Abstract
Background
N-terminal pro-brain natriuretic peptide (NT-proBNP) is associated with an increased risk of cardiac insufficiency, which possibly leads to heart failure. However, the relationship between resting heart rate and NT-proBNP is unclear.
Objective
This study focuses on this relativity between resting heart rate and plasma NT-proBNP levels in a surveyed community-based population.
Methods
We evaluated the relativity between resting heart rate and plasma levels of NT-proBNP in 1,567 participants (mean age 61.0 years, range 21–96 years) from a community-based population in Beijing, People’s Republic of China.
Results
In patients with high resting heart rate (≥75 beats/min), NT-proBNP was higher than in those having low resting heart rate (<75 beats/min). In multiple linear stepwise regression analysis, plasma NT-proBNP was associated with resting heart rate (partial correlation coefficient, 0.82; 95% confidence interval, 0.18–1.51; P=0.011). A subsequent subgroup analysis revealed that the association between resting heart rate and plasma NT-proBNP was strengthened in subjects over 60 years old (partial correlation coefficient 1.28; 95% confidence interval, 0.49–2.36; P=0.031); while the relativity between resting heart rate and plasma NT-proBNP was not emerged in the younger subgroup (<60 years old).
Conclusions
Resting heart rate was associated with plasma NT-proBNP in the elderly, which indicated a relationship between resting heart rate and cardiac function damage.
Introduction
Increased resting heart rate is associated with development of hypertension, atherosclerosis, sudden death, and coronary heart diseases, which all increase cardiovascular morbidity and mortality.Citation1,Citation2 In addition, increased resting heart rate is associated with oxidative stress, subclinical inflammation, sympathetic tone, and endothelial dysfunction. All of these may lead to the development of cardiac function damage.Citation3 Whether the resting heart rate is associated with cardiac function damage to the cardiovascular system is still unclear.
B-type natriuretic peptide (BNP) is a member of a four natriuretic peptide family that shares a common 17-peptide ring structure.Citation4 Circulating levels of the BNP system can help in the diagnosis of cardiovascular disease (CVD) and provide prognostic information not only in patients with heart failure but also the general population and other patient groups.Citation5 Changes over time also carry prognostic information, and studies are assessing BNP-guided treatment strategies.Citation6 Is possible to exclude the diagnosis of heart failure with the use of natriuretic peptides, but that they are not able to discriminate the two clinical and echocardiographic types of heart failure, ie, heart failure with preserved and the one with reduced ejection fraction, which must be differentiated using ultrasound.Citation7 Values of N-terminal pro-brain natriuretic peptide (NT-proBNP) are affected by age or the presence of one or several comorbidities, such as chronic renal failure, type 2 diabetes, and acute coronary syndrome.Citation8
Whether resting heart rate is associated with plasma levels of NT-proBNP in asymptomatic subjects has not been well established yet. The present study investigated the association between measures of resting heart rate and manifestations of cardiac function damage (NT-proBNP) in a community-dwelling population without overt CVD.
Materials and methods
Study population and design
This was a community-based cross-sectional study of people living in the Pingguoyuan area of the Shijingshan district in a metropolitan area of Beijing, People’s Republic of China. After routine health checkups between September 1, 2007 to January 31, 2009, 1,859 permanent residents were recruited for the study as described previously.Citation9 Of these, 31 subjects with bedridden status, mental illness, arrhythmia, and severe systemic diseases were excluded from the analysis.
Resting heart rate assessment was attempted in 1,828 subjects. Adequate measurement was either not attempted or not obtained in 86 excluded participants. A total of 141 participants with overt CVD (defined as a composite of coronary heart disease [recognized or unrecognized myocardial infarction, angina pectoris, or coronary insufficiency], cerebrovascular disease [stroke or transient ischemic attack], congestive heart failure, and intermittent claudication) were excluded. Thus, testing of cardiac biomarkers was attempted in 1,680 subjects. Among these, a total of 1,567 subjects (mean age 61 years, range 21–96 years) with available NT-proBNP results were eligible for analysis. The study was approved by the ethics committee of the Chinese People’s Liberation Army (PLA) General Hospital, and each participant provided informed consent.
Clinical data collection
Information on medical history, family history of CVD, and lifestyle was obtained through self-reporting standardized questionnaires. Anthropometrics were deployed in the clinic with participants wearing light clothing and no shoes. Height was measured in centimeters by a wall-mounted measuring tape, and weight was measured in kilograms by a digital scale. Resting heart rate was measured by cardiac auscultation for 1 minute. Tobacco smoking was defined as having smoked at least one cigarette per day for 1 year or more; one cigarette was considered to be equivalent to 1 gram of tobacco.
Systolic blood pressure (SBP) and diastolic blood pressures (DBP) were measured by well-trained staff members on the right arm of the seated participant, after at least 5 minutes of rest, with a mercury sphygmomanometer and an appropriately sized cuff. Three sequential BP measurements were obtained, and the average was used for analysis.
Biomarker variable determination
All subjects underwent full laboratory evaluation (lipid profile and liver and kidney function indices). Blood samples were obtained between 8 am and 10 am from fasting participants after they had been in the supine position for 10 to 15 minutes. Samples were centrifuged immediately, and stored at −80°C until assays were performed. Concentrations of NT-proBNP were determined with an electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany) using a Roche analyzer (Roche Diagnostics, Indianapolis, IN, USA), which has a measuring range from 5 to 35,000 pg/mL. According to the manufacturer’s information, values below the detection limit are reported as 4.99 pg/mL. Concentrations of fasting glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, homocysteine, and uric acid were determined using the Roche enzymatic assays (Roche Diagnostics GmbH) on a Roche AutoAnalyzer (Roche Diagnostics). Concentrations of high-sensitivity C-reactive protein were determined by an immunoturbidimetric assay (Siemens Healthcare Diagnostics, USA) using a Dimension RxL Max analyzer (Siemens Healthcare Diagnostics). Concentrations of serum creatinine were measured by enzymatic assay (Roche Diagnostics GmbH) on a Hitachi 7600 autoanalyser (Hitachi, Tokyo, Japan).
All testing was performed by well-trained personnel blinded to clinical data in the Department of Biochemistry of Chinese PLA General Hospital.
Definition of variables
Resting heart rate measurements were conducted in a quiet environment at stable temperature. Subjects were requested to abstain from caffeine, smoking, and alcohol for at least 12 hours before assessment was performed. Participants were studied in the supine position after resting 5 to 10 minutes.
Body mass index was calculated as weight in kilograms divided by the height in square meters (kg/m2). Hypertension was defined as a mean SBP ≥140 mmHg, a mean DBP ≥90 mmHg, or use of antihypertensive medication. Diabetes mellitus was defined as a fasting glucose ≥7.0 mmol/L, nonfasting glucose ≥11.1 mmol/L, or use of antihyperglycemic medication.Citation10 The creatinine was standardized using a calibration equation: Jaffe’s kinetic method Scr (mg/dL) =0.795 × (enzymatic method Scr [mg/dL]) +0.29.Citation11 The estimated glomerular filtration rate (eGFR) was calculated with the Chinese-modified Modification of Diet in Renal Disease equation as follows: eGFR (mL/min/1.73m2) = 175 × standardized creatinine (mg/dL)−1.234 × age (year)−0.179 × 0.79 (if female).Citation12
Statistical analysis
Continuous variables are presented as mean ± standard deviation or median and with interquartile range. Dichotomous variables are presented as numbers and percentages. The distribution test of continuous variables was performed; NT-proBNP levels were logarithmically transformed to normalize their distributions. Resting heart rate was classified into a high level group (≥75 beats/min) or a low level group (<75 beats/min). Differences in log NT-proBNP levels between the high and low resting heart rate groups were analyzed with Student’s t-tests.
We assessed the association of resting heart rate with manifestations of cardiac function damage (NT-proBNP) by means of multiple regression analysis models. NT-proBNP was treated as the dependent variable. Forward stepwise multiple regression analysis was performed to obtain the partial correlation coefficient (PR) and 95% confidence intervals (CIs). Regression models were adjusted with age and sex as independent variables (model 1) and additionally adjusted for the factors hypertension, diabetes, SBP, DBP, current smoking, body mass index, waist circumference, resting heart rate, levels of plasma fasting glucose, total cholesterol, triglyceride, and high-density lipoprotein cholesterol, eGFR as the independent variable (model 2). Model 3 was adjusted from model 2 plus use of medications.
Because age is an important determinant of NT-proBNP levels, we repeated the regression analysis on participants younger than 60 years old (n=688) and 60 years of age and older (n=879) respectively.
All statistical analyses were performed using Stata software (version 11.0, Stata Corporation, College Station, TX). A bilateral value of P<0.05 was considered significant.
Results
Characteristics
Altogether, 1,567 participants were included in the present study. The mean ± SD age of participants in the study was 61.0±11.2 years. The characteristics of the study population are summarized in .
Table 1 Characteristics of the study sample
Distribution of NT-proBNP concentrations
Among the 1,567 participants, 1,474 (94.1%) had detectable values of NT-proBNP (≥5 pg/mL). The range of detectable NT-proBNP concentrations was 5.07–3,804 pg/mL with a median value of 42.95 pg/mL (interquarile range, 1.9–81.9 pg/mL).
Resting heart rate and the presence of NT-proBNP concentrations
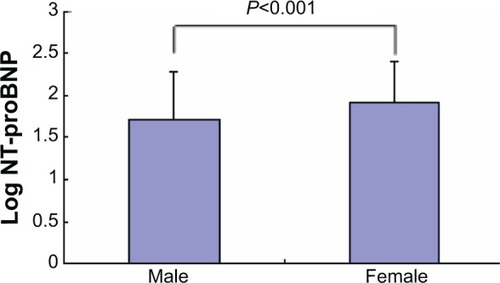
The levels of NT-proBNP in the high resting heart rate group were higher than the levels in the low resting heart rate group (P=0.002) (). The levels of NT-proBNP increased within females ().
Figure 1 Plasma Levels of log NT-proBNP in the high resting heart rate group and low resting heart rate group.
Abbreviation: NT-proBNP, N-terminal pro-brain natriuretic peptide.
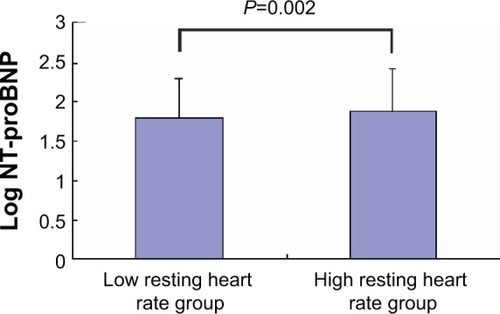
Figure 2 Plasma Levels of log NT-proBNP in male and female groups.
On univariate regression analysis, the NT-proBNP levels were significantly related to resting heart rate (P<0.01). In patients with high resting heart rates (≥75 beats/min), NT-proBNP was higher than in those having low resting heart rates (<75 beats/min). In multiple linear stepwise regression analysis, plasma NT-proBNP was associated with resting heart rate (PR, 0.82; 95% CI, 0.18–1.51; P=0.011) ().
Table 2 Relationship between resting heart rate and levels of NT-proBNP
A subsequent subgroup analysis revealed that the association between resting heart rate and plasma NT-proBNP was strengthened in subjects over 60 years old (PR, 1.28; 95% CI, 0.49–2.36; P=0.031), while the relativity between resting heart rate and plasma NT-proBNP was not emerged in the younger subgroup (<60 years old). However, in participants younger than 60 years of age, the relationship between resting heart rate (PR, −0.06; 95% CI, −0.58 to 0.60; P=0.729) and NT-proBNP levels disappeared ().
Table 3 Relationship between resting heart rate and levels of NT-proBNP for participants younger that 60 years of age and 60 years of age and older
Discussion
In this study, we demonstrated for the first time that in a community-dwelling asymptomatic population, resting heart rate was positively associated with plasma NT-proBNP levels independent of age, sex, or other risk factors. These results indicated an independent association between resting heart rate and cardiac function damage. Notably, in the predefined subgroup analysis, the association between resting heart rate and cardiac function damage was strengthened in elderly participants but not present in those younger than 60 years old.
Higher resting heart rate has been reported to be associated with oxidative stress, subclinical inflammation, higher sympathetic tone, and endothelial dysfunction. And these pathologic changes are known to promote hypertension, atherosclerosis, and coronary heart diseases.Citation1–Citation3 In the present study, we demonstrated an association between resting heart rate and levels of NT-proBNP, which is a sensitive marker for the assessment of cardiac function damage. The findings of the present study suggest that higher resting heart rate might be partly mediated by cardiac function damage.
There are several ways that resting heart rate may predispose cardiac function damage. Firstly, an increased resting heart rate may have direct detrimental effects on cardiovascular function by increasing myocardial oxygen consumption and reducing coronary blood flow.Citation10 Secondly, an increased resting heart rate can exert local haemodynamic forces that can adversely impact on the arterial wall.Citation10 In previous studies,Citation13–Citation14 pressure or volume overload were considered the major stimuli for BNP release. Thirdly, an increased resting heart rate might be a trigger for the activation of the sympathetic nervous system.Citation10 Fourthly, several prospective studies have reported resting heart rate be a risk predictor for certain specific causes of death, including CVD and non-CVD deaths. These studies include the Framingham Study, the NHANES I Epidemiologic Follow-up Study, the NIPPONDATA80 Study, and others.Citation15–Citation19 The mechanisms by which increased resting heart rate increases the risk of CVD are still largely unknown. Findings from the study of Liu et alCitation20 suggest the resting heart rate–CVD association may be related to the positive association between resting heart rate and blood pressure. Increased blood pressure might be an important trigger for BNP release.
As in previous studies,Citation21–Citation23 we found that female sex was an independent positive factor for NT-proBNP levels. Because post-menopausal women are rarely treated with oral estrogens in the People’s Republic of China,Citation24 an influence of oral estrogens on NT-proBNP levels is likely negligible.
In this study, resting heart rate was associated with cardiac function damage only in elderly participants. This difference can be attributed to a number of factors. Firstly, our study population was relatively old, with 53.1% of the participants being older than or equal to 65 years of age (range, 21–75 years; median, 60 years). Resting heart rate increases with age, the steepest rise occurs after the age of 65, resulting in strengthened cardiac function damage in older subjects. Secondly, age itself is one of the most important cardiovascular risk factors, heavily modifying the strength of the others. Thirdly, elderly subjects had a higher presence of other vascular risk factors than younger participants. These factors can interact with resting heart rate, which may increase susceptibility to cardiac function damage in this group of subjects.
The present study also has some limitations. Firstly, the present study was performed in Chinese residents from one community in Beijing; the results may not represent Chinese from other areas of the People’s Republic of China and might not be applicable to other ethnic groups. Secondly, because of the cross-sectional design and its inherent limitations, the present study cannot determine causal relationships among the factors. Therefore, our observations need confirmation in longitudinal and interventional studies. Thirdly, a significant proportion of residents were excluded because of missing or inadequate clinical and biomarker data. This is a well-known but unavoidable limitation of large epidemiological studies that may bias toward the null hypothesis because of loss of cases that presumably had more extreme values for the analyzed variables. Fourthly, the presence of sex, current smoking and potential comorbidities (such as diastolic dysfunction, left ventricular hypertrophy, hypertension, diabetes mellitus, obesity) may influence the association of resting heart rate and NT-proBNP. Although the results were adjusted for multiple covariates that might be associated with NT-proBNP levels, the possibility of residual confounding still remained.
There are several strengths to our study. Firstly, to the best of our knowledge, the present investigation is the first study evaluating the association between resting heart rate and cardiac function damage in a large community-based population. Secondly, the most sensitive detection method of cardiac function damage (NT-proBNP) and several manifestations of clinical data are included, which allows us to explore the relationship between resting heart rate and cardiac function damage.
Conclusion
In conclusion, we observed a robust, cross-sectional association between resting heart rate and NT-proBNP, which indicated a consistent positive relationship between resting heart rate and cardiac function damage, particularly in elderly subjects. However, long-term follow-up studies are needed to evaluate whether increased resting heart rate can cause manifestations such as cardiac function damage. Whether reducing the resting heart rate can have a favorable effect on cardiac function needs to be investigated further in prospective intervention studies using heart rate-lowering drugs.
Acknowledgments
This work was supported by grants from the Key National Basic Research Program of China (2012CB517503, 2013CB530804) and Nature Science Foundation of China (81270941) to P Ye and the Beijing Nova Program (Z121107002513124) to Y Bai.
Disclosure
The authors declare no conflicts of interest in this work.
References
- PalatiniPRole of elevated heart rate in the development of cardiovascular disease in hypertensionHypertension201158574575021896939
- ZhangGQZhangWHeart rate, lifespan, and mortality riskAgeing Res Rev200981526019022405
- KwonHSLimYHKimHYAssociation of ambulatory blood pressure and heart rate with advanced white matter lesions in ischemic stroke patientsAm J Hypertens201427217718324168916
- RaizadaVThakoreKLuoWMcGuirePGCardiac chamber-specific alterations of ANP and BNP expression with advancing age and with systemic hypertensionMol Cell Biochem20012161–213714011216858
- McMurrayJJAdamopoulosSAnkerSDESC Committee for Practice GuidelinesESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESCEur Heart J201233141787184722611136
- TroughtonRMichael FelkerGJanuzziJLJrNatriuretic peptide-guided heart failure managementEur Heart J2014351162424216390
- MariesLManitiuIDiagnostic and prognostic values of B-type natriuretic peptides (BNP) and N-terminal fragment brain natriuretic peptides (NT-pro-BNP)Cardiovasc J Afr201324728628924217307
- deFilippiCRChristensonRHGottdienerJSKopWJSeligerSLDynamic cardiovascular risk assessment in elderly people. The role of repeated N-terminal pro-B-type natriuretic peptide testingJ Am Coll Cardiol201055544145020117457
- BaiYYePLuoLArterial stiffness is associated with minimally elevated high-sensitivity cardiac, troponin T levels in a community-dwelling populationAtherosclerosis2011218249349821784424
- LangCCGuptaSKalraPElevated heart rate and cardiovascular outcomes in patients with coronary artery disease: Clinical evidence and pathophysiological mechanismsAtherosclerosis201021211820152981
- ZhangLZuoLXuGCommunity-based screening for chronic kidney disease among populations older than 40 years in BeijingNephrol Dial Transplant20072241093109917210584
- MaYCZuoLChenJHModified glomerular filtration rate estimating equation for Chinese patients with chronic kidney diseaseJ Am Soc Nephrol200617102937294416988059
- DanielsLBMaiselASNatriuretic peptidesJ Am Coll Cardiol200750252357236818154959
- de LemosJAMcGuireDKDraznerMHB-type natriuretic peptide in cardiovascular diseaseLancet2003362938031632212892964
- OkamuraTHayakawaTKadowakiTResting heart rate and cause-specific death in a 16.5-year cohort study of the Japanese general populationAm Heart J200414761024103215199351
- KaplanJRManuckSBClarksonTBThe influence of heart rate on coronary artery atherosclerosisJ Cardiovasc Pharmacol198710suppl 2S100S102 discussion S1032481158
- GillumRFMakucDMFeldmanJJPulse rate, coronary heart disease, and death: the NHANES I Epidemiologic Follow-up StudyAm Heart J19911211721771985358
- DrukteinisJSRomanMJFabsitzRRCardiac and systemic hemodynamic characteristics of hypertension and prehypertension in adolescents and young adults: the Strong Heart StudyCirculation2007115222122717210838
- FranklinSSPioJRWongNDPredictors of new-onset diastolic and systolic hypertension: the Framingham Heart StudyCirculation200511191121112715723980
- LiuLMizushimaSIkedaKNaraYYamoriYCardiovascular Disease and Alimentary Comparison Study GroupResting heart rate in relation to blood pressure: results from the World Health Organization-Cardiovascular Disease and Alimentary Comparison studyInt J Cardiol20101451737419446895
- GalaskoGILahiriABarnesSCCollinsonPSeniorRWhat is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease?Eur Heart J200526212269227616040618
- Costello-BoerrigterLCBoerrigterGRedfieldMMAmino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide in the general community: determinants and detection of left ventricular dysfunctionJ Am Coll Cardiol200647234535316412859
- RedfieldMMRodehefferRJJacobsenSJMahoneyDWBaileyKRBurnettJCJrPlasma brain natriuretic peptide concentration: impact of age and genderJ Am Coll Cardiol200240597698212225726
- ZhouJLLinSQShenYChenYZhangYChenFLSerum lipid profile changes during the menopausal transition in Chinese women: a community-based cohort studyMenopause2010175997100320551848
