Abstract
Background
Osteoporotic fractures are important causes of morbidity, mortality, and increased health care costs. However, the risk of osteoporotic fractures can be decreased, with clinical studies supporting the use of calcium and vitamin D supplements to promote bone health. Vitamin D insufficiency is widespread, particularly among postmenopausal women with osteoporosis, and this indicates that dietary intake is suboptimal, even though vitamin D supplements are widely available.
Methods
We conducted an observational study, using telephone surveys, to estimate vitamin D and calcium intake and the use of prescription osteoporosis medications in Spanish women aged ≥ 50 years with osteoporosis.
Results
Among the study participants, mean dietary calcium intake was 1239 mg/day and generally appeared sufficient in terms of the recommended daily intake guidance documents. Participants aged ≥ 75 years had a significantly lower mean dietary calcium intake (988 mg/day), thus one-half were below the level advised by the World Health Organization. Daily calcium intake was also lower in participants who were not taking prescription medications for bone health. Dietary vitamin D intake was 167 IU/day, which is well below both the established target dose (400 IU/day) and the more recent, higher guideline recommended for postmenopausal women (800–1300 IU/day). Dietary vitamin D intake was even lower for participants aged ≥ 75 years (120 IU/day) and was not related to the use of bone health prescription medications.
Conclusion
These results support the need for greater promotion of the benefits of higher vitamin D intake in Spanish women with osteoporosis.
Background
Osteoporotic fractures are common in women aged ≥ 50 years but are potentially preventable. The lifetime risk of fracture is >50% for women at age 50 and is >20% for men of the same age,Citation1 with such fractures estimated to affect 20 million Europeans.Citation2,Citation3 Osteoporotic fractures are associated with serious complications and contribute to an increase in mortality rates of up to 20% in the elderly.Citation4
Osteoporosis presents a considerable health burden for individual European countries. In Spain, postmenopausal women experience a lifetime fracture risk of 50.4%;Citation5 the prevalence of osteoporotic hip fracture is about 7.20 per 1000 people aged ≥ 60 years, with 74% of sufferers being women and 26% being men.Citation6 The total annual direct cost of hospitalization for hip fractures in Spain was about 216 million Euros in 1996.Citation7
Adequate calcium and vitamin D are indispensable for maintaining bone health. Dietary calcium is required for normal calcium balance and prevents bone loss due to dietary deficiency. Study findings support a role for calcium and vitamin D supplementation in osteoporosis treatment, as the diets of many osteoporotic patients are deficient in one or both.Citation8 Serum levels of the active metabolite 25-hydroxyvitamin D are the best way to assess vitamin D sufficiency. Serum levels of 25-hydroxyvitamin D are correlated with bone mineral density in many studies.Citation9–Citation11 However, key to achieving bone health benefits is the use of an appropriate vitamin D dose, with a daily dose of at least 700–800 IU recommended to produce adequate serum 25-hydroxyvitamin D.Citation12 Similar favorable effects on bone mass and, in some studies, fracture risk have been associated with calciumCitation13,Citation14 and vitamin D plus calciumCitation15–Citation17 supplementation of nutritionally deficient populations.
As there are few natural food sources of vitamin D, the failure of postmenopausal women with osteoporosis to take sufficient vitamin D supplements can result in vitamin D inadequacy.Citation18 Studies conducted in various European countries showed that a substantial proportion of patients with osteoporosis, ranging from 32.1%Citation19 to 81.6%,Citation20 have suboptimal serum 25-hydroxyvitamin D levels.Citation19–Citation22 Widespread vitamin D insufficiency in patients with osteoporosis may be due to a number of factors, including the biological consequences of aging, lack of sun exposure, and limited awareness of the importance of vitamin D supplementation by both patients and their physicians.Citation18,Citation23
At present, there are limited data on the dietary and supplemental intake of vitamin D and calcium in patients with osteoporosis. The objective of this study was to assess vitamin D and calcium intake, from both food and dietary supplements, in Spanish females aged ≥ 50 years with osteoporosis.
Methods
Study participants
Spanish physicians (107) were identified using national stratified physician lists purchased from national councils and the local national health system. The physicians were contacted and those willing to participate in the study were asked to refer their qualifying patients with osteoporosis who were subsequently contacted by telephone. Patients interested in participating in the study were asked to phone a toll-free number for additional information and to determine whether they qualified. Inclusion criteria included being a female aged ≥ 50 years diagnosed with postmenopausal osteoporosis, and whose residence was in Spain. The study design and questionnaire were reviewed and approved by the Essex Institutional Review Board (Lebanon, NJ, USA). Respondents who met the inclusion criteria were read a statement of informed consent. This statement included a brief description of the study, its voluntary nature, participant confidentiality, and contacts for specific questions about participants’ health conditions, participants’ rights, and general information about the study. Those who did not provide informed consent to participate in the study were excluded. The study was conducted by a third-party contract research organization.
It was determined that a sample size of 207 was required to detect a statistically significant difference (5% level of significance) in mean population calcium intakes, assuming a mean standard deviation [SD] intake of 1200 (577) mg/day, the effect size of 100 mg/day yields 80% power for a sample size of N = 207 at 5% level of significance.
Survey questions
The survey was conducted by trained, native Spanish-speaking interviewers; an average of 15 minutes was given to participants for survey completion. Questions were drafted in English and translated into Spanish. Subsequently, the questions were translated back into English to ensure that the questions had been accurately translated.
Survey responses provided information on prescribed osteoporosis medications, calcium, and vitamin D intake from the diet and supplements. Participants were asked, “Are you currently taking prescription medication(s) for your bone health?” If their answer was affirmative, they were asked, “What prescription medication(s) are you currently taking for bone health?” Participants were also asked to describe the frequency with which they consumed certain foods, using the Supplementation en Vitamines et Mineraux Antioxydants (SU.VI.MAX) food-frequency questionnaire;Citation24 a list of the most common foods consumed was broken down by type. Participants were also asked eight questions about their use of vitamin and mineral supplements, including calcium or calcium-containing antacids. They were asked if they took multivitamins regularly and, if so, how often (possible responses: every day, 4–6 days per week, 1–3 days per week, 1–3 days per month, and <1 day per month). Participants were asked if the calcium products contained vitamin D and were prompted to look at the package label to report the calcium dosage (<500 mg, 500–599 mg, 600–999 mg, ≥1000 mg). Participants were also asked, “During the past month, have you sunbathed or travelled to a sunny climate or region?” and “During the past month, on average, how many hours per week did you spend outside without and with sun protection (sunscreen or protective clothing)?” Of the twelve questions, two were from the National Health and Nutrition Examination Survey (NHANES) to facilitate validation.Citation25
The questionnaires included a vitamin D assessment component from the Health Habits and History Questionnaire (HHHQ), the Spanish Food Frequency Questionnaire (FFQ), and a short survey on calcium and vitamin D intake.Citation24,Citation26 The HHHQ is a self-administered diet history questionnaire. It has been validated for use in epidemiological and clinical studies. The FFQ consist of questions on frequency of intake of foods such as dairy, eggs, meat, fish, vegetables, fruit, legumes, fats, sweets and pastries, drinks, pre-cooked or pre-prepared food, and miscellaneous food. Possible responses included, “never,” “yearly,” “monthly,” “weekly,” or “daily.” The Spanish FFQ has been validated and used in previous epidemiological studies.Citation27,Citation28
Published references were used to determine the calcium and/or vitamin D content per food serving and the number of required servings per listed item.Citation24,Citation29 The average daily intake of calcium and vitamin D per serving for each food item was computed as: (calcium or vitamin D content) × (times per year/365), (calcium or vitamin D content) × (times per month/30), (calcium or vitamin D content) × (times per week/7), or (calcium or vitamin D content) × (times per day). Daily values for all foods were then added to achieve the total daily intake of calcium and vitamin D.
Daily calcium intake from calcium or calcium-containing antacids was computed as reported daily elemental calcium intake at <800 mg, 800–1200 mg, or ≥1200 mg. Respondents who regularly used a standard multivitamin typically received 400 IU vitamin D, and daily vitamin D intake from supplements was computed as daily use at <200 IU, 200–400 IU, or <400 IU.
Statistical analysis
Mean daily calcium and vitamin D intake were computed. A one-sample t-test was performed to estimate whether the mean daily vitamin D intake was significantly lower than the recommended average daily dose of 400 IU/day.Citation30 A similar analysis was done to estimate whether the sample mean daily calcium intake was significantly lower than the 800 mg recommended daily dose.Citation31 To identify factors associated with calcium and vitamin D intake, in addition to their relative effects, least squares regressions were conducted. Fisher’s exact tests were used to analyze the differences of vitamin D/calcium intake in patients on different prescribed medications for bone health and the differences of vitamin D/calcium intake from diets in patients among different age groups.
Results
Patient characteristics
Of the 207 women who participated, 62.8% were aged 50–64 years, 20.8% were aged 65–74 years, and 16.4% were aged ≥ 75 years.
Vitamin D intake from food
The mean (SD) intake of vitamin D from food was 167 (±87) IU/day (), which is notably less than the recommended daily dose of 400 IU/day. Vitamin D intake was not significantly different (P = 0.114) in patients taking bisphosphonates (186 ± 92 IU/day) compared with those taking non-bisphosphonates (156 ± 64 IU/day) or no prescription medications for bone health (148 ± 85 IU/day).
Table 1 Daily vitamin D intake from food
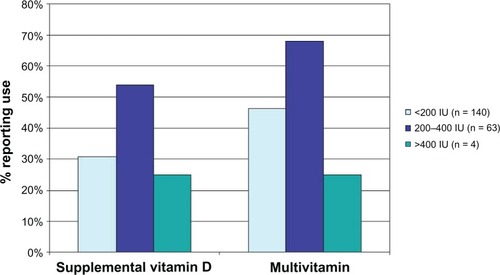
Supplemental vitamin D and multivitamin use
Of those participants who derived 200–400 IU/day of vitamin D from their diets, 68% reported taking a multivitamin with vitamin D and 54% reported taking supplemental vitamin D alone (). Use of a multivitamin with vitamin D and supplemental vitamin D alone by groups obtaining <200 IU/day and >400 IU/day from their diet was notably lower, as shown in . When considered by age group, women aged ≥ 75 years reported a significantly lower mean daily intake of vitamin D from food (120 ± 65 IU/day versus 177 ± 77 IU/day for the 50–64 years age group and 176 ± 115 IU/day for the 65–74 years age group; P = 0.034) ().
Calcium intake from food
The mean (SD) calcium intake from food was 1239 (±457) mg/day (), which was notably higher than the recommended daily dose of 800 mg/day. Daily calcium intake was also significantly lower (P = 0.037) in patients not taking prescription medications for bone health (1054 ± 336 mg/day) compared with those taking bisphosphonates (1365 ± 448 mg/day) or non-bisphosphonates (1167 ± 432 mg/day).
Table 2 Daily calcium intake from food
The predominant sources of dietary calcium were dairy products (mean 477.4 mg) and vegetables (371.3 mg), with more participants taking milk every day than the other major sources of calcium (). The proportion of participants eating a portion each day of all major calcium sources was higher for those with a daily calcium intake of more than 800 mg.
Table 3 Contributors to dietary calcium intake
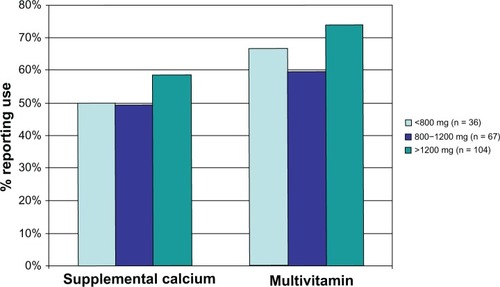
Supplemental calcium and multivitamin use by dietary calcium intake
Of those participants who derived < 800 mg/day of calcium from their diet, 67% reported taking a multivitamin with calcium and 50% reported taking supplemental calcium alone (). Similar incidences of multivitamin with calcium, and supplemental calcium alone use were seen in participants obtaining 800–1200 mg/day and ≥1200 mg/day from their diet, as shown in . When considered by age group, women aged ≥ 75 years reported a significantly lower mean daily intake of calcium from food (988 ± 346 mg/day versus 1314 ± 461 mg/day for the 50–64 age group and 1209 ± 460 mg/day for the 65–74 age group; P < 0.0001) ().
Of the participants who reported taking a calcium supplement, 31.3% reported taking <500 mg daily, 30.4% reported taking 500–599 mg, 8.9% reported taking 600–999 mg, 10.7% reported taking >1000 mg, and 18.8% reported not knowing how much they were taking. In addition, 69.6% of those participants who reported taking calcium supplements also reported that the calcium products contained vitamin D.
Discussion
The results of this observational study in postmenopausal Spanish women indicate a high prevalence of insufficient vitamin D intake (mean 167 IU/day from food) in women with osteoporosis, particularly in those aged ≥ 75 years. Although the amount of vitamin D obtained from supplements was not specified in this study, the low proportion of subjects taking supplements and multivitamins combined with a low dietary intake supports this conclusion. In fact, these results are likely to underestimate the prevalence of vitamin D insufficiency, because a low threshold for vitamin D sufficiency (400 IU/day) was applied. In contrast, Food and Agriculture Organization of the United Nations/World Health Organization guidelines recommend a minimum vitamin D intake of 600 IU/day for women aged > 65 years.Citation32 More recent European guidelines recommend a minimum intake of 800 IU per day to reduce fracture risk.Citation30
In contrast, the mean dietary calcium intake in postmenopausal Spanish women was higher (1239 mg/day) than the recommended daily dose of 800 mg/day, and was comparable across all age groups assessed. This daily intake of calcium is consistent with the level recommended in the “Nutritional objectives for the Spanish population.”Citation31 Calcium intake from food was significantly higher in participants taking osteoporosis medications. Calcium supplementation occurred with comparable frequency in women irrespective of their dietary calcium intake. The target calcium intake level of 800 mg/day used in this study is lower than the 1300 mg/day recommended by the Food and Agriculture Organization of the United Nations/World Health Organization for postmenopausal women;Citation32 however, only postmenopausal Spanish women aged ≥ 75 years had a dietary calcium intake substantially below this higher target.
Comparison with literature findings
A number of recent studies have also shown suboptimal vitamin D intake in elderly Spanish populationsCitation33,Citation34 and in various groups of postmenopausal Spanish women.Citation35–Citation37 However, the findings reported in this study are somewhat at odds with those presented in a recent study conducted in postmenopausal European women with osteoporosis or osteopenia.Citation19 Despite a high prevalence of vitamin D inadequacy in European subjects, Bruyère et al showed a mean 25-hydroxyvitamin D level of 85.2 (±33.3) nmol/L in Spanish subjects, a level well above all recommended cutoffs.Citation19 This mean value did, however, equate to low 25-hydroxyvitamin D levels for 45.8% of Spanish participants. The finding of more widespread vitamin D inadequacy in our study could result from the absence of any assessment of the contribution of endogenous vitamin D synthesis following exposure to sunlight; Bruyère et al noted that levels of 25-hydroxyvitamin D were significantly different when sampling occurred in winter than when it occurred during the summer months.Citation19
The literature considering dietary calcium intake in Spanish populations shows considerable variability. Bruyère et al reported a dietary intake of 1074 mg/day for postmenopausal Spanish women with osteoporosis,Citation19 which is not substantially different from our finding. Their study went on to identify that the majority of dietary calcium ingested was derived from dairy sources, consistent with previous reports.Citation38,Citation39 In contrast, other studies report a lower mean daily calcium intake, of approximately 800 mg, for elderly/postmenopausal women in various regions of Spain.Citation34,Citation35,Citation37 These studies assessed nutrient levels in specific areas of Spain, raising the prospect that regional variation in dietary patterns probably affects calcium intake.
Methods of improving vitamin D sufficiency
In our study, vitamin D intake from food was not notably different in women who did or did not receive prescribed medication for osteoporosis. This finding is somewhat surprising, given that women regularly taking such treatments might be expected to be more aware of other methods of optimizing their bone health. Vitamin D supplementation could help to promote bone health in Spanish women with osteoporosis.Citation34,Citation35
Study limitations
There are several limitations inherent in our study design. The study was observational in its nature and, although likely to be reflective of usual-care practice, may be subject to selection bias. Results may be biased by the use of a convenience sample and by the selection of patients who consented to the study and contacted the interviewers: these patients may be more aware of their health needs, more motivated to seek care, and/or have more favorable views of their health care compared with patients who did not agree to participate. This disparity may have led to our underestimating the actual level of vitamin D inadequacy in Spanish postmenopausal women. In addition, the study results are based on patient self-report, which is subject to the influence of memory and other subjective factors.
Although 69.6% of participants reported that their calcium supplements contained vitamin D, this study did not ask participants to quantify the amount of vitamin D contained in the calcium supplements. The amounts of vitamin D in the vitamin D supplements were also not specified, thus the total daily intake of vitamin D from both food and supplements could not be estimated.
The data consider the dietary intake of both vitamin D and calcium rather than serum levels of the active components. Endogenous synthesis following exposure to sunlight is a major source of vitamin D.Citation40 Our study did not assess different levels of exposure to sunlight, which are known to affect serum levels of 25-hydroxyvitamin D.Citation33,Citation35 In addition, our study did not assess different types of diets. A recent study showed that calcium absorption and utilization are influenced by dietary composition, with a Mediterranean diet potentially favoring nutrient utilization to a greater extent than other diets.Citation41 In a study by Mataix et al, 40% of individuals participating in a survey in Southern Spain had a low calcium intake, yet plasma calcium concentrations were below the reference range in only 15%.Citation42
The extent to which our results apply to the general European population is unclear, and the findings cannot be extrapolated to men with osteoporosis. Elderly men are also at high risk of developing osteoporosis,Citation1,Citation6 with the resulting fractures being associated with substantial morbidity and mortality.Citation43
Future studies are needed to better define the optimal use of vitamin D supplements in promoting bone health and preventing osteoporotic fractures. Some previous studies have failed to demonstrate a significant benefit for vitamin D supplementation on fracture risk.Citation44,Citation45 For example, in a study of postmenopausal women recruited to a Women’s Health Initiative trial with or without osteoporosis, calcium plus vitamin D supplementation increased hip bone mineral density.Citation44 However, a significant effect of supplementation on the incidence of hip fracture was observed only after data from non-treatment-compliant subjects were censored. In the Randomised Evaluation of Calcium Or vitamin D (RECORD) trial, calcium and/or vitamin D supplementation did not significantly reduce the incidence of low-energy fracture.Citation45 A limitation of both studies was the inclusion of subjects who had not been diagnosed with osteoporosis. In addition, the Women’s Health Initiative highlights the importance of achieving sufficiently high vitamin D intake, which is increasingly being cited as instrumental to optimizing bone health benefits.Citation44
Conclusion
Inadequate vitamin D intake is common among postmenopausal women with osteoporosis in Spain. Further initiatives, including improved patient education, lifestyle, and vitamin D supplementation or pharmacotherapy, are needed to promote adequate vitamin D intake in elderly populations to avoid serious adverse consequences for bone health.
Authors’ contributions
TF, SS, and GN conceived and designed the study. TF performed statistical analyses. AM and LS led data presentation and report drafting. All authors contributed to the interpretation of study data, the intellectual content of the report, and approval of the final manuscript.
Acknowledgments
Study funding was provided by Merck & Company, Inc. We thank Melissa Stauffer, PhD, Lauren Weisenfluh, and Dimitra Panagiotoglou, all in affiliation with SCRIBCO, for medical writing assistance.
Disclosure
All the authors are employees of Merck & Company, Inc.
References
- van StaaTPDennisonEMLeufkensHGCooperCEpidemiology of fractures in England and WalesBone200129651752211728921
- JohnellOKanisJAAn estimate of the worldwide prevalence and disability associated with osteoporotic fracturesOsteoporos Int200617121726173316983459
- International Osteoporosis Foundation (IOF)Osteoporosis in the EU: Improving the Assessment of Fracture RiskNyonIOF2006 Available from: http://www.iofbonehealth.org/sites/default/files/PDFs/EU%20Reports/eu-report-2006.pdfAccessed March 11, 2013
- MeltonLJ3rdAdverse outcomes of osteoporotic fractures in the general populationJ Bone Miner Res20031861139114112817771
- ReyesBalaguer JMorenoOlmos JPrevalence of osteopenia and osteoporosis in postmenopausal womenAten Primaria2005357342345 Spanish15871793
- HerreraAMartínezAAFerrandezLGilEMorenoAEpidemiology of osteoporotic hip fractures in SpainInt Orthop2006301111416328387
- European CommissionReport on Osteoporosis in the European Community: Action for PreventionLuxembourgOffice for Official Publications of the European Commission1998 Available from: http://www.iofbonehealth.org/sites/default/files/PDFs/EU%20Reports/eu_report_1998.pdfAccessed March 11, 2013
- LipsPBouillonRvan SchoorNMReducing fracture risk with calcium and vitamin DClinical Endocrinol (Oxf)201073327728520796001
- MalavoltaNPratelliLFrigatoMMulèRMasciaMLGnudiSThe relationship of vitamin D status to bone mineral density in an Italian population of postmenopausal womenOsteoporos Int200516121691169715959621
- Bischoff-FerrariHADietrichTOravEJDawson-HughesBPositive association between 25-hydroxy vitamin D levels and bone mineral density: a population-based study of younger and older adultsAm J Med2004116963463915093761
- von MühlenDGGreendaleGAGarlandCFWanLBarrett-ConnorEVitamin D, parathyroid hormone levels and bone mineral density in community-dwelling older women: the Rancho Bernardo StudyOsteoporos Int200516121721172615928802
- Bischoff-FerrariHVitamin D: what is an adequate vitamin D level and how much supplementation is necessary?Best Pract Res Clin Rheumatol200923678979519945690
- CummingRGCalcium intake and bone mass: a quantitative review of the evidenceCalcif Tissue Int19904741942012146986
- PrinceRLDevineADhaliwalSSDickIMEffects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly womenArch Intern Med2006166886987516636212
- LarsenERMosekildeLFoldspangAVitamin D and calcium supplementation prevents osteoporotic fractures in elderly community dwelling residents: a pragmatic population-based 3-year intervention studyJ Bone Miner Res200419337037815040824
- ChapuyMCPamphileRParisECombined calcium and vitamin D3 supplementation in elderly women: confirmation of reversal of secondary hyperparathyroidism and hip fracture risk: the Decalyos II studyOsteoporos Int200213325726411991447
- Dawson-HughesBHarrisSSKrallEADallalGEEffect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or olderN Engl J Med1997337106706769278463
- ReschHWalliserJPhillipsSWehrenLESenSSPhysician and patient perceptions on the use of vitamin D and calcium in osteoporosis treatment: a European and Latin American perspectiveCurr Med Res Opin20072361227123717559732
- BruyèreOMalaiseONeuprezAColletteJReginsterJYPrevalence of vitamin D inadequacy in European postmenopausal womenCurr Med Res Opin20072381939194417631697
- MonizCDewTDixonTPrevalence of vitamin D inadequacy in osteoporotic hip fracture patients in LondonCurr Med Res Opin200521121891189416368037
- NeuprezABruyèreOColletteJReginsterJYVitamin D inadequacy in Belgian postmenopausal osteoporotic womenBMC Public Health200776417462085
- GaugrisSHeaneyRPBoonenSKurthHBentkoverJDSenSSVitamin D inadequacy among post-menopausal women: a systematic reviewQJM200598966767616006498
- ViethRLadakYWalfishPGAge-related changes in the 25-hydroxyvitamin D versus parathyroid hormone relationship suggest a different reason why older adults require more vitamin DJ Clin Endocrinol Metab200388118519112519850
- HercbergSGalanPPreziosiPThe SU.VI.MAX study: a randomized, placebo-controlled trial of the health effects of antioxidant vitamins and mineralsArch Intern Med2004164212335234215557412
- FanTBogleSNoceaGSenSSValidity and reproducibility of questionnaire about preventive behaviors among French and Spanish postmenopausal women with osteoporosis in the Calcium and Vitamin Intake (CaVit) StudyCalcif Tissue Int200882S188
- BlalockSJNortonLLPatelRACabralKThomasCLDevelopment and assessment of a short instrument for assessing dietary intakes of calcium and vitamin DJ Am Pharm Assoc (2003)200343668569314717265
- KesseEBertraisSAstorgPDairy products, calcium and phosphorus intake, and the risk of prostate cancer: results of the French prospective SU.VI.MAX (Supplémentation en Vitamines et Minéraux Antioxydants) studyBr J Nutr200695353954516512941
- Kesse-GuyotEBertraisSDuperrayBDairy products, calcium and the risk of breast cancer: results of the French SU.VI.MAX prospective studyAnn Nutr Metab200751213914517536191
- SuzukiYWhitingSJDavisonKSChilibeckPDTotal calcium intake is associated with cortical bone mineral density in a cohort of postmenopausal women not taking estrogenJ Nutr Health Aging2003729629912917743
- International Osteoporosis FoundationVitamin D Available from: http://www.iofbonehealth.org/vitamin-d-0Accessed April 5, 2013
- Serra-MajemLArancetaJSENC Working Group on Nutritional Objectives for the Spanish PopulationSpanish Society of Community NutritionNutritional objectives for the Spanish population. Consensus from the Spanish Society of Community NutritionPublic Health Nutr20014(6A1409141311918491
- Food and Agriculture Organization of the United Nations (FAO)Human Vitamin and Mineral Requirements: Report of a Joint FAO/WHO Expert Consultation Bangkok, ThailandRomeFAO2001 Available from: ftp://ftp.fao.org/es/esn/nutrition/Vitrni/pdf/TOTAL.pdfAccessed March 11, 2013
- VaqueiroMBareMAntonEHypovitaminosis D associated to low sun exposure in the population over 64 years oldMed Clin (Barc)20071298287291 Spanish17878021
- VaqueroMPSánchez-MunizFJCarbajalAGarcía-LinaresMCGarcía-FernándezMCGarcía-AriasMTMineral and vitamin status in elderly persons from Northwest Spain consuming an Atlantic variant of the Mediterranean dietAnn Nutr Metab200448312513315133316
- Pérez-LlamasFLópez-ContrerasMJBlancoMJLópez-AzorínFZamoraSMoreirasOSeemingly paradoxical seasonal influences on vitamin D status in nursing-home elderly people from a Mediterranean areaNutrition200824541442018329850
- UbedaNBasagoitiMAlonso-AperteEVarela-MoreirasGDietary food habits, nutritional status and lifestyle in menopausal women in SpainNutr Hosp2007223313321 Spanish17612373
- Serra-MajemLRibas-BarbaLSalvadorGTrends in energy and nutrient intake and risk of inadequate intakes in Catalonia, Spain (1992–2003)Public Health Nutr20071011A1354136717988407
- Jodral-SegadoAMNavarro-AlarcónMLópez-Ga de la SerranaHLópez-MartínezMCMagnesium and calcium contents in foods from SE Spain: influencing factors and estimation of daily dietary intakesSci Total Environ20033121–3475812873398
- OrozcoLópez PZwartSalmerón MVilertGarrofa EOlmosDomínguez CINDICAD Study 2001Prediction of the total calcium intake from consumption of milk products in Spain adult population. INDICAD Study 2001Aten Primaria2004335237243 Spanish15033092
- BrownSEVitamin D and fracture reduction: an evaluation of the existing researchAltern Med Rev2008131213318377100
- SeiquerIMesíasMHoyosAMGaldóGNavarroMPA Mediterranean dietary style improves calcium utilization in healthy male adolescentsJ Am Coll Nutr200827445446218978164
- MataixJArandaPLópez-JuradoMSánchezCPlanellsELlopisJFactors influencing the intake and plasma levels of calcium, phosphorus and magnesium in southern SpainEur J Nutr200645634935416967192
- GennariLBilezikianJPOsteoporosis in menEndocrinol Metab Clin North Am200736239941917543726
- JacksonRDLaCroixAZGassMCalcium plus vitamin D supplementation and the risk of fracturesN Engl J Med2006354766968316481635
- GrantAMAvenellACampbellMKRECORD Trial GroupOral vitamin D3 and calcium for secondary prevention of low-trauma fractures in elderly people (Randomised Evaluation of Calcium Or vitamin D, RECORD): a randomised placebo-controlled trialLancet200536594711621162815885294