from Canadian Consortium on Neurodegeneration in Aging (CCNA), with funding from Canadian Institutes of Health Research (CIHR). MKA reports grant funding and honoraria from Sanofi, GSK, Pfizer and the Canadian Frailty Network for work relating to frailty and vaccine preventable illness. All other authors declare that they have no competing interests.
Additional information
Funding
References
- Andrew MK. Frailty and social vulnerability. In: Theou O, Rockwood K, editors. Interdisciplinary Topics in Gerontology and Geriatrics. Vol. 41. S. Karger AG; 2015:186–195. doi:10.1159/000381236
- WHO Commission on Social Determinants of Health, World Health Organization, eds. Closing the gap in a generation: health equity through action on the social determinants of health: commission on social determinants of health final report. World Health Organization, Commission on Social Determinants of Health; 2008.
- Bronfenbrenner U. Ecological models of human development. In: Husen T, Postlethwaite T, editors. International Encyclopedia of Education. Vol. 3. 2nd ed. Pergamon Press; 1994:1643–1647.
- Glanz K, Rimer BK, Viswanath K, editors. Chapter 20: ecological models of health behavior. In: Health Behavior and Health Education: Theory, Research, and Practice. Jossey-Bass; 2008:591.
- Andrew MK, Keefe JM. Social vulnerability from a social ecology perspective: a cohort study of older adults from the National Population Health Survey of Canada. BMC Geriatr. 2014;14(1):90. doi:10.1186/1471-2318-14-90
- World Health Organization. Social determinants of health. Available from: https://www.who.int/health-topics/social-determinants-of-health#tab=tab_1. Accessed June 25, 2021.
- Andrew MK, Mitnitski A, Kirkland SA, Rockwood K. The impact of social vulnerability on the survival of the fittest older adults. Age Ageing. 2012;41(2):161–165. doi:10.1093/ageing/afr176
- Andrew MK, Mitnitski A, Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS One. 2008;3(5):e2232. doi:10.1371/journal.pone.0002232
- Wallace LMK, Theou O, Pena F, Rockwood K, Andrew MK. Social vulnerability as a predictor of mortality and disability: cross-country differences in the survey of health, aging, and retirement in Europe (SHARE). Aging Clin Exp Res. 2015;27(3):365–372. doi:10.1007/s40520-014-0271-6
- Armstrong JJ, Andrew MK, Mitnitski A, Launer LJ, White LR, Rockwood K. Social vulnerability and survival across levels of frailty in the Honolulu-Asia Aging Study. Age Ageing. 2015;44(4):709–712. doi:10.1093/ageing/afv016
- Andrew MK, Rockwood K. Social vulnerability predicts cognitive decline in a prospective cohort of older Canadians. Alzheimers Dement. 2010;6(4):319–325.e1. doi:10.1016/j.jalz.2009.11.001
- Godin J, Theou O, Black K, McNeil SA, Andrew MK. Long-term care admissions following hospitalization: the role of social vulnerability. Healthcare. 2019;7(3):91. doi:10.3390/healthcare7030091
- Stolz E, Mayerl H, Waxenegger A, Rásky É, Freidl W. Impact of socioeconomic position on frailty trajectories in 10 European countries: evidence from the Survey of Health, Ageing and Retirement in Europe (2004–2013). J Epidemiol Community Health. 2017;71(1):73–80. doi:10.1136/jech-2016-207712
- Bonnefoy J, Morgan A, Kelly MP, Butt J, Bergman V. Constructing the evidence base on the social determinants of health: a guide. In: World Health Organization Commission on Social Determinants of Health. 2007:337.
- Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health. 2010;64(4):284–291. doi:10.1136/jech.2008.082743
- Andermann A. Taking action on the social determinants of health in clinical practice: a framework for health professionals. CMAJ. 2016;188(17–18):E474–E483. doi:10.1503/cmaj.160177
- Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;a1655. doi:10.1136/bmj.a1655
- Guise J-M, Butler ME, Chang C, Viswanathan M, Pigott T, Tugwell P. AHRQ series on complex intervention systematic reviews—paper 6: PRISMA-CI extension statement and checklist. J Clin Epidemiol. 2017;90:43–50. doi:10.1016/j.jclinepi.2017.06.016
- McGowan J, Sampson M, Salzwedel DM, Cogo E, Foerster V, Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–46. doi:10.1016/j.jclinepi.2016.01.021
- Ogilvie D. Systematic reviews of health effects of social interventions: 1. Finding the evidence: how far should you go? J Epidemiol Community Health. 2005;59(9):804–808. doi:10.1136/jech.2005.034181
- Coll-Planas L, Nyqvist F, Puig T, Urrútia G, Solà I, Monteserín R. Social capital interventions targeting older people and their impact on health: a systematic review. J Epidemiol Community Health. 2017;71(7):663–672. doi:10.1136/jech-2016-208131
- Kelly ME, Duff H, Kelly S, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev. 2017;6(1):259. doi:10.1186/s13643-017-0632-2
- Dickens AP, Richards SH, Greaves CJ, Campbell JL. Interventions targeting social isolation in older people: a systematic review. BMC Public Health. 2011;11(1):647. doi:10.1186/1471-2458-11-647
- Cattan M, White M, Bond J, Learmouth A. Preventing social isolation and loneliness among older people: a systematic review of health promotion interventions. Ageing Soc. 2005;25(01):41–67. doi:10.1017/S0144686X04002594
- Ashworth NL, Chad KE, Harrison EL, Reeder BA, Marshall SC. Home versus center based physical activity programs in older adults. Cochrane Database Syst Rev. 2005. doi:10.1002/14651858.CD004017.pub2
- Jian-Yu E, Li T, McInally L, et al. Environmental and behavioural interventions for reducing physical activity limitation and preventing falls in older people with visual impairment. Cochrane Database Syst Rev. 2020. doi:10.1002/14651858.CD009233.pub3
- Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;2019(1). doi:10.1002/14651858.CD012424.pub2
- Campbell S. Filter to retrieve studies related to geriatrics from the ovid MEDLINE database; 2021. Available from: https://docs.google.com/document/d/1cawy4Zx8v_FyFBPBM7PGGAb8P5_ZAgegIlA6-zSi_mI/edit. Accessed March 22, 2022.
- Social Determinants of Health. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2030; 2020. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health. Accessed March 4, 2021.
- Government of Canada. Social determinants of health and health inequalities; 2019. Available from: https://www.canada.ca/en/public-health/services/health-promotion/population-health/what-determines-health.html. Accessed June 29, 2020.
- Clarivate. Endnote; 2013. Available from: https://endnote.com/. Accessed April 04, 2022.
- Hong Q, Pluye P, Fabregues S, et al. Mixed Methods Appraisal Tool (MMAT); 2018.
- Pearson A, White H, Bath-Hextall F, Salmond S, Apostolo J, Kirkpatrick P. A mixed-methods approach to systematic reviews. Int J Evid Based Healthc. 2015;13(3):121–131. doi:10.1097/XEB.0000000000000052
- McKenzie JE, Brennan SE. Chapter 12: synthesizing and presenting findings using other methods. In: Cochrane Handbook for Systematic Reviews of Interventions Version 6.0. Cochrane; 2019:57. Available from: https://training.cochrane.org/handbook. Accessed March 22, 2022.
- Borenstein M, ed. Introduction to Meta-Analysis. John Wiley & Sons; 2009.
- Harrison S, Jones HE, Martin RM, Lewis SJ, Higgins JPT. The albatross plot: a novel graphical tool for presenting results of diversely reported studies in a systematic review. Res Syn Meth. 2017;8(3):281–289. doi:10.1002/jrsm.1239
- Thomson H, Thomas S, Sellstrom E, Petticrew M. Housing improvements for health and associated socio-economic outcomes. Cochrane Database Syst Rev. 2013. doi:10.1002/14651858.CD008657.pub2
- Bae S, Lee S, Lee S, et al. The effect of a multicomponent intervention to promote community activity on cognitive function in older adults with mild cognitive impairment: a randomized controlled trial. Complement Ther Med. 2019;42:164–169. doi:10.1016/j.ctim.2018.11.011
- Blancafort Alias S, Monteserín Nadal R, Moral I, Roqué Fígols M, Rojano I Luque X, Coll-Planas L. Promoting social capital, self-management and health literacy in older adults through a group-based intervention delivered in low-income urban areas: results of the randomized trial AEQUALIS. BMC Public Health. 2021;21(1):84. doi:10.1186/s12889-020-10094-9
- Bøen H, Dalgard OS, Johansen R, Nord E. A randomized controlled trial of a senior centre group programme for increasing social support and preventing depression in elderly people living at home in Norway. BMC Geriatr. 2012;12(1):20. doi:10.1186/1471-2318-12-20
- Hikichi H, Kondo K, Takeda T, Kawachi I. Social interaction and cognitive decline: results of a 7-year community intervention. Alzheimers Dement. 2017;3(1):23–32. doi:10.1016/j.trci.2016.11.003
- Hikichi H, Kondo N, Kondo K, Aida J, Takeda T, Kawachi I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: propensity score matching and instrumental variable analyses, JAGES Taketoyo study. J Epidemiol Community Health. 2015;69(9):905–910. doi:10.1136/jech-2014-205345
- Harada K, Masumoto K, Katagiri K, et al. Three-year effects of neighborhood social network intervention on mental and physical health of older adults. Aging Ment Health. 2020:1–11. doi:10.1080/13607863.2020.1839858
- Daban F, Garcia-Subirats I, Porthé V, et al. Improving mental health and wellbeing in elderly people isolated at home due to architectural barriers: a community health intervention. Aten Primaria. 2021;53(5):102020. doi:10.1016/j.aprim.2021.102020
- Taylor J, Cole R, Kynn M, Lowe J. Home away from home: health and wellbeing benefits of men’s sheds. Health Promot J Austr. 2018;29(3):236–242. doi:10.1002/hpja.15
- Liotta G, Inzerilli M, Palombi L, et al. Social interventions to prevent heat-related mortality in the older adult in Rome, Italy: a Quasi-experimental study. IJERPH. 2018;15(4):715. doi:10.3390/ijerph15040715
- Jacobs EA, Schwei R, Hetzel S, et al. Evaluation of peer-to-peer support and health care utilization among community-dwelling older adults. JAMA Netw Open. 2020;3(12):e2030090. doi:10.1001/jamanetworkopen.2020.30090
- Chapin RK, Sergeant JF, Landry S, et al. Reclaiming joy: pilot evaluation of a mental health peer support program for older adults who receive medicaid. Gerontologist. 2013;53(2):345–352. doi:10.1093/geront/gns120
- Chiang Y-H, Hsu H-C. Health outcomes associated with participating in community care centres for older people in Taiwan. Health Soc Care Community. 2019;27(2):337–347. doi:10.1111/hsc.12651
- Galbraith AA, Meyers DJ, Ross-Degnan D, et al. Long-term impact of a postdischarge community health worker intervention on health care costs in a safety-net system. Health Serv Res. 2017;52(6):2061–2078. doi:10.1111/1475-6773.12790
- Balaban RB, Galbraith AA, Burns ME, Vialle-Valentin CE, Larochelle MR, Ross-Degnan D. A patient navigator intervention to reduce hospital readmissions among high-risk safety-net patients: a randomized controlled trial. J Gen Intern Med. 2015;30(7):907–915. doi:10.1007/s11606-015-3185-x
- Scharlach AE, Graham CL, Berridge C. An integrated model of co-ordinated community-based care. Gerontologist. 2015;55(4):677–687. doi:10.1093/geront/gnu075
- Hood S, Lu YY-F, Jenkins K, et al. Exploration of perceived psychosocial benefits of senior companion program participation among urban-dwelling, low-income older adult women volunteers. Innov Aging. 2018;2(2). doi:10.1093/geroni/igy018
- Evans WN, Kroeger S, Munnich EL, Ortuzar G, Wagner KL. Reducing readmissions by addressing the social determinants of health. Am J Health Econ. 2021;7(1):1–40. doi:10.1086/711725
- Stevens AB, Hochhalter AK, Basu R, et al. A model program of community-based supports for older adults at risk of nursing facility placement. J Am Geriatr Soc. 2015;63(12):2601–2609. doi:10.1111/jgs.13831
- Watkins L, Hall C, Kring D. Hospital to home: a transition program for frail older adults. Prof Case Manag. 2012;17(3):117–123. doi:10.1097/NCM.0b013e318243d6a7
- Szanton SL, Wolff JL, Leff B, et al. Preliminary data from community aging in place, advancing better living for elders, a patient‐directed, team‐based intervention to improve physical function and decrease nursing home utilization: the first 100 individuals to complete a centers for medicare and medicaid services innovation project. J Am Geriatr Soc. 2015;63(2):371–374. doi:10.1111/jgs.13245
- Szanton SL, Thorpe RJ, Boyd C, et al. Community aging in place, advancing better living for elders: a bio-behavioral-environmental intervention to improve function and health-related quality of life in disabled older adults. J Am Geriatr Soc. 2011;59(12):2314–2320. doi:10.1111/j.1532-5415.2011.03698.x
- Szanton SL, Xue Q-L, Leff B, et al. Effect of a biobehavioral environmental approach on disability among low-income older adults: a randomized clinical trial. JAMA Intern Med. 2019;179(2):204. doi:10.1001/jamainternmed.2018.6026
- Szanton SL, Leff B, Wolff JL, Roberts L, Gitlin LN. Home-based care program reduces disability and promotes aging in place. Health Aff. 2016;35(9):1558–1563. doi:10.1377/hlthaff.2016.0140
- Crews DC, Delaney AM, Walker taylor JL, et al. Pilot intervention addressing social support and functioning of low socioeconomic status older adults with ESRD: the seniors optimizing community integration to advance better living with ESRD (SOCIABLE) study. Kidney Med. 2019;1(1):13–20. doi:10.1016/j.xkme.2018.12.001
- Spoelstra SL, Sikorskii A, Gitlin LN, Schueller M, Kline M, Szanton SL. Dissemination of the CAPABLE model of care in a Medicaid Waiver program to improve physical function. J Am Geriatr Soc. 2018;jgs.15713. doi:10.1111/jgs.15713
- Prior MK, Bahret BA, Allen RI, Pasupuleti S. The efficacy of a senior outreach program in the reduction of hospital readmissions and emergency department visits among chronically ill seniors. Soc Work Health Care. 2012;51(4):345–360. doi:10.1080/00981389.2011.644103
- Castle N, Resnick N. Service-enriched housing: the staying at home program. J Appl Gerontol. 2016;35(8):857–877. doi:10.1177/0733464814540049
- Gusmano MK, Rodwin VG, Weisz D. Medicare beneficiaries living in housing with supportive services experienced lower hospital use than others. Health Aff. 2018;37(10):1562–1569. doi:10.1377/hlthaff.2018.0070
- Turcotte DA, Woskie S, Gore R, Chaves E, Adejumo KL. Asthma, COPD, and home environments. Ann Allergy Asthma Immunol. 2019;122(5):486–491. doi:10.1016/j.anai.2019.02.026
- Park CM, Oh G, Lee H, et al. Multicomponent intervention and long‐term disability in older adults: a nonrandomized prospective study. J Am Geriatr Soc. 2021;69(3):669–677. doi:10.1111/jgs.16926
- Tohn E, Wilson J, Van Oss T, Gurecka M. Incorporating injury prevention into energy weatherization programs. J Public Health Manag Pract. 2020;26(1):80–82. doi:10.1097/PHH.0000000000000947
- Callaghan L, Brookes N, Palmer S. Older people receiving family-based support in the community: a survey of quality of life among users of ‘Shared Lives’ in England. Health Soc Care Community. 2017;25(5):1655–1666. doi:10.1111/hsc.12422
- Aguila E, Smith JP. Supplemental income program design: a cluster-randomized controlled trial to examine the health and wellbeing effects on older adults by gender, duration, and payment frequency. Soc Sci Med. 2020;259:113139. doi:10.1016/j.socscimed.2020.113139
- Aguila E, Kapteyn A, Smith JP. Effects of income supplementation on health of the poor elderly: the case of Mexico. Proc Natl Acad Sci USA. 2015;112(1):70–75. doi:10.1073/pnas.1414453112
- Herity LB, Upchurch G, Schenck AP. Senior PharmAssist: less hospital use with enrollment in an innovative community‐based program. J Am Geriatr Soc. 2018;66(12):2394–2400. doi:10.1111/jgs.15617
- Jo HE, Jo JS, Veblen KK, Potter PJ. Enoch senior’s college for korean immigrant seniors: quality of life effects. Can J Aging. 2018;37(3):345–359. doi:10.1017/S0714980818000211
- Molina-Luque F, Casado N, Stončikaitė I. University stakeholders, intergenerational relationships and lifelong learning: a European case study. Educ Gerontol. 2018;44(12):744–752. doi:10.1080/03601277.2018.1555366
- Suominen MH, Puranen TM, Jyväkorpi SK, et al. Nutritional guidance improves nutrient intake and quality of life, and may prevent falls in aged persons with Alzheimer disease living with a spouse (NuAD trial). J Nutr Health Aging. 2015;19(9):901–907. doi:10.1007/s12603-015-0558-0
- Courtin E, Kim S, Song S, Yu W, Muennig P. Can social policies improve health? A systematic review and meta‐analysis of 38 randomized trials. Milbank Q. 2020;98(2):297–371. doi:10.1111/1468-0009.12451
- Cappelli M, Bordonali A, Giannotti C, et al. Social vulnerability underlying disability amongst older adults: a systematic review. Eur J Clin Invest. 2020;50(6). doi:10.1111/eci.13239