Abstract
Human papillomavirus (HPV) is the main cause of cervical cancer, and many countries now offer vaccination against HPV to girls by way of government-funded national immunization programs. Monitoring HPV prevalence in adolescents could offer a near-term biological measure of vaccine impact, and urine sampling may be an attractive large-scale method that could be used for this purpose. Our objective was to provide an overview of the literature on HPV DNA detection in urine samples, with an emphasis on adolescents. We searched the PubMed database using the terms “HPV” and “urine” and identified 21 female and 14 male study populations in which HPV prevalence in urine samples was reported, four of which included only asymptomatic female adolescents. We provide herein an overview of the recruitment setting, age, urine sampling procedure, lesion type, HPV assay, and HPV prevalence in urine samples and other urogenital samples for the studies included in this review. In female study populations, concordance for any HPV type and type-specific concordance in paired urine and cervical samples are provided in addition to sensitivity and specificity. We concluded that few studies on HPV prevalence in urine samples have been performed in asymptomatic female adolescent populations but that urine samples may be a useful alternative to cervical samples to monitor changes in HPV prevalence in females in the post-HPV vaccination era. However, care should be taken when extrapolating HPV findings from urine samples to the cervix. In males, urine samples do not seem to be optimal for monitoring HPV prevalence due to a low human genomic DNA content and HPV DNA detection rate compared to other urogenital sites. In each situation the costs and benefits of HPV DNA detection in urine compared to alternative monitoring options should be carefully considered.
Human papillomavirus (HPV) is the main cause of cervical cancer.Citation1,Citation2 More than 35 HPV types have been identified in the genital tract, and HPV16 and 18 are responsible for approximately 70% of cervical cancer.Citation3,Citation4 Two HPV vaccines, a quadrivalent vaccine that protects against HPV6, 11, 16, and 18 and a bivalent vaccine that protects against HPV16 and 18, have been developed and approved by the United States Food and Drug Administration (FDA) for females 9–25 years and 9–26 years of age, respectively.Citation5,Citation6 The quadrivalent vaccine has also been approved by the FDA for males 9–26 years of age for the prevention of genital warts (caused by HPV6 and 11) and in both males and females 9–26 years of age for the prevention of precancerous anal lesions and anal cancer associated with the vaccine HPV types.Citation7 However, in many countries the debate continues as to whether or not to offer the vaccine to boys in the framework of government-funded national immunization programs as is done for girls.Citation8 Although the safety, immunogenicity, and efficacy of the two vaccines have been monitored closely in clinical trials,Citation9–Citation14 it is also necessary to monitor their impact in the general population.Citation15 In addition to vaccine coverage and the incidence of cervical cancer and other HPV-related lesions, it is also recommended to monitor changes in HPV prevalence in the general population, particularly in females aged 15–20 years soon after initiation of sexual activity as this could offer a near-term biological measure of vaccine impact.Citation16
HPV DNA detection in urine samples could be a viable alternative to detection in cervical samples for monitoring the impact of vaccination on overall and type-specific HPV prevalence.Citation17,Citation18 HPV DNA detection in urine samples is particularly attractive as a large-scale method among female adolescents as pelvic examination might not be feasible or ethically acceptable in this age group. HPV detection has also been performed in urine samples from males as well as at many urogenital sites.Citation19 The urogenital sites most commonly sampled have been penile skin, specifically coronal sulcus and glans penis, and the urethra.Citation20 In a recent review by Vorsters et al,Citation17 41 published studies on HPV DNA in urine samples were evaluated with respect to factors that have an impact on HPV detection, such as urine sampling procedure, sample preparation, DNA extraction, and DNA amplification. They concluded that HPV DNA detection in urine is feasible and may become a useful tool but necessitates further improvement and standardization. In the same vein, Sehgal et alCitation21 reviewed the pros and cons of using HPV DNA detection in urine samples for cervical cancer screening.Citation21 One of their conclusions was that further research is needed to standardize and optimize the corresponding technology before recommending it as a mass screening tool for cervical cancer.
The aim of this literature review was to evaluate whether HPV DNA detection in urine samples would be a feasible approach for monitoring HPV prevalence in male and female adolescents in the general population. To this end, a list of relevant studies and their main characteristics, including HPV positivity in paired urine and cervical samples and their concordance is provided. Since only a few studies monitored HPV prevalence in urine samples from adolescents, we included relevant studies from older age groups as well. For details on factors that affect HPV DNA detection, such as urine sampling procedure, storage, centrifugation, DNA extraction, and assays for detection of human genomic and HPV DNA and an overview of the use of urine samples in a screening setting, we refer the reader to the reviews by Vorsters et alCitation17 and Sehgal et al.Citation21
Materials and methods
We used the terms “HPV” and “urine” to search the PubMed database in August 2012 for relevant literature. The identified studies were then individually evaluated to ascertain whether results on HPV prevalence in adolescents were reported. Studies in HIV-positive populations and renal allograft recipients were excluded as these patient groups have a reported increased risk of HPV infection. Studies that included paired urine and cervical samples were sought as they would allow for comparison of the presence of HPV in both samples. We therefore excluded female studies in which HPV DNA was detected in urine samples only, with the exception of the four studies including adolescents as they shed some light on the expected urinary HPV prevalence rates in this group. As few studies in asymptomatic male populations were found, we included the male populations of four studies despite the fact that they may be at greater risk of HPV infection: two studies on male partners of HPV-positive women, one on male partners of women with cervical cancer, and one on males with urethritis.
Whenever possible we extracted information on country, recruitment setting, age (range and mean), urine sampling procedure, total sample size, percentage of samples containing human genomic DNA, HPV assay used, proportion and type of cervical lesions, and availability of cervical sample. As a main result we report HPV prevalence in urine samples and cervical samples in female study populations. We also report sensitivity, ie, the probability of an HPV-positive urine sample given an HPV-positive cervical sample, and specificity, ie, the probability an HPV-negative urine sample given an HPV-negative cervical sample. Concordance for any HPV type and for HPV16 (and/or HPV18) was measured as the percentage of paired urine and cervical samples that yielded the same HPV result, ie, either both positive or both negative. In contrast, type-specific concordance (combined concordance for a group of HPV types) was measured only in the set of paired urine and cervical samples that were both positive for any HPV type. Within this smaller set of samples, type-specific concordance was calculated as the percent of paired urine and cervical samples that were positive for the same HPV type.
Results
HPV prevalence in females
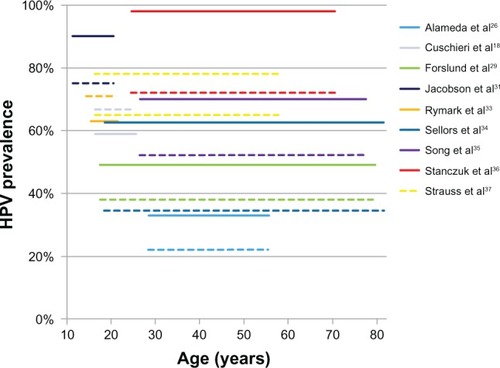
Results from 21 female study populations from 17 publications that reported HPV prevalence in urine samples are summarized in . Four of these studies reported age-specific HPV prevalence in asymptomatic adolescents. Prusty et alCitation22 and Manhart et alCitation23 included females 18–25 years of age, while only two studies, one from Scotland by O’Leary et alCitation24 and one from India by Hussain et al,Citation25 included females less than 18 years of age ( and ). The HPV prevalence (any type) varied from 1.1% in the age group 11–14 years in the O’Leary et alCitation24 study to 29.6% in the age group 20–21 years in the Manhart et alCitation23 study. O’Leary et alCitation24 reported the lowest percentage of samples (83.6%) containing amplifable human genomic DNA; Prusty et alCitation22 reported the highest percentage (100%).
Figure 1 Human papillomavirus prevalence by age in urine samples from asymptomatic populations.
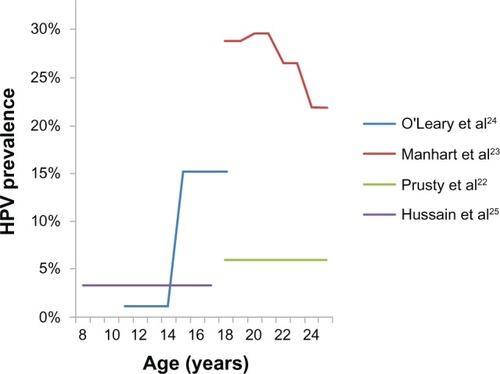
Table 1 Studies with human papillomavirus DNA detected in urine samples from asymptomatic adolescents (A) and in paired urine and cervical samples from symptomatic females all ages (B)
We identified 14 studies that measured HPV positivity in paired urine and cervical samples from symptomatic females;Citation18,Citation22,Citation26–Citation37 of these studies, nine reported the age range and nine the mean age of the study population. These studies included women with symptoms that led to various gynecological complaints and women diagnosed with invasive cervical cancer. Urine and cervical samples were collected at gynecological, colposcopy, genitourinary, sexually transmitted disease, and adolescent clinics. In general, HPV prevalence increased with the severity of cytological or pathological findings, and this was observed both in urine samples and cervical samples. All studies that reported age-specific HPV prevalence showed lower prevalence in urine samples than paired cervical samples, with the majority of the studies reporting a 10%–20% lower HPV prevalence, save the studies by Rymark et alCitation33 and Cuschieri et alCitation18 (). With the exception of studies by Rymark et alCitation33 and Jacobson et al,Citation31 which covered narrow age ranges (16–21 years and 11–20 years, respectively), the studies in this review generally reported HPV prevalence in a broad age range. Populations presenting cytological or histological pathology generally had a higher HPV prevalence compared to those with normal cytology ( and ).
HPV concordance in paired urine and cervical samples
The studies showed a 75%–100% concordance for any HPV type in paired urine and cervical samples (or 41%–93% by kappa agreement). Type-specific concordance was reported in five studies, showing 100%, 90.5%, 71.0%, 70.8%, and 40.0% concordance. The latter estimates were calculated by including HPV-negative samples from either (not both) site, thereby reducing the type-specific concordance. Eight of the eleven studies published after 2000 also reported either type-specific concordance for HPV16 or HPV18, or concordance for the two types in combination. HPV16-specific concordance in the studies reviewed varied from 64%–100%.
HPV16-specific concordance or concordance for any HPV type by severity of cervical lesion was reported in three studies. Daponte et alCitation28 showed an increase in HPV16/18-specific concordance with increasing severity. In contrast Alameda et alCitation26 reported a higher concordance for any HPV type in low grade squamous intraepithelial lesion (LSIL) than in high grade squamous intraepithelial lesion (HSIL). Forslund et alCitation29 showed neither an increase nor a decrease in concordance for any HPV type with increasing severity.
The only study that estimated sensitivity and specificity for HPV DNA detection in urine samples compared to cervical samples in a presumably asymptomatic, drop-in, sexual health service clinic population was published by Cuschieri et alCitation18 who reported a sensitivity of 90.6% (95% confidence interval [CI] 79.3%–96.9%) and a specificity of 67.6% (95% CI 50.2%–82.0%). In the studies with symptomatic populations, the sensitivity varied from 52.9% to 100%. Specificity varied from 66.7% to 100%.
HPV positivity in males
We identified 14 male study populations from 13 publications that reported HPV positivity in urine samples and at least one other urogenital site (). Only the studies by Lazcano-Ponce et alCitation38 and Cuschieri et alCitation18 included males less than 18-years old. The 117 males aged 16–25 years in the Cuschieri et alCitation18 study showed a 36.7% HPV prevalence in urine samples versus 29.1% in samples taken from the shaft of the penis. The study by Lazcano-Ponce et alCitation38 included 120 healthy males aged 14–55 years in Mexico (43 males in the range 14–20 years) and reported a 6.9% and 42.7% HPV prevalence in urine samples and urethra samples, respectively. Similarly, HPV prevalence in the other studies listed in was generally lower in urine samples than in other urogenital samples. For example, Weaver et alCitation39 recruited 317 sexually active university students, aged 18–25 years, and measured HPV prevalence in urine samples as well as in samples from the glans, penile shaft, scrotum, and foreskin. Samples taken from the foreskin showed the highest prevalence (28.1%), while urine samples showed the lowest prevalence (5.8%).
Table 2 Studies with human papillomavirus (HPV) DNA detected in urine from males
The percentage of urine samples in which human genomic DNA could be detected varied substantially between the studies. While Weaver et alCitation39 detected human genomic DNA in 99.7% of urine samples and 94.0%–98.3% of samples from other sites, Giuliano et al only detected human genomic DNA in 51.3% of urine samples and 84.0%–98.0% of samples from other sites, with semen samples having the highest human genomic DNA detection rate. In the study by Hernandez et al,Citation40 semen samples and urine samples had the lowest human genomic DNA detection rate, with 56.1% and 57.0%, respectively, compared to 78.8%–95.1% from other urogenital sites.
Technical issues affecting human genomic DNA and HPV DNA detection
To illustrate some of the technical variability in these studies, we have listed the urine sampling procedure and the DNA detection method used ( and ). The most common urine sampling procedure in both female and male populations was first-void urine in contrast to mid-stream urine, which Vorsters et alCitation17 suggested would be preferable if the goal were to analyze a maximum number of exfoliated cells. The order of urine and cervical sampling may also affect the HPV DNA detection rate in urine, and some studies have suggested that it is preferable to collect the urine sample first (reviewed in Sehgal et al).Citation21 In the female populations listed in , urine sampling was not always carried out prior to cervical sampling and was sometimes done after washing the genitals. For HPV DNA detection, variants of the MY09/MY11 primer were most commonly used, but other primers, such as general primer GP5+/6+, in-house primers, E6-primers, hybrid capture II, and DNA chip assays were also used. In summary, the technical variability may contribute substantially to HPV DNA detection rates.
Discussion
According to the World Health Organization (WHO), 33 countries have implemented HPV vaccination as part of their national immunization program.Citation41 Generally, vaccination is provided to girls, and it is therefore recommended to monitor the impact of vaccination on HPV prevalence among female adolescents.Citation15 In August 2012, we identified four publications that reported HPV prevalence in urine samples from asymptomatic female adolescents. HPV prevalence has been strongly associated with age, being nearly nonexistent in preadolescents, gradually increasing with sexual activity among adolescents, and generally peaking around 25 years of age.Citation42 However, regional differences in HPV prevalence do exist.Citation43 Therefore, the first step when monitoring HPV prevalence is to establish the baseline HPV prevalence in the relevant age groups. To date, only Hussain et al and O’Leary et al reported baseline HPV prevalence based on urine samples from a large unvaccinated adolescent population.Citation24,Citation25 The Hussain et alCitation25 study from India used self-collected urine of the cervix and that care should be taken when samples from healthy children attending public school and achieved a 57.3% participation rate. O’Leary et alCitation24 analyzed urine samples from 11–18-year-old school and college males (1121) and females (1341) in Scotland 4 months before vaccination was introduced in the national immunization schedule in 2008. A limitation of the study was that the estimated response rate for providing a urine sample was as low as 14%. While the low response rate can introduce bias and lead to erroneous estimates of the overall HPV prevalence, it was not directly related to the sampling method and probably refects a general challenge to achieve high response rates in this age group. This, in turn, could partially explain why only few studies measuring HPV prevalence in urine samples from female adolescents in the general population have been performed and published.
The five studies that reported HPV prevalence by lesion severity showed a similar association for paired urine and cervical samples, with higher HPV prevalence in the most severe lesions. There were major variations in HPV prevalence in urine samples across the studies. This is to some degree related to regional differences in HPV prevalence,Citation43 the age distribution of the different study populations,Citation43 and the setting in which the women were recruited. There were also differences in sampling procedures and HPV detection methods, including the number of types detected by a given assay. It is therefore not possible, as Vorsters et alCitation17 pointed out, to perform a meta-analysis on the present urine-based HPV prevalence studies.
Detection of human genomic DNA is commonly used to control for the adequacy of samples for HPV detection. Studies including female populations showed a high detection rate of human genomic DNA in urine samples (83%–100%), while male populations showed a larger range of detection rates (30%–100%). In an HPV monitoring setting, a low human genomic DNA detection rate would lead to reduced coverage and create a concern of bias in HPV estimates. In general, studies on female populations in this review indicated that high detection rates of human genomic DNA are feasible.
In cervical screening the main focus is to detect HPV or cervical abnormalities at the individual level, while population-based HPV prevalence is used more in a monitoring or epidemiological setting. Therefore, although prevalence in urine samples was lower than in cervical samples in the studies included in this review, monitoring by regular urine measurements over time may still be a useful way of identifying shifts in HPV prevalence due to imparted immunity against vaccine HPV types. However, the differences in HPV concordance of paired urine and cervical samples illustrates that HPV positivity in urine should be interpreted independently of the cervix and that care should be taken when inferring that a similar change is taking place in the cervix. On the other hand HPV detection in urine samples could be considered an independent measurement of the impact of HPV vaccination but it would have only limited public health interest. Furthermore, we observed that HPV negativity in the cervix commonly predicted an HPV-negative result in the urine as well, while HPV positivity in the cervix less commonly predicted HPV positivity in the urine. Although Daponte et al showed an increased concordance with increased lesion severity for any HPV type, other studies like Alameda et al,Citation26 Rymark et al,Citation33 and Gupta et alCitation30 showed a relatively high concordance, even in populations where HPV prevalence is low. The variability of HPV16/18-specific concordance, the types included in both of the available HPV vaccines, further exemplifies the uncertainty of using urine samples to estimate future changes in the incidence of cervical lesions.
The most comprehensive monitoring of changes in HPV prevalence would be carried out by establishing baseline HPV prevalence before measuring any impact of vaccination as well as regular measurements of HPV prevalence in both vaccinated and unvaccinated females and males. The age group (or groups) and sample size to include in HPV monitoring should be carefully selected to assure there is enough statistical power to identify changes in overall HPV prevalence as well as HPV type-specific changes. Models suggest that there will be a significant reduction in the prevalence of vaccine HPV types in males in the future because after vaccination, fewer girls will transmit HPV to their male partners.Citation44 Monitoring HPV prevalence in males could therefore be a near-term end point that could also help to estimate the effect of herd immunity. However, monitoring HPV prevalence in males presents several challenges. The differences in HPV prevalence across different urogenital sites illustrates that no single site repeatedly shows the highest HPV DNA detection rate and that urine in particular has a relatively low HPV DNA detection rate compared to other sites. In addition, male urine generally has a lower detection rate for human genomic DNA than samples from other urogenital sites. With lower detection rates for human genomic DNA, a larger sample size would be needed to detect changes with the same power as other urogenital sites. Based on these aspects, other anatomical sites seem more favorable for males.
Monitoring changes in HPV prevalence requires regular prevalence measurements over many years. A protocol with sufficient detail on technical and practical issues that influence HPV detection is therefore necessary to ensure comparability between these measurements. This includes, among other issues, urine sampling procedure, handling of samples, extraction of DNA, and assay used for HPV genotyping.Citation17 In addition it might be useful to store an extra aliquot of extracted DNA from each regular measurement to be able to perform HPV genotyping on all DNA collected from urine samples over many years. This would also allow for using any novel genotyping technology that may have developed during the monitoring period. Information on more aspects of HPV monitoring can also be found in the Human Papillomavirus Laboratory Manual issued in 2009 by the WHO HPV Laboratory Network (WHO HPV LabNet).Citation45 This manual covers guidance on specimen collection and handling for HPV testing, with the aim to assist in establishing the laboratory support required for implementation and monitoring of HPV vaccination programs. Several of the WHO HPV LabNet members are actively undertaking studies of HPV detection in urine, and a leading role for the WHO HPV LabNet in further standardizing and optimizing the technology for HPV detection in urine seems appropriate.Citation18,Citation45,Citation46
This is the first review that focuses solely on the use of urine to monitor changes in HPV prevalence in an asymptomatic population. The major shortcoming of this review is that, to date, there are few studies on the topic. We have therefore included studies from symptomatic populations and older populations that used urine for purposes other than monitoring, although these are not comparable to asymptomatic adolescents in all aspects. In addition, the studies highlighted in the present review as well as in the reviews of Vorsters et alCitation17 and Seghal et al,Citation21 showed that the large variability in sampling and genotyping methodology make direct comparisons of data, like concordance, inaccurate.Citation17,Citation21
Assuming a future reduction in overall HPV prevalence and vaccine HPV type-specific prevalence and using urine testing as a monitoring method, care should be taken when interpreting the data. Indeed the data may not necessarily mimic the true HPV distribution in the cervix nor estimate the expected reductions in cervical cancer and high-grade lesions, as indicated by variable vaccine HPV type-specific (HPV16/18) concordance between paired urine and cervical samples. There is great scientific and political interest in monitoring the early effects of HPV vaccination in the general population. However, monitoring HPV prevalence as an early measurement of vaccine impact is only possible in a few countries as substantial financial and human resources are needed as well as a 5–10-year commitment in order to demonstrate results.Citation16
Conclusion
Urine is an adequate alternative biospecimen for monitoring HPV prevalence in female adolescents to determine the early effect of HPV vaccination on a population level. Strategies for recruitment should be optimized to avoid low response rates, sampling and HPV detection protocols should be detailed and standardized to ensure comparability, and importantly, care should be taken when extrapolating findings to the cervix. In males, urine samples do not seem to be optimal for monitoring HPV prevalence due to a low human genomic DNA content compared to other urogenital sites. Although urine sampling has some advantages and is the only relevant option for sampling the general population in the youngest age groups, it also has several disadvantages, most importantly the fact that HPV prevalence in urine is only a distant measure of the main end point of vaccine impact, cervical cancer. In each situation the costs and benefits of HPV DNA detection in urine, compared to alternative monitoring options, should be carefully considered.Citation16,Citation47
Acknowledgments
We thank Elisabete Weiderpass for initiating the study and critically revising the manuscript and Trudy Perdrix-Thoma for editorial assistance.
Disclosure
EE and CO report no conflicts of interest in this work. MN has received research funding from Merck through the institution.
References
- WalboomersJMJacobsMVHuman papillomavirus is a necessary cause of invasive cervical cancer worldwideJ Pathol19991891121910451482
- zur HausenHPapillomavirus infections — a major cause of human cancersBiochim Biophys Acta199612882F55F788876633
- MunozNBoschFXde SanjoseSEpidemiologic classification of human papillomavirus types associated with cervical cancerN Engl J Med2003348651852712571259
- BoschFXde SanjoseSChapter 1: Human papillomavirus and cervical cancer — burden and assessment of causalityJ Natl Cancer Inst Monogr20033131312807939
- AultKAEffect of prophylactic human papillomavirus L1 virus-like-particle vaccine on risk of cervical intraepithelial neoplasia grade 2, grade 3, and adenocarcinoma in situ: a combined analysis of four randomised clinical trialsLancet200736995761861186817544766
- PaavonenJJenkinsDBoschFXEfficacy of a prophylactic adjuvanted bivalent L1 virus-like-particle vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trialLancet200736995802161217017602732
- Food and Drug AdministrationCenter for Biologics and Evaluation and Research, Office of Vaccines and Related Product Applications Available from: http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm094042.htmAccessed September 17, 2012
- VillaLLHPV prophylactic vaccination: The first years and what to expect from nowCancer Lett2011305210611221190794
- PaavonenJNaudPSalmeronJEfficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young womenLancet2009374968630131419586656
- BlockSLBrownDRChatterjeeAClinical trial and post-licensure safety profile of a prophylactic human papillomavirus (types 6, 11, 16, and 18) l1 virus-like particle vaccinePediatr Infect Dis J20102929510119952863
- DescampsDHardtKSpiessensBSafety of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine for cervical cancer prevention: a pooled analysis of 11 clinical trialsHum Vaccin20095533234019221517
- GiulianoARLazcano-PonceEVillaLImpact of baseline covariates on the immunogenicity of a quadrivalent (types 6, 11, 16, and 18) human papillomavirus virus-like-particle vaccineJ Infect Dis200719681153116217955433
- MunozNManalastasRJrPitisuttithumPSafety, immunogenicity, and efficacy of quadrivalent human papillomavirus (types 6, 11, 16, 18) recombinant vaccine in women aged 24–45 years: a randomised, double-blind trialLancet200937396791949195719493565
- RomanowskiBde BorbaPCNaudPSSustained efficacy and immunogenicity of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine: analysis of a randomised placebo-controlled trial up to 6.4 yearsLancet200937497061975198519962185
- FergusonMWilkinsonDEZhouTWHO meeting on the standardization of HPV assays and the role of the WHO HPV Laboratory Network in supporting vaccine introduction held on January 24–25, 2008, Geneva, SwitzerlandVaccine200927333734719007840
- Monitoring the coverage and impact of human papillomavirus vaccine — report of WHO meeting, Nov 2009Wkly Epidemiol Rec2010852523724320583384
- VorstersAMicalessiIBilckeJIevenMBogersJVan DammePDetection of human papillomavirus DNA in urine. A review of the literatureEur J Clin Microbiol Infect Dis201231562764021818524
- CuschieriKNandwaniRMcGoughPUrine testing as a surveillance tool to monitor the impact of HPV immunization programsJ Med Virol201183111983198721915874
- DunneEFNielsonCMStoneKMMarkowitzLEGiulianoARPrevalence of HPV infection among men: A systematic review of the literatureJ Infect Dis200619481044105716991079
- GiulianoARNielsonCMFloresRThe optimal anatomic sites for sampling heterosexual men for human papillomavirus (HPV) detection: the HPV detection in men studyJ Infect Dis200719681146115217955432
- SehgalAGuptaSParashariASodhaniPSinghVUrine HPV-DNA detection for cervical cancer screening: prospects and prejudicesJ Obstet Gynaecol200929758358919757259
- PrustyBKKumarAAroraRBatraSDasBCHuman papillomavirus (HPV) DNA detection in self-collected urineInt J Gynaecol Obstet200590322322716043176
- ManhartLEHolmesKKKoutskyLAHuman papillomavirus infection among sexually active young women in the United States: Implications for developing a vaccination strategySex Transm Dis200633850250816572039
- O’LearyMCSinkaKRobertsonCHPV type-specific prevalence using a urine assay in unvaccinated male and female 11- to 18-year olds in ScotlandBr J Cancer201110471221122621343934
- HussainSBharadwajMNasareVHuman papillomavirus infection among young adolescents in India: impact of vaccinationJ Med Virol201284229830522170551
- AlamedaFBellosilloBFustePHuman papillomavirus detection in urine samples: an alternative screening methodJ Low Genit Tract Dis20071115717194943
- BissettSLHowell-JonesRSwiftCHuman papillomavirus genotype detection and viral load in paired genital and urine samples from both females and malesJ Med Virol201183101744175121837790
- DaponteAPournarasSMademtzisIEvaluation of high-risk human papillomavirus types PCR detection in paired urine and cervical samples of women with abnormal cytologyJ Clin Virol200636318919316690350
- ForslundOHanssonBGRymarkPBjerreBHuman papillomavirus DNA in urine samples compared with that in simultaneously collected urethra and cervix samplesJ Clin Microbiol1993318197519798396581
- GuptaAAroraRGuptaSHuman papillomavirus DNA in urine samples of women with or without cervical cancer and their male partners compared with simultaneously collected cervical/penile smear or biopsy specimensJ Clin Virol200637319019416931139
- JacobsonDLWomackSDPeraltaLConcordance of human papillomavirus in the cervix and urine among inner city adolescentsPediatr Infect Dis J200019872272810959740
- PayanCDucancelleAAboubakerMHHuman papillomavirus quantification in urine and cervical samples by using the Mx4000 and LightCycler general real-time PCR systemsJ Clin Microbiol200745389790117229868
- RymarkPForslundOHanssonBGLindholmKGenital HPV infection not a local but a regional infection: experience from a female teenage groupGenitourin Med199369118228383095
- SellorsJWLorinczATMahonyJBComparison of self-collected vaginal, vulvar and urine samples with physician-collected cervical samples for human papillomavirus testing to detect high-grade squamous intraepithelial lesionsCMAJ2000163551351811006761
- SongESLeeHJHwangTSClinical efficacy of human papillomavirus DNA detection in urine from patients with various cervical lesionsJ Korean Med Sci20072219910417297259
- StanczukGAKayPAllanBDetection of human papillomavirus in urine and cervical swabs from patients with invasive cervical cancerJ Med Virol200371111011412858416
- StraussSJordensJZMcBrideDDetection and typing of human papillomavirus DNA in paired urine and cervical scrapesEur J Epidemiol199915653754310485346
- Lazcano-PonceEHerreroRMunozNHigh prevalence of human papillomavirus infection in Mexican males: comparative study of penile-urethral swabs and urine samplesSex Transm Dis200128527728011354266
- WeaverBAFengQHolmesKKEvaluation of genital sites and sampling techniques for detection of human papillomavirus DNA in menJ Infect Dis2004189467768514767822
- HernandezBYWilkensLRZhuXCircumcision and human papillomavirus infection in men: a site-specific comparisonJ Infect Dis2008197678779418284369
- ArbynMSanjoseSDSaraiyaMEUROGIN 2011 roadmap on prevention and treatment of HPV-related diseaseInt J Cancer201213191969198222623137
- BruniLDiazMCastellsagueXFerrerEBoschFXde SanjoseSCervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findingsJ Infect Dis2010202121789179921067372
- de SanjoseSDiazMCastellsagueXWorldwide prevalence and genotype distribution of cervical human papillomavirus DNA in women with normal cytology: a meta-analysisLancet Infect Dis20077745345917597569
- ChessonHWEkwuemeDUSaraiyaMDunneEFMarkowitzLEThe cost-effectiveness of male HPV vaccination in the United StatesVaccine201129468443845021816193
- Organization WHWHO HPV Laboratory Network Available from: http://www.who.int/biologicals/vaccines/hpv/en/index.htmlAccessed November 23, 2012
- JohnsonAMMercerCHBeddowsSEpidemiology of, and behavioural risk factors for, sexually transmitted human papillomavirus infection in men and women in BritainSex Transm Infect201288321221722261135
- WongCASaraiyaMHaririSApproaches to monitoring biological outcomes for HPV vaccination: challenges of early adopter countriesVaccine201129587888520971113
- AstoriGPipanCMuffatoGBottaGADetection of HPV-DNA in semen, urine and urethral samples by dot blot and PCRNew Microbiol19951821431497603341
- RintalaMAPollanenPPNikkanenVPGrenmanSESyrjanenSMHuman papillomavirus DNA is found in the vas deferensJ Infect Dis2002185111664166712023775
- FifeKHCoplanPMJansenKUPoor sensitivity of polymerase chain reaction assays of genital skin swabs and urine to detect HPV 6 and 11 DNA in menSex Transm Dis200330324624812616145
- D’HauwersKDepuydtCBogersJPUrine versus brushed samples in human papillomavirus screening: study in both gendersAsian J Androl20079570571017712490
- ShigeharaKSasagawaTKawaguchiSPrevalence of human papillomavirus infection in the urinary tract of men with urethritisInt J Urol201017656356820345431