Abstract
Objective
To retrospectively evaluate the long-term efficacy and safety of radiofrequency ablation (RFA) with systemic chemotherapy (CT) in treatment of solitary liver metastasis after surgery for colorectal cancer (CRC).
Methods
This single-center study was conducted at the Hunan Provincial Cancer Hospital from June 2006 to December 2015 with median follow-up time of 26 months. Percutaneous ultrasound-guided RFA was carried out on eligible patients with solitary liver metastasis after surgery for CRC. After a week, ablation status was confirmed by MRI. Post MRI, all patients received systemic CT with or without molecular-targeted therapy. Survival rate was evaluated and survival curve was constructed with Kaplan–Meier analysis. Log-rank test and Cox regression model were used for univariate and multivariate analysis, respectively, to determine the independent prognostic factors for survival rate.
Results
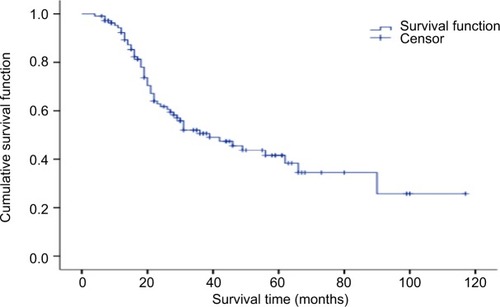
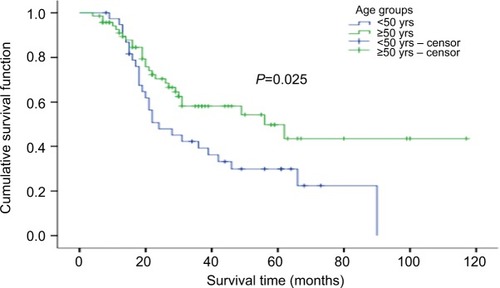
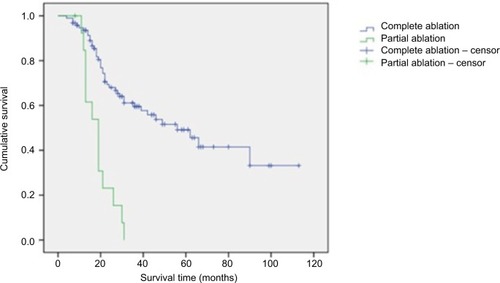
A total of 109 eligible patients (mean age, 53.84±11.71; mean tumor mass diameter, 3.4+2.01 cm) were enrolled in this 10-year study. After RFA, 95 patients achieved complete ablation, and 14 patients achieved partial ablation, with median ablation time of 26 minutes (range: 12–120 minutes). The median survival time required for achieving complete and partial ablation was 56.0 and 19.0 months, respectively (P<.01). After RFA and adjuvant systemic CT, the 1-, 3-, and 5-year survival rates were 92.3%, 50.7%, and 41.6%, respectively, with the median (mean) survival time of 39.0 (56.5) months. Age was the only significant independent prognostic factor with better survival rate observed in patients aged ≥50 years than those aged <50 years (P<0.05). The incidence of complications was minimal (1.8%) with only two cases: one biliary fistula and one liver hemorrhage.
Conclusion
RFA combination with systemic CT was safe; it showed long-term efficacy in patients with solitary liver metastasis after surgery for CRC and can be a preferred treatment.
Introduction
Colorectal cancer (CRC) is one of the most commonly diagnosed cancers worldwide, and is ranked second and third in female and male patients, respectively.Citation1 Though the incidence is the highest in North America, Europe, and New Zealand/Australia, there has been an evolving trend in Asia and eastern Europe due to change in lifestyle.Citation1,Citation2 According to the 2015 statistics in China, CRC is the fifth most commonly diagnosed cancer in male patients and fourth most commonly diagnosed cancer in female patients, causing one of the highest mortalities (191,000 deaths in 2015).Citation3 A study by Dennis DL et al revealed that majority of patients with CRC were not as physically active as subjects without cancer, on a regular basis.Citation4 Also, western lifestyle changes, such as alcohol consumption, sleep deprivation, obesity, etc correlate with higher incidences of CRC.Citation5
Liver is one of the most common sites for metastasis in CRC and in about 50% of the metastasis of liver cases observed.Citation6 The gold standard of treatment for colorectal liver metastasis (CRLM) is surgical resection.Citation7 The 5-year survival after resection ranged between 35% and 58% in patients with CRLM.Citation8–Citation11 Due to the anatomic, functional, and medical complexities, resection is possible only in about 10%–20% of patients with liver metastasis.Citation12 Moreover, after resection, the recurrence is about 60% in patients with CRLM.Citation13,Citation14 Chemotherapy (CT) is also widely used in the treatment of CRLM. The addition of irinotecan and oxaliplatin to the traditional 5-fluorouracil and leucovorin combination improved the response from 20% to about 56%.Citation15–Citation18 Target therapies, such as bevacizumab or cetuximab in combination with CT with FOLFIRI showed a response rate of about 70% in patients with CRC.Citation19 The overall survival (OS) rate for bevacizumab and FOLFOXIRI combination was reported to be 24.9%,Citation20 whereas that for cetuximab and FOLFOXIRI combination was 46.2%.Citation21 However, CT has serious complications such as steatohepatitis and sinusoidal obstruction syndrome, causing hepatic injury in patients undergoing liver resection for CRLMs.Citation22 Hence, less-invasive ablative procedures like radiofrequency ablation (RFA), microwave coagulation therapy, and percutaneous ethanol injection have emerged as treatment of choice in nonsurgical CRLM cases.Citation23–Citation26 RFA has proved advantageous compared with other local ablative techniques in hepatocellular carcinoma due to several factors, including its minimal invasiveness, tumor control with good long-term survival with acceptable morbidity.Citation27–Citation29 CRLM patients treated with RFA have shown a 5-year survival of about 26%–33%.Citation30,Citation31 Though RFA has shown a local recurrence of 12%–18%,Citation32,Citation33 few studies have shown a recurrence as high as 47%.Citation34 This has led to the need for adjuvant therapy. However, few studies used a combination of RFA and CT in the treatment of CRLM patients and found a recurrence of about 15% (26 out of 168 subjects) with no recurrence at the site of RFA.Citation35 Similar study with combination of RFA and CT in 202 subjects reported an OS rate of 48% though 32% showed recurrence at RFA site; however, retreatment with ablation increased their OS compared with those who received no retreatment (45.5 vs 31.1 months, P<.001),Citation36 suggesting that combination therapy improves long-term survival in patients with CRLM. In a country like China, where the mortality rate is high, there is an unmet need of large-scale studies to improve the OS in this challenging area of cancer. Therefore, the present study was designed in China to evaluate the efficacy and safety of RFA therapy combined with systemic CT in patients with solitary CRLM.
Materials and methods
Study design and patient selection
This single-center study was conducted at the Hunan Provincial Cancer Hospital from June 2006 to December 2015. The eligibility criteria included male or female patients aged between 18 and 85 years, who had a histologically confirmed adenocarcinoma after surgery for CRC, an Eastern Cooperative Oncology Group score between 0 and 1,Citation37 single intrahepatic metastatic lesion confirmed by MRI or CT, etc. All subjects included in this study had clinically diagnosed liver metastasis after CRC surgery.
The study was approved by the Hunan Provincial Cancer Hospital review board. Written informed consent was taken from patients before enrolling into the study. There was no bias in selecting the patient population. Based on patient’s affordability and tissue biopsy and gene detection test for KRAS and NRAS genes were conducted prior to RFA.
RFA procedure and CT
An ultrasound-guided RFA through percutaneous approach under general anesthesia was performed in all patients. The devices used for the procedure were as follows: (i) RFA treatment system using internally cooled tip electrodes (Valleylab, Boulder, CO, USA) for generating radiofrequency; and (ii) ultrasound equipment (GE LOGIQ P5 Color and Philips CX50 portable color Doppler ultrasound, convex array probe, the frequency of 3.5–4.0 MHz) that acts as a guide for the needle electrode to reach the tumor location. Examination of blood, urine, liver, and renal function, and electrolytes was examined prior to RFA. For pathologic analysis, biopsy tissue sample was obtained by tumor puncture from those who agreed for biopsy test and centesis. Due to age and economic reasons, liver tissue was taken only from some patients to examine KRAS and NRAS genes.
The RFA technique and design depended on the morphology of the lesion: (i) for the long lesion, single-needle multi-point ablation for 12 minutes per hour; ii) for flat oval lesions, multi-needle multipoint ablation for 12 minutes per point; iii) for cylindrical lesions, multi-needle point up and down for 12 minutes per hour; and iv) for the liver surface, RF needle was placed 5 mm from the organ with caution for high-risk areas like gallbladder, bile duct, etc. MRI was performed 1 week after RFA to check on the ablation status. Blood, liver, and renal function were repeated about 1 week after RFA, then to prolong the effects of RFA and prevent recurrence, systemic CT or systemic CT along with molecular-targeted therapy (cetuximab or bevacizumab) was initiated.
Data collection, outcomes measured, and follow-up
All cases were followed up till June 30, 2016 via telephone, letters, personal visit, and household registration survey from police department, for determining survival and cause of death. Survival time was calculated from the time of hospitalization for liver metastasis. No patient was lost to follow-up. All patients who underwent RFA and systemic CT were evaluated. The patients were followed up at least once a year during the study. The outcomes studied included as follows: (i) 1-, 3-, and 5-year survival rate; and ii) survival difference with respect to gender (male and female), age (<50 and ≥50 years old), tumor site (left and right liver), tumor size (≤5 - and >5 cm), and CT regimen after RFA (systemic CT and systemic CT combined with molecular-targeted therapy).
Statistical analysis
The statistical analysis was performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA). Descriptive statistics was used to summarize baseline characteristics. Continuous variables (age, tumor mass size, tumor mass location, survival time, number of subjects receiving CT, and number of subjects receiving CT along with molecular-targeted therapy) were expressed as mean, median, and SD. Kaplan–Meier method was used to predict long-term survival. To compare the survival difference with respect to gender, age, tumor mass site, tumor mass size, and CT regimen after RFA, univariate analysis was performed by log-rank test. P value <0.05 was considered statistically significant. For those variables which were significant in the univariate analysis, Cox regression model was used for multivariate analysis to predict the independent prognostic factors for survival rate.
Results
Patient demographics and clinicopathologic features
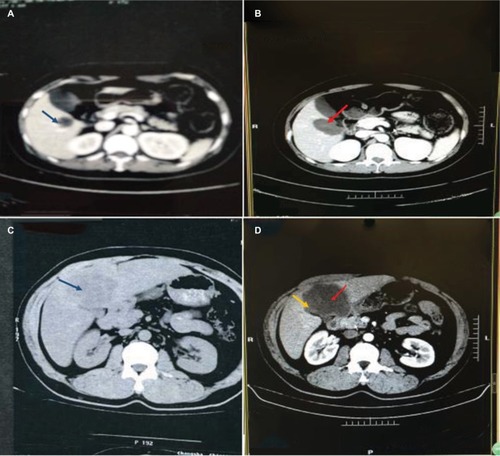
A total of 109 patients with CRC and single liver metastasis were enrolled over the 10-year study period. The median follow-up time was 26.0 months, with the longest survival time of 113 months. Most of the patients visited hospital 2–4 times in 1 year to be reviewed. Although no cases dropped out of the study, 54 out of 109 patients died and the cause of all deaths were tumor-related and not RFA-related. The mean age of the study population was 53.84+11.71 years. The mean tumor mass size among all subjects was 3.4+2.01 cm (maximum: 12.4 cm), with 80.7% of subjects having the right liver lobe as the tumor location. There were 92 patients with tumor measuring ≤5 cm and 17 with tumor measuring >5 cm. Ablation was complete (, blue arrow marks lesion and red arrow points toward ablated area) in 95 (87.2%) patients and partial (, yellow arrow points toward remanant lesion) in 14 (12.8%) patients with median RFA time of 26 minutes (range: 12–120 minutes). Post RFA, the number of patients who underwent standardized systemic CT and standardized systemic CT combined with molecular-targeted therapy was 83.4% and 16.5%, respectively. The demographic and clinicopathologic data are summarized in .
Table 1 Patient demographics and clinicopathological features
Figure 1 Partial and complete ablation.
Notes: (A) Sigmoid colon cancer postoperative right hepatic gallbladder 2.4 cm metastasis (blue arrow). (B) RFA showed 3.7 cm complete ablation area (red arrow). (C) Ascending colon cancer postoperative right liver 8.5 cm metastases (blue arrow). (D) RFA showed partial ablation (red arrow), the surrounding a little residue (yellow arrow).
Abbreviation: RFA, radiofrequency ablation.
Biopsy of liver lesions is important; however, some patients disagreed for biopsy, and some were not suitable for percutaneous needle biopsy because of special locations of the lesions (n=39).
Survival outcome
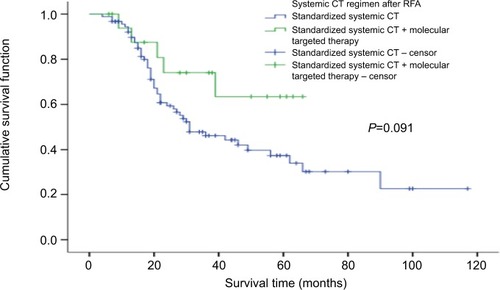
The 1-, 3-, and 5-year cumulative survival rates were 92.3%, 50.7%, and 41.6%, respectively. The overall mean survival time was 56.5 months and the overall median survival time was 39.0 months. The 1-, 3-, and 5-year survival rates for standardized systemic CT were 94.4%, 46.2%, and 37.2%, respectively, with mean survival time of 52.8 months and median survival time of 31.0 months (). The 1-, 3-, and 5-year survival rates for standardized systemic CT+ molecular targeting were 93.8%, 74.0%, and 63.5%, respectively, with mean survival time of 50.3 months.
Factors affecting survival outcome
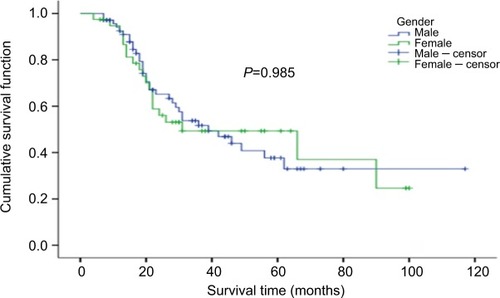
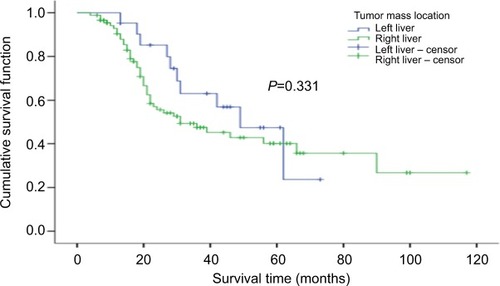
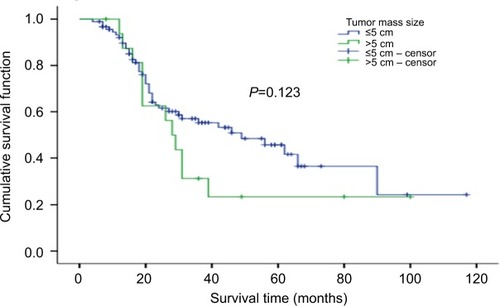
Log-rank method was used to compare survival rate difference between different groups, including age, gender, tumor size, tumor location, and CT regimen after RFA (). No significant difference in survival rates were observed between male and female patients (P=0.985; ). A significant difference in the survival rate was observed among the different age groups (P=0.025; ) with the survival rate being better for patients aged ≥50 years. For ≥50 years group, the 1-, 3-, and 5-year survival rates were 91.0%, 58.0%, and 49.7%, respectively, with median (mean) survival time of 56.0 (67.3) months. For <50 years group, the 1-, 3-, and 5-year survival rates were 94.7%, 39.2%, and 29.8%, respectively, with median (mean) survival time of 24.0 (40.8) months. There was no significant difference in survival between different tumor sites and tumor mass size groups (P=0.331 and P=0.123; and , respectively). Also, no statistically significant difference in survival was noticed between the different CT regimen after RFA (P=0.091; ). Age was included as an independent prognostic factor for the final equation by Cox regression analysis. Those patients aged ≥50 years were 0.550 times at risk of death than patients aged <50 years (). Other factors were excluded in the equation.
Table 2 Univariate analysis of prognostic factors of long-time survival
Table 3 Multivariate analysis of independent prognostic factors for survival rates
Figure 7 Comparison of survival rates of different treatment regimens.
Abbreviations: CT, chemotherapy; RFA, radiofrequency ablation.
The 1-, 3-, and 5-year survival rates for patients who underwent complete ablation were 93.5%, 59.5%, and 49.1%, respectively. The 1- and 2-year survival rates for patients who underwent partial ablation were 84.6% and 23.1%, respectively, while the 3- and 5-year survival rate cannot be calculated. The median survival time for patients who underwent complete ablation and partial ablation on liver tumor were 56.0 and 19.0 months, respectively, with a statistically significant difference observed (P<0.01) ().
Treatment complications
The incidence of serious complications was 1.8% (2/109). There was a case of biliary fistula, which was treated by B-guided puncture followed by anti-inflammatory agents. One case of liver hemorrhage was treated through hepatic artery catheterization embolization. No other serious com plications like intestinal fistula, intestinal or gallbladder perforation were reported.
Discussion
In this study, we studied the efficacy of RFA with systemic CT in the treatment of solitary liver metastasis after surgery for CRC. In our study, post RFA and systemic CT, the survival rate of patients was found to be satisfactory with age emerging as the independent prognostic factor. On follow-up, minimal complications were observed in the 10-year study period.
Surgical resection is the standard therapy for CRLM associated with high survival rate and low mortality and morbidity.Citation9,Citation11,Citation38 The mortality rate reported in our study was comparable with other published reports. There was no case of mortality related to RFA. There was no case of mortality related to RFA. All deaths reported were due to tumor. Similarly, Solbiati L et al did not observe procedure-related death,Citation39 whereas in study by Boame N et al,Citation40 postoperative death was reported in 1.2% of subjects. CT and RFA are the proposed alternative methods in unresectable hepatic neoplasms.Citation41,Citation42 RFA is a minimal invasive procedure based on the principle of tumor cell death by coagulative necrosis at a temperature >60°C. The RF waves produce thermal energy, causing intracellular protein denaturation, destruction of the cell membrane, and thrombosis of the microvasculature.Citation28,Citation29,Citation43 Though RFA has advantages of easy applicability and safety, it is not suggested for larger tumors (>5–6 cm) as it is incapable of complete necrosis in these cases.Citation44 The biggest drawback of RFA in tumors of liver tissue is its high recurrence rate.Citation45,Citation46
In case of solitary metastasis of liver, RFA is a better choice.Citation31,Citation47,Citation48 Multiple studies have compared surgical resection and RFA in patients with CRLM. A 10-year retrospective study on patients with CRLM reported overall recurrence to be common after RFA (84%) compared with RFA + resection (64%) and resection alone (52%, P<0.001).Citation11 The OS at 5 years was the highest (58%) after resection. Both liver-only recurrence and true local recurrence were significantly more common after RFA compared with resection.Citation11 The 4-year survival was significantly lower in patients with RFA compared with resection and combination therapy of resection and RFA (22%, 65%, 36%; P<0.0001).Citation11 However, in cases where resection was not possible, the survival in RFA + resection or RFA monotherapy was higher than CT alone (P<0.0017).Citation11 Another retrospective study analyzing 12-year data showed significantly lower recurrence (5% vs 37%, P<0.001); a significantly higher 5-year OS was observed in patients with CRLM, who were treated with hepatic resection, compared with RFA (71% vs 27%; P<0.001).Citation49 The local recurrence was higher in RFA compared with resection and the 5-year recurrence-free survival was significantly lower in RFA treated patients compared with patients who underwent resection (P<0.001).Citation49 On the contrary, Leblanc et al reported that the local recurrence and survival rates were comparable and not statistically different between RFA, surgical resection, and combination therapy when size and topographic characteristics of liver metastases were considered for RFA.Citation50 Similar results were observed in other studies on recurrence rates and OS between RFA and hepatic resection in small tumors (<3 cm) in solitary CRLM.Citation51,Citation52 Thus, these studies support that RFA could be an alternative in case of unresectable tumors of small size. In our study, we kept 5 cm as the tumor diameter because threshold has been used in previously reported studies on colon cancerCitation53,Citation54 and safety and efficacy of RFA in smaller tumor (average range of tumor diameter: 2.8 and 2.1–3.4 cm)Citation40,Citation55 are already reported.
CT used after resection has proven to lower recurrence compared with resection alone.Citation56 Based on these data, studies using RFA and CT were conducted in patients with CRLM. In our study, the 1-, 3-, and 5-year cumulative survival rates were 92.3%, 50.7%, and 41.6%, respectively, after RFA and CT. The mean survival time was 56.5 months and the median survival time was 39.0 months. Our results are comparable with several other studies that reported survival benefits of RFA and systemic CT in patients with solitary CRLM. A study by Gillams et al reported a median survival of 59 months with 1-, 3-, and 5-year survival rates being 97%, 84%, and 40%, respectively in 40 patients with solitary, unresectable CLRM, with an average diameter of 2.3 cm (range: 0.8–4.0 cm).Citation57
Another study reported similar survival outcomes in 100 patients with CRLM, who underwent RFA, as the first-and second-line treatment after CT. The 1-, 3-, and 5-year survival rates were 90%, 42%, and 30.5%, respectively.Citation58 A study, comparing systemic therapy and RFA+ systemic therapy, reported a survival rate of 61.7% for 30 months in combination arm with median OS of 45.3 months. There was also a significant improvement in the 3-year progression-free survival rate in case of combination therapy.Citation59 A retrospective study conducted by Knudsen et al evaluated patients with CRLM treated with RFA after systemic CT. The results showed a 5-year survival of 34% with a median survival time of 39 months.Citation60 Gillams et al conducted a study of 69 patients with CRLM who were not eligible for resection. The patients underwent RFA with CT (either before, after, or along with RFA). The median survival time was 27 months with 1-, 3-, and 4-year survival of 90%, 34%, and 22%, respectively.Citation61
Complete ablation was defined as no abnormal enhancement in and around lesions by enhanced CT or MRI 1 week after RFA on liver tumor. Partial ablation was defined as abnormal enhancement in and around lesions by enhanced CT or MRI 1 week after RFA on liver tumor. The previous studies reported safety and efficacy of this treatment regimen in relatively smaller tumors (average tumor size: 2.8 cm55; tumor diameter range: 2.1–3.4 cm40), whereas in our study, we have compared safety and efficacy of RFA in tumors with a diameter of ≤5 and >5 cm. Out of 109 patients in this study, there were 92 patients with a tumor diameter of ≤5 cm, 17 with that of >5 cm, which averages the diameter to 3.4+2.01 cm (maximum: 12.4 cm). The size of tumor substantially affects the efficacy and thereby, the recurrence rate of RFA.Citation55,Citation62 The 1-, 3-, and 5-year survival rates were 92.3%, 50.7%, and 41.6%, respectively, with mean survival at 56.5 months and median at 39.0 months. Our results were lower compared with Gillams’ results in terms of median survival (39 vs 59 months) and 3-year survival rate (50.7% vs 84%), while the results were comparable in terms of 5-year survival rate (41.6% vs 40%). Our results were better than those reported by MachiCitation48 (5-year survival rate: 30.8%, median survival: 28 months) and TreskaCitation52 regarding long-term survival rate. Some of these studies included multi-liver metastatic lesions and some only included ≤3 cm solitary lesion, and most of the studies did not include cases with lesions >3 or even >5 cm.
Although several factors were studied, including gender, age group, tumor location, tumor size, the association between survival outcomes and systemic CT, and the association between systemic CT and molecular-targeted therapy after RFA, age was the only independent prognostic predictor for survival on multivariate analysis as subjects <50 years of age had higher risk of death than those aged ≥50 years. We suspect that the comparatively higher survival rate observed in patients aged >50 years might be due to presence of more aggressive tumors in younger subjects (aged <50 years).Citation63–Citation65 Similar results were observed in another study that used RFA as first- or second-line treatment after CT; age (70 years) was found to be the significant parameter, affecting survival, on multivariate analysis.Citation36,Citation58
Although RFA is easy to operate and is less invasive, some serious complications have been reported. The complications include bleeding, needle track seeding, biliary fistula, intestinal fistula, liver abscess, portal vein thrombosis, biliary perforation, and in some cases, pulmonary problem.Citation28 The incidence of complication in the present study was 1.8%, which was similar to another study that reported 1.3% of adverse events.Citation36
To the best of our knowledge, this was the first long-term study conducted in China, which evaluated the efficacy and safety of ultrasound-guided RFA along with systemic CT and molecular-targeted therapy used in the treatment of solitary CRLM. The results were satisfactory with improvement in OS. We also believe that: (i) single-operation technology can significantly reduce the blindness and number of punctures, thereby improving the accuracy and efficacy; (ii) according to the morphology and size of solitary lesion, single-needle multipoint or multi-needle multipoint, 12 minutes per point design could be used, thereby expanding ablation area and reducing the residual tissue and local recurrence. In this study, the median ablation duration was 26 minutes and the complete ablation rate was 87.2%. The median survival time of patients of complete and partial ablation were 56.0 and 19.0 months, respectively, with a statistically significant difference observed (P<0.01). Although survival rate was higher in the RFA along with systemic CT and molecular-targeted therapy compared with RFA and systemic CT, it could not reach any statistical significance due to the small sample size. More large-scale randomized studies are warranted to explore the efficacy of RFA in combination with systemic CT and RFA in combination with systemic and targeted therapies in increasing the OS benefit of solitary CRLM; and (iii) solitary large liver metastatic lesion was reported in this study. A total of 17 patients had lesions of >5 cm diameter with the largest among them being of 12.4 cm diameter. This is the first study reporting RFA targeted at large tumors.
Conclusion
RFA along with systemic CT is effective and safe in patients with solitary liver metastasis after surgery for CRC. However, randomized control trials with more frequent follow-ups are warranted in future to ascertain its efficacy in treating solitary liver metastasis after surgery for CRC.
Acknowledgments
The authors would like to acknowledge Wu Shengqi, Chief Physician, Hunan Provincial Cancer Hospital, China, who helped in the treatment protocol and has extended support in carrying out the statistical analysis for the study. All the investigators involved in the study contributed in development and approval of the manuscript. The authors acknowledge Dr Priyanka Nair and Dr Anuradha Nalli’s support (Indegene Pvt Ltd) in providing medical writing assistance in the development of this manuscript, funded by Medtronic China Co Ltd. The study was funded by Medtronic China Co Ltd.
Disclosure
The authors report no conflicts of interest in this work.
References
- TorreLABrayFSiegelRLGlobal cancer statistics, 2012: Global Cancer Statistics, 2012CA Cancer J Clin2015658710825651787
- CenterMMJemalASmithRAWardEWorldwide variations in colorectal cancerCA Cancer J Clin200959636637819897840
- ChenWZhengRBaadePDCancer statistics in China, 2015: Cancer Statistics in China, 2015CA Cancer J Clin20166611513226808342
- DennisDLWaringJLPayeurNCosbyCDaudtHMMaking lifestyle changes after colorectal cancer: insights for program developmentCurr Oncol2013206493511
- DurkoLMalecka-PanasELifestyle Modifications and Colorectal CancerCurr Colorectal Cancer Rep201410455424659930
- GeogheganJGScheeleJTreatment of colorectal liver metastasesBr J Surg199986215816910100781
- McloughlinJMJensenEHMalafaMResection of colorectal liver metastases: current perspectivesCancer Control2006131324116508624
- PawlikTMScogginsCRZorziDEffect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastasesAnn Surg2005241571572415849507
- ChotiMASitzmannJVTiburiMFTrends in long-term survival following liver resection for hepatic colorectal metastasesAnn Surg2002235675976612035031
- ScheeleJStanglRAltendorf-HofmannAHepatic metastases from colorectal carcinoma: impact of surgical resection on the natural historyBr J Surg19907711124112462253003
- AbdallaEKVautheyJNEllisLMRecurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastasesAnn Surg2004239681882715166961
- FelibertiECWagmanLDRadiofrequency ablation of liver metastases from colorectal carcinomaCancer Control2006131485116508626
- NordlingerBQuilichiniMAParcRHepatic resection for colorectal liver metastases. Influence on survival of preoperative factors and surgery for recurrences in 80 patientsAnn Surg198720532562633827361
- BozzettiFDociRBignamiPMorabitoAGennariLPatterns of failure following surgical resection of colorectal cancer liver metastases. Rationale for a multimodal approachAnn Surg198720532642703827362
- de GramontAFigerASeymourMLeucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancerJ Clin Oncol200018162938294710944126
- TournigandCAndréTAchilleEFOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR studyJ Clin Oncol200422222923714657227
- SaltzLBCoxJVBlankeCIrinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study GroupN Engl J Med20003431390591411006366
- DouillardJYCunninghamDRothADIrinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trialLancet200035592091041104710744089
- EngCShalanNBiological agents versus chemotherapy in the treatment of colorectal cancerExpert Opin Pharmacother20067101251127116805714
- AzvolinskyAColorectal cancer: to stack or sequence therapy?J Natl Cancer Inst20151075djv138djv13825957442
- FolprechtGGruenbergerTBechsteinWSurvival of patients with initially unresectable colorectal liver metastases treated with FOLFOX/cetuximab or FOLFIRI/cetuximab in a multidisciplinary concept (CELIM study)Ann Oncol20142551018102524585720
- KhanAZMorris-StiffGMakuuchiMPatterns of chemotherapy-induced hepatic injury and their implications for patients undergoing liver resection for colorectal liver metastasesJ Hepatobiliary Pancreat Surg200916213714419093069
- ShiinaSTerataniTObiSNonsurgical treatment of hepatocellular carcinoma: from percutaneous ethanol injection therapy and per-cutaneous microwave coagulation therapy to radiofrequency ablationOncology200262Suppl 1646811868788
- OkadaSLocal ablation therapy for hepatocellular carcinomaSemin Liver Dis199919332332810518311
- BartolozziCLencioniREthanol injection for the treatment of hepatic tumoursEur Radiol1996656826968934135
- LeeMJMuellerPRDawsonSLPercutaneous ethanol injection for the treatment of hepatic tumors: indications, mechanism of action, technique, and efficacyAJR Am J Roentgenol199516412152207998542
- LivraghiTGoldbergSNLazzaroniSSmall hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injectionRadiology1999210365566110207464
- MinamiYKudoMRadiofrequency ablation of hepatocellular carcinoma: Current statusWorld J Radiol201021141721179308
- RhimHLimHKRadiofrequency ablation of hepatocellular carcinoma: pros and consGut Liver20104Suppl 1S11321103289
- GillamsARLeesWRFive-year survival in 309 patients with colorectal liver metastases treated with radiofrequency ablationEur Radiol20091951206121319137310
- GwakJHOhBYLeeRAChungSSKimKHClinical applications of radio-frequency ablation in liver metastasis of colorectal cancerJ Korean Soc Coloproctol201127420221980591
- van TilborgAAMeijerinkMRSietsesCLong-term results of radiofrequency ablation for unresectable colorectal liver metastases: a potentially curative interventionBr J Radiol201184100255656521159807
- JakobsTFHoffmannRTTrummCReiserMFHelmbergerTKRadio-frequency ablation of colorectal liver metastases: mid-term results in 68 patientsAnticancer Res2006261B67168016739337
- van DuijnhovenFHJansenMCJunggeburtJMFactors influencing the local failure rate of radiofrequency ablation of colorectal liver metastasesAnn Surg Oncol200613565165816538411
- BoameNGreshamGJonkerDUse of chemotherapy and radio-frequency ablation to treat colorectal cancer metastases: a retrospective review of The Ottawa Hospital Cancer Centre over 7 yearsCurr Oncol2014214557
- SolbiatiLAhmedMCovaLSmall liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-upRadiology2012265395896823091175
- WatanabeAYangCCheungWYECOG performance status as a predictor of adjuvant chemotherapy (AC) toxicities in stage III colorectal cancer (CRC) patientsJ Clin Oncol2017354 Suppl789789
- FernandezFGDrebinJALinehanDCDehdashtiFSiegelBAStrasbergSMFive-year survival after resection of hepatic metastases from colorectal cancer in patients screened by positron emission tomography with F-18 fluorodeoxyglucose (FDG-PET)Ann Surg2004240343845015319715
- SolbiatiLAhmedMCovaLIeraceTBrioschiMGoldbergSNSmall liver colorectal metastases treated with percutaneous radiofrequency ablation: local response rate and long-term survival with up to 10-year follow-upRadiology2012265395896823091175
- BoameNGreshamGJonkerDUse of chemotherapy and radio-frequency ablation to treat colorectal cancer metastases: a retrospective review of The Ottawa Hospital Cancer Centre over 7 yearsCurr Oncol2014214557
- BilchikAJWoodTFAllegraDCryosurgical ablation and radio-frequency ablation for unresectable hepatic malignant neoplasms: a proposed algorithmArch Surg2000135665766210843361
- MericFPattYZCurleySASurgery after downstaging of unresectable hepatic tumors with intra-arterial chemotherapyAnn Surg Oncol20007749049510947016
- McgahanJPBrockJMTeslukHGuWZSchneiderPBrowningPDHepatic ablation with use of radio-frequency electrocautery in the animal modelJ Vasc Interv Radiol1992322912971627876
- BuscariniESavoiaABrambillaGRadiofrequency thermal ablation of liver tumorsEur Radiol200515588489415754165
- KuvshinoffBWOtaDMRadiofrequency ablation of liver tumors: influence of technique and tumor sizeSurgery2002132460561212407343
- SolbiatiLLivraghiTGoldbergSNPercutaneous radio-frequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patientsRadiology2001221115916611568334
- OshowoAGillamsAHarrisonELeesWRTaylorIComparison of resection and radiofrequency ablation for treatment of solitary colorectal liver metastasesBr J Surg200390101240124314515293
- LivraghiTSolbiatiLMeloniFIeraceTGoldbergSNGazelleGSPercutaneous radiofrequency ablation of liver metastases in potential candidates for resection: the “test-of-time approach”Cancer200397123027303512784338
- AloiaTAVautheyJNLoyerEMSolitary colorectal liver metastasis: resection determines outcomeArch Surg2006141546046616702517
- LeblancFFonckMBrunetRBecouarnYMathoulin-PélissierSEvrardSComparison of hepatic recurrences after resection or intraoperative radiofrequency ablation indicated by size and topographical characteristics of the metastasesEur J Surg Oncol200834218519017998155
- KimKHYoonYSYuCSCsYComparative analysis of radiofrequency ablation and surgical resection for colorectal liver metastasesJ Korean Surg Soc20118112522066097
- HurHKoYTMinBSComparative study of resection and radiofrequency ablation in the treatment of solitary colorectal liver metastasesAm J Surg2009197672873618789428
- ZhaiZGuJInfluence of tumor size on the prognosis in patients with colon cancerZhonghua Wei Chang Wai Ke Za Zhi Chin J Gastrointest Surg201215495498
- ChenCHHsiehMCHsiaoPKLinEKLuYJWuSYA critical reappraisal for the value of tumor size as a prognostic variable in rectal adenocarcinomaJ Cancer20178101927193428819391
- van DuijnhovenFHJansenMCJunggeburtJMFactors influencing the local failure rate of radiofrequency ablation of colorectal liver metastasesAnn Surg Oncol200613565165816538411
- NordlingerBSorbyeHGlimeliusBPerioperative chemotherapy with FOLFOX4 and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC Intergroup trial 40983): a randomised controlled trialLancet200837196171007101618358928
- GillamsARLeesWRFive-year survival following radiofrequency ablation of small, solitary, hepatic colorectal metastasesJ Vasc Interv Radiol200819571271718440460
- MachiJOishiAJSumidaKLong-term outcome of radio-frequency ablation for unresectable liver metastases from colorectal cancer: evaluation of prognostic factors and effectiveness in first- and second-line managementCancer J200612431832616925977
- RuersTPuntCVan CoevordenFEORTC Gastro-Intestinal Tract Cancer Group, Arbeitsgruppe Lebermetastasen und-tumoren in der Chirurgischen Arbeitsgemeinschaft Onkologie (ALM-CAO) and the National Cancer Research Institute Colorectal Clinical Study Group (NCRI CCSG)Radiofrequency ablation combined with systemic treatment versus systemic treatment alone in patients with non-resectable colorectal liver metastases: a randomized EORTC Intergroup phase II study (EORTC 40004)Ann Oncol201223102619262622431703
- KnudsenARKannerupASMortensenFVNielsenDTRadiofrequency ablation of colorectal liver metastases downstaged by chemotherapyActa Radiol200950771672119488894
- GillamsARLeesWRSurvival after percutaneous, image-guided, thermal ablation of hepatic metastases from colorectal cancerDis Colon Rectum200043565666110826427
- AbdallaEKVautheyJNEllisLMRecurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastasesAnn Surg2004239681882715166961
- TricoliJVBlairDGAndersCKBiologic and clinical characteristics of adolescent and young adult cancers: Acute lymphoblastic leukemia, colorectal cancer, breast cancer, melanoma, and sarcomaCancer201612271017102826849082
- BleyerABarrRHayes-LattinBBiology and Clinical Trials Subgroups of the US National Cancer Institute Progress Review Group in Adolescent and Young Adult OncologyThe distinctive biology of cancer in adolescents and young adultsNat Rev Cancer20088428829818354417
- HubbardJMGrotheyAAdolescent and young adult colorectal cancerJ Natl Compr Canc Netw201311101219122524142823