Abstract
Background
Gastric carcinoma (GC) is the third most frequent malignancy and the second most common cancer-related cause of death cause worldwide. Gastric intraepithelial neoplasia (GIN) is a well-documented precancerous lesion of GC. In this case–control study, we comprehensively explored the clinical and pathological characteristics of GIN, with the aim to identify its potential risk factors.
Patients and methods
A total of 630 consecutive patients who underwent endoscopic submucosal dissection or mucosal resection for GIN were initially included. The detailed characteristics of all eligible patients and well-matched healthy controls were recorded and analyzed. Both univariate and multivariate logistic regression analyses were performed and presented with odds ratio (OR) and 95% confidential interval (CI), with additional subgroup analyses based on lesion location.
Results
A total of 485 GIN-eligible patients were selected, among which 156 had proximal GIN. After follow-up, 434 patients with GIN and 310 age- and gender-matched healthy controls were included in the comparative analyses. Family cancer history (FCH); alcohol abuse; tobacco abuse; intake of high sodium, preserved food, spicy food, and less fruit; Helicobacter pylori (Hp) infection; and atrophic gastritis with intestinal metaplasia were more frequent in GIN patients. Thus, FCH (OR =3.485, 95% CI: 2.031–5.981), high sodium intake (OR =2.830, 95% CI: 1.645–4.868), less fruit intake (OR =4.082, 95% CI: 2.515–6.625), Hp infection (OR =2.307, 95% CI: 1.417–3.755), and atrophic gastritis with intestinal metaplasia (OR =15.070, 95% CI: 8.999–25.237) were independent risk factors for GIN. Further subgroup analyses demonstrated that the specific independent risk factor for proximal GIN was age (OR =2.001, 95% CI: 1.003–3.994), whereas that for distal GIN was intake of high sodium (OR =3.467, 95% CI: 1.896–6.338).
Conclusion
This study reported a comprehensive overview of the clinical and pathological characteristics of GIN. FCH, high sodium intake, less fruit intake, Hp infection, and atrophic gastritis were identified as the independent risk factors for GIN.
Introduction
Gastric carcinoma (GC) is the third most common malignancy worldwide with approximately 1.3 million newly diagnosed cases.Citation1 In People’s Republic of China, GC ranks as the second most frequently occurring cancer and cause of cancer deaths; approximately 679,100 new cases and 498,000 GC-related deaths were projected to occur in 2015.Citation2 The prognosis of GC differs significantly in accordance with various stages; the 5-year overall survival rate of early GC is over 90%, while that of advanced GC is about 15%.Citation3 Early diagnosis and treatment of GC could contribute to the prolonged survival of GC patients.Citation4
Gastric intraepithelial neoplasia (GIN) is well accepted as a precancerous lesion of GC, which can be divided into 2 categories according to lesion location: proximal and distal intraepithelial neoplasia (PGIN and DGIN, respectively).Citation5 The annual incidence of GC is 6% for high-grade GIN patients within 5 years after diagnosis.Citation6 To date, numerous efforts have been devoted to identify the clinical and epidemiological features of GC;Citation7,Citation8 however, GIN remains poorly understood. Furthermore, previous studies demonstrated that proximal and distal GC (PGC and DGC) are 2 distinct entities with different epidemiologic, clinicopathologic, and molecular biological features.Citation9–Citation11 Hence, it is of vital importance to explore the potential variety between risk factors for PGIN and DGIN.
In the current study, we retrospectively enrolled 485 GIN patients to provide a comprehensive overview of the clinical and pathological features of GIN. Furthermore, 310 age- and gender-matched healthy volunteers were recruited for comparison to identify the potential risk factors for GIN.
Patients and methods
Patient selection
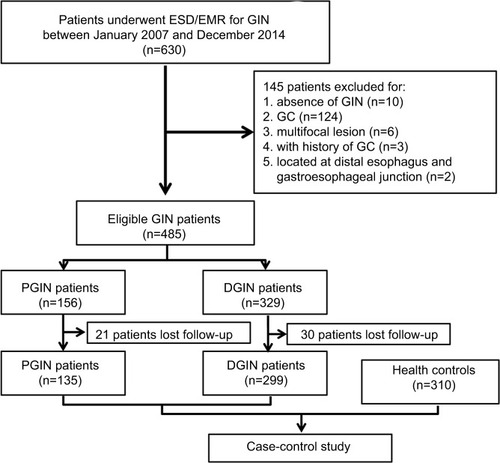
From January 2007 to December 2014, 630 consecutive patients who underwent endoscopic submucosal dissection (ESD) or endoscopic mucosal resection (EMR) for GIN at Nanjing Drum Tower Hospital were initially included in the current study. The inclusion criteria were set as follows: 1) age ≥18 years and 2) pathologically diagnosed with GIN after ESD/EMR by 2 independent experienced pathologists. The exclusion criteria were as follows: 1) pathologically diagnosed with GC after operation, 2) multifocal lesion which was defined as the distance between 2 lesions over 20 mm, 3) a history of GC, and 4) tumor located at distal esophagus and gastroesophageal junction. The detailed selection criteria are demonstrated in . A total of 485 patients with GIN were finally enrolled in this study. Furthermore, 310 gender- and age-matched outpatients who underwent endoscopy and biopsy confirmed to be negative for GC or GIN were recruited as the control group. The study protocol was approved by the institutional review board of Nanjing Drum Tower Hospital, and written informed consent was obtained from all individual participants.
Figure 1 Study flow chart.
Notes: A total of 485 eligible GIN patients were included in this study, among which 434 patients with detailed follow-up information were compared with 310 well-matched controls.
Abbreviations: EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection; GC, gastric carcinoma; GIN, gastric intraepithelial neoplasia; DGIN, distal GIN; PGIN, proximal GIN.
Study procedure
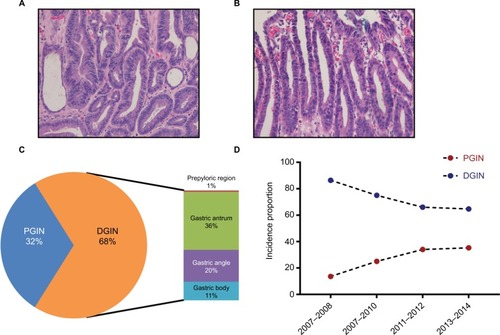
All endoscopy procedures including ESD/EMR were performed by well-trained physicians. The endoscopic morphology of superficial lesions was recoded according to the Paris classification system.Citation12 The representative histologic images of low- and high-grade GIN are shown in , respectively. Furthermore, the GIN lesions were categorized into 2 groups: PGIN, which was defined as a lesion located within 30 mm from the gastroesophageal junction and DGIN, which was described as a lesion located in the remaining regions. The electronic medical records were thoroughly reviewed, and clinical follow-up was performed by office visit or telephone contact. Information, including history of cancer, personal history, dietary habit, and present relevant diseases, were collected in a uniform form as was previously reported.Citation13 presents the detailed items and corresponding definitions.
Figure 2 Overview of GIN distribution.
Notes: Representative histological images of low-grade intraepithelial neoplasia (A); high-grade intraepithelial neoplasia (B); location distribution of GIN (C); and proportion of 2 GIN types (D). (A, B) Magnification was set at ×200.
Abbreviations: GIN, gastric intraepithelial neoplasia; DGIN, distal GIN; PGIN, proximal GIN.
Statistical analysis
The continuous variables are presented as mean ± SD after the confirmation of normal distribution and were compared using Student’s t-test or 1-way analysis of variance test. The categorical variables are presented as counts and percentages and compared with χ2 statistics or Fisher’s exact test when appropriate. To identify the potential risk factors, the univariate and multivariate logistic regression analyses were applied and are presented as odds ratio (OR) with the corresponding 95% confidential interval (95% CI). The statistical analyses were performed using SPSS (version 22.0; IBM Corporation, Armonk, NY, USA), and statistical significance was taken as a 2-sided P-value <0.05.
Results
Baseline clinical and pathological characteristics
A total of 485 GIN patients were enrolled in this study. Among these participants, 156 were diagnosed with PGIN (). The proportion of incident PGIN cases increased gradually from 13.6% in 2007–2008 to 35.3% in 2012–2014 (). The mean age was 62.3 years and differed between 2 groups (PGIN vs DGIN: 63.8±8.5 vs 61.6±9.4 years, P=0.018; ). As summarized in , significant differences were observed in the distributions of age, gender, endoscopic morphology, histologic grade, occurrence of gastritis cystica profunda, and pancreatic metaplasia between PGIN and DGIN patients. During the follow-up period, 51 (10.5%) were patients lost to followup, and the remaining 434 GIN patients with 310 age- and gender-matched healthy controls were included in the comparative analyses ().
Table 1 Clinical and pathological characteristics of patients with GIN
Comparison of risk factors for GIN and subgroup analyses stratified by PGIN and DGIN
Compared to the control group, family cancer history (FCH); alcohol abuse; tobacco abuse; intake of high sodium, preserved food, spicy food, less fruit; Helicobacter pylori (Hp) infection, and atrophic gastritis with intestinal metaplasia were more frequent in GIN patients (). Further stratification analyses revealed the similar results in both groups, except that the number of patients with PGIN aged over 60 years was higher than that of patients with DGIN (P=0.001, ).
Table 2 Comparison of subject characteristics between groups
Identification of risk factors for GIN
To identify potential risk factors for GIN, univariate logistic regression analyses were conducted, and it was found that FCH; alcohol abuse; tobacco abuse; intake of high sodium, preserved food, spicy food, and less fruit; Hp infection; and atrophic gastritis with intestinal metaplasia were found as potential risk factors for GIN (). The subgroup analyses showed that age (≥60 years) was a high risk for PGIN (OR =2.265, 95% CI: 1.455–3.524, P=0.001) than for DGIN (OR =1.348, 95% CI: 0.975–1.864, P=0.070).
Table 3 Univariate analysis of risk factors for early PGIN and DGIN
Subsequently, multivariate logistic regression analyses were performed (). FCH, high sodium intake, less fruit intake, Hp infection, and atrophic gastritis with intestinal metaplasia were identified as independent risk factors for GIN. Further stratification analyses confirmed that FCH, less fruit intake, Hp infection, and atrophic gastritis with intestinal metaplasia were independent risk factors for both PGIN and DGIN. One specific independent risk factor for PGIN was age, while that for DGIN was intake of high sodium.
Table 4 Multivariate analysis of risk factors for PGIN and DGIN
Discussion
GC is a major public health problem globally,Citation14,Citation15 and GIN has been well accepted as the premalignant lesion of GC.Citation3,Citation16 In the present study, we comprehensively explored the clinical and pathological characteristics of GIN in the Chinese population. The findings were as follows: 1) PGIN had half the number incidences of DGIN, but exhibited increasing trends during the study period, 2) age, FCH, less fruit intake, Hp infection, and atrophic gastritis with intestinal metaplasia were independent risk factors for GIN, and 3) age was a specific independent risk factor for PGIN, whereas that for DGIN was high sodium intake.
Emerging evidence indicated that GC could be divided into 2 categories, namely, PGC and DGC, due to different epidemiologic, clinicopathologic, and molecular biological characteristics.Citation9,Citation10,Citation17,Citation18 However, recent studies challenged this classification because they found that PGC was more like DGC rather than esophageal adenocarcinoma.Citation19–Citation21 Considering the existing controversy about PGC and DGC, the current study was conducted to comprehensively explore the characteristics of GC’s precancerous lesion, ie, GIN, and compare the difference between PGIN and DGIN. Among all 485 patients with GIN, 329 were diagnosed with DGIN and accounted for 67.8% of the population; a similar proportion of DGC was found in all GC cases.Citation13,Citation22 Furthermore, our results showed an increasing trend for PGIN as its proportion increased gradually during the study period 2007–2014, which was similar to the trends for PGC.Citation23–Citation25
To identify risk factors for GIN, a total of 434 GIN patients with 310 well-matched controls were recruited. Based on the results of logistic regression analyses, FCH, high sodium, less fruit intake, Hp infection, and atrophic gastritis with intestinal metaplasia were identified as independent risk factors for GIN. All abovementioned parameters except Hp infection were also well documented as the risk factors for GC, which can support the conclusion that GIN is one of the important premalignant lesions of GC to some extent.Citation26,Citation27 In this study, Hp infection has been identified as an independent risk factor for GIN with an OR of 2.307 (95% CI: 1.417–3.755). Although some controversies still exist, a growing body of evidence indicated that Hp infection is etiologically related to gastric cancer, and the eradication of Hp infection could contribute to a reduced incidence of GC.Citation27,Citation28 However, the detailed biological mechanisms underlying Hp infection-induced GIN remain far from understood. In addition, we also examined the association between anxiety/depression status and GIN risk; however, the results were negative. In a Chinese report including 118 patients with gastroesophageal precancerous lesions and 210 healthy controls, it was demonstrated that the anxiety and depression scale scores were higher in patients.Citation29
Considering the potential variations between PGIN and DGIN, subgroup analyses were conducted. FCH, less fruit intake, Hp infection, and atrophic gastritis with intestinal metaplasia were proven as the independent risk factors for both PGIN and DGIN. In particular, age was a specific independent risk factor for PGIN while that for DGIN was intake of high sodium. The results suggested that PGIN and DGIN shared similar etiology, similar to PGC and DGC. Further studies are warranted to validate the findings.
This study comprehensively explored the potential risk factors for Chinese GIN patients in the real-world setting and found some positive results. However, some limitations should be acknowledged in interpreting the results. First, the retrospective nature might induce selection bias, even though the study was stringently designed and conducted. Second, the limited sample size in a single institute might reduce the statistical power of the results. Third, the lost follow-up rate was relatively high (10.5%), though various efforts have been devoted and the statistical analysis showed balanced in both PGIN and DGIN groups.
Conclusion
In summary, this study provided a comprehensive overview of the clinical and pathological characteristics of GIN. FCH, high sodium intake, less fruit intake, Hp infection, and atrophic gastritis were identified as the independent risk factors for GIN. Further well-designed, prospective, and unbiased studies with a larger sample size should be conducted to verify our findings.
Supplementary material
Table S1 Detailed items and the corresponding definitions
Disclosure
The authors report no conflicts of interest in this work.
References
- Global Burden of Disease Cancer CollaborationFitzmauriceCAllenCGlobal, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the Global Burden of Disease StudyJAMA Oncol20173452454827918777
- ChenWZhengRBaadePDCancer statistics in China, 2015CA Cancer J Clin201666211513226808342
- Van CutsemESagaertXTopalBHaustermansKPrenenHGastric cancerLancet2016388100602654266427156933
- Lopez-BasaveHNMorales-VasquezFRuiz-MolinaJMGastric cancer in young people under 30 years of age: worse prognosis, or delay in diagnosis?Cancer Manag Res20135313623580357
- KatoMDiagnosis and therapies for gastric non-invasive neoplasiaWorld J Gastroenterol20152144125131251826640329
- de VriesACvan GriekenNCLoomanCWGastric cancer risk in patients with premalignant gastric lesions: a nationwide cohort study in the NetherlandsGastroenterology2008134494595218395075
- KarimiPIslamiFAnandasabapathySFreedmanNDKamangarFGastric cancer: descriptive epidemiology, risk factors, screening, and preventionCancer Epidemiol Biomarkers Prev201423570071324618998
- AshktorabHKupferSSBrimHCarethersJMRacial disparity in gastrointestinal cancer riskGastroenterology2017153491092328807841
- Cancer Genome Atlas Research NetworkComprehensive molecular characterization of gastric adenocarcinomaNature2014513751720220925079317
- HayakawaYSethiNSepulvedaARBassAJWangTCOesophageal adenocarcinoma and gastric cancer: should we mind the gap?Nat Rev Cancer201616530531827112208
- YuXHuFLiCYaoQZhangHXueYClinicopathologic characteristics and prognosis of proximal and distal gastric cancerOnco Targets Ther2018111037104429520154
- Endoscopic Classification Review GroupUpdate on the paris classification of superficial neoplastic lesions in the digestive tractEndoscopy200537657057815933932
- FangCHuangQLuLRisk factors of early proximal gastric carcinoma in Chinese diagnosed using WHO criteriaJ Dig Dis201516632733625754397
- AllemaniCMatsudaTDi CarloVGlobal surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countriesLancet2018391101251023107529395269
- SitarzRSkieruchaMMielkoJOfferhausGJAMaciejewskiRPolkowskiWPGastric cancer: epidemiology, prevention, classification, and treatmentCancer Manag Res20181023924829445300
- MarkowskiARMarkowskaAGuzinska-UstymowiczKPathophysiological and clinical aspects of gastric hyperplastic polypsWorld J Gastroenterol201622408883889127833379
- SouzaRFSpechlerSJConcepts in the prevention of adenocarcinoma of the distal esophagus and proximal stomachCA Cancer J Clin200555633435116282279
- XingXJiaSWuJClonality analysis of synchronous gastro-oesophageal junction carcinoma and distal gastric cancer by whole-exome sequencingJ Pathol2017243216517528671728
- HuangQShiJFengAGastric cardiac carcinomas involving the esophagus are more adequately staged as gastric cancers by the 7th edition of the American Joint Commission on Cancer Staging SystemMod Pathol201124113814620852593
- SuhYSHanDSKongSHShould adenocarcinoma of the esophagogastric junction be classified as esophageal cancer? A comparative analysis according to the seventh AJCC TNM classificationAnn Surg2012255590891522504190
- ZhaoELingTXuJTurning left or right? A comparative analysis in adenocarcinomas of the esophagogastric junction according to the seventh AJCC TNM classification for cancers of the esophagus and stomach: experience in a Chinese single institutionInt J Clin Exp Med201587106681067726379858
- ShiJSunQXuBYChanging trends in the proportions of small (≤2 cm) proximal and non-proximal gastric carcinomas treated at a high-volume tertiary medical center in ChinaJ Dig Dis201415735936624720626
- HuangQFangCShiJDifferences in clinicopathology of early gastric carcinoma between proximal and distal location in 438 Chinese patientsSci Rep201551343926310451
- SedefAMKoseFSumbulATPatients with distal intestinal gastric cancer have superior outcome with addition of taxanes to combination chemotherapy, while proximal intestinal and diffuse gastric cancers do not: does biology and location predict chemotherapy benefit?Med Oncol201532247625572818
- LuoGZhangYGuoPWangLHuangYLiKGlobal patterns and trends in stomach cancer incidence: age, period and birth cohort analysisInt J Cancer201714171333134428614909
- VeneritoMLinkARokkasTMalfertheinerPGastric cancer – clinical and epidemiological aspectsHelicobacter201621Suppl 1394427531538
- GrahamDYHelicobacter pylori update: gastric cancer, reliable therapy, and possible benefitsGastroenterology20151484719731.e325655557
- LeeYCChiangTHChouCKAssociation between Helicobacter pylori eradication and gastric cancer incidence: a systematic review and meta-analysisGastroenterology2016150511131124.e526836587
- MaSRMaQHaoCQAnalysis of psychological status and relevant factors of patients with esophageal and gastric cardia precancerous lesions in Linzhou of HenanZhonghua Yu Fang Yi Xue Za Zhi2017518670674 Chinese28763913
