Abstract
Purpose
Social isolation and depression have an impact on cognitive frailty. However, the underlying mechanisms between these variables have not been well defined. This study aims to investigate the mediating role of depressive symptoms in the association between social isolation and cognitive frailty among older adults in China.
Methods
From Mar 2023 to Aug 2023, a cross-sectional study was conducted with 496 community-dwelling older adults aged ≥60 years in Nanjing, Jiangsu Province, China. Demographic information was collected using the General Information Questionnaire. The Lubben Social Network Scale-6 (LSNS-6), Geriatric Depression Scale 15-item (GDS-15), Montreal Cognitive Assessment (MoCA), Clinical Dementia Rating (CDR), and FRAIL scale were used for the questionnaire survey. Multiple linear regression and binary logistic regression were utilized to explore the associations among social isolation, depressive symptoms, and cognitive frailty, and Bootstrap analysis was used to explore the mediating role of depressive symptoms in social isolation and cognitive frailty.
Results
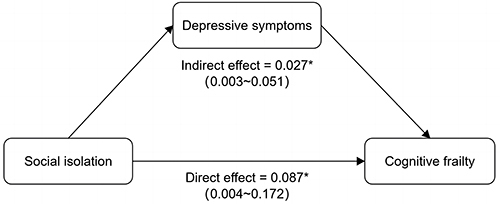
Linear regression results revealed that social isolation was positively associated with depressive symptoms (β = 0.873, p < 0.001). Logistic regression analysis showed that social isolation (OR = 1.769, 95% CI = 1.018~3.075) and depressive symptoms (OR = 1.227, 95% CI = 1.108~1.357) were significantly associated with cognitive frailty. Mediation analysis demonstrated that depressive symptoms significantly mediated the relationship between social isolation and cognitive frailty, with an indirect effect of 0.027 (95% CI = 0.003~0.051), and the mediating effect accounted for 23.6% of the total effect.
Conclusion
Social isolation is associated with cognitive frailty in community-dwelling older adults, and depressive symptoms partially mediate the effect between social isolation and cognitive frailty. Active promotion of social integration among older individuals is recommended to enhance their mental health, reduce the incidence of cognitive frailty, and foster active aging.
Introduction
Cognitive frailty is a heterogeneous clinical condition characterized by the simultaneous presence of physical frailty and mild cognitive impairment (MCI), without meeting the criteria for a dementia diagnosis.Citation1 Cognitive frailty is associated with a higher risk of adverse outcomes, including functional disability, poor quality of life, hospitalization, dementia, and mortality,Citation2,Citation3 compared to the risks associated with frailty or MCI alone. Previous research has found that cognitive frailty may be reversible.Citation4 Therefore, investigating the influencing factors of cognitive frailty and implementing early identification and intervention strategies can be instrumental in averting or delaying the adverse effects associated with cognitive frailty.
The development of cognitive frailty in older adults is influenced by various factors, encompassing demographic characteristics, lifestyle, and diseases.Citation5,Citation6 Recently, there has been a growing focus on understanding the impact of social factors on cognitive frailty. Social isolation is defined as an objective state of reduced social interaction, limited social network size, and lack of social support.Citation7 Social isolation has emerged as a global public health concern, which seriously threatens the physical and mental health of older persons.Citation8 Research has indicated that social isolation is associated with an increased risk of physical frailty and cognitive impairment in older adults. A prospective study conducted in Japan revealed an increased risk of frailty in older adults associated with friendship-related social isolation.Citation9 Pan et alCitation10 identified a bidirectional temporal association between social isolation and frailty in Chinese older individuals. Nie et alCitation11 discovered that older adults with smaller social networks and lesser social activity participation showed poorer cognitive function. Moreover, a Spanish cohort study demonstrated that baseline social isolation correlated with cognitive decline three years later in middle-aged and older adults above 50.Citation12 While social isolation may elevate the risk of cognitive frailty in older adults, the underlying psychological processes and mechanisms linking the two remain inadequately understood.
Depression is one of the most prevalent mental disorders with a high prevalence among the global older population. Previous studies have validated indicators of social isolation that have an impact on depression, including being single, living alone, weak social networks, and reduced social activities.Citation13 Results from longitudinal studies have also shown an association between social isolation and increased risk of depression in older adults.Citation14 Social relationships play an important role in the regulation of mood in individuals, and positive social relationships endow older adults with enhanced access to diverse social resources and support, to buffer them against stress and negative life events, counteracting the onset of depressive symptoms or mitigating the negative effects.Citation15 Conversely, older adults with social isolation often encounter a deficiency in both material and emotional support and show higher rates of depression and depressive symptoms.Citation16
In addition, depression stands out as an independent influencing factor for cognitive frailty. A meta-analysis has underscored the role of depression in escalating the risk of cognitive frailty among older adults.Citation17 According to Zhou et alCitation18 research, older persons with depressive symptoms had a 4.218-fold increased chance of developing cognitive frailty compared to those without depressive symptoms. The co-occurrence of depression and cognitive frailty may be attributed to shared pathophysiological pathways, which include oxidative stress, chronic inflammation, cerebrovascular disorders, and mitochondrial dysfunction.Citation19 Therefore, we further hypothesize that depressive symptoms mediate the relationship between social isolation and cognitive frailty in community-dwelling older individuals.
A synthesis of the existing literature indicates that social isolation and depression both have an impact on cognitive frailty. However, the collective influence of these factors on cognitive frailty and their underlying mechanisms remains unknown. To bridge this knowledge gap, the primary objective of this study is to elucidate the relationship between social isolation, depressive symptoms, and cognitive frailty in community-dwelling older adults, with a specific emphasis on investigating the mediating role of depressive symptoms in the link between social isolation and cognitive frailty. This investigation seeks to identify the pivotal factors contributing to cognitive frailty, providing insights for formulating preventive and intervention measures for cognitive frailty among community-dwelling older adults.
Methods
Study Design and Participants
This cross-sectional study was conducted from March 2023 to August 2023. Older residents from three communities in Nanjing, China were recruited through convenience sampling. Potential participants were recruited through posters on community bulletin boards and leaflets distributed to residents, coordinated by community staff. The inclusion criteria were participants who: (1) Age ≥ 60 years old; (2) Residing in the area for at least 6 months; (3) Voluntary participation in the study. The exclusion criteria were those who: (1) Self-reported disease history of neurological and psychiatric disorders, such as Alzheimer’s disease and other forms of dementia, Parkinson’s disease, epilepsy, schizophrenia, bipolar disorder, or Clinical Dementia Rating (CDR) score ≥ 1; (2) Severe hearing, vision impairment or communication difficulties; (3) Inability to cooperate with this study. A total of 600 older people were initially recruited for the study. Among them, 58 refused to participate, 3 reported a history of neurological and psychiatric disorders, 10 were aged < 60, and 9 with impaired vision or hearing. A total of 520 participants were assessed, and 19 participants with missing data and 5 CDR scores ≥ 1 were further excluded, the final analysis included data from 496 participants. Approval for this study was obtained from the Ethical Review Committee of Nanjing Hospital of Traditional Chinese Medicine (Approval No. KY2022004) and complied with the Declaration of Helsinki.
Data Collection
Five researchers (all postgraduate nursing students) attended the neuropsychological scale assessment training at Nanjing Brain Hospital and obtained relevant qualifications. Unified training on communication methods and assessment processes was carried out before the start of the survey to ensure the consistency of methods. All information was collected by the researchers using a structured questionnaire through face-to-face, one-to-one personal interviews. At the time of the survey, the purpose and methods of the study were systematically described to the participants, all participants were assured that their responses would be anonymous and confidential, and their written informed consent was obtained. At the end of the survey, a small gift was given as compensation to participants who completed this survey.
Measurements
Cognitive Frailty
The overall cognitive function was evaluated using the Beijing version of the Montreal Cognitive Assessment (MoCA),Citation20 comprising seven dimensions: visuospatial and executive functions, naming, attention, language, abstraction, delayed memory, and orientation. Scores ranged from 0 to 30, with scores ≥26 classified as normal. To mitigate the educational bias of the MoCA, an adjustment was made by adding one point for individuals with ≤12 years of education (provided that the total score did not exceed 30 points after this adjustment). MoCA is widely employed in prior research, and the Beijing version exhibits robust reliability and validity.Citation21
The Clinical Dementia Rating (CDR)Citation22 was utilized to evaluate cognitive status, including memory, orientation, judgment and problem-solving ability, social ability, and personal self-care ability. Dementia severity was assessed through interviews with patients or their family members. Memory is the primary domain, while the other five comprise a composite score. The scoring standard was 0 points for normal cognition and 0.5 for suspected dementia. Mild, moderate, and severe dementia were 1, 2, and 3 points, respectively.
Physical frailty status was assessed using the FRAIL scale,Citation23 consisting of five questions: (1) Fatigue: Have you felt fatigued in the past month? (2) Low resistance: Is it difficult to climb one flight of stairs without aid and the help of others? (3) Ambulation: Is it difficult to walk 100 meters without aid and the help of others? (4) Illnesses: Do you suffer from five or more diseases? (5) Loss of weight: Have you lost ≥5% of your body weight in the past year? Each component was scored 0–1, with “yes” earning a score of “0” and “no” earning a score of “1”. Total scores ranged from 0 to 5, indicating no frailty (0), pre-frailty (1–2), and frailty (3–5). Dong et alCitation24 validated the FRAIL scale for Chinese older adults, demonstrating great reliability and validity.
According to the definition of cognitive frailty by Ruan et al,Citation25 individuals with physical frailty or pre-frailty accompanied by mild cognitive impairment, are classified as cognitive frailty. Therefore, the evaluation criteria of cognitive frailty in this study are as follows: FRAIL score 1–5, MoCA score < 26, CDR=0.5, and excluding dementia diagnosis.
Social isolation
Lubben Social Network Scale-6 (LSNS-6)Citation26 was employed to measure the social isolation of individuals. The scale includes 2 dimensions: family network and friend network, with 3 items in each dimension. The 3 questions of family network are: “How many relatives do you see or contact at least every month?” “How many relatives do you think you can turn to for help?” And “How many relatives can you talk to about personal matters?” In the three questions of the friend dimension, the word “relative” is replaced with the word “friend”. Each item was scored from 0 to 5 points, with the total score ranging from 0 to 30 points. The lower the score, the higher the likelihood of existing social isolation; a score below 12 is considered an indicator of social isolation, the scale has high reliability and validity in the Chinese population.Citation27
Depressive Symptoms
The Chinese version of the 15-item Geriatric Depression Scale (GDS-15)Citation28 was utilized to evaluate depressive symptoms among older adults. This 15-item scale is a reliable and valid tool for this purpose. Each item required participants to indicate “yes” or “no” based on their personal circumstances, with scores assigned as 1 or 0 respectively. The total score ranges from 0 to 15, with higher scores indicating greater levels of depression; scores exceeding 5 suggest the presence of depression symptoms. The Chinese version of the GDS-15 showed satisfactory reliability and validity.Citation29
Covariates
According to previous studies, we included as covariates confounders that may influence the relationship between social isolation and cognitive frailty.Citation30–32 The demographic characteristics considered in this study encompassed gender, age, educational level, average monthly income, and marital status. Marital status was dichotomized into married and single categories, with the latter including individuals who were unmarried, widowed, or divorced. Health status variables included body mass index (BMI), chronic diseases, and sleep quality. BMI was calculated by dividing weight (kg) by the square of height (m). The resulting BMI values were categorized as falling within the normal range (18.5~23.9), while values below 18.5 or above 23.9 were considered abnormal.Citation33 Self-reported chronic diseases included hypertension, diabetes, heart disease, cerebrovascular disease, lung diseases, malignant tumors, kidney diseases, and arthritis. The number of chronic diseases was divided into 0 kind, 1 kind, and ≥ 2 kinds. Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI), which comprises seven dimensions: subjective sleep quality, sleep onset latency, total sleep time, sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. The total PSQI score ranges from 0 to 21, with a score of ≥8 indicating the presence of sleep disturbances.Citation34
Statistical Methods
The statistical analysis for all data was performed using Stata 16.0 software. Categorical variables were presented as n (%), and inter-group comparisons were conducted using the χ2 test. Continuous variables were expressed as mean ± standard deviation (SD), and inter-group comparisons were performed with the t-test. To investigate the role of depressive symptoms in the association between social isolation and cognitive frailty, we utilized the mediation model proposed by MacKinnon and Dwyer.Citation35 Initially, multiple linear regression analysis was employed to examine the relationship between social isolation and depressive symptoms. Subsequently, binary logistic regression analysis was used to assess the associations among social isolation, depressive symptoms, and cognitive frailty. Finally, the Bootstrap analysis method was applied to explore the mediating effect of depressive symptoms in the relationship between social isolation and cognitive frailty. The presence of a depressive symptoms-mediated effect was considered if the Bootstrap 95% confidence interval did not include 0, and the regression coefficients were statistically significant. All statistical tests were conducted at a significance level of α=0.05.
Results
General Characteristics of Participants
A total of 496 participants were included in our study, there were 237 men and 259 women. The participants ranged in age from 60 to 91 years, with a mean age of 70.05±6.9 years. Their characteristics are summarized in . Among these participants, the incidence of social isolation was 24.8%, the mean GDS-15 score was 2.31±2.25, the mean FRAIL score was 0.68±0.72, the mean MoCA score was 24.25±3.42, and the incidence of cognitive frailty was 18.5%.
Table 1 Description and Univariate Analysis of Cognitive Frailty Among Community-Dwelling Older Adults (N = 496)
Compared to older adults without cognitive frailty, those with cognitive frailty are older, less educated, have lower average monthly incomes, more chronic diseases, and more sleep disorders (p < 0.05).
Mediation Analysis of Depressive Symptoms in the Relationship Between Social Isolation and Cognitive Frailty
A multiple linear regression model was constructed with depressive symptoms as the dependent variable and social isolation as the independent variable. The results indicated that, after adjusting for confounding factors such as gender, age, educational level, average monthly income, marital status, BMI, number of chronic diseases, and sleep disorder, social isolation demonstrated a positive correlation with depressive symptoms (β = 0.873, p < 0.001). In other words, older individuals experiencing social isolation were more prone to have depressive symptoms, as shown in . All variance inflation factor (VIF) values were below 10, indicating the absence of multicollinearity in our dataset.
Table 2 Linear Regression Analysis of the Relationship Between Social Isolation and Depressive Symptoms
Upon adjusting for covariates, logistic regression Model 1 was developed with social isolation as the independent variable and cognitive frailty as the dependent variable. Subsequently, logistic regression Model 2 was established, integrating social isolation and depressive symptoms as independent variables, with cognitive frailty as the dependent variable. The findings from Model 1 revealed that social isolation had a significant direct predictive effect on cognitive frailty (OR = 2.132, 95% CI = 1.253~3.628). Results from Model 2 indicated that, even after adjusting social isolation, depressive symptoms significantly predicted cognitive frailty (OR = 1.227, 95% CI = 1.108~1.357). The predictive effect of social isolation on cognitive frailty was still significant, but the predictive effect was attenuated (OR = 1.769, 95% CI = 1.018~3.075). It indicated that depressive symptoms mediated the influence of social isolation on cognitive frailty ().
Table 3 Logistic Regression Analysis of the Relationship Between Social Isolation, Depressive Symptoms and Cognitive Frailty
Bootstrap analysis showed that after adjusting the control variables, the direct effect of social isolation on cognitive frailty was 0.087 (95% CI = 0.004~0.172). The indirect effect of social isolation on cognitive frailty through depressive symptoms was 0.027 (95% CI = 0.003~0.051), and the mediating effect of depressive symptoms accounted for 23.6% of the total effect of social isolation on cognitive frailty, see and for details.
Table 4 Bootstrap Analysis of the Mediating Effects of Depressive Symptoms
Discussion
This study is the first to examine the correlation between social isolation and cognitive frailty and to investigate the mediating influence of depressive symptoms in this relationship. The findings indicate that social isolation has a direct impact on cognitive frailty and also indirectly influences the occurrence of cognitive frailty through the mediating role of depressive symptoms. The outcomes of this study offer potential insights for the formulation and implementation of intervention strategies and measures targeting cognitive frailty.
In this study, 92 community-dwelling older adults with cognitive frailty accounted for 18.5%. The result is higher than the prevalence of cognitive frailty reported in mainland China (8.9%)Citation36 and Japan (2.1%).Citation37 However, it is lower than older adults in Malaysia (39.6%)Citation38 and Spain (23.6%).Citation39 A meta-analysis reported large variations in prevalence across countries, ranging from 2.5% to 50%.Citation40 The difference in the prevalence of cognitive frailty may be related to the different operational definitions of cognitive frailty and the lack of uniformity in assessment tools, economic level, medical technology and cross-cultural differences between countries may also contribute to differences.Citation41 Our study further revealed that age, educational level, average monthly income, number of chronic diseases, and sleep disorder were independently associated with cognitive frailty. Additionally, the findings of our study reveal a social isolation occurrence rate of 24.8% among community-dwelling older adults, consistent with a recent meta-analysis result,Citation42 this research identified a global prevalence of 25% for social isolation among community-dwelling older adults. These results indicate that social isolation has become a prevalent issue among older individuals. It underscores the imperative to intensify attention on social isolation in older individuals and relevant policies should be established in time to maintain the social network of older adults.
This study indicates social isolation is associated with an increased risk of cognitive frailty in older adults. Although direct evidence regarding the relationship between social isolation and cognitive frailty is currently lacking, some studies have separately reported associations of social isolation with frailty and cognitive dysfunction.Citation9–12 These pieces of evidence indirectly support our study findings. Social isolation-induced dysregulation of circadian rhythms, oxidative stress, and neuroendocrine dysregulation may lead to sarcopenia, resulting in the loss of muscle strength and decreased physical activity, ultimately contributing to the onset of frailty.Citation43 In addition, social isolation increases an individual’s susceptibility to life stressors, and increased glucocorticoid secretion due to maladaptive responses to stress has been shown to cause hippocampal damage that increases the risk of cognitive impairment.Citation44 According to the Cognitive Reserve Theory,Citation45 social networks can stimulate the formation of neuronal networks in the brain that resist structural damage to the brain associated with age or disease and delay cognitive decline. Older adults experiencing social isolation lack social contact and fail to receive sufficient emotional and cognitive stimulation, impacting cognitive reserve and leading to cognitive decline. Furthermore, older individuals with social isolation face a lack of material and informational support and are more likely to engage in poor health behaviors (such as smoking, physical inactivity, and poor diet quality),Citation46 increasing the risk of cardiovascular disease and malnutrition, indirectly affect cognitive decline or frailty onset.
This study further explores the psychological mechanisms underlying the impact of social isolation on the occurrence of cognitive frailty through depressive symptoms. Our research indicates a positive correlation between social isolation and depressive symptoms, consistent with previous research findings. Family and friend networks are the most important social networks for individuals.Citation47 The family network is an essential source for older adults to seek social support, and the lack of support and contact from family members can lead to negative emotions such as loneliness and helplessness, which can induce depressive symptoms. In contrast, the composition of friend networks is more diverse and provides more social activities. Older adults who suffer from friend isolation have limited social contacts and lack peer support from friends, which may also have adverse effects on mental health.Citation48 This study also revealed that depressive symptoms were significantly associated with cognitive frailty, consistent with previous research findings.Citation17,Citation18 Depression and cognitive frailty may share common pathophysiological mechanisms. Older individuals with depression exhibit elevated levels of cytokines such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP),Citation49 while research has confirmed an association between cognitive frailty and increased levels of inflammatory biomarkers.Citation50 Additionally, excessive activation of the hypothalamic-pituitary-adrenal (HPA) axis leads to elevated cortisol levels, decreased levels of insulin-like growth factor-1 (IGF-1), and testosterone, potentially serving as an endocrine mechanism underlying depression and cognitive frailty.Citation51 Finally, mitochondrial dysfunction can be observed in many neurodegenerative diseases and depression, which may be an important pathway in the pathophysiology of both depression and cognitive frailty.Citation19
This study provides a new direction for the prevention and management of cognitive frailty. Interventions aimed at improving social isolation in older individuals may help to prevent or delay the occurrence and development of depression and cognitive frailty. It is recommended that community workers regularly assess the social network status of older adults, dynamically monitor the mental health of those with weak social relationships, and provide professional psychological counseling services when necessary, to reduce or prevent the occurrence of depressive symptoms. In addition, through measures such as organizing various social and cultural activities and setting up mutual help groups, social contacts and interactions among older individuals are facilitated to avoid persistent social isolation, thereby promoting mental health and reducing the incidence of cognitive frailty. With the rapid development and availability of digital technology, the use of the internet (such as email, social media, and video calls) provides additional avenues and opportunities to alleviate social isolation among older adults. Studies have confirmed that training in digital technology can enhance the digital literacy of older persons and promote their social contacts.Citation52,Citation53 Technology-based interventions may be one of the effective solutions for addressing cognitive frailty associated with social isolation. Communities should actively leverage their educational role in bridging the digital divide among older adults, providing guidance on the application of Internet technologies, and facilitating their enhanced participation in social interactions.
This study has the following limitations: Firstly, the cross-sectional design employed in this study prevents the inference of causal relationships among social isolation, depressive symptoms, and cognitive frailty. Secondly, as the application of convenience sampling and the sample size is relatively small, prevalence estimates are subjected to sampling bias, which limits the generalizability of the findings. Thirdly, this study used a variety of questionnaires for data collection, which may lead to bias in recall and reporting. Lastly, we only examined one mediating variable, necessitating further exploration of other potential variables associated with cognitive frailty.
Conclusion
In conclusion, the study found that social isolation is associated with cognitive frailty in community-dwelling older adults, and depressive symptoms partially mediate the relationship between social isolation and cognitive frailty. These findings provide guidance for the development of targeted interventions in the future, measures aimed at alleviating social isolation and depressive symptoms may help to prevent the occurrence of cognitive frailty.
Ethics Approval and Informed Consent
This study was performed in line with the principles of the Declaration of Helsinki, and was approved by the Ethical Review Committee of Nanjing Hospital of Traditional Chinese Medicine (Approval No. KY2022004, 28 Feb 2022). Informed consent was obtained from all subjects involved in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
Data Sharing Statement
The data supporting this study’s findings are available on request from the corresponding author.
Additional information
Funding
References
- Kelaiditi E, Cesari M, Canevelli M, et al. Cognitive frailty: rational and definition from an (I.A.N.A./I.A.G.G.) International Consensus Group. J Nutr Health Aging. 2013;17(9):726–734. doi:10.1007/s12603-013-0367-2
- Tang KF, Teh PL, Lee SWH. Cognitive Frailty and Functional Disability Among Community-Dwelling Older Adults: a Systematic Review. Innov Aging. 2023;7(1):igad005. doi:10.1093/geroni/igad005
- Chen B, Wang M, He Q, et al. Impact of frailty, mild cognitive impairment and cognitive frailty on adverse health outcomes among community-dwelling older adults: a systematic review and meta-analysis. Front Med Lausanne. 2022:9. doi:10.3389/fmed.2022.1009794
- Solfrizzi V, Scafato E, Lozupone M, et al. Additive Role of a Potentially Reversible Cognitive Frailty Model and Inflammatory State on the Risk of Disability: the Italian Longitudinal Study on Aging. Am J Geriatric Psychiatry. 2017;25(11):1236–1248. doi:10.1016/j.jagp.2017.05.018
- Corral-Pérez J, Casals C, Ávila-Cabeza-de-Vaca L, et al. Health factors associated with cognitive frailty in older adults living in the community. Front Aging Neurosci. 2023:15. doi:10.3389/fnagi.2023.1232460
- Lu S, Xu Q, Yu J, et al. Prevalence and possible factors of cognitive frailty in the elderly with hypertension and diabetes. Front Cardiovasc Med. 2022:9. doi:10.3389/fcvm.2022.1054208
- Nicholson NR. Social isolation in older adults: an evolutionary concept analysis. J Adv Nurs. 2009;65(6):1342–1352. doi:10.1111/j.1365-2648.2008.04959.x
- Tragantzopoulou P, Giannouli V. Social isolation and loneliness in old age: exploring their role in mental and physical health. Psychiatriki. 2021;32(1):59–66. doi:10.22365/jpsych.2021.009
- Uno C, Okada K, Matsushita E, et al. Friendship-related social isolation is a potential risk factor for the transition from robust to prefrailty among healthy older adults: a 1-year follow-up study. Eur Geriatr Med. 2021;12(2):285–293. doi:10.1007/s41999-020-00422-y
- Pan C. Bidirectional Relationships and Mediating Effects Between Social Isolation, Loneliness, and Frailty in Chinese Older Adults. Innov Aging. 2024;8(3):igae019. doi:10.1093/geroni/igae019
- Nie Y, Richards M, Kubinova R, et al. Social networks and cognitive function in older adults: findings from the HAPIEE study. BMC Geriatr. 2021;21(1):570. doi:10.1186/s12877-021-02531-0
- Lara E, Caballero FF, Rico‐Uribe LA, et al. Are loneliness and social isolation associated with cognitive decline? Int J Geriatr Psychiatry. 2019;34(11):1613–1622. doi:10.1002/gps.5174
- Holt-Lunstad J, Steptoe A. Social isolation: an underappreciated determinant of physical health. Curr Opin Psychol. 2022;43:232–237. doi:10.1016/j.copsyc.2021.07.012
- Noguchi T, Saito M, Aida J, et al. Association between social isolation and depression onset among older adults: a cross-national longitudinal study in England and Japan. BMJ Open. 2021;11(3):e045834. doi:10.1136/bmjopen-2020-045834
- Ditzen B, Heinrichs M. Psychobiology of social support: the social dimension of stress buffering. Restor Neurol Neurosci. 2014;32(1):149–162. doi:10.3233/RNN-139008
- Herbolsheimer F, Ungar N, Peter R. Why Is Social Isolation Among Older Adults Associated with Depressive Symptoms? The Mediating Role of Out-of-Home Physical Activity. Int J Behav Med. 2018;25(6):649–657. doi:10.1007/s12529-018-9752-x
- Zhang T, Ren Y, Shen P, et al. Prevalence and Associated Risk Factors of Cognitive Frailty: a Systematic Review and Meta-Analysis. Front Aging Neurosci. 2022;13:755926. doi:10.3389/fnagi.2021.755926
- Zhou Q, Zhou J, Min K, et al. The prevalence and determinants of cognitive frailty among institutionalized older adults. J Nurs Sci. 2020;35(09):88–92.
- Zou C, Yu Q, Wang C, et al. Association of depression with cognitive frailty: a systematic review and meta-analysis. J Affect Disord. 2023;320:133–139. doi:10.1016/j.jad.2022.09.118
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: a Brief Screening Tool For Mild Cognitive Impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi:10.1111/j.1532-5415.2005.53221.x
- Wang X, Zhang J, Chen C, et al. The association between physical activity and cognitive function in the elderly in rural areas of northern China. Front Aging Neurosci. 2023:15. doi:10.3389/fnagi.2023.1168892
- Morris JC. Clinical Dementia Rating: a Reliable and Valid Diagnostic and Staging Measure for Dementia of the Alzheimer Type. Int Psychogeriatr. 1997;9(S1):173–176. doi:10.1017/S1041610297004870
- van Kan GA, Rolland YM, Morley JE, et al. Frailty: toward a Clinical Definition. J Am Med Dir Assoc. 2008;9(2):71–72. doi:10.1016/j.jamda.2007.11.005
- Dong L, Qiao X, Tian X, et al. Cross-Cultural Adaptation and Validation of the FRAIL Scale in Chinese Community-Dwelling Older Adults. J Am Med Dir Assoc. 2018;19(1):12–17. doi:10.1016/j.jamda.2017.06.011
- Ruan Q, Yu Z, Chen M, et al. Cognitive frailty, a novel target for the prevention of elderly dependency. Ageing Res Rev. 2015;20:1–10. doi:10.1016/j.arr.2014.12.004
- Lubben J, Blozik E, Gillmann G, et al. Performance of an Abbreviated Version of the Lubben Social Network Scale Among Three European Community-Dwelling Older Adult Populations. Gerontologist. 2006;46(4):503–513. doi:10.1093/geront/46.4.503
- Chang Q, Sha F, Chan CH, et al. Validation of an abbreviated version of the Lubben Social Network Scale (“LSNS-6”) and its associations with suicidality among older adults in China. PLoS One. 2018;13(8):e0201612. doi:10.1371/journal.pone.0201612
- Yesavage JA, Brink TL, Rose TL, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17(1):37–49. doi:10.1016/0022-3956(82)90033-4
- Jea W. The prevalence of depressive symptoms and predisposing factors in an elderly Chinese population. Acta Psychiatr Scand. 1994;89(1):8–13. doi:10.1111/j.1600-0447.1994.tb01478.x
- Hou D, Sun Y, Liu Z, et al. A longitudinal study of factors associated with cognitive frailty in middle-aged and elderly population based on the health ecology model. J Affect Disord. 2024;352:410–418. doi:10.1016/j.jad.2024.02.014
- Ge L, Yap CW, Heng BH. Associations of social isolation, social participation, and loneliness with frailty in older adults in Singapore: a panel data analysis. BMC Geriatr. 2022;22(1):26. doi:10.1186/s12877-021-02745-2
- Fang F, Hughes TF, Weinstein A, et al. Social Isolation and Loneliness in a Population Study of Cognitive Impairment: the MYHAT Study. J Appl Gerontol. 2023;42(12):2313–2324. doi:10.1177/07334648231192053
- Hou P, Xue H, Zhang Y, et al. Mediating Effect of Loneliness in the Relationship between Depressive Symptoms and Cognitive Frailty in Community-Dwelling Older Adults. Brain Sci. 2022;12(10):1341. doi:10.3390/brainsci12101341
- Zhang C, Zhang H, Zhao M, et al. Reliability, Validity, and Factor Structure of Pittsburgh Sleep Quality Index in Community-Based Centenarians. Front Psychiatry. 2020:11. doi:10.3389/fpsyt.2020.573530
- Mackinnon DP, Dwyer JH. Estimating Mediated Effects in Prevention Studies. Eval Rev. 1993;17(2):144–158. doi:10.1177/0193841X9301700202
- Kong LL, Xie W, Dong ZY, et al. Cognitive frailty and its association with disability among Chinese community-dwelling older adults: a cross-sectional study. BMC Geriatr. 2024;24(1):189. doi:10.1186/s12877-024-04773-0
- Kim H, Awata S, Watanabe Y, et al. Cognitive frailty in community-dwelling older Japanese people: prevalence and its association with falls. Geriatr Gerontol Int. 2019;19(7):647–653. doi:10.1111/ggi.13685
- Malek Rivan NF, Shahar S, Rajab NF, et al. Cognitive frailty among Malaysian older adults: baseline findings from the LRGS TUA cohort study. Clin Interv Aging. 2019;14:1343–1352. doi:10.2147/CIA.S211027
- Corral-Pérez J, Casals C, Ávila-Cabeza-de-Vaca L, et al. Health factors associated with cognitive frailty in older adults living in the community. Front Aging Neurosci. 2023;15:1232460. doi:10.3389/fnagi.2023.1232460
- Bu Z, Huang A, Xue M, et al. Cognitive frailty as a predictor of adverse outcomes among older adults: a systematic review and meta-analysis. Brain Behav. 2021;11(1):e01926. doi:10.1002/brb3.1926
- Makri E, Giannouli V. Cross-cultural cognitive and affective differences in aging: can culture shape the expression and perception of psychopathology in old age? ENCEPHALOS. 2022;59:34–43.
- Teo RH, Cheng WH, Cheng LJ, et al. Global prevalence of social isolation among community-dwelling older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2023;107:104904. doi:10.1016/j.archger.2022.104904
- Yang J, Huang J, Yang X, et al. The association of living alone and social isolation with sarcopenia: a systematic review and meta-analysis. Ageing Res Rev. 2023;91:102043. doi:10.1016/j.arr.2023.102043
- Kim EJ, Pellman B, Kim JJ. Stress effects on the hippocampus: a critical review. Learn Mem. 2015;22(9):411–416. doi:10.1101/lm.037291.114
- Bennett DA, Schneider JA, Tang Y, et al. The effect of social networks on the relation between Alzheimer’s disease pathology and level of cognitive function in old people: a longitudinal cohort study. Lancet Neurol. 2006;5:406–412. doi:10.1016/S1474-4422(06)70417–3
- Luo J, Hendryx M. Mediation analysis of social isolation and mortality by health behaviors. Prev Med (Baltim). 2022;154:106881. doi:10.1016/j.ypmed.2021.106881
- Harasemiw O, Newall N, Shooshtari S, et al. From Social Integration to Social Isolation: the Relationship Between Social Network Types and Perceived Availability of Social Support in a National Sample of Older Canadians. Res Aging. 2018;40(8):715–739. doi:10.1177/0164027517734587
- Litwin H. The association between social network relationships and depressive symptoms among older Americans: what matters most? International Psychogeriatrics. 2011;23(6):930–940. doi:10.1017/S1041610211000251
- Cudjoe TKM, Selvakumar S, Chung SE, et al. Getting under the skin: social isolation and biological markers in the National Health and Aging Trends Study. J Am Geriatr Soc. 2022;70(2):408–414. doi:10.1111/jgs.17518
- Diniz BS, Lima-Costa MF, Peixoto SV, et al. Cognitive Frailty is Associated With Elevated Proinflammatory Markers and a Higher Risk of Mortality. Am J Geriatr Psychiatry. 2022;30(7):825–833. doi:10.1016/j.jagp.2022.01.012
- Panza F, Solfrizzi V, Sardone R, et al. Depressive and Biopsychosocial Frailty Phenotypes: impact on Late-life Cognitive Disorders. J Alzheimers Dis. 2023;94(3):879–898. doi:10.3233/JAD-230312
- Ibarra F, Baez M, Cernuzzi L, et al. A Systematic Review on Technology-Supported Interventions to Improve Old-Age Social Wellbeing: loneliness, Social Isolation, and Connectedness. J Healthc Eng. 2020;2020:2036842. doi:10.1155/2020/2036842
- Gadbois EA, Jimenez F, Brazier JF, et al. Findings From Talking Tech: a Technology Training Pilot Intervention to Reduce Loneliness and Social Isolation Among Homebound Older Adults. Innov Aging. 2022;6(5):igac040. doi:10.1093/geroni/igac040