Abstract
Background
Surgeons are increasingly faced with consultation for intervention in residents of geriatric centers or in patients who suffer from end stage medical disease. We review our experience with consult services dedicated to the needs of these frail patients.
Study design
Patients were prospectively followed after being evaluated by three different geriatric surgical consult services: Group 1 was based at a geriatric center associated with a tertiary medical center, Group 2 was based at a community geriatric center, and Group 3 was based with an hospital-based service for ambulatory patients with end stage congestive heart failure.
Results
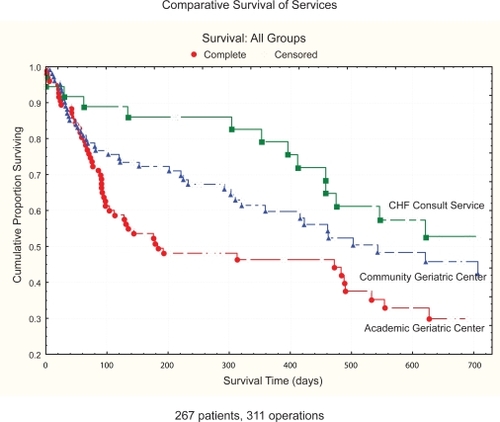
A total of 256 frail elderly patients underwent of 311 general surgical procedures ranging from major abdominal and vascular procedures to minor procedures such as debridement of decubitus ulcers, long-term intravenous access, enterostomy and enteral tube placement. Almost half of the surgical volume in Group 1 and 3 were ‘maintenance’ (decubitus debridement, long term intravenous or stomal or tube care); all of Group 2 were for treatment of decubiti. There was minimal morbidity and mortality from surgery itself, and overall one year survival for Groups 1, 2, and 3 was 46%, 60%, and 79%, respectively. Multivariate analysis showed that each group had its own unique indicators of decreased survival: Group 1 dementia and coronary artery disease, in Group 2 gender and coronary artery disease, and Group 3, gender alone. Age, number of comorbid illnesses, and type of surgery (major vs minor) were not significant indicators.
Conclusions
This is the first review of the role of dedicated surgical consult services which focused on residents of geriatric centers and frail elderly. Conditions routinely encountered in this population such as dementia, end stage disease, multiple comorbidities, polypharmacy, decreased functional and nutritional status are not frequently encountered by general surgeons. But the surgery is safe, and survival data is comparable to those in geriatric centers who did not undergo surgery. A multidisciplinary team approach gives the most effective care, with a primary goal of palliation.
Introduction
As our population continues to age, elderly patients will develop surgical disease. While much has been published on results of surgical procedures performed on elderly patients, these reports usually conclude that the “healthy” elderly, with good physiologic reserve, can survive to lead functional lives.Citation1 Typically, age itself is not a predictor of survival-active comorbid illnesses and emergency surgeries are much more powerful indicators.
Not much is known about the surgical outcomes in the frail elderly. In general, frailty has been defined as “a state of reduced physiologic reserve associated with increased susceptibility to disability”.Citation2 While criteria are being developed to stratify frailty,Citation3 in this paper we define frailty as patients with severe medical disability- residents of geriatric centers or patients with end stage medical disease. Almost all of these patients have significantly diminished physiologic reserves, poor nutritional status, significant comorbidities, and mental and physical disabilities.
The general surgeon must be aware of the issues present in this population to provide appropriate care. These include unfamiliar primary diagnoses (dementia, inability to perform basic activities of daily living, end stage congestive heart failure), and operations with palliative, not curative, goals.
The purpose of this paper is to update and review our experience in establishing three different dedicated geriatric consult services. We originally reported our experience with nursing home patients associated with an academic medical center.Citation4 We now review this experience and add data from patients we treated at a community based nursing home, and from a unique experience with a frail population of patients cared for by a dedicated congestive heart failure service. We report the patient demographics of a these populations, the type and severity of surgical diseases encountered, procedures peformed, and overall survival after consultation. We also analyze independent variables such as age, gender, presence of coronary artery disease (CAD), significant comorbidity, and their effect on survival within this population.
Methods
Data was prospectively obtained from three separate cohort studies examining the utility of a general surgical consult service dedicated to providing comprehensive care to elderly and frail patients.
The first cohort (Group 1) has been previously publishedCitation4 and consisted of residents in a geriatric nursing home closely associated with an academic medical center who were referred for general surgical intervention. These patients were followed longitudinally from 1991–1994. Detailed demographic information was obtained including admission diagnosis, consult diagnosis, comorbidities and medications. Information was obtained regarding surgical interventions, and death or discharge from the geriatric facility.
The second cohort of patients (Group 2) consisted of patients residing in a community nursing home that were referred to a surgical consult service established at Albert Einstein College of Medicine from 1995–1997. The bulk of these patients were referred for decubitus care. These patients were prospectively studied and overall survival was analyzed as well as the effect of independent variables such as age, gender, presence of CAD, presence of dementia, and location and severity of ulcer on survival.
The third cohort of patients (Group 3) consisted of ambulatory patients who were followed by the Albert Einstein College of Medicine Heart Failure Group who were referred for elective general surgery. These patients represent a particular subset of the geriatric population since they have a significant comorbidity (congestive heart failure [CHF]), and represent an ambulatory population who are frail. These patients were followed prospectively from May 1995 to June 2000. Patient information was obtained regarding demographics, New York Heart Association (NYHA) functional class, comorbid conditions, CHF medications, ejection fraction and social history. Comorbid conditions were defined as significant illness in other organ systems aside from cardiac dysfunction. The endpoints of this study were either death or the termination date of the follow-up period.
For survival statistics, data was entered into a computer database for analysis (Statistica, Statsoft, Tulsa, OK). Survival analysis was first determined for individual groups by Kaplan–Meier product limit estimation. Within each group, univariate analysis of variables was performed by the non-parametric log-rank test for censored data. For determination of risk factors influencing survival, multivariate modeling by Cox proportional hazard model was used. Statistical significance was defined as p < 0.05.
Results
Group 1: Academic geriatric center patients referred for surgical care
This cohort was previously publishedCitation4 and gives a picture of the types of patients referred for consultation at geriatric centers associated with academic medical centers.
Demographics
This cohort consisted of a total of 153 patients, with the mean age of 72.9 ± 1.1 years, and followed for an average of 14.5 ± 0.6 months (range 0–24 months). A total of 168 procedures were performed in 117 patients; the distribution of types is depicted in (Group 1). Polypharmacy was observed in most of the patients; only 30% were on no medications.
Table 1 Comparison of operative procedures done in patients referred to geriatric surgical consultation services
Survival
The 30-day mortality rate following all surgical interventions was 8.5%. Using Kaplan–Meier product limit estimations, the one-year actuarial survival rate for this cohort was 46% and the two-year survival rate was 33% (). Multivariate factors that affected survival are depicted in ). There was no difference in survival when patients were stratified by gender, by major or minor surgery, or by the presence of an active do not resuscitate order.
Table 2 Comparison of multivariate analysis of variables affecting survival
Table 3 Tools for comprehensive geriatric assessment that can be employed by dedicated consultation services
Group 2: Community geriatric center patients referred for surgical care
This cohort gives a picture of the types of patients referred for surgical consultation from community geriatric centers.
Demographics
There were of 105 nursing home patients referred to the consult service, all for debridement of chronic decubitus ulcers. The mean age of this cohort was 75 ± 1.3 year. Seventy percent were female, a higher percentage compared to Group 1. These patients were followed from January 1995 to August 1997 for a mean ±SEM of 10.9 ± 1.0 months (range 0–36 months). Thirty-four percent suffered from CAD, 31% had diabetes, 21% respiratory disease, and 9% from renal disease.
Most decubiti were debrided at the bedside in the nursing facility. Thirty-three percent were extremity decubiti, 27% trunk, and 17% were on both the extremity and trunk, and 23% were not specified.
Survival
Most surgeries in this group were minor. We observed one- and two-year actuarial survival rates to be 60% and 42.7%, respectively (). Univariate analysis demonstrated that in this population, gender and the presence of coronary artery disease significantly affected overall survival, but age greater than 70, presence of dementia or comorbid illness did not. Multivariate analysis confirmed this ().
Group 3: Heart failure patients referred for elective general surgery
This cohort gives a picture of the types of patients referred from specialized hospital-based consult services of ambulatory frail patients.
Demographics
This cohort consisted of 45 patients referred to surgery from a population of 600 patients with severe CHF managed by a dedicated service. Their average age was 65.3 years (median 67) and 38% were women. The average NYHA class of CHF at first enrollment in cohort was 2.9 ± 0.1, at the time of surgical intervention was 3.34 ± 0.12, and at final follow up for survivors was 3.16 ± 0.12. The mean Goldman scoreCitation5 for this cohort was 25.1 ± 2.1. At the time of surgical intervention the mean left ventricular ejection fraction was 29.6 ± 1.7%. Patients were followed from May 1995–June 2000, for a mean ±SEM 16.3 ± 2.2 months (range 0–64 months).
Seventy seven percent of this cohort had additional significant comorbid conditions including diabetes, hypertension or renal insufficiency. As we observed in the academic geriatric center patients (Group 1) polypharmacy was common, but in this group the medications were focused on the primary cardiac disease. Most patients (70%) were on an angiotensin-converting enzyme (ACE) inhibitor and diuretic, while 35% were on triple therapy: an ACE inhibitor, digoxin, and diuretic. Ten to thirty percent were on calcium channel blockers, β-blockers, or antiarrythmics.
Thirty-four patients in this group underwent 38 procedures. Fifteen major abdominal procedures were performed in this cohort (). These included eight colectomies for cancer, one intestinal resection for chronic gastrointestinal bleed, open drainage of a psoas abscess, laparoscopic cholecystectomy and one laparoscopic Nissen fundoplication for gastrointestinal reflux. In this group there were three complications (20%) and one postoperative death (6.7%). The latter was in a patient who underwent uneventful right colectomy for cancer and suffered a fatal complication from a balloon thermodilution catheter on postoperative day 1.
Twenty-three procedures were performed under local anesthesia, the most common being ‘maintenance’ surgery-central venous access for inotropic support (). Other procedures performed under local anesthesia included transanal excision of a rectal cancer, hemorrhoidectomy, feeding jejeunostomy, and a vein excision for thrombophlebitis. There were two complications in this group (9.1%) and no deaths.
Survival
One- and two-year survival for the entire group was 78.5% and 48.8%, respectively (). Univariate analysis showed that age greater than 65 years, male gender, the presence of any other comorbid illness, use of tobacco or ethanol and race adversely affected survival (). Multivariate analysis of risk revealed that of all the factors, only female gender was the factor predictive of increased survival.
Importantly, as we observed in Group 1, when patients in this group underwent major abdominal surgery with general anesthesia were compared to those who had local procedures (predominantly chronic central venous catheters placed for home inotropic therapy), survival rates were similar.
Discussion
This report updates our experience in establishing dedicated geriatric surgical consult services to provide care for the frail elderly: a rapidly growing segment of the general surgical population. A total of 311 procedures performed in 267 patients is reported; the largest to date. The study has three potential flaws. First, there is a selection bias since the patients, while frail, were healthy enough to be referred for elective surgery. This is a potential strength since by not addressing acute illnesses we were able to give a more accurate picture of nonemergency surgery in the frail. Second, the three groups studied seemed very different. While their venues did differ, from a geriatric perspective, all the patients were frail elderly.
Observations
The important observation was that common general surgical disease occurs in patients who reside in geriatric centers and who have end stage medical disease (). While ‘maintenance care’ (drainage/feeding tubes, decubitus care, chronic intravenous access) made up a significant proportion of the procedures (>45% in Group 1; 100% in Group 2; 32% in group 3), other common surgical procedures such as biliary, abdominal, hernia, breast surgery were also performed, with minimal morbidity and mortality.
The observed survival for patients in these groups was poor. For patients who were residents in academic and community geriatric centers the one year survival was 50%–60%. For those outpatients with controlled, but significant CHF, survival was better at nearly 80%. This difference is likely attributed to the differences in frailty of the populations. Specifically, the institutionalized patients have less mobility, more dementia, and more chronic conditions necessitating ‘maintenance care’. The patients with end stage CHF had comorbid illnesses, but they had no dementia and were outpatients.
Univariate analysis in each group showed that multiple factors contributed to survival, such as age, dementia, gender, CAD, length of stay in the geriatric center, number of comorbidities, polypharmacy, and even use of tobacco or ethanol in patients with CHF. When subjected to the more rigorous multivariate analysis, most variables – including age – fell out of statistical significance (), a phenomenon seen in many other geriatric studies. In the academic geriatric center, coronary artery disease, and dementia were significant predictors of survival: gender was not even significant using univariate analysis.Citation4 But, in the community geriatric center and CHF outpatient group, gender and CAD was a predictor. The type of surgery (major vs minor) or the presence of a do-not-resusicate (DNR) order had no impact on life expectancy. The small group size of the CHF group (Group 3) does preclude accurate statistical analysis, but the fact remains that these frail patients did do well after major elective surgery (only one death out of 15).
Issues for surgeons who take care of these patients
Geriatric centers
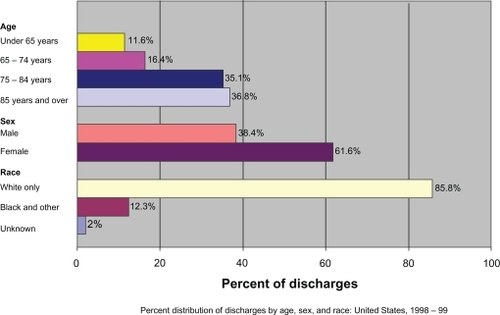
In 1999 there were 2.5 million discharges from geriatric centers in the US.Citation6 Ninety percent of these residents were over the age of 65. Approximately 37% of these residents were over the age of 85. Kemper and colleagues showed that the expected use of geriatric centers is high: 36%, 60%, and 71% for patients grouped 75–84 years, 85–94 years, and greater than 95 years, respectively. It is expected that 43% of persons over 60 years of age will eventually use a nursing home. Thirty-two percent will reside there for over three months, 24% for over one year, and 9% for over five years.Citation7
demonstrates the current demographic profile of US geriatric center residents. Frailty is common in this group. Nearly half of these residents are admitted from a medical facility and one of the most common causes for discharge from a nursing facility was for admission to a hospital. A significant proportion of this elderly population will therefore require medical care, some of which will be surgical. A specialized geriatric general consult service for these frail patients would provide a forum to coordinate for both maintenance care and major abdominal and vascular procedures.
Frailty
Frailty is a chronic condition, but can also be the result of an acute change in functional reserve. Criteria for frailty have been established: age greater than 85 years, dependence in one or more activities of daily living, presence of three or more comorbid conditions and presence of one of more geriatric syndromes (such as delirium, incontinence, osteoporosis, falls risk and failure to thrive).Citation7 Patients who reside in geriatric centers and outpatients with end stage medical diseases (such as CHF) should also be considered frail.
Frail elderly are encountered in the hospital, geriatric center, and outpatient setting. Understanding the frail elderly can help prevent the progression of disability and reduce the risk of unplanned hospitalizations, nursing home admissions and reductions in cost of medical care delivery to this population. While patients over 65 years of age account for 31% of acute care hospital admissions and 45% of hospital expenditures for adults,Citation8,Citation9 frail elderly require more medical resources.Citation10
The median survival of a frail elderly patient has been estimated to be in excess of two years. Surgical intervention should therefore not be aimed at increasing survival but rather maintain quality of remaining life.Citation11 This paradigm is of particular importance to general surgeons who are not all trained under this paradigm.
Congestive heart failure
The annual incidence of CHF is near 10 per 1,000 (in patients over 65), and the prevalence has increased to some 400,000 new cases each year, with at least 4–5 million people affected in the US.Citation12 This translates to 875,000 hospitalizations and 2.9 million physician visits per year. In 1993, there were 42,000 reported deaths from CHF, with an additional 219,000 deaths where CHF was a significant contributor.
While the prognosis for patients with CHF is improving, there are no accurate predictors of survival. Studies have shown that CHF patients have a greater than 50% predicted chance of living two months on the day before their actual death.Citation13–Citation15 These are patients now being referred for both minor and major surgery.
The case for focused geriatric surgery consult services
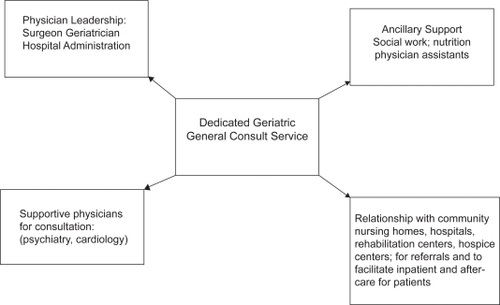
Frail and geriatric patients present with medical issues that general surgeons are not trained to recognize or treat: dementia, delirium, depression, propensity for falls, multiple medical comorbidities and polypharmacy, depressed cognition and nutrition, and problems with social support, alcohol and abuse.Citation14 The need for a dedicated multidisciplinary team approach to address these is critical ().
The earliest trial evaluating the efficacy of a hospital based geriatric evaluation unit was conducted in 1979 at the Sepulveda VA Medical Center.Citation16 Elderly patients who were assigned to the unit showed a 50% reduction in one year mortality compared with the control group, and less need for long-term care. Furthermore, the study demonstrated improved diagnostic accuracy, reduced use of medications, reduced need for institutionalization and improved functional status.
Several other clinical trials evaluating geriatric evaluation services yielded with conflicting results on survival and cost effectiveness.Citation17 But they generally concluded that geriatric units have a positive impact on elderly patients’ quality of life, examples being in “nonmedical” interventions such as cognition, depression or preventative measures.Citation18,Citation19 At the very least, a dedicated unit will efficiently implement the necessary medical, social, and economic interventions, all of which can be complicated.
Elements of the service
A multidisciplinary, integrated team can perform a comprehensive geriatric assessment that will be able to guide appropriate management, for the frail geriatric patients (). A comprehensive nonsurgical geriatric assessment includes overall health status, functional status, nutrition, cognition, socioeconomic and emotional evaluations, assessment for geriatric syndromes such as delirium, incontinence, osteoporosis, risk of fall and failure to thrive.Citation18 Once completely assessed, the role for surgery, whether curative, palliative, or maintenance, can be decided.
For this team to function, a physician leader, usually a surgeon and geriatrician, and support staff, nurses, social workers, nutritionists, psychologists, and physician extenders, are all needed. A dedicated unit with appropriate physical facilities, eg, support railings in the hallway, handicapped baths, day-rooms, signs for daily orientation, is essential.
Disclosure
The authors report no conflicts of interest in this work.
References
- PofahlWEPoriesWJCurrent status and future directions of geriatric general surgeryJ Am Geriatr Soc200351S351S35412823667
- BuchnerDMWagnerEHPreventing frail healthClin Geriatr Med199281171576567
- FerrucciLThe frailty syndrome: a critical issue in geriatric oncologyCrit Rev Oncol Hermatol200346127137
- ZenilmanMEBenderJSMagnusonTHSmithGSGeneral surgical disease in the nursing home patient: Results of a dedicated geriatric surgery consult serviceJ Am Coll Surg19961833613708925122
- GoldmanLCalderaDLNussbaumSRMultifactorial index of cardiac risk in noncardiac surgical proceduresN Engl J Med1977297845850904659
- JonesAThe National Nursing Home Survey: 1999 Summary. National Center for Health StatisticsVital Health Stat2002131521116
- KemperPMurtaughCMLifetime use of nursing home careN Engl J Med19913245956001992320
- WinogradCHGeretyMBBrownEKolodnyVTargeting the hospitalized elderly for geriatric consultationJ Am Geriatr Soc198836111311193192889
- LandefeldCSPalmerRMKresevicDMFortinskyRHKowalJA randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older adultsN Engl J Med1995332133813447715644
- FerrucciLGuralnikJMCavazziniCThe frailty syndrome: a critical issue in geriatric oncologyCrit Rev Oncol Hematol20034612713712711358
- RepettoLVenturinoAFratinoLGeriatric oncology: a clinical approach to the older patient with cancerEur J Cancer20033987088012706355
- EichornEJPrognosis determination in heart failureAm J Med20011101435
- LevensonJWMcCarthyEPLynnJThe last six months of life for patients with congestive heart failureJ Am Geriatr Soc2000485 SupplS101S10910809463
- TenoJMHarrellFEKnausWPrediction of survival for older hospitalized patients: The HELP survival modelJ Am Geriatr Soc2000485 SupplS516S524
- BalducciLBegheCCancer and age in the USACrit Rev Oncol Hemotol200137137145
- RubensteinLZWielandDEnglishPJosephsonKSayreJAAbrassIBThe Sepulveda VA Geriatric Evaluation Unit: data on four-year outcomes and predictors of improved patient outcomesJ Am Geriatr Soc1984325035126736515
- EllisGLanghornePComprehensive geriatric assessment for older hospital patientsBr Med Bull200571455915684245
- BalducciLBegheCThe application of the principles of geriatrics to the management of the older person with cancerCrit Rev Oncol Hematol20003514715410960797
- ReubenDBBorokGMWolde-TsadikGRandomized trial of comprehensive geriatric assessment in the care of hospitalized patientsN Engl J Med1995332134513507715645