Abstract
Background
The validity of a cardiovascular risk self-screening method was assessed. The results obtained for self-measurement of blood pressure, a point-of-care system’s assessment of lipid profile and glycated hemoglobin, and a self-administered questionnaire (sex, age, diabetes, tobacco consumption) were compared with the standard screening (gold standard) conducted by a health professional.
Methods
Crossover clinical trial on a population-based sample from Girona (north-eastern Spain), aged 35–74, with no cardiovascular disease at recruitment. Participants were randomized to one of the two risk assessment sequences (standard screening followed by self-screening or vice versa). Cardiovascular risk was estimated with the Framingham-REGICOR function. Concordance between methods was estimated with the intraclass correlation coefficient (ICC). Sensitivity, specificity, and positive and negative predictive values were estimated, considering 5% cardiovascular risk as the cutoff point. ClinicalTrials.gov Registration #NCT02373319. Clinical Research Ethic Committee of the Parc de Salut Mar Registration #2014/5815/I.
Results
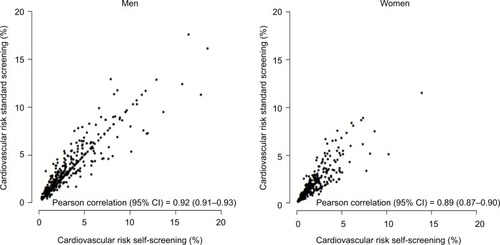
The median cardiovascular risk in men was 2.56 (interquartile range: 1.42–4.35) estimated by standard methods and 2.25 (1.28–4.07) by self-screening with ICC=0.92 (95% CI: 0.90–0.93). In women, the cardiovascular risk was 1.14 (0.61–2.10) by standard methods and 1.10 (0.56–2.00) by self-screening, with ICC=0.89 (0.87–0.90). The sensitivity, specificity, and positive and negative predictive values for the self-screening method were 0.74 (0.63–0.82), 0.97 (0.95–0.99), 0.86 (0.77–0.93), and 0.94 (0.91–0.96), respectively, in men. In women, these values were 0.50 (0.30–0.70), 0.99 (0.98–1), 0.81 (0.54–0.96), and 0.97 (0.95–0.99), respectively.
Conclusion
The self-screening method for assessing cardiovascular risk provided similar results to the standard method. Self-screening had high clinical performance to rule out intermediate or high cardiovascular risk.
Background
Cardiovascular diseases are the main cause of death in the developed world and are gaining importance in low-income countries.Citation1 Nonetheless, a substantial fall in cardiovascular disease mortality has been observed in developed countries, approximately half of which has been attributed to cost-effective evidence-based treatments used in clinical cardiology and half to the crucial role of healthy diet, increased physical activity, and decreased consumption of tobacco and alcohol.Citation2,Citation3 These key drivers are increasingly recognized as being potentially powerful, rapid, equitable, and cost-saving.Citation4
Currently, the first step in cardiovascular risk screening is the estimation of cardiovascular risk using validated risk functions.Citation5,Citation6 This procedure, usually performed in primary care settings under the supervision of health professionals, has limitations.Citation5,Citation7 For instance, there is a wide gap between expert recommendations and actual preventive practice.Citation8 Physicians have been found to have difficulty meeting the international standards even when they strongly believe that preventive care is important and that risk factors for cardiovascular disease can and should be reduced.Citation9,Citation10 Moreover, the current screening strategy may not reach young, healthy people, who are less likely to visit primary care settingsCitation11 but are also the main audience for the preventive message because cumulative exposure to cardiovascular risk factors over time precedes the clinical expression of cardiovascular diseases.
In addition, the trends in coronary heart disease mortality in the USA show a troubling contrast between the steep decrease recently observed in older populations and the small decreases in young populations.Citation12 Although the low burden of cardiovascular diseases in younger populations would make it difficult to observe dramatic decreases, the implementation of preventive programs in young people is key to reduce the incidence at older ages. This paradigm may change if individuals can be empowered to assume a leading role in making decisions about their own health.Citation13 Thus, the use of a self-screening method to assess cardiovascular risk may help to increase population awareness and shared responsibility for cardiovascular disease prevention.
To better address a key target population for the preventive message, the objective of the present study was to evaluate the validity of a cardiovascular risk self-screening method that includes self-measurement of blood pressure, a point-of-care assessment of lipid profile and glycated hemoglobin, and a self-administered questionnaire (sex, age, diabetes, tobacco consumption), compared with the standard screening (gold standard) conducted by a health professional.
Methods
In a randomized crossover clinical trial in the city of Girona and surrounding areas (northeastern Spain), individuals were randomly selected from the reference population. Those aged 35–74 who did not present with cardiovascular diseases at baseline were included in the study. Participants were randomly assigned to one of two cardiovascular risk screening sequences: standard screening followed by self-screening or vice versa. Both screening methods were performed the same day and included the eight variables used to estimate cardiovascular risk with the Framingham function, adapted and validated for the Spanish populationCitation14 using the standard methodologyCitation15: sex, age, systolic and diastolic blood pressure, total cholesterol, high-density lipoprotein (HDL) cholesterol, tobacco consumption, and diabetes. The only difference between the screening methods was the active role of the team of trained nurses in the standard screening and their minimal supervision of the self-screening, mainly related to blood capillary extraction and analysis.
We needed a sample size of 900 individuals to estimate a kappa index of 0.8 with 95% CI, considering that 65% of the reference population presented with low risk (<5%), 25% with intermediate risk (≥5% and <10%), and 10% with high risk (≥10%).Citation6
All participants provided written informed consent before enrollment. The present study was approved by the Clinical Research Ethic Committee of the Parc de Salut Mar (CEIC-PSMAR, #2014/5815/I) and has been registered in ClinicalTrials.gov (#NCT02373319).
Blood pressure measurement
Blood pressure was measured with an automatic blood pressure monitor and a cuff adapted to upper arm perimeter (young, adult, obese) for each participant. After a 5-min rest, two measurements were taken, at least 2 minutes apart, and the lower value was recorded for the study. The cutoff points for hypertension followed the criteria in the Seventh Report of the Joint National Committee.Citation16 The team of nurses performed these measures in the standard screening; in the self-screening, computer prompts guided the participants to independently measure and record their blood pressure.
Laboratory tests
To determine the lipid profile (total cholesterol, HDL cholesterol, and triglycerides) and the glycated hemoglobin in the standard screening procedure, blood was withdrawn in <60 seconds after 10–14 h fasting. Serum sample aliquots were stored at –80°C. Total cholesterol and HDL cholesterol concentrations were determined by enzymatic and direct methodologies, respectively (ABX-Horiba, Montpellier, France). When triglycerides were <300 mg/dL, low-density lipoprotein cholesterol was calculated using the Friedewald formula. Glycated hemoglobin was determined by colorimetry and latex agglutination procedures (ABX-Horiba). All analyses were performed in a central laboratory. When participants used the self-screening methodology, they performed a capillary blood analysis with the Cobas b101 (Roche Diagnostics, Basel, Switzerland) point-of-care device under nurse supervision. Total and HDL cholesterol (ApoB precipitation) were determined by enzymatic methods and glycated hemoglobin by latex agglutination procedure.
Other variables collected
Both screening methods collected data on sex, age, educational level, tobacco consumption, and self-reported diabetes and related treatment with self-administered standard questionnaires. Although educational level was not required to estimate the cardiovascular risk, this variable was collected for the assessment of comparability of the two study groups. Diabetes was considered whenever an individual reported a history of the disorder, was being treated with insulin or oral antidiabetic treatments, or presented with a glycated hemoglobin ≥6.5%.Citation17
A precision scale of easy calibration was used for weight measurement with participants in underwear. Height was measured with a standard measuring rod, with participants standing barefoot. Body mass index was determined as weight divided by squared height (kg/m2). Waist perimeter was also collected.
Statistical analysis
All analyses were stratified by sex. Categorical variables were presented as proportions and continuous variables as mean and SD or median and interquartile range when their distribution departed from normal.
To compare the results of the standard and the self- screening methods, the intraclass correlation coefficient (ICC) and kappa index were estimated for continuous (total and HDL cholesterol, glycated hemoglobin, systolic and diastolic blood pressure, cardiovascular risk) and categorical variables (diabetes), respectively. We also estimated the kappa index in a sensitivity analysis, considering glycemia in the estimate of diabetes prevalence for the standard screening. Additionally, the concordance of lipid measurements and glycated hemoglobin between the ABX-Horiba Pentra autoanalyzer® (standard screening) and the Cobas b101® point-of-care device (self-screening) was measured using the R2 coefficient of determination and Bland–Altman plots.Citation18 We estimated the Pearson correlation between the two screening methods and compared the distribution in three cardiovascular risk categories (low <5%, intermediate ≥5% and <10%, and high ≥10%) with chi-square tests. We described the intermediate/high-risk individuals identified with each strategy and estimated sensitivity, specificity, and the positive and negative predictive value, likelihood ratios of a positive and a negative test, diagnostic accuracy and odds ratio, Youden Index, and area under the receiver operator characteristics (ROC) curve at a cutoff point ≥5%.Citation19
All the statistical analyses were performed with the R Statistical Package (R Foundation for Statistical Computing, Vienna, Austria; V.3.3.2).
Results
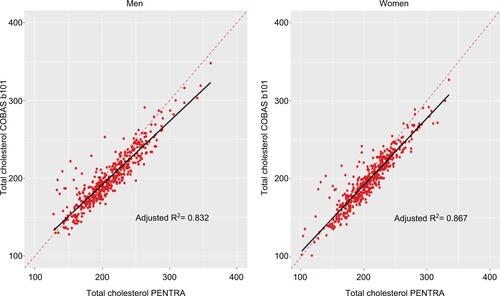
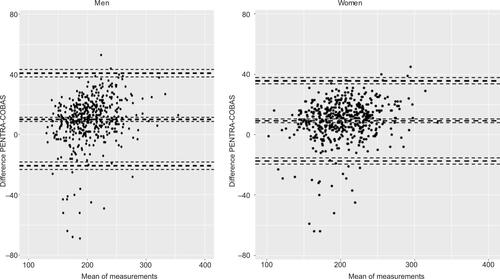
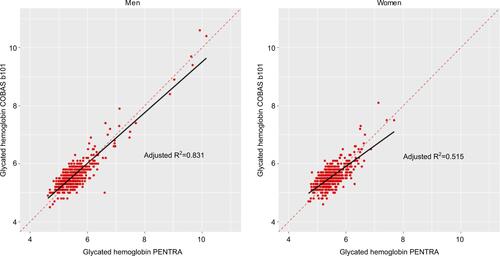
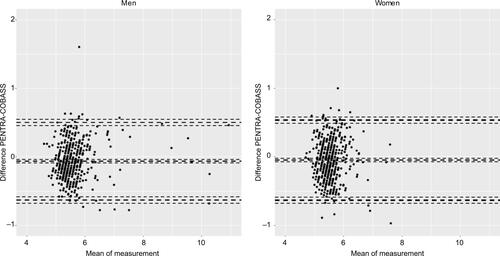
The present study included 937 individuals (52.3% women) with mean age of 50 years (SD=10) () and a response rate of 60%. No sex or age differences were found between participants and nonparticipants. summarizes the main characteristics of the participants by sex and screening sequence. The additional variables, not used to estimate the cardiovascular risk, have been described using the same stratification in . The concordance between self-screening and standard measures was high for all single variables studied (ICC≥0.86), except for glycated hemoglobin in women (ICC=0.72). The ICCs for cardiovascular risk were high in both men and women (0.92 [95% CI: 0.90–0.93] and 0.89 [0.87–0.90], respectively) ( and ). The results of the sensitivity analysis using glycemia for the standard screening yielded similar results (kappa index in men and in women: 0.94 and 0.86, respectively). – show the linear regression plots with the estimated R2 and the Bland–Altman plots for total and HDL cholesterol and glycated hemoglobin levels as measured with the Pentra autoanalyzer® and Cobas b101® point-of-care device.
Figure 1 Flow chart of the participants in the ACRISC Study.
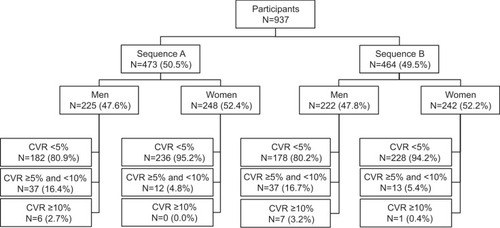
Table 1 Participant characteristics by screening sequence
Table 2 Concordance between self-screening and standard measures needed to estimate cardiovascular risk, stratified by sex
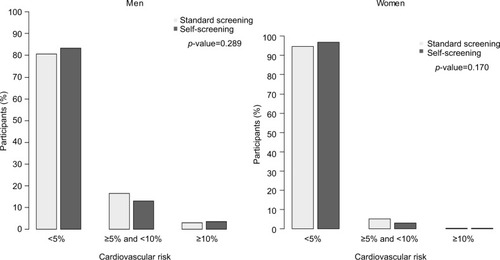
The standard and self-screening methods did not differ significantly in their classification of individuals by risk category (<5%, ≥5% and <10%, and ≥10%) with a kappa index =0.80 ().
Figure 3 Distribution of participants by cardiovascular risk category according to standard screening and self-screening results.
Self-screening of cardiovascular risk considering a cutoff point ≥5% showed high specificity and negative predictive value in both men and women. The likelihood ratio for a positive test (26.5 in men and 77.3 in women) indicated high probability of increased risk and the likelihood ratio for a negative test showed low probability of increased risk (0.27 and 0.50, respectively). The diagnostic accuracy was also high, pointing out a marked proportion of correctly classified subjects. In addition, the estimates of diagnostic odds ratio, the Youden Index, and the area under the ROC curve showed a satisfactory discriminative power of the self-screening using the 5% cutoff point ().
Table 3 Sensitivity, specificity, positive and negative predictive values, diagnostic accuracy and odds, Youden’s Index, and area under the ROC curve of self-screening compared with standard screening, stratified by sex
Discussion
The estimation of cardiovascular risk is acknowledged as the first step in cardiovascular prevention, enabling application of the most efficient preventive strategy in each individual. The innovative self-screening method proposed empowers the individual to measure and record the eight health variables (blood pressure, lipid profile, glycated hemoglobin, age, sex, tobacco consumption, diabetes) required to assess cardiovascular risk, with minimal supervision by a health professional. As results obtained were similar to the gold-standard clinical method, healthy people who do not frequent clinical settings could increase their awareness and avoid preventable cardiovascular disease by conducting their own risk assessment at their convenience.
Empowerment for the prevention of cardiovascular diseases
Population empowerment is considered a key principle of health promotion by the World Health Organization.Citation20 This concept emphasizes that all persons have strengths and providing appropriate resources enhances these strengths. This focus on lifestyle choices and personal responsibility has the potential to change how healthy people avoid preventable cardiovascular diseases as well as other chronic diseases and could indirectly promote choices of healthful activities. Recent reports have identified two approaches, improvement of individual patient skills and transfer of power and decision-making authority about interventions to patients, as effective empowerment strategies.Citation21 The present study aimed to validate an easy procedure to self-collect eight variables of general interest (age, sex, tobacco consumption, diabetes, systolic and diastolic blood pressure, and total and HDL cholesterol) to estimate cardiovascular risk. As in previous studies, lifetime risk increased exponentially after 55 years of age according to the number of cardiovascular risk factors above the recommended levels.Citation22 Additionally, the combination of such variables in a cardiovascular risk score (e.g., Framingham-REGICOR score validated for the Spanish population) provides valid information about an individual’s 10-year cardiovascular risk.Citation6 General practitioners play an important role in the primary prevention of cardiovascular disease; however, mhealth has the potential to promote patient self-management, as a complement to the doctor’s intervention, and encourage greater participation in medical decision making. Our solution could be used together with usual office consultation and remote patient monitoring to implement a health care model including personalized health care delivery with an early diagnosis and treatment if needed. Although our self-screening method is not the first to be described in the literature,Citation23,Citation24 its novelty is the self-collection of objective variables (e.g., blood pressure, lipid profile, weight) with validated devices.
Prevention of cardiovascular disease in healthy individuals
Numerous innovations in health information technology are empowering individuals to assume a more active role in monitoring and managing their health and wellness, as well as their chronic conditions and therapeutic regimens.Citation25 The effectiveness of self-management in chronic diseases has been analyzed through traditional education programs or, more recently, through mobile apps and other information and communication technologies.Citation25–Citation27 Regarding the latter, innovative approaches have been reported for overcoming obesity,Citation28 encouraging regular physical activityCitation29 and smoking cessation,Citation30 control of hypertensionCitation31 and dyslipidemia,Citation32 and treating diabetes mellitus.Citation33 However, a major limitation of these innovative technologies is the absence of published evaluations. The present crossover clinical trial validates a new self-screening system that aims to empower individuals to assess their own cardiovascular risk. This device also could be used to estimate the risk of other chronic diseases such as cancerCitation34–Citation36 or cognitive declineCitation37 in which the assessed comorbidities (hypertension, diabetes, obesity, dyslipidemia) play a crucial role. The added value of this validated procedure is the stratification of population risk, as users become aware about their own health and the most efficient strategies for preventing chronic diseases. Self-screening for cardiovascular risk yielded remarkable specificity and negative predictive values compared with the gold standard. In addition, there was high concordance between methods in the estimated cardiovascular risk category.
Limitations
Risk estimation is considered the best tool to prioritize primary prevention strategies.Citation5,Citation8 Our crossover clinical trial aimed to validate a new self-screening method in a population-based sample that covered a very wide range of cardiovascular risk. Participants were randomized to one of two sequences of risk assessment (i.e., the current gold standard followed by self-screening or vice versa) and all four risk measurements (systolic and diastolic blood pressure, total and HDL cholesterol) were collected with both methodologies. Selection bias may affect the present study, but is likely to be modest because it was population-based and participants were not selected on the basis of cardiovascular risk. In addition, the low cardiovascular risk traditionally observed in Mediterranean womenCitation38 and also reflected in our analysis may explain the low sensitivity of the self-screening (50%) to rule out intermediate or high cardiovascular risk. Despite the availability of a cardiovascular risk score with no laboratory and blood pressure determinations that has been validated for the Spanish population,Citation39 we preferred to validate the self-screening procedure using the more accurate Framingham-REGICOR cardiovascular risk chart.Citation6,Citation14 The aim of the study was to assess the validity of a cardiovascular risk self-screening method by comparing the results with a gold standard (current clinical practice). However, we did not test whether the self-screening had an effect on health outcomes. Further randomized clinical trials should be performed to answer this question. Finally, although our aim is to empower individuals to monitor their cardiovascular health, preferably at home, the blood capillary extraction and analysis must be supervised by a health care professional. Thus, the present version of the system must be implemented at a centralized location that is readily accessible to the target population (e.g., pharmacies, primary health care settings).
Future directions
This self-screening system encourages users to take responsibility for their own health and well-being. Although health care professionals are ideally positioned to provide advice and education on risk factors and lifestyle modifications to people living with chronic conditions, a large part of the healthy population seldom visits a health care provider. Thus, a validated self-management system based on objective measurements empowers healthy people to avoid preventable cardiovascular and other chronic diseases. Our innovative method makes it possible to expand screening coverage to healthy populations, encouraging personal empowerment and increasing self-awareness of individual risk. A feedback strategy could be combined with tailored lifestyle recommendations to improve adherence to healthier habits and encourage effective disease prevention strategies.
Conclusion
The self-screening method for assessing cardiovascular risk provided similar results to the standard method. In addition, this innovative system showed high clinical performance to rule out intermediate or high cardiovascular risk (i.e., ≥5%).
Author contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Acknowledgments
The authors wish to thank Marta Cabañero, Leny Franco, Neus Guday, Montse Peris, Martina Sidera, and Susanna Tello for their contribution to the data collection and management of this project and appreciate the revision of the English text by Elaine Lilly, Ph D. This study was partially financed with unconditional support from Roche Diagnostics and by Spain’s Ministry of Economy and Competitiveness through the Carlos III Health Institute FEDER (CM12/03287, CPII17/00012, and FIS14/00449).
Supplementary materials
Figure S3 Linear regression analysis for HDL cholesterol (mg/dL) by sex.
Abbreviation: HDL, high-density lipoprotein.
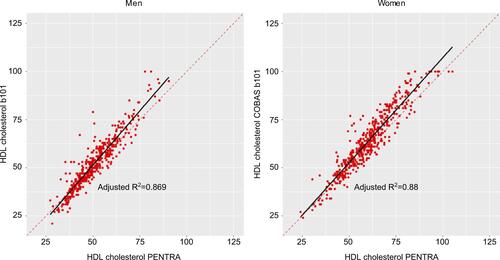
Figure S4 Bland–Altman plot for HDL cholesterol (mg/dL).
Abbreviation: HDL, high-density lipoprotein.
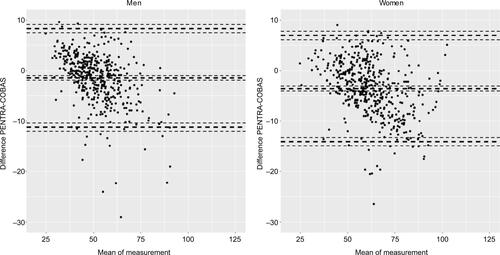
Table S1 Participant characteristics (additional variables) by screening sequence
Disclosure
The authors report no conflicts of interest in this work.
References
- World Health Statistics Monograph on the InternetGenevaWorld Health Organization Available from: https://apps.who.int/infobase/Accessed January 27 2017
- CapewellSFordESCroftJBCritchleyJAGreenlundKJLabartheDRCardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of AmericaBull World Health Organ201088212013020428369
- Flores-MateoGGrauMO’FlahertyMAnalyzing the coronary heart disease mortality decline in a Mediterranean population: Spain 1988–2005Rev Esp Cardiol20116411988996 Spanish21962958
- O’FlahertyMBuchanICapewellSContributions of treatment and lifestyle to declining CVD mortality: why have CVD mortality rates declined so much since the 1960s?Heart201399315916222962283
- GrauMMarrugatJRisk functions and the primary prevention of cardiovascular diseaseRev Esp Cardiol200861440441618405521
- MarrugatJVilaJBaena-DíezJMRelative validity of the 10-year cardiovascular risk estimate in a population cohort of the REGICOR studyRev Esp Cardiol2011645385394 Spanish21482004
- McKeeGKerinsMHamiltonGBarriers to ESC guideline implementation: results of a survey from the European Council on Cardiovascular Nursing and Allied Professions (CCNAP)Eur J Car-diovasc Nurs2017168678686
- PiepoliMFHoesAWAgewallS2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical PracticeEur Heart J201637292315238127222591
- GjelsvikBConflicts and dilemmas in prevention of cardiovascular disease. The new, Norwegian guidelines–a new approach to risk managementEur J Gen Pract2012181566222283824
- VancheriFStrenderLEBacklundLGGeneral practitioners’ coronary risk estimates, decisions to start lipid-lowering treatment, gender and length of clinical experience: their interactions in primary preventionPrim Health Care Res Dev201314439440223351666
- Catalán-RamosAVerdúJMGrauMPopulation prevalence and control of cardiovascular risk factors: what electronic medical records tell usAten Primaria2014461152424325864
- WilmotKAO’FlahertyMCapewellSFordESVaccarinoVCoronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially womenCirculation201513211997100226302759
- FeiginVLNorrvingBMensahGAPrimary prevention of cardiovascular disease through population-wide motivational strategies: insights from using smartphones in stroke preventionBMJ Glob Health201722e000306
- MarrugatJSubiranaIComínEVERIFICA InvestigatorsValidity of an adaptation of the Framingham cardiovascular risk function: the VERIFICA StudyJ Epidemiol Community Health2007611404717183014
- Manual of The MONICA Project [Manual on the Internet]GenevaWorld Health Organisation2000 Available from: http://www.ktl.fi/publications/monica/manual/index.htmAccessed January 8, 2017
- ChobanianAVBakrisGLBlackHRJoint National Committee on Prevention, Detection Evaluation, and Treatment of High Blood PressureNational Heart, Lung, and Blood InstituteNational High Blood Pressure Education Program Coordinating CommitteeSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034261206125214656957
- SacksDBArnoldMBakrisGLNational Academy of Clinical BiochemistryGuidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitusDiabetes Care2011346e61e9921617108
- BlandJMAltmanDGStatistical methods for assessing agreement between two methods of clinical measurementLancet198613073102868172
- ŠimundićAMMeasures of diagnostic accuracy: basic definitionsEJIFCC200919420321127683318
- WoodallJRaineGSouthJWarwick-BoothLEmpowerment and Health & Well-Being: Evidence ReviewLeedsCentre for Health Promotion Research, Leeds Metropolitan University2010
- WallersteinNWhat is the evidence on effectiveness of empowerment to improve health?2006CopenhagenWHO Regional Office for Europe (Health Evidence Network report Available from: http://www.euro.who.int/Document/E88086.pdfAccessed October 1, 2017
- BerryJDDyerACaiXLifetime risks of cardiovascular diseaseN Engl J Med2012366432132922276822
- NeufingerlNCobainMRNewsonRSWeb-based self-assessment health tools: who are the users and what is the impact of missing input information?J Med Internet Res2014169e21525261155
- PatelRSLagordCWaterallJMothMKnaptonMDeanfieldJEOnline self-assessment of cardiovascular risk using the Joint British Societies (JBS3)-derived heart age tool: a descriptive studyBMJ Open201669e011511
- BurkeLEMaJAzarKMCurrent science on consumer use of mobile health for cardiovascular disease prevention: a scientific statement from the American Heart AssociationCirculation2015132121157121326271892
- WarsiAWangPSLaValleyMPAvornJSolomonDHSelf-management education programs in chronic disease: a systematic review and methodological critique of the literatureArch Intern Med2004164151641164915302634
- KimBYLeeJSmart devices for older adults managing chronic disease: a scoping reviewJMIR Mhealth Uhealth201755e6928536089
- SiopisGCheyTAllman-FarinelliMA systematic review and meta-analysis of interventions for weight management using text messagingJ Hum Nutr Diet201528Suppl 2115
- Bort-RoigJGilsonNDPuig-RiberaAContrerasRSTrostSGMeasuring and influencing physical activity with smartphone technology: a systematic reviewSports Med201444567168624497157
- WhittakerRMcRobbieHBullenCBorlandRRodgersAGuYMobile phone-based interventions for smoking cessationCochrane Database Syst Rev201211CD00661123152238
- UhligKPatelKIpSKitsiosGDBalkEMSelf-measured blood pressure monitoring in the management of hypertension: a systematic review and meta-analysisAnn Intern Med2013159318519423922064
- DekkersJCvan WierMFAriënsGAComparative effectiveness of lifestyle interventions on cardiovascular risk factors among a Dutch overweight working population: a randomized controlled trialBMC Public Health20111114921261935
- PalKEastwoodSVMichieSComputer-based diabetes self-management interventions for adults with type 2 diabetes mellitusCochrane Database Syst Rev20133CD00877623543567
- KoeneRJPrizmentAEBlaesAKonetySHShared risk factors in cardiovascular disease and cancerCirculation2016133111104111426976915
- Baena-DíezJMPeñafielJSubiranaIRisk of cause-specific death in individuals with diabetes: a competing risks analysisDiabetes Care201639111987199527493134
- BarrosoMGodayARamosRFRESCO InvestigatorsInteraction between cardiovascular risk factors and body mass index and 10-year incidence of cardiovascular disease, cancer death, and overall mortalityPrev Med2018107818929155226
- SrinivasaRNRossettiHCGuptaMKCardiovascular risk factors associated with smaller brain volumes in regions identified as early predictors of cognitive declineRadiology2016278119820426218598
- GrauMElosuaRCabrera de LeónACardiovascular risk factors in Spain in the first decade of the 21st century, a pooled analysis with individual data from 11 population-based studies: the DARIOS studyRev Esp Cardiol201164429530421397375
- MarrugatJSubiranaIRamosRFRESCO InvestigatorsDerivation and validation of a set of 10-year cardiovascular risk predictive functions in Spain: the FRESCO StudyPrev Med201461667424412897