Abstract
Background
The prognostic value of neutrophil–lymphocyte ratio (NLR) in patients with castration-resistant prostate cancer (CRPC) had been investigated in previous studies; however, the results remain inconsistent. This study was aimed to investigate the prognostic value of NLR in CRPC patients.
Materials and methods
Literature was identified from PubMed, Embase, Web of Science, and Cochrane, which investigated the relationship between pretreatment NLR and prognosis in CRPC patients. HRs for overall survival (OS) and progression-free survival (PFS) were extracted from eligible studies. Heterogeneity was assessed using the I2 value. The fixed-effects model was used if there was no evidence of heterogeneity; otherwise, the random-effects model was used. Publication bias was evaluated using Begg’s funnel plot test.
Results
A total of 5,705 patients from 16 studies were included in this analysis. The pooled results showed that an elevated NLR predict poor OS (pooled HR = 1.52, 95% CI: 1.41–1.63, P<0.001) and PFS (pooled HR = 1.50, 95% CI: 1.21–1.85, P<0.001) in patients with CRPC. Subgroup analysis revealed that an elevated NLR significantly predicted poor OS in Asian studies group (HR = 2.43, 95% CI: 1.47–4.01, P=0.001). The elevated NLR also significantly predicted poor PFS in Asian studies group (HR = 1.99, 95% CI: 1.30–3.06, P=0.002).
Conclusion
This study suggests that an elevated NLR predict poor prognosis in patients with CRPC.
Introduction
Prostate cancer is one of the most common malignancies in Western males, which accounts for 9% of death in males, and the second leading cause of male cancer-related death.Citation1 The standard treatment for advanced or metastatic prostate cancer is androgen deprivation therapy (ADT).Citation2 Despite the high response rate of ADT, most prostate cancer patients progressed gradually and irreversibly to castration-resistant prostate cancer (CRPC).Citation3 Docetaxel, the first-line use of chemotherapeutic agents to treat patients with CRPC, has been shown to confer a survival benefit in patients with CRPC.Citation4,Citation5 Several other agents, including cabazitaxel (CBZ),Citation6 enzalutamide (ENZ),Citation7,Citation8 abiraterone acetate (AA),Citation9,Citation10 radium-223,Citation11 and sipuleucel-T,Citation12 also have been shown to confer a survival benefit in patients with metastatic CRPC (mCRPC). Although some prognostic factors and biomarkers have been reported, a more proper predictive and prognostic biomarker is required to predict the response of patients with CRPC-received chemotherapy accurately.
Cancer-related inflammatory response plays an important role in the progression of cancer development.Citation13,Citation14 Neutrophil-to-lymphocyte ratio (NLR), a marker of the systemic inflammatory response that can be easily measured from routine complete blood counts (CBCs) in the peripheral blood, has been reported to be an independent prognostic factor in cancers.Citation15–Citation18 NLR has shown to predict poor survival of patient with localized prostate cancer and CRPC.Citation19–Citation24 However, the results of these studies for the prognostic value of NLR are inconsistent. We conducted a comprehensive meta-analysis to drive a more precise estimate of the prognostic value of the NLR in patients with CRPC.
Materials and methods
Literature search
We comprehensively searched PubMed, Embase, Web of Science, and the Cochrane electronic databases for studies published before November 17, 2017. The search strategy combined key terms related to “castration resistant prostate cancer” or “hormone-refractory prostate cancer” or “androgen independent prostate cancer” or “metastatic prostate cancer” and “Neutrophil to Lymphocyte Ratio” or “NLR” and “prognosis” or “survival” or “outcome” in humans. Two reviewers (ZW and SP) independently screened the titles and abstracts of all initially identified studies according to the selection criteria. Full-text articles of studies that met the following selection criteria were retrieved.
Inclusion and exclusion criteria
Inclusion criteria for publication selection were as follows: 1) retrospective studies on the value of NLR in predicting prognosis in castration-resistant prostate cancer patients; 2) the HRs and their 95% CIs for overall survival (OS) or progression-free survival (PFS) analysis were reported in text or could be computed from given data; 3) the value of NLR was obtained for blood sample testing; 4) defined the cutoff value of increased NLR. When multiple reports describing the same population were published, the most recent or complete report was used.
The major exclusion criteria were as follows: abstract, review, case report or comment letter; laboratory studies; animal studies; duplicate publications; published not in English.
Data extraction and quality
Two investigators (ZW and SP) independently extracted data, and a consensus was reached in case of any inconsistency with the involvement of a third author (HX). The following data were extracted from the eligible studies: first author, year of publication, country of origin, median age (range), treatment, median follow-up time, number of elevated NLR, cutoff value, and HR for survival (OS and/or PFS). For articles that only provided survival data in a Kaplan–Meier curve, software designed by Jayne F Tierney and Matthew R Sydes was used to digitize and extract the relative risk and its 95% CI.Citation25
Statistical analysis
Data were analyzed using Stata SE12.0 (StataCorp LP, College Station, TX, USA). HR with a 95% CI was selected as the effect to measure prognostic outcomes. Study heterogeneity was evaluated using the chi-squared test and ICitation2 statistic (100%×[(Q–df)/Q]),Citation26,Citation27 the value of Pheterogeneity<0.1 and ICitation2>50% represents significant heterogeneity. The fixed-effects model was used when the value of Pheterogeneity >0.1 and ICitation2<50%, otherwise the random-effects model was applied. Subgroup analysis was performed for OS and PFS analysis. Begg’s funnel plot and Egger’s linear regression test were used to evaluate the potential for publication bias. Two-tailed P-value <0.05 was considered statistically significant.
Results
Features of included studies
The selection process for this study is shown in . Through systematic literature searching, a total of 190 potentially relevant studies were identified. Overall, 94 duplicated articles were removed. 61 articles were excluded after screening titles and abstracts, including reviews, letters, meeting abstracts, laboratory studies, and other articles irrelevant to our study. After assessing the full text, 19 additional articles were excluded. Finally, 16 retrospective studies were included in the following meta-analysis.
Figure 1 Flow diagram of the study selection process.
Abbreviation: CRPC, castration-resistant prostate cancer.
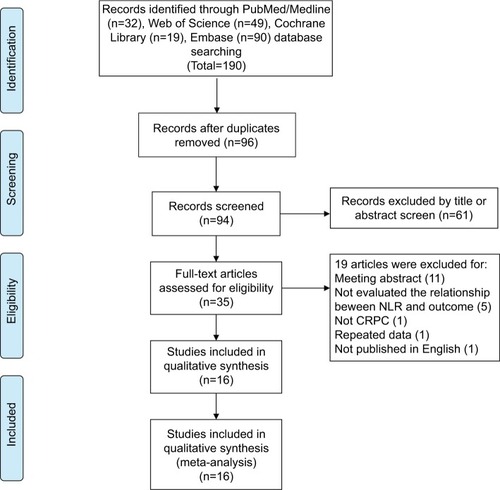
Summary characteristics of these eligible studies are shown in . The 16 selected studies (17 cohorts) published between 2013 and 2017 were included in the meta-analysis.Citation21–Citation24,Citation28–Citation39 The sample size ranged from 33 to 1,224 patients, and a total of 5,705 patients were included. All trials were conducted in adult patients with CRPC. Three studies were conducted in Asian countries (JapanCitation24,Citation30 and ChinaCitation35). Thirteen studies were conducted in non-Asian countries, including Italy,Citation34,Citation36,Citation39 UK,Citation19,Citation23 Australia,Citation29,Citation31 Germany,Citation21,Citation22 USA,Citation37 Turkey,Citation33 Canada,Citation38 and the Netherlands.Citation32 The NLR cutoff value ranged from 2.1 to 5. For the prognostic indicator of NLR in CRPC patients, six articles reported both OS and PFS, nine (10 cohorts) articles reported OS, and one article reported PFS.
Table 1 Main characteristics of the included studies
Survival outcome
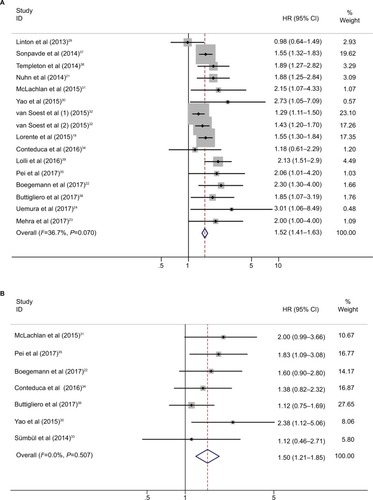
The relationship between cancer prognosis and NLR was detected in the included studies. OS and PFS were quantitatively synthesized. OS values were available from 16 cohorts with 5,571 patients with CRPC. The elevated NLR was significantly associated with poor OS (HR=1.52, 95% CI: 1.41–1.63, P<0.001; ICitation2=37.7%, Pheterogeneity=0.07; , ), which meant that patients with a higher NLR had a greater mortality risk than those with a low NLR. Seven studies with 642 patients evaluated PFS outcome. The pooled results favored the patients with low NLR (HR=1.50, 95% CI: 1.21–1.85, P<0.001; ICitation2=0.0%, Pheterogeneity =0.507).
Table 2 NLR pooled HRs and 95% CIs in meta-analysis for OS and PFS
Subgroup analysis
Subgroup analysis for OS and PFS was performed according to the cutoff value of NLR, nation, and treatment ( and ; ).
Figure 3 Subgroup analysis of pooled overall survival based on a neutrophil–lymphocyte ratio cutoff value (A), nation (B), treatment (C), and number of patients (D).
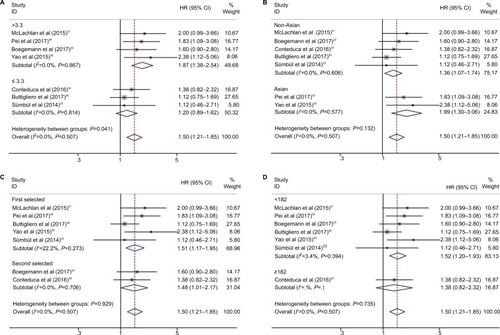
Figure 4 Subgroup analysis of pooled progression-free survival based on neutrophil–lymphocyte ratio cutoff value (A), nation (B), treatment (C), and number of patients (D).
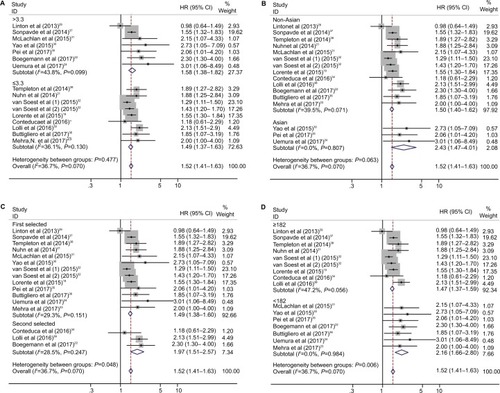
The pooled results showed that elevated NLR predicted worse OS in Asian studies (HR=2.43, 95% CI: 1.47–4.01, P<0.001; , ) and second-line treatment studies (HR=1.97, 95% CI: 1.51–2.57, P<0.001; , ). For PFS, elevated NLR predicted worse prognosis in cutoff value >3.3 studies (HR=1.87, 95% CI: 1.38–2.54, P<0.001; , ) and Asian studies (HR=1.99, 95% CI: 1.30–3.06, P=0.002; , ).
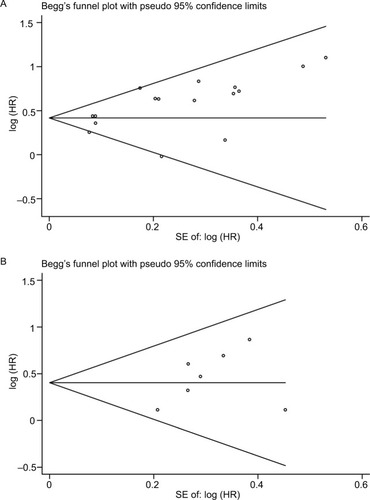
Publication bias
The publication bias in the meta-analysis was assessed by Begg’s funnel plots. Funnel plots for meta-analysis of elevated NLR and OS and PFS are shown in . The Begg’s funnel plot test (OS: P=0.096, PFS: P=0.230; ) verified that there was no obvious publication bias.
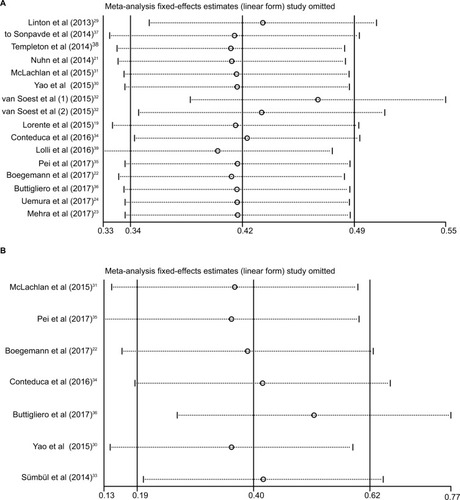
Sensitivity analysis
To evaluate the stability of the pooled results, a sensitivity analysis was performed. The result of the sensitivity analysis showed that for OS and PFS, the pooled result did not tend to exhibit alterations when an individual study was excluded ().
Discussion
The incidence of prostate cancer has been increasing in the past few years.Citation40 Most of the prostate cancer patients progressed to CRPC eventually.Citation3 Several chemotherapeutic agents, including docetaxel, CBZ, ENZ, and AA, have been shown to confer a survival benefit in patients with mCRPC. A more proper predictive and prognostic biomarker is required to predict the response of patients with CRPC-received chemotherapy accurately. It is reported that inflammatory status is associated with the progression of cancer development.Citation13,Citation14 The marker of the systemic inflammatory response, NLR, suggests an independent prognostic factor in cancers.Citation15–Citation18 NLR has shown to predict poor survival in patients with CRPC. In this meta-analysis, we included 5,705 patients from 16 selected studies (17 cohorts) to evaluate the prognostic role of the NLR in CRPC patients. The pooled results indicated that an elevated NLR is an independent predictor of poor prognosis in CRPC patients.
According to the subgroup analysis, an NLR cutoff value >3.3 had a more significant prognostic value than a cutoff value <3.3 (), which indicated that a higher NLR cutoff is more specific to predict a poor prognosis in patients with CRPC. An elevated NLR in Asian group had a more significant prognostic value than that in non-Asian group, indicating that a higher NLR is more specific to predict a poor prognosis in Asian patients with CRPC. Given the limited number of the eligible studies in the meta-analysis, although the pooled results showed that an elevated NLR is associated with a poor prognosis, it will need further investigation to identify that NLR can serve as a clinical marker of prognosis in CRPC patients.
The heterogeneity was relatively small in the included studies. It may be partially explained by nation, sample size, cutoff value, and treatment. And the subgroup analysis showed that the prognostic value of NLR was not affected by the factors included in the analysis. The sensitivity analysis also indicated that the pooled results were relatively conclusive.
Both increased neutrophil-dependent systemic inflammatory response and a lower lymphocyte-mediated antitumor immune response will lead to an elevated NLR.Citation41,Citation42 As a predominant leukocyte subset in human peripheral blood, neutrophils play an important role in tumor progression.Citation43 In comparison, lymphocytes are critical components of antitumor immunity.Citation44,Citation45 NLR is an indicator of systemic inflammatory and immune response of the host; it is also associated with the progression of cancers.Citation15–Citation18 NLR can be easily measured from routine CBCs in the peripheral blood, which is low cost, convenient, and reproducible. Moreover, NLR is closely related to the prognosis of CRPC. These reasons indicate that NLR could serve as a prognostic marker for patients with CRPC.
Several meta-analyses have been conducted on the prognosis of NLR for localized prostate cancer and mCRPC; however, the studies included in their meta-analysis were relatively small and the heterogeneity were high.Citation46–Citation48 We conducted a comprehensive meta-analysis for the prognostic value of NLR for CRPC, which included 5,705 patients from 16 selected studies (17 cohorts); the pooled results indicated that an elevated NLR is an independent predictor of poor prognosis in patients with CRPC.
Limitations
Several limitations should be acknowledged in the meta- analysis. First, the NLR cutoff value differed among the included studies, potential heterogeneity may exist. Therefore, more studies are required to identify the most suitable NLR cutoff value. Second, NLR could be affected by other diseases, such as inflammatory diseases, infection, renal diseases, and liver diseases.Citation49,Citation50 Third, the number of eligible studies in the meta-analysis is relatively small. Finally, studies with positive results are potentially more likely published than work with negative results, which could cause publication bias.Citation51
Conclusion
Our analysis on the currently available clinical evidence suggests that elevated NLR predicted a poor OS and PFS in patients with CRPC. The NLR could serve as an indicator of the efficacy of the treatment of CRPC.
Acknowledgments
This work was supported by National Natural Science Foundation of China (grants 81472682 and 81772756), and Natural Science Foundation of Tianjin (17JCZDJC35300, 15JCZDJC35400 and 15JCYBJC27200).
Disclosure
The authors report no conflicts of interest in this work.
References
- SiegelRMaJZouZJemalACancer statistics, 2014.CA Cancer J Clin201464192924399786
- HeidenreichABastianPJBellmuntJEAU guidelines on prostate cancer. Part II: Treatment of advanced, relapsing, and castration-resistant prostate cancerEur Urol201465246747924321502
- FriedlanderTWRyanCJTargeting the androgen receptorUrol Clin North Am201239445346423084523
- BertholdDRPondGRSobanFde WitREisenbergerMTannockIFDocetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer: updated survival in the TAX 327 studyJ Clin Oncol200826224224518182665
- TannockIFde WitRBerryWRDocetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancerN Engl J Med2004351151502151215470213
- de BonoJSOudardSOzgurogluMPrednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trialLancet201037697471147115420888992
- FroehnerMWirthMPEnzalutamide in metastatic prostate cancer before chemotherapyN Engl J Med20143711817551755
- ScherHIFizaziKSaadFIncreased survival with enzalu-tamide in prostate cancer after chemotherapyN Engl J Med2012367131187119722894553
- BerrutiAPiaATerzoloMAbiraterone and increased survival in metastatic prostate cancerN Engl J Med20113658766766
- RyanCJSmithMRde BonoJSAbiraterone in metastatic prostate cancer without previous chemotherapyN Engl J Med2013368213814823228172
- ParkerCNilssonSHeinrichDAlpha emitter radium-223 and survival in metastatic prostate cancerN Engl J Med2013369321322323863050
- PezaroCAttardGProstate cancer in 2011: redefining the therapeutic landscape for CRPCNat Rev Urol201292636422249187
- KowalewskaMNowakRChechlinskaMImplications of cancer-associated systemic inflammation for biomarker studiesBiochim Biophys Acta20101806216317120600631
- SaitoKKiharaKC-reactive protein as a biomarker for urological cancersNat Rev Urol201181265966622025173
- Akinci OzyurekBSahin OzdemirelTBuyukyaylaci OzdenSErdoganYKaplanBKaplanTPrognostic value of the neutrophil to lymphocyte ratio (NLR) in lung cancer casesAsian Pac J Cancer Prev20171851417142128612596
- OrdituraMGaliziaGDianaANeutrophil to lymphocyte ratio (NLR) for prediction of distant metastasis-free survival (DMFS) in early breast cancer: a propensity score-matched analysisESMO Open201612e00003827843594
- HaHNamARBangJHSoluble programmed death-ligand 1 (sPDL1) and neutrophil-to-lymphocyte ratio (NLR) predicts survival in advanced biliary tract cancer patients treated with palliative chemotherapyOncotarget2016747766047661227780932
- LiSXuXLiangDTianGSongSHeYPrognostic value of blood neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) in patients with gastric cancerZhonghua Zhong Liu Za Zhi2014361291091525623765
- LorenteDMateoJTempletonAJBaseline neutrophil–lymphocyte ratio (NLR) is associated with survival and response to treatment with second-line chemotherapy for advanced prostate cancer independent of baseline steroid useAnn Oncol201526475075525538172
- CorreaRGKrajewskaMWareCFGerlicMReedJCThe NLR-related protein NWD1 is associated with prostate cancer and modulates androgen receptor signalingOncotarget2014561666168224681825
- NuhnPVaghasiaAMGoyalJAssociation of pretreatment neutrophil-to-lymphocyte ratio (NLR) and overall survival (OS) in patients with metastatic castration-resistant prostate cancer (mCRPC) treated with first-line docetaxelBJU Int20141146bE11E1724529213
- BoegemannMSchlackKThomesSThe role of the neutrophil to lymphocyte ratio for survival outcomes in patients with metastatic castration-resistant prostate cancer treated with abirateroneInt J Mol Sci2017182380
- MehraNSharpALorenteDNeutrophil to lymphocyte ratio in castration-resistant prostate cancer patients treated with daily oral corticosteroidsClin Genitourin Cancer201715667868428606735
- UemuraKKawaharaTYamashitaDNeutrophil-to-lymphocyte ratio predicts prognosis in castration-resistant prostate cancer patients who received cabazitaxel chemotherapyBiomed Res Int201720177538647753865528948170
- TierneyJFStewartLAGhersiDBurdettSSydesMRPractical methods for incorporating summary time-to-event data into meta-analysisTrials200781617555582
- HandollHHSystematic reviews on rehabilitation interventionsArch Phys Med Rehabil200687687516731227
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ2003327741455756012958120
- LorenteDMateoJTempletonAJBaseline neutrophil-lymphocyte ratio (NLR) is associated with survival and response to treatment with second-line chemotherapy for advanced prostate cancer independent of baseline steroid useAnn Oncol201526475075525538172
- LintonAPondGClarkeSVardyJGalskyMSonpavdeGGlasgow prognostic score as a prognostic factor in metastatic castration-resistant prostate cancer treated with docetaxel-based chemotherapyClin Geni-tourin Cancer2013114423430
- YaoASejimaTIwamotoHHigh neutrophil-to-lymphocyte ratio predicts poor clinical outcome in patients with castration-resistant prostate cancer treated with docetaxel chemotherapyInt J Urol201522982783326087772
- McLachlanJMChanDLCrumbakerMAMarxGMNeutrophil– lymphocyte ratio prior to steroids as a prognostic marker in men with metastatic castration-resistant prostate cancerCancer Treat Commun201548185
- van SoestRJTempletonAJvera-BadilloFENeutrophil-to-lymphocyte ratio as a prognostic biomarker for men with metastatic castration-resistant prostate cancer receiving first-line chemotherapy: data from two randomized phase III trialsAnn Oncol201526474374925515657
- SümbülATSezerAAbalıHNeutrophil-to-lymphocyte ratio predicts PSA response, but not outcomes in patients with castration-resistant prostate cancer treated with docetaxelInt Urol Nephrol20144681531153524526335
- ConteducaVCrabbSJJonesRJPersistent neutrophil to lymphocyte ratio >3 during treatment with enzalutamide and clinical outcome in patients with castration-resistant prostate cancerPLoS One2016117e015895227434372
- PeiXQHeDLTianGPrognostic factors of first-line docetaxel treatment in castration-resistant prostate cancer: roles of neutrophil-to-lymphocyte ratio in patients from Northwestern ChinaInt Urol Nephrol201749462963528161841
- ButtiglieroCPisanoCTucciMPrognostic impact of pretreatment neutrophil-to-lymphocyte ratio in castration-resistant prostate cancer patients treated with first-line docetaxelActa Oncol201756455556228068151
- SonpavdeGPondGRArmstrongAJPrognostic impact of the neutrophil-to-lymphocyte ratio in men with metastatic castration-resistant prostate cancerClin Genitourin Cancer201412531732424806399
- TempletonAJPezaroCOmlinASimple prognostic score for metastatic castration-resistant prostate cancer with incorporation of neutrophil-to-lymphocyte ratioCancer2014120213346335224995769
- LolliCCaffoOScarpiESystemic immune-inflammation index predicts the clinical outcome in patients with mCRPC treated with abirateroneFront Pharmacol2016737627790145
- IshiokaJSaitoKSakuraMDevelopment of a nomogram incorporating serum C-reactive protein level to predict overall survival of patients with advanced urothelial carcinoma and its evaluation by decision curve analysisBr J Cancer201210771031103622918396
- CoffeltSBKerstenKDoornebalCWIL-17-producing γδ T cells and neutrophils conspire to promote breast cancer metastasisNature2015522755634534825822788
- TazzymanSNiazHMurdochCNeutrophil-mediated tumour angiogenesis: subversion of immune responses to promote tumour growthSemin Cancer Biol201323314915823410638
- GrivennikovSIGretenFRKarinMImmunityKMImmunity, inflammation, and cancerCell2010140688389920303878
- RamanathanSGagnonJIlangumaranSAntigen-nonspecific activation of CD8+ T lymphocytes by cytokines: relevance to immunity, autoimmunity, and cancerArch Immunol Ther Exp2008565311323
- MuranskiPRestifoNPAdoptive immunotherapy of cancer using CD4(+) T cellsCurr Opin Immunol200921220020819285848
- CaoJZhuXZhaoXLiXFXuRNeutrophil-to-lymphocyte ratio predicts PSA response and prognosis in prostate cancer: a systematic review and meta-analysisPLoS One2016117e015877027368058
- GuXGaoXLiXPrognostic significance of neutrophil-to-lymphocyte ratio in prostate cancer: evidence from 16,266 patientsSci Rep201662208926912340
- TangLLiXWangBPrognostic value of neutrophil-to-lymphocyte ratio in localized and advanced prostate cancer: a systematic review and meta-analysisPLoS One2016114e015398127096158
- AlkhouriNMorris-StiffGCampbellCNeutrophil to lymphocyte ratio: a new marker for predicting steatohepatitis and fibrosis in patients with nonalcoholic fatty liver diseaseLiver Int201232229730222097893
- BaltaSCakarMDemirkolSArslanZAkhanMHigher neutrophil to lymphocyte ratio in patients with metabolic syndromeClin Appl Thromb Hemost201319557923344995
- SuttonAJSongFGilbodySMAbramsKRModelling publication bias in meta-analysis: a reviewStat Methods Med Res20009542144511191259