Abstract
Objective
Prostate cancer is the most common noncutaneous cancer among Danish men. During the last decade, use of prostate specific antigen (PSA) testing has increased, and in clinically localized prostate cancer, curative intended treatment has gained a footing. Our aim was to examine possible changes in the short- and long-term survival of patients with prostate cancer during 1998–2009.
Study design and setting
From two Danish regions (population, 1.8 million) we included all patients (N = 10,547) with an incident diagnosis of prostate cancer retrieved from the Danish National Registry of Patients. We determined survival after 1, 3, and 5 years, stratified by age, and estimated mortality rate ratios (MRRs) using Cox proportional hazard regression to assess changes over time, controlling for age.
Results
During the study period, the annual number of incident prostate cancer patients more than doubled, and the median age at diagnosis decreased from 74 to 70 years. The survival improved over the study period, particularly in the last half of the period (2004–2009). Thus, 1-year survival increased from 80% (1998–2000) to 90% (2007–2009), corresponding to an age-adjusted MRR of 0.54 (95% confidence interval CI: 0.46–0.63). The expected increase in 3- and 5-year survival was even more pronounced: 47%–73% and 34%–60%, respectively. This corresponded to a 3-year age-adjusted MRR of 0.46 (95% CI: 0.42–0.51) and a 5-year MRR of 0.50 (95% CI: 0.46–0.54). The 1-, 3-, and 5-year overall survival increased in all age groups (<70 years, 70–79 years, ≥80 years).
Conclusion
Survival after prostate cancer has improved in Denmark within the last decade. Although diagnosis and treatment improvements could explain this, length and lead time bias are likely to have influenced our results.
Keywords:
Introduction
Clinically significant prostate cancer is a serious condition with a high mortality, which in 2009 caused 1216 deaths in Danish men, corresponding to a mortality rate of 20.9 per 100,000 men per year when standardized to the age distribution of the Danish population in the year 2000 (DK-2000).Citation1 With 3900 new cases in 2009, prostate cancer has become the far most common cancer among Danish men, with an age-standardized (DK-2000) incidence rate of 138 per 100,000 men per year.Citation2 During the last decades, the incidence of prostate cancer has increased significantly, probably due to diagnostic changes, with more widespread use of prostate specific antigen (PSA) testing, either on the basis of lower urinary tract symptoms, for example, or as part of a general health checkup.Citation3–Citation6 During the period 1998–2005, treatment primarily for patients with clinical localized prostate cancer in Denmark has changed. Especially since 2003, these patients more frequently have been offered curative intended surgery or radiation therapy, instead of being observed until disease progression and palliative endocrine treatment was assessed as necessary, which was standard before 2003.Citation7 In addition to the rising number of curative intended therapies in clinically localized disease, chemotherapy has since 2005 been offered systematically to symptomatic castration-resistant prostate cancer patients. On top of the introduction of the aggressive diagnostic and treatment strategies, the last decade has seen major principal changes on a national level in the organization of handling prostate cancer. Only 10 years ago, prostate cancer patients in Denmark could be treated in surgical departments without specialized urologists. Since then, several smaller hospitals have been merged into larger hospitals, and urology departments have been included in highly specialized uro-oncological centers. Despite the introduction of curative intended therapy and a life-extending therapy in incurable patients, the age-standardized annual death rate per 100,000 individuals in Denmark has been completely unchanged the last decade.Citation1
The impact of changes in prostate cancer diagnosis, setting, and treatments has previously been assessed based on Danish registry data from 1985 to 2004.Citation8 We extended that study and examined changes in mortality and survival in prostate cancer patients within the last decade (1998 to 2009) by using data from the Danish National Registry of Patients (DNRP).
Material and methods
We conducted this study in the central and the northern Denmark regions, with a combined population of 1.8 million persons. The National Health Service provides tax-supported health care for all inhabitants of Denmark, guaranteeing free access to hospitals. Virtually no prostate cancer patients were treated in private hospitals during the study period.
Identification of prostate cancer patients
Through the DNRP, we identified all patients who had a first-time hospitalization with prostate cancer in the period January 1, 1998 through December 31, 2009. The DNRP contains information about all admissions from nonpsychiatric hospitals in Denmark since 1977.Citation9 Outpatient and emergency room visits at hospitals have been included since 1995. This registry includes information on civil registration number, dates of admission and discharge, surgical procedure(s) performed, and up to 20 diagnoses from each hospital contact. Diagnoses have been classified according to the International Classification of Diseases (ICD) 8th edition until the end of 1993 and the 10th edition (ICD-10) thereafter. Surgical procedures have been classified according to a Danish version of the Nordic Classification of Surgical Procedures (NCSP).
The ICD-10 codes used to identify prostate cancer were C 61.9.
Survival
Since 1968, the Central Office of Civil Registration has assigned a unique 10-digit personal identification number to all Danish citizens.Citation10 This number, unique to each Danish resident, is used in all Danish registries, allowing unambiguous individual-level data linkage. From the Civil Registration System, we obtained information on vital status (dead or alive), date of death, and residence for all cancer patients.
Statistical analysis
We followed each patient from date of cancer diagnosis until emigration, death, or June 25, 2010, whichever came first. To visualize crude survival we constructed Kaplan–Meier curves stratified according to the period of diagnosis (1998–2000, 2001–2003, 2004–2006, and 2007–2009). We estimated 1-, 3-, and 5-year survival. In the latter periods we estimated 3- and 5-year survival using a hybrid analysis in which survival was estimated using the survival experience of patients in the previous periods.Citation11 To compare mortality over time we used Cox proportional hazards regression analysis with 1998–2000 as the reference period to estimate 1-, 3-, and 5-year mortality rate ratios (MRRs) and corresponding 95% confidence intervals (CIs) adjusting for age group (<70 years, 70–79 years, ≥80 years).
Analyses were performed using SAS version 9.2 (SAS Institute Inc, Cary, NC).
Results
A total of 10,547 men was diagnosed with prostate cancer in the period 1998–2009. The number of patients diagnosed increased every year (). In addition, the median age at diagnosis decreased from 74 years in the 1998–2000 period to 70 years in the 2007–2009 period (). The age distribution is shown in . In general, survival improved over the study period, although the 2004–2006 and the 2007–2009 periods showed almost similar results (). Thus, the 1-year cumulative survival improved from 80% (1998–2000) to 90% (2007–2009). This corresponds to an adjusted MRR of 0.54 (95% CI 0.46–0.63) in 2007–2009, using 1998–2000 as reference (). The expected increase in 3- and 5-year survival was even more pronounced: 47%–73% and 34%–60%, respectively.
Figure 1 The age distribution of men diagnosed with prostate cancer in the period 1998–2009 in two of the five Danish regions.
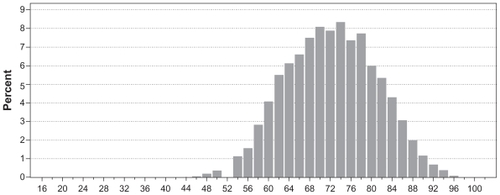
Figure 2 Overall survival in Danish prostate cancer patients diagnosed in the period 1998–2009 in two of the five Danish regions.
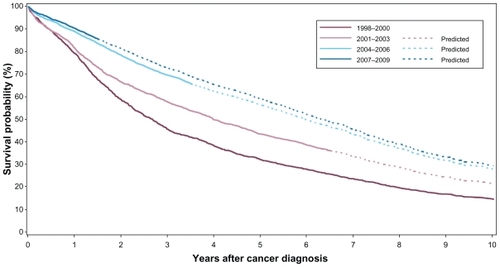
Table 1 The 1-, 3-, and 5-year overall survival and MRR adjusted for age in the four time periods
The annual number of diagnosed prostate cancer patients more than doubled over the study period, while the median age at diagnosis decreased. The annual number of patients more than tripled for patients < 70 years. Although most pronounced in younger age groups, an increase in annual number of incident prostate cancer patients occurred in all age groups (). Among patients 15–69 years of age, the 1-year survival increased over the study period from 88% to 97%, while the 3- and 5-year survival was expected to increase from 60% to 86% and from 48% to 78%, respectively (). Patients in the age groups 70–79 and 80+ years had slightly lower survival than patients aged 15–69 years, but survival increased in all three age groups over the study period ().
Table 2 The 1-, 3-, and 5-year survival in the four time periods according to three different age groups
Discussion
In this regional population-based cohort study we found that the survival after prostate cancer increased between 1998 and 2009. This increased survival was present across age groups. In addition, the annual number of diagnosed prostate cancer patients more than doubled over the study period, while the median age at diagnosis decreased. Although the national clinical guidelines for prostate cancer persistently argue against a formalized PSA screening program, PSA measurements are increasingly performed.Citation6
Our study is based on a well defined cohort representing approximately one-third of the total Danish male population, with nearly complete registration of prostate cancer patients. We obtained complete vital status follow-up by using the Civil Registry System. Cancer data in Denmark are usually derived from the nationwide Danish Cancer Registry because of its high completeness and accuracy.Citation12,Citation13 However, until recently there has been a substantial delay between the time of data submission and availability for outcome monitoring and scientific purposes. Therefore, data from the Danish Cancer Registry have not been optimal for updated studies of cancer survival. Fortunately, data from the DNRP are updated and thus facilitates studies that evaluate recent changes. However, data from the DNRP might be affected by misclassification of prostate cancer diagnoses. Nevertheless, a Danish ovarian cancer study used the same data source as in the current study and validated the diagnosis codes against those recorded in the Danish Cancer Registry.Citation14 The ovarian cancer data proved a completeness of 96% in the hospital discharge registry, with a high positive predictive value (87%), and we have no reason to expect that the coding of prostate cancer in the DNRP is inferior to the coding of ovarian cancer.
The finding of an increasing annual number of incident prostate cancers and the decreasing median age at time of diagnosis is an expected scenario at a time with a generally more aggressive diagnostic strategy. PSA testing has never been used more frequently in Denmark than it is today.Citation6 We found that survival increased particularly from 2004 to 2009, which covers the time period of the curative intended treatment approach in Denmark. Our study thus extends findings from a previous study in the exact same geographical area which demonstrated an improved prostate cancer survival between the years 1985 and 2004.Citation8 In that study, improvement in survival was most markedly observed during the last part of the period (2000–2004) and especially in patients younger than 70 years of age. Furthermore, the results of two nationwide studies presenting Danish prostate cancer relative survival estimates corresponding with our study, thereby supporting the idea that the general increase in life expectancy in the Danish population during the study period was not the reason for the observed survival improvement in prostate cancer patients.Citation15,Citation16 Traditionally, Denmark has been very conservative with respect to the diagnosis and treatment of prostate cancer, and starting treatment at a very late stage of the disease was recommended until less than 15 years ago. This fact is probably a key explanation why Danish prostate cancer patients previously have had a significantly lower survival rate than prostate cancer patients from countries practicing a more aggressive strategy toward this disease.Citation17 In the current study, survival increased in all age groups. Besides the tremendous curative intended treatment effort in younger and clinically localized patients during the last decade,Citation7 the phenomenon that survival benefit seems independent of patient age at diagnosis could in part reflect the introduction of chemotherapy in 2005 intended for disseminated disease. Before that there existed no life-extending treatment in castration-resistant prostate cancer.
The current results should be interpreted cautiously. The widespread use of PSA tests will inevitable result in patients being diagnosed at earlier disease stage, which automatically leads to patients living longer with a cancer diagnosis than previously observed (lead-time bias). Additionally, more patients with slowly developing tumors having a more favorable prognosis will be diagnosed (length-ime bias), some of whom might never become symptomatic during the patient’s life (over-diagnosis). The fact that a significant portion of prostate cancer patients suffer from harmless clinically insignificant disease has been shown previously,Citation18 and the risk of over-diagnosis as well as over-treatment is well documented.Citation18,Citation19 Overall, we find it likely that the massive increase in observed survival in prostate cancer patients to a greater degree reflects a change in the patient population than a real improvement in survival. This is also supported by the absence of change in the age standardized annual death rate in Denmark during the last decade.Citation1 Similarly, the predicted survival should be interpreted with caution. Since the predicted values are based on the survival observed in previous periods, those will as a consequence from the above probably be conservative survival estimates (under-rating). A limitation of this study is the lacking information on disease stage, which would have been very informative. Adjusting for stage would probably have allowed some degree of separation of screening effects from treatment effects. However, quality data of the TNM (tumor, lymph node, metastasis) coding were not available for the given period of observation.
A previous Danish study based on nationwide registry data from the period 1943–1996 found that the incidence of prostate cancer increased about 1.6% per year.Citation20 It was concluded that the epidemiological pattern of prostate cancer incidence seemed to be dominated by changes in diagnosis and registration rather than changes in causal factors, which supports our speculation concerning the current results.
The EUROCARE project was set up in 1989 to measure and explain international differences in cancer survival in Europe.Citation21 The last EUROCARE report stated that the 5-year survival rates for prostate cancer varied significantly more than for any other cancer, going from <40% to >80%. EUROCARE thus concluded that the wide range in survival rates was largely attributable to the differences in the intensity of diagnostic and screening activity, especially PSA testing.Citation21 This point of view is supported by our study and data from Austria, where intensive PSA screening has been ongoing since 1992.Citation22 However, the paradigm handling prostate cancer has changed during the last 10 years, and patients with clinical localized prostate cancer are now offered curative treatment. All together, the most likely explanation for the steadily increasing incidence and survival in Danish prostate cancer patients is identical to observations in other Western countries:Citation23 the increased use of PSA resulting in identification of earlier and eventually clinically insignificant disease, rather than a real improvement in survival.
Conclusion
In the last decade (1998–2009) the number of incident prostate cancer patients in central and northern Denmark increased. At the same time, long-term survival of prostate cancer patients has continuously improved significantly. Both the rise in incidence and long-term outcome improvement was most pronounced in men younger than 70 years of age. Although the treatment paradigm has changed significantly in the last decade, it seems most likely that the results to a greater degree reflect lead and length time bias rather than a real improvement in survival.
Support
The study obtained support from the Western Danish Research Forum for Health Sciences and the Danish Cancer Society.
Disclosure
The authors report no conflicts of interest in this work.
References
- The National Board of HealthThe Danish registry of death causes 2009 [in Danish] Available from: http://www.sst.dk/publ/Publ2010/DOKU/Registre/Doedsaarsagsregisteret2009.pdfAccessed May 18, 2011
- The National Board of HealthCancer incidence in Denmark 2009 [in Danish] Available from: http://www.sst.dk/publ/Publ2010/DOKU/Registre/Cancerregisteret2009.pdfAccessed May 18, 2011
- BrettTDAn analysis of digital examination and serum-prostate-specific antigen in the early detection of prostate cancer in general practiceFam Pract19981552953310078792
- FeneleyMRBrewsterSOpportunities and outcomes in early prostate cancer: a commentary on policy, patient perspectives, trials and strategiesBJU Int20039117717812580998
- JønlerMEddyBPoulsenJProstate-specific antigen testing in general practice: a survey among 325 general practitioners in DenmarkScand J Urol Nephrol20053921421816118092
- OstersenTMBroFPedersenKVVedstedPUse of prostate-specific antigen testingUgeskr Læger20101729696700
- BorreMIversenPBendixenAIversenMGKehletHOrganisation and early outcome after radical prostatectomy in Denmark 2004–2007Ugeskr Laeger2008170342545254918761836
- LundLJacobsenJBorreMImproved survival of patients with prostate cancer in Northern Denmark, 1985–2004Scand J Urol and Nephr200741308313
- AndersenTFMadsenMJorgensenJMellemkjoerLOlsenJHThe Danish National Hospital Register. A Valuable Source of Data for Modern Health SciencesDan Med Bull19994626326810421985
- PedersenCBGotzscheHMollerJOMortensenPBThe Danish Civil Registration System. A cohort of eight million personsDan Med Bull20065344144917150149
- BrennerHRachetBHybrid analysis for up-to-date long-term survival rates in cancer registries with delayed recording of incident casesEur J Cancer20044024912501
- StormHHCompleteness of cancer registration in Denmark 1943–1966 and efficacy of record linkage proceduresInt J Epidemiol19881744493384548
- StormHHMichelsenEVClemmensenIHPihlJThe Danish Cancer Registry history, content, quality and useDan Med Bull1997445355399408738
- TetscheMSNørgaardMSkriverMVAndersenESLashTLSørensenHTAccuracy of ovarian cancer ICD-10 diagnosis in a Danish population-based hospital discharge registryEur J Gyn Oncol200526266270
- BrayFKlintAGislumMTrends in survival of patients diagnosed with male genital cancers in the Nordic countries 1964–2003 followed up until the end of 2006Acta Oncol6201049564465420151937
- StormHHGislumMKejsAMEngholmGSurvival of Danish cancer patients 1995–2006Ugeskr Laeger2010172332213221720727286
- TretliSHaldorsenAHakulinenTProstate cancer – look to Denmark?J Natl Can Inst199688128
- HolmbergLBill-AxelssonAHelgesenFA randomised trial comparing radical prostatectomy with watchful waiting in early prostate cancerN Engl J Med200234778178912226148
- SchröderFHHugossonJRoobolMJfor the ERSPC InvestigatorsScreening and prostate-cancer mortality in a randomized European studyN Engl J Med2009360131320132819297566
- MøllerHTrends in incidence of testicular cancer and prostate cancer in DenmarkHuman Reprod20011610071011
- ColemanMPGattaGVerdecchiaAEUROCARE Working GroupEUROCARE-3 summary: cancer survival in Europe at the end of the 20th centuryAnn Oncol200314Suppl 5v128v14914684503
- MicheliACoeberghJWMugnoEthe EUROCARE Working groupEuropean health systems and cancer careAnn Oncol2003144160
- GjertsonCKAlbertsenPCUse and assessment of PSA in prostate cancerMed Clin North Am201195119120021095422