Abstract
Background
To investigate the effect of frailty on the long-term prognosis of elderly patients with acute myocardial infarction (AMI).
Methods
The data of 238 AMI patients (aged ≥75 years) were retrospectively reviewed. They were divided into two groups according to the Modified Frailty Index (mFI): frailty group (mFI≥0.27, n=143) and non-frailty group (mFI<0.27, n=95). The major adverse cardiovascular and cerebrovascular events (MACEs) and Kaplan–Meier survival curves of the two groups were compared. Multivariate Cox regression analysis was used to identify the risk factors for MACEs.
Results
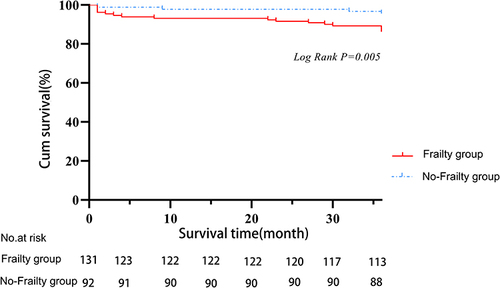
The frailty group showed a significantly older age as well as a higher N-terminal proB-type natriuretic peptide level, Global Registry of Acute Coronary Events score, and CRUSADE bleeding score compared with the non-frailty group (P<0.05). A significantly greater proportion of patients with combined heart failure, atrial fibrillation, comorbidity, and activities of daily living score of <60 was also observed in the frailty group compared with the non-frailty group (P<0.05). At 36 months after AMI, the frailty group vs the non-frailty group showed a significantly poorer survival (log-rank P=0.005), higher incidence of MACEs (50.35 vs 29.47, P=0.001), higher overall mortality rate (20.98% vs 7.37%, P=0.006), higher 30-day mortality rate (13.99% vs 5.26%, P=0.033), higher major bleeding rate (14.69% vs 5.26, P=0.018), and lower repeat revascularization rate (2.10% vs 8.42%, P=0.03). Frailty, type 2 diabetes, and N-terminal proB-type natriuretic peptide ≥1800 pg/mL were independent risk factors for MACEs.
Conclusion
Frailty is an independent risk factor affecting the long-term prognosis of elderly patients with AMI.
Introduction
With the aging of the population worldwide, the proportion of elderly patients with cardiovascular diseases (CVDs) is gradually increasing. A recent epidemiological report by the American Heart Association indicates that the prevalence of CVDs is 75–77% in people aged 60–79 years old and 89–90% in people aged over 80 years old.Citation1 Acute myocardial infarction (AMI) is one of the most severe CVDs. Elderly patients with AMI often have multiple comorbidities, a longer hospital stay, and a worse prognosis compared to young patients.Citation2 However, age is not the only factor affecting the prognosis of patients with AMI. A study by Rizzuto et al has revealed that AMI leads to decreased physiological function in elderly patients.Citation3–5 Frailty, which refers to a clinical state of increased vulnerability and reduced stress resistance resulting from the age-associated decline in physical and cognitive reserve and function, is a reliable indicator for decreased physiological function. The clinical manifestations of frailty include multisystem dysfunction, chronic inflammatory status, cachexia, and muscle loss. How frailty affects the prognosis of elderly patients with AMI warrants further investigation. A study comprising a large sample size of AMI patients aged 65 years and older showed that approximately 1/6 of the patients exhibited frailty.Citation6 Among AMI patients aged 75 years and above, the prevalence of frailty was reported to be between 35% and 48%.
Frailty often coexists with CVDs due to their common pathophysiological mechanisms. Persistent, chronic, low-grade inflammation in patients with frailty has been identified as a key contributor to the development of atherosclerotic CVDs.Citation7 Increasing evidence has demonstrated that frailty not only leads to an increased incidence of multiple CVDs but also affects the choice of treatment options and disease prognosis. Therefore, frailty has been used as a reliable indicator for anesthesia and surgery risk assessment in elderly patients.Citation8,Citation9 It also has been recognized as an independent predictor for a poor prognosis in elderly patients with AMI and heart failure.Citation10–13 However, most studies have focused on the effects of frailty on in-hospital durations and the one-year mortality rate in elderly patients with AMI, and the follow-up time is short.Citation14,Citation15 In the present study, we investigated the effect of frailty on the long-term prognosis, mostly the occurrence of major adverse cardiovascular and cerebrovascular events (MACEs), in elderly patients with AMI using a simple frailty assessment tool.
Materials and Methods
Study Population
In this retrospective study, the clinical data of patients who were diagnosed with type 1 AMI and hospitalized in the Department of Cardiology, Beijing Chaoyang Hospital, between May 2017 and October 2019 were obtained from the electric medical record system and reviewed. The diagnosis of type 1 AMI was in accordance with the American College of Cardiology, the American Heart Association, the European Society of Cardiology, and the World Heart Federation criteria. Patients who were aged ≥75 years old, treated either with medications alone or with invasive therapy, and with complete hospitalization and follow-up data were qualified for screening. The exclusion criteria were as follows: (1) incomplete demographic or clinical data; (2) death during hospitalization; (3) combined with malignant tumors, severe hepatic or renal insufficiency, or immune disorders. This study was reviewed and approved by the Ethics Committee of Beijing Chaoyang Hospital. All methods were performed in accordance with the relevant guidelines and regulations. Written informed consent was waived by the ethical committee in accordance with the national legislation and the institutional requirements. All data were anonymized and kept confidential, in compliance with the ethical guidelines of the Declaration of Helsinki.
Methods
The Modified Frailty Index (mFI) was used to stratify the patients based on their level of frailty. It includes 11 variables: history of diabetes mellitus; changes in daily activity; lung problems; history of congestive heart failure; history of myocardial infarction; history of percutaneous coronary intervention (PCI), cardiac surgery, or angina; hypertension; peripheral vascular disease; clouding or delirium; transient ischemic attack; and cerebrovascular accident with deficit. The presence of each variable equals 1 point, and the total points are divided by 11 to obtain the final mFI score (range: 0–1.0). An mFI of ≥0.27 is considered frailty.Citation16 The Charlson Comorbidity Index (CCI) was used to assess comorbidity. A CCI of ≥2 indicates comorbidity.Citation17 The Barthel index was applied to evaluate the activities of daily living (ADL).Citation18 MACEs included all-cause death, recurrence of myocardial infarction, stroke, major hemorrhage, repeat revascularization, and hospitalization because of heart failure.Citation19,Citation20 Major hemorrhage was defined as meeting one of the following criteria: (1) fatal bleeding; (2) symptomatic bleeding in a critical area or organ, such as intracranial, intraductal, intraocular, retroperitoneal, intraarticular, or fascial compartment syndrome; (3) bleeding resulting in a decrease in the hemoglobin level of ≥20 g/L (1.24 mmol/L), or resulting in transfusion of two or more units of whole blood or red blood cells. The primary endpoint of this study was a MACE.
Statistical Analysis
SPSS 25.0 software was used for all data analyses. All continuous variables were tested for normality. Normally distributed data were expressed as the mean±standard deviation and compared by the independent samples t-test. Categorical data were expressed as a number and percentage, and compared by the chi-squared test. The cumulative survival rate of patients in both groups was plotted by the Kaplan–Meier method and compared using the Log rank test. Multivariate Cox regression analysis including the following factors was performed to identify the influencing factors for MACEs: age, body mass index (BMI), atrial fibrillation, heart failure, blood glucose levels, creatinine levels, left ventricular ejection fraction (LVEF)<50%, comorbidity, ADL score<60, N-terminal proB-type natriuretic peptide (NT-proBNP)≥1800 pg/mL, CRUSADE score>50, and GRACE score>140. A P-value of less than 0.05 was considered statistically significant.
Results
Basic Demographic and Clinical Characteristics
A total of 238 elderly patients with AMI were recruited, with a mean age of 81.17±4.30 years old. There were 113 (47.47%) males. The patients were then divided into the frailty (n=143, 60.08%) and non-frailty (n=95, 39.91%) groups based on their mFI. The basic demographic and clinical characteristics of the two groups are shown in . The prevalence of frailty was 60.08%, with a higher prevalence in women than in men (56.64% vs 43.36%, P=0.145). There was no significant difference in sex, history of smoking, type 2 diabetes (T2DM), hypertension, myocardial infarction, rate of ST-segment elevation myocardial infarction (STEMI) or PCI, or the length of hospitalization stay between the two groups (all P>0.05). However, the patients with frailty showed a significantly older age and higher blood glucose levels, creatinine levels, number of cases with NT-proBNP≥1800 pg/mL, GRACE score, and CRUSADE score in comparison with the non-frailty group (all P<0.05). The proportion of patients combined with heart failure, atrial fibrillation, comorbidity, and an ADL score of <60 was significantly higher, while BMI and LVEF were significantly lower in the frailty group vs the non-frailty group (all P<0.05).
Table 1 Basic Demographic and Clinical Characteristics
Vascular Lesions
Among the 238 patients, 85 underwent PCI (non-frailty group: n=35, frailty group: n=51). There was no significant difference in the proportion of patients receiving emergency PCI or elective PCI, or with triple vessel disease or left main coronary lesions between the two groups (all P>0.05) ().
Table 2 Vascular Lesions
MACEs
All clinical events that occurred in the in-hospital and out-of-hospital phases were registered, with a mean follow-up time of 31.98±10.92 months. A total of 100 MACEs occurred, with an incidence rate of 41.15%. As shown in , the incidence of MACEs was greater in the frailty group than in the non-frailty group (50.35% vs 29.47%, P<0.05). The frailty group also showed a significantly greater incidence of all-cause death (20.98% vs 7.37%, P<0.05;) 30-day mortality (13.99% vs 5.26%, P<0.05), and major hemorrhage (14.69% vs 5.26, P<0.05) as well as a lower incidence of repeat revascularization (2.10% vs 8.42%, P<0.05) compared with the non-frailty group. There was no significant difference in death after 30 days, recurrence of myocardial infarction, stroke, or hospitalization due to heart failure between the two groups (all P>0.05).
Table 3 Follow-Up and MACEs
Cox Regression Analysis of MACEs
Multivariate Cox regression analysis was then performed to identify the influencing factors for the primary endpoint MACE. The characteristics that were significantly different between the two groups were included (ie, age, BMI, atrial fibrillation, heart failure, comorbidity, blood glucose levels, creatinine levels, NT-proBNP≥1800 pg/mL, LVEF<50%, ADL score<60, GRACE score>140, and CRUSADE score>50). The results showed that frailty, T2DM, and NT-proBNP≥1800 pg/mL were independent risk factors for MACEs ().
Table 4 Cox Regression Analysis of MACEs
Discussion
The prevalence of frailty has been gradually increasing in recent years with the growth of the aging population worldwide. In China, approximately 7–10% of the elderly in the communities are frail, and the number is even higher in hospitals.Citation21 Research teams from Japan and Spain have reported that the prevalence of frailty in elderly patients with AMI is 25–58%.Citation22,Citation23 Current available frailty assessment scales include the Fried Frailty Syndrome Criteria, the Rockwood Frailty Index, the Clinical Frailty Scale (CFS), the Frailty Index (FI), the Frailty Screening Questionnaire, the FRAIL scale, and the mFI. Currently, the most commonly used assessment tools for frailty in clinical settings are the Fried Frailty Syndrome Criteria, the CFS, and the FI. The CFS is the preferred screening tool, while the FI is the optimal assessment tool. The CFS is typically the preferred screening tool, while the FI serves as the optimal assessment tool.Citation24 Due to the extensive number of FI entries and the multidomain assessment nature of the mFI, it serves as a better predictor of mortality rate, disability rate, and hospitalization rate compared to the FI, with better diagnostic accuracy.Citation25 Therefore, mFI was used in this study. The prevalence of frailty was 60.1% in this cohort, with a higher prevalence in women than in men. Gender differences may have resulted from biological, psychosocial, and behavioral factors. Women often exhibit a higher prevalence of “non-life-threatening” chronic diseases, and the long-term mortality rate for women with frailty is lower than that of men, a phenomenon often referred to as the “frailty paradox”.Citation26 The discrepancies among different studies may be due to different assessment tools and varied disease spectrums of the enrolled population.Citation27
Frailty has been shown to increase the morbidity and mortality in patients with CVDs. It is also an independent risk factor for a variety of MACEs, such as death, stroke, heart failure readmission, and postoperative cardiac complications.Citation27–30 CVDs, in turn, exacerbate the progression of frailty. A recent study by Tashiro et al has demonstrated that 29.5% of the patients with STEMI and older than 80 years old experienced progression of frailty.Citation31 They exhibited more severe illness, worse cardiac function, and increased dependency on mechanical circulatory support compared with those without frailty. In a meta-analysis including 274,976 elderly patients with AMI, the prevalence of frailty was increased after PCI, and the frailty group showed increased mortality, hemorrhage, and rehospitalization.Citation32 Another study, in which patients with non-STEMI received invasive therapy and were followed for 5 years, has reported that frailty was independently associated with all-cause mortality, myocardial infarction, stroke, repeat revascularization, and significant major hemorrhage.Citation33 In the present study, the patients in the frailty group were older and had a lower BMI, a higher GRACE score and CRUSADE score, a higher incidence of comorbidity and atrial fibrillation, poorer cardiac function, and a higher risk of hemorrhage and death in comparison with those in the non-frailty group. However, the proportions of patients with STEMI, different vascular lesions, and PCI treatment did not significantly differ between the two groups. These findings were different from the results of previous studies, which showed a lower rate of invasive treatment in STEMI patients (≥65 years) with frailty.Citation11 These discrepancies may be explained by the different ages of the enrolled population, different classifications of heart attack, and different assessment tools for frailty.
Our study revealed that frailty significantly affected both the short-term and long-term prognoses in patients with AMI. The survival rate was significantly lower in the frailty group than in the non-frailty group, implying that frailty may have an adverse effect on the prognosis of patients. Furthermore, we found an increased incidence of MACEs, all-cause death, 30-day mortality, and major hemorrhage in the frailty group, which may be explained by the fact that frail patients are often combined with multiple comorbidities and therefore given more medications, possibly leading to more adverse drug reactions and making them less likely to receive guideline-recommended drug therapy. There is a discrepancy between guidelines and the actual clinical care for acute coronary syndrome, with frail older adults being significantly less likely to receive guideline-indicated treatments, including PCI (6.7–43.7% vs 30.4–69.5%).Citation34,Citation35 Our study showed that PCI did not significantly differ between the two patient groups; however, patients in the frailty group exhibited a worse prognosis. Previous evidence has revealed a lower proportion of frail patients undergoing complete revascularization, lower utilization of statins and angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, and a higher frequency of adverse drug reactions.Citation5 Patients with AMI often require anticoagulation and antithrombotic therapy for 12 months, and frail patients have at a higher risk of bleeding.Citation36 Consequently, these patients are more likely to experience interruptions in antithrombotic drug therapy due to adherence or bleeding. The risk of hemorrhage and thrombosis should be evaluated in AMI patients with frailty. In AMI patients with frailty, it is crucial to carefully consider the benefits and risks of vascular intervention. The incidence of repeat revascularization was significantly less in the frailty group than in the non-frailty group, possibly because patients with frailty have a reduced physiological function and thus are more prone to undergo invasive examinations and treatments, which may lead to a series of complications. Thus, both the European Society of Cardiology and the American Heart Association underscore the significance of evaluating frailty and comorbidities in the management of older patients with acute coronary syndrome.Citation15
Our Cox regression analysis showed that frailty, T2DM, and NT-proBNP≥1800 pg/mL were independent risk factors for MACEs. Although there was a significant difference in the proportion of patients with a history of heart failure between the two groups, it did not affect MACEs in the multifactorial regression analysis, as it was not identified as an independent risk factor for MACEs. However, the NT-proBNP levels were associated with the severity of heart failure and were therefore correlated with MACEs. Patients with diabetes mellitus tend to have combined multibranch vasculopathy or diffuse vasculopathy; therefore, they are more susceptible to recurrent thrombotic events or ischemic heart failure. Patients with diabetes mellitus often exhibit concurrent multivessel disease or diffuse vascular disease, making them more vulnerable to recurrent thrombotic events or ischemic heart failure. Thus, early diagnosis and intervention of frailty may improve their survival.
The limitations of the present study should be acknowledged. First, this was a single-center study with a small sample size. Second, only retrospective analyses were performed. Third, the prognostic impact of these drugs was not evaluated. Future prospective, multicenter studies are needed to further evaluate the prognosis of this population.
Conclusions
In conclusion, the current study identified frailty as an independent risk factor for the long-term prognosis of elderly patients with AMI. This information may facilitate the development of clinical interventions for frailty and therefore improve the prognosis of these patients.
Abbreviations
CVD, cardiovascular disease; AMI, acute myocardial infarction; MACEs, major adverse cardiovascular events; mFI, Modified Frailty Index; STEMI, ST-segment elevation acute myocardial infarction; PCI, percutaneous coronary intervention; BMI, body mass index; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TC, total cholesterol; TG, triglyceride; NT-proBNP, N-terminal B-type natriuretic peptide precursor; LVEF, left ventricular ejection fraction; LVEDD, left ventricular end-diastolic diameter; GRACE, Global Registry of Acute Coronary Events.
Ethics Approval and Informed Consent
This study was reviewed and approved by the Ethics Committee of Beijing Chaoyang Hospital. All methods were performed in accordance with the relevant guidelines and regulations. The requirement for informed consent was waived by the Ethics Committee of Beijing Chaoyang Hospital because of the retrospective nature of the study. All data were anonymized and kept confidential, in compliance with the ethical guidelines of the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
Data Sharing Statement
The datasets generated and analyzed during the current study are not publicly available due to limitations of ethical approval involving the patient data and anonymity but are available from the corresponding author on reasonable request.
Additional information
Funding
References
- Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021;143:e254–e743. doi:10.1161/cir.0000000000000950
- Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi:10.1093/eurheartj/ehx393
- Rizzuto D, Melis RJF, Angleman S, Qiu C, Marengoni A. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. 2017;65:1056–1060. doi:10.1111/jgs.14868
- Chen X, Mao G, Leng SX. Frailty syndrome: an overview. Clin Interv Aging. 2014;9:433–441. doi:10.2147/cia.s45300
- Bebb O, Smith FG, Clegg A, Hall M, Gale CP. Frailty and acute coronary syndrome: a structured literature review. Eur Heart J Acute Cardiovasc Care. 2018;7:166–175. doi:10.1177/2048872617700873
- Dodson JA, Hochman JS, Roe MT, et al. The association of frailty with in-hospital bleeding among older adults with acute myocardial infarction. JACC Cardiovasc Interv. 2018;11(22):2287–2296. doi:10.1016/j.jcin.2018.08.028
- Conte M, Petraglia L, Poggio P, et al. Inflammation and cardiovascular diseases in the elderly: the role of epicardial adipose tissue. Front Med. 2022;9:844266. doi:10.3389/fmed.2022.844266
- Rodrigues MK, Marques A, Umeda IIK, Lobo DML, Oliveira MF. Pre-frailty status increases the risk of rehospitalization in patients after elective cardiac surgery without complication. J Card Surg. 2020;35:1202–1208. doi:10.1111/jocs.14550
- Zazzara MB, Vetrano DL, Carfì A, Onder G. Frailty and chronic disease. Panminerva Med. 2019;61:486–492. doi:10.23736/s0031-0808.19.03731-5
- Damluji AA, Huang J, Bandeen-Roche K, et al. Frailty among older adults with acute myocardial infarction and outcomes from percutaneous coronary interventions. J Am Heart Assoc. 2019;8:e013686. doi:10.1161/jaha.119.013686
- Patel A, Goodman SG, Yan AT, et al. Frailty and outcomes after myocardial infarction: insights from the CONCORDANCE registry. J Am Heart Assoc. 2018;7:e009859. doi:10.1161/jaha.118.009859
- Llaó I, Ariza-Solé A, Sanchis J, et al. Invasive strategy and frailty in very elderly patients with acute coronary syndromes. EuroIntervention. 2018;14:e336–e342. doi:10.4244/eij-d-18-00099
- Murali-Krishnan R, Iqbal J, Rowe R, et al. Impact of frailty on outcomes after percutaneous coronary intervention: a prospective cohort study. Open Heart. 2015;2:e000294. doi:10.1136/openhrt-2015-000294
- Anand A, Cudmore S, Robertson S, et al. Frailty assessment and risk prediction by GRACE score in older patients with acute myocardial infarction. BMC Geriatr. 2020;20:102. doi:10.1186/s12877-020-1500-9
- Ekerstad N, Javadzadeh D, Alexander KP, et al. Clinical frailty scale classes are independently associated with 6-month mortality for patients after acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2022;11:89–98. doi:10.1093/ehjacc/zuab114
- Li B, Meng X, Zhang X, Hai Y. Frailty as a risk factor for postoperative complications in adult patients with degenerative scoliosis administered posterior single approach, long-segment corrective surgery: a retrospective cohort study. BMC Musculoskelet Disord. 2021;22:333. doi:10.1186/s12891-021-04186-9
- Villacampa-Fernández P, Navarro-Pardo E, Tarín JJ, Cano A. Frailty and multimorbidity: two related yet different concepts. Maturitas. 2017;95:31–35. doi:10.1016/j.maturitas.2016.10.008
- Pashmdarfard M, Azad A. Assessment tools to evaluate Activities of Daily Living (ADL) and Instrumental Activities of Daily Living (IADL) in older adults: a systematic review. Med J Islam Repub Iran. 2020;34:33. doi:10.34171/mjiri.34.33
- D’Errigo P, Seccareccia F, Barone AP, et al. Effectiveness of invasive reperfusion therapy and standard medical treatment in AMI. Acta Cardiol. 2010;65:645–652. doi:10.1080/ac.65.6.2059861
- Liu Q, Shi RJ, Zhang YM, et al. Risk factors, clinical features, and outcomes of premature acute myocardial infarction. Front Cardiovasc Med. 2022;9:1012095. doi:10.3389/fcvm.2022.1012095
- Ma L, Tang Z, Chan P, Walston JD. Novel Frailty Screening Questionnaire (FSQ) predicts 8-year mortality in older adults in China. J Frailty Aging. 2019;8:33–38. doi:10.14283/jfa.2018.38
- Nishihira K, Yoshioka G, Kuriyama N, et al. Impact of frailty on outcomes in elderly patients with acute myocardial infarction who undergo percutaneous coronary intervention. Eur Heart J Qual Care Clin Outcomes. 2021;7:189–197. doi:10.1093/ehjqcco/qcaa018
- García-Blas S, Bonanad C, Fernández-Cisnal A, et al. Frailty scales for prognosis assessment of older adult patients after acute myocardial infarction. J Clin Med. 2021;10(18):4278. doi:10.3390/jcm10184278
- Liang YD, Zhang YN, Li YM, et al. Identification of frailty and its risk factors in elderly hospitalized patients from different wards: a Cross-Sectional Study in China. Clin Interv Aging. 2019;14:2249–2259. doi:10.2147/cia.S225149
- Testa G, Curcio F, Liguori I, et al. Physical vs. multidimensional frailty in older adults with and without heart failure. ESC Heart Fail. 2020;7:1371–1380. doi:10.1002/ehf2.12688
- Park C, Ko FC. The science of frailty: sex differences. Clin Geriatr Med. 2021;37:625–638. doi:10.1016/j.cger.2021.05.008
- Udell JA, Lu D, Bagai A, et al. Preexisting frailty and outcomes in older patients with acute myocardial infarction. Am Heart J. 2022;249:34–44. doi:10.1016/j.ahj.2022.03.007
- Damluji AA, Chung SE, Xue QL, et al. Frailty and cardiovascular outcomes in the National Health and Aging Trends Study. Eur Heart J. 2021;42:3856–3865. doi:10.1093/eurheartj/ehab468
- Shrauner W, Lord EM, Nguyen XT, et al. Frailty and cardiovascular mortality in more than 3 million US veterans. Eur Heart J. 2022;43:818–826. doi:10.1093/eurheartj/ehab850
- Liu X, Tou NX, Gao Q, Gwee X, Wee SL, Ng TP. Frailty and risk of cardiovascular disease and mortality. PLoS One. 2022;17:e0272527. doi:10.1371/journal.pone.0272527
- Tashiro H, Tanaka A, Takagi K, et al. Incidence and predictors of frailty progression among octogenarians with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Arch Gerontol Geriatr. 2022;102:104737. doi:10.1016/j.archger.2022.104737
- Yu Q, Guo D, Peng J, et al. Prevalence and adverse outcomes of frailty in older patients with acute myocardial infarction after percutaneous coronary interventions: a systematic review and meta-analysis. Clin Cardiol. 2023;46(1):5–12. doi:10.1002/clc.23929
- Ratcovich H, Beska B, Mills G, et al. Five-year clinical outcomes in patients with frailty aged ≥75 years with non-ST elevation acute coronary syndrome undergoing invasive management. Eur Heart J Open. 2022;2:oeac035. doi:10.1093/ehjopen/oeac035
- Ekerstad N, Swahn E, Janzon M, et al. Frailty is independently associated with short-term outcomes for elderly patients with non-ST-segment elevation myocardial infarction. Circulation. 2011;124:2397–2404. doi:10.1161/circulationaha.111.025452
- Alonso salinas GL, Sanmartín Fernández M, Pascual Izco M, et al. Frailty is a short-term prognostic marker in acute coronary syndrome of elderly patients. Eur Heart J Acute Cardiovasc Care. 2016;5:434–440. doi:10.1177/2048872616644909
- Alonso Salinas GL, Sanmartín Fernández M, Pascual Izco M, et al. Frailty predicts major bleeding within 30days in elderly patients with acute coronary syndrome. Int J Cardiol. 2016;222:590–593. doi:10.1016/j.ijcard.2016.07.268