Abstract
Background
The aspartate aminotransferase-to-platelet ratio index (APRI) has been correlated with clinical outcome in patients with hepatocellular carcinoma (HCC), but controversial results were obtained with previous studies. This study was aimed to evaluate the prognostic value of the APRI in patients with HCC.
Materials and methods
A literature survey was conducted by searching PubMed, Web of Science, Cochrane library, Embase, Wanfang, and National Knowledge Infrastructure for publications released prior to March 1, 2018. Pooled hazard ratios (HRs) with 95% CIs were calculated to assess the association between the APRI and HCC prognosis using Stata SE 12.0 software.
Results
Analysis was performed on a total of 15 articles that included 5,051 patients. The pooled results showed that APRI was significantly associated with overall survival for patients with HCC (HR =1.62, 95% CI: 1.23–2.01). Furthermore, HCC patients with higher APRI were at significantly greater risk of short recurrence-free survival (HR =1.83, 95% CI: 1.48–2.18) and poor disease-free survival (HR =1.46, 95% CI: 1.26–1.66).
Conclusions
APRI could serve as a promising and noninvasive marker for predicting HCC prognosis.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer and the third leading cause of cancer-related death globally.Citation1,Citation2 Despite great advances in early diagnosis and treatments, the prognosis, especially the long-term survival, remains dissatisfactory in patients with HCC.Citation3–Citation6 Additionally, the prognostic markers of HCC have not been completely elucidated. Established prognostic factors can contribute to predicting the survival and relapse for HCC patients as well as guiding their clinical management.
Recently, several serum markers that can be used as noninvasive tools have been identified in human cancers, including HCC.Citation7–Citation10 Among them, there has been great interest in the aspartate aminotransferase-to-platelet ratio index (APRI) because it is an inexpensive and feasible test that can be used for daily oncologic practice.
It has been reported that APRI might be a candidate as a prognostic biomarker in HCC.Citation11–Citation20 However, there were shortcomings in the current clinical studies because they were of limited sample sizes, and some results regarding the clinical value of APRI in HCC were inconsistent and debatable.Citation14,Citation21,Citation22 Therefore, we conducted this systematic review and meta-analysis based on all relevant studies for a better understanding of the relationship between APRI and prognosis of HCC patients.
Materials and methods
Search strategy and study selection
A comprehensive literature search was performed in several electronic databases to retrieve the eligible studies before March 1, 2018. The online databases included PubMed, Web of Science, Cochrane library, Embase, Wanfang, and National Knowledge Infrastructure. The combined key words and search terms were as follows: (aspartate aminotransferase-to-platelet ratio index OR aspartate aminotransferase/platelet count ratio index OR AST-to-platelet ratio index OR AST/PLT ratio index OR APRI) AND (liver cancer OR HCC OR hepatocellular carcinoma OR liver neoplasms OR hepatic tumor). We also manually reviewed the references in retrieved papers for potential studies.
Publications with full text that met the following criteria were considered to be eligible and were included in this meta-analysis: 1) studies concerned with the prognostic impact of APRI in primary HCC, 2) a definite cutoff value of APRI was given, 3) the hazard ratio (HR) with 95% CI for prognosis was available, and 4) patients with HCC were divided into two groups according to the APRI value.
Data extraction and quality assessment
The collected information from all studies included name of the first author, study country, year of publication, included time, sample size, number of male and female patients, age distribution, survival type, follow-up period, cutoff value for APRI, cutoff selection, treatment methods, tumor stage, HR, and the corresponding 95% CI. HRs and the corresponding 95% CIs were directly extracted from the original article if a study reported the HRs and 95% CIs in univariate and/or multivariate analysis. Otherwise, Engauge Digitizer software (version 4.1) was used to estimate the HR from the Kaplan–Meier curve.
All included studies were assessed by the Newcastle–Ottawa quality assessment scale (NOS). In this method, NOS scores ranged from 0 (lowest) to 9 (highest) points. A study with an NOS score ≥6 was considered to be of high quality.
Statistical analysis
In this meta-analysis, statistical analyses for pooled HRs were executed using Stata 12.0 software (Stata, College Station, TX, USA).
For measuring the heterogeneity among research studies, Cochran’s Q test and Higgins I-squared statistic were applied. A probability value of PQ <0.05 or I2 >50%indicated that heterogeneity existed. If heterogeneity was present, the random-effects model was used to calculate the integrated HRs. If there was no significant heterogeneity across studies, the fixed-effects model was adopted.
Funnel plot and Begg’s test were used to judge the potential publication bias. Sensitivity analysis was applied to evaluate the robustness of the pooled results. All P-values <0.05 were regarded as statistically significant.
Results
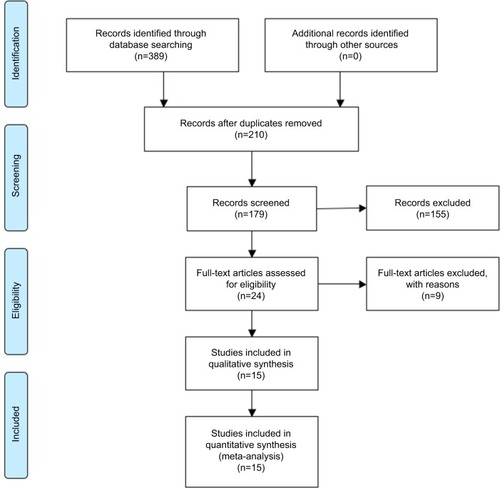
The detailed steps of the potential literature search are shown in . Based on the selection criteria for the eligible studies, high-quality articles (including 17 studies) written in English were identified in this meta-analysis.Citation11–Citation25 A total of 5,051 patients with HCC were enrolled. All included studies were retrospective and reported the relationship between the APRI value and HCC prognosis. The detailed characteristics of all included studies are summarized in .
Table 1 Main characteristics of all included studies
Relationship between APRI and overall survival in HCC
A total of 12 articles (including 14 studies) with 4,558 subjects reported the relationship between APRI and overall survival (OS) in patients with HCC. Considering the significant heterogeneity among these articles (I2=62.9%, PQ =0.001), a random-effects model was applied. As shown in , the overall results indicated that elevated APRI predicted a poor outcome for OS of HCC (HR =1.62, 95% CI: 1.23–2.01).
Figure 2 Forest plot for the relationship between APRI and OS.
Abbreviations: APRI, aminotransferase-to-platelet ratio index; HR, hazard ratio; OS, overall survival.
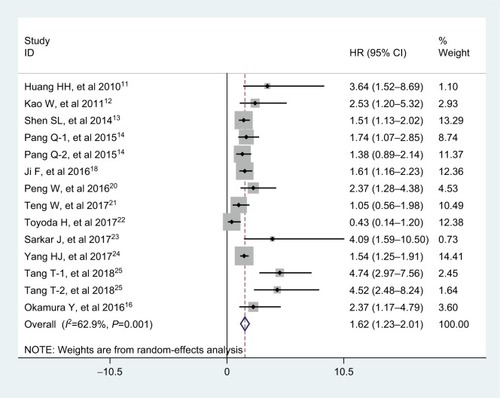
Exploratory subgroup analyses were performed according to analysis type (multivariate analysis and univariate analysis), cutoff value selection (receiver operating characteristic curve and Others), and treatments (With surgery, No surgery, and Mixed). shows that the calculated pooled HR values were significantly >1.0 in those subgroup analyses. Interestingly, the APRI could be an independent predictor of OS in patients with HCC (HR =1.41, 95% CI: 1.08–1.73, P<0.001).
Table 2 Results of subgroup analysis of pooled HRs of OS of HCC patients with high APRI
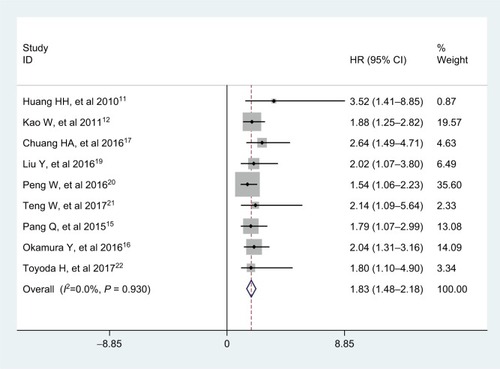
Nine studies with a total of 2,965 HCC patients reported the prognostic value of APRI for recurrence-free survival (RFS). No significant heterogeneity was observed among studies (I2=0.0%, PQ =0.930), and the fixed-effects model was adopted. The pooled HR was 1.83 (95% CI: 1.48–2.18, P<0.001; ), indicating that high APRI was an unfa-vorable factor for RFS in HCC. In addition, we found that the analysis types, cutoff value selections, and treatments did not affect the prognostic predictor of RFS in HCC patients from the subgroup analyses ().
Table 3 Results of subgroup analysis of pooled HRs of RFS of HCC patients with high APRI
Figure 3 Forest plot for the relationship between APRI and RFS.
Abbreviations: APRI, aminotransferase-to-platelet ratio index; HR, hazard ratio; RFS, recurrence-free survival.
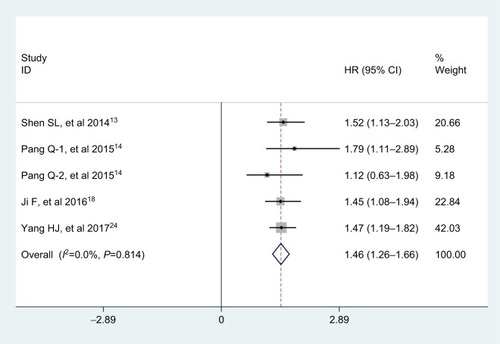
Five studies, consisting of 1,677 patients, explored the association between APRI and disease-free survival (DFS) in multivariate analysis. There was no obvious heterogeneity across studies (I2=0.0%, PQ =0.814), and therefore, the fixed-effects model was used. Analysis revealed the pooled HR of 1.46 with 95% CI: 1.26–1.66 (P<0.001), which showed that APRI was an independent predictive factor of DFS in patients with HCC ().
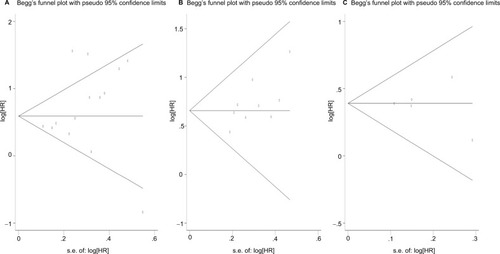
Publication bias
Funnel plot and Begg’s test both suggested no evidence of publication bias for OS, RFS, and DFS (Pr Begg’s test>|z|=0.228 for OS; Pr Begg’s test>|z|=0.118 for RFS; Pr Begg’s test>|z|=1.000 for DFS; ).
Figure 5 Funnel plots for publication bias test.
Note: (A) For OS; (B) for RFS; (C) for DFS.
Abbreviations: DFS, disease-free survival; HR, hazard ratio; OS, overall survival; RFS, recurrence-free survival.
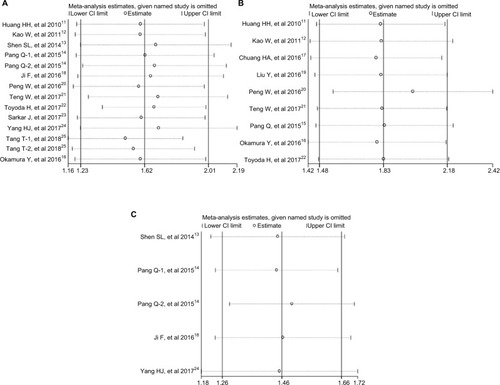
Sensitivity analysis
Sensitivity analysis was performed to assess the potential impact of each individual study on the overall results. The results showed that any single study had little influence on the pooled results (), thus indicating that our results were relatively stable and credible.
Figure 6 Sensitivity analysis of the relationship between APRI and HCC prognosis.
Note: (A) For OS; (B) for RFS; (C) for DFS.
Abbreviations: APRI, aspartate aminotransferase-to-platelet ratio index; DFS, disease-free survival; HCC, hepatocellular carcinoma; OS, overall survival; RFS, recurrence-free survival.
Discussion
As a noninvasive scoring marker, APRI consists of two routinely available clinical and laboratory variables, aspartate aminotransferase (AST) and platelets (PLT), and can be calculated using the following formula: (AST/the upper limit of normal value)×100: PLT (109/L).Citation26 It was firstly proposed as a simple, straightforward test to assess liver fibrosis stage and liver function reserve.Citation27–Citation29 In-depth studies determined that APRI also had potential prognostic value and could be used as a stable marker to predict the outcome of patients with HCC.Citation11–Citation13 It has been known that AST and PLT play an important role in tumor progression and are associated with prognosis in several human cancers, including HCC.Citation15,Citation30,Citation31 APRI is a combination of the above two predictors, and it is low in cost and more easily detectable. Its clinical predictive value could be enhanced due to its stability and reliability.
The exact mechanisms governing the prognostic values of APRI still remain unclear; however, there are some possible explanations.Citation24,Citation25 HCC patients with a high APRI value frequently have elevated AST levels, and the level of AST could represent the cirrhosis level or the injury to the hepa-tocytes, and could also reflect liver stress or damage arising from progressive liver fibrosis or reactivation of hepatitis virus replication. All of these are major contributors to liver carcinogenesis.Citation32–Citation34 In contrast, many patients with HCC and elevated APRI often have a low PLT level. Progressive destruction of an enlarged spleen and progressive liver fibrosis can often lead to low preoperative PLT,Citation35–Citation37 and there were also close relationships between low preoperative PLT and great risk of major liver-related complications.Citation37,Citation38 All of these factors and events are closely linked to poor clinical outcomes in HCC patients.
To the best of our knowledge, this is the first meta-analysis that comprehensively assesses the prognostic value of APRI in HCC. In the present meta-analysis, a total of 15 published articles with 5,051 HCC patients were collected. When the out comes from all available studies were combined and pooled, we found that an elevated APRI was significantly associated with poor OS (HR =1.62, 95% CI: 1.23–2.01) in HCC, although there was heterogeneity. Furthermore, the subgroup analyses revealed that APRI could be an independent prognostic factor of OS in patients with HCC. For the relationship between APRI and secondary endpoints, the combined results showed that APRI might act as a prognostic indicator for RFS in HCC (HR =1.83, 95% CI: 1.48–2.18), and the subgroup analyses also confirmed the prognostic value of APRI for RFS in HCC. Furthermore, HCC patients with high APRI had a worse DFS when compared with that of patients with low APRI (HR =1.46, 95% CI: 1.26–1.66). Thus, the APRI might represent a predictive biomarker with great clinical utility in HCC patients.
Nevertheless, there are some limitations existing in the meta-analysis that should be carefully interpreted. Firstly, all studies enrolled were retrospective, and the number of published studies included was not sufficiently large for a more detailed subgroup analysis. Secondly, because the majority of studies included were from Asian countries (China, Japan, and Korea), additional clinical studies from other countries are required. Thirdly, four of 14 studies for OS only reported HRs in the univariate analysis, which might cause a bias toward overestimation of the prognostic role of APRI. In addition, some heterogeneity was observed among studies for OS, which was probably due to factors such as the adjusted multivariate analysis of studies with different factors or different start time to follow-up or diverse therapies applied. In addition, there are some other factors that could influence AST and PLT, such as antiviral drugs and other accompanying diseases of the patients, and this should also be noted. Finally, the cutoff value for defining high or low APRI differed in studies, and it is essential that they be unified before APRI can be utilized in clinical prognostication for HCC.
In summary, the results of our study suggest that high APRI indicated poor prognosis in HCC patients, and APRI could serve as a cost-effective, significant biomarker for predicting HCC survival outcome. Considering the limitations mentioned above, larger well-designed clinical studies with more diverse populations are warranted in the future to validate our findings.
Disclosure
The authors report no conflicts of interest in this work.
References
- FornerALlovetJMBruixJHepatocellular carcinomaLancet201237998221245125522353262
- MaluccioMCoveyARecent progress in understanding, diagnosing, and treating hepatocellular carcinomaCA Cancer J Clin201262639439923070690
- TangAHallouchOChernyakVKamayaASirlinCBEpidemiology of hepatocellular carcinoma: target population for surveillance and diagnosisAbdom Radiol20184311325
- ZhangJLinHWangXYPredictive value of microRNA-143 in evaluating the prognosis of patients with hepatocellular carcinomaCancer Biomark201719325726228436387
- YangXPZhouLXYangQJDiagnostic and prognostic roles of serum vitronectin in hepatitis B-related hepatocellular carcinomaCancer Biomark201617327127927802203
- ChenCJGlobal elimination of viral hepatitis and hepatocellular carcinoma: opportunities and challengesGut201867459559829367206
- WangYAttarBMFuentesHEJaiswalPTafurAJEvaluation of the prognostic value of platelet to lymphocyte ratio in patients with hepa-tocellular carcinomaJ Gastrointest Oncol2017861065107129299368
- ZhaoTCuiLLiAThe significance of RDW in patients with hepatocellular carcinoma after radical resectionCancer Biomark201616450751227062565
- NishijimaTFMussHBShacharSSTamuraKTakamatsuYPrognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: A systematic review and meta-analysisCancer Treat Rev2015411097197826481060
- LinHJiaoXYuBClinical significance of serum 14-3-3 beta in patients with hepatocellular carcinomaCancer Biomark201720214315028869445
- HungHHSuCWLaiCRFibrosis and AST to platelet ratio index predict post-operative prognosis for solitary small hepatitis B-related hepatocellular carcinomaHepatol Int20104469169921286339
- KaoWYChiouYYHungHHRisk factors for long-term prognosis in hepatocellular carcinoma after radiofrequency ablation therapy: the clinical implication of aspartate aminotransferase-platelet ratio indexEur J Gastroenterol Hepatol201123652853621537128
- ShenSLFuSJChenBPreoperative aspartate aminotransfer-ase to platelet ratio is an independent prognostic factor for hepatitis B-induced hepatocellular carcinoma after hepatic resectionAnn Surg Oncol201421123802380924849520
- PangQZhangJYXuXSThe prognostic values of 12 cirrhosis-relative noninvasive models in patients with hepatocellular carcinomaScand J Clin Lab Invest2015751738425465804
- PangQZhangJYXuXSSignificance of platelet count and platelet-based models for hepatocellular carcinoma recurrenceWorld J Gastroenterol201521185607562125987786
- OkamuraYAshidaRYamamotoYThe FIB-4 index is a significant prognostic factor in patients with non-B non-C hepatocellular carcinoma after curative surgeryLangenbecks Arch Surg2016401219520326943655
- ChungHAKimJHHwangYNoninvasive fibrosis marker can predict recurrence of hepatocellular carcinoma after radiofrequency ablationSaudi J Gastroenterol2016221576326831608
- JiFLiangYFuSJA novel and accurate predictor of survival for patients with hepatocellular carcinoma after surgical resection: the neutrophil to lymphocyte ratio (NLR) combined with the aspartate amino-transferase/platelet count ratio index (APRI)BMC Cancer20161613726907597
- LiuYWangZXCaoYPreoperative inflammation-based markers predict early and late recurrence of hepatocellular carcinoma after curative hepatectomyHepatobiliary Pancreat Dis Int201615326627427298102
- PengWLiCWenTFPostoperative aspartate aminotransferase to platelet ratio index change predicts prognosis for hepatocellular carcinomaMedicine20169530e416027472685
- TengWHsiehYCLuiKWEradication of hepatitis C virus profoundly prolongs survival in hepatocellular carcinoma patients receiving transarterial chemoembolizationJ Viral Hepat201724121160116728643457
- ToyodaHKumadaTTadaTDifferences in the impact of prognostic factors for hepatocellular carcinoma over timeCancer Sci2017108122438244428945309
- SarkarJDeleonTWongLLMELD score and AST-to-platelet ratio index (APRI) predict long-term survival in patients with a small hepa-tocellular carcinoma following non-transplant therapies: a pilot studyHepatoma Res20173798529075672
- YangHJJiangJHYangYTStratified aspartate aminotransferase-to-platelet ratio index accurately predicts survival in hepatocellular carcinoma patients undergoing curative liver resectionTumour Biol2017393 1010428317695944
- TangTQiuJLLiGWAspartate aminotransferase-to-platelet ratio predicts response to transarterial chemoembolisation and prognosis in hepatocellular carcinoma patientsClin Radiol201873325926529032942
- WaiCTChengCLWeeANon-invasive models for predicting histology in patients with chronic hepatitis BLiver Int200626666667216842322
- BaranovaALalPBirerdincAYounossiZMNon-invasive markers for hepatic fibrosisBMC Gastroenterol2011119121849046
- ShaheenAAMyersRPDiagnostic accuracy of the aspartate amino-transferase-to-platelet ratio index for the prediction of hepatitis C-related fibrosis: a systematic reviewHepatology200746391292117705266
- ElsebaeMMAbu-ZekriNBA study of the effect of splenectomy on hepatic functional reserve and structural damage in patients with chronic hepatitis C virus infection by non-invasive serum markers. A prospective studyInt J Surg20086536236618662898
- ChenSLXueNWuMTInfluence of preoperative serum aspartate aminotransferase (AST) level on the prognosis of patients with non-small cell lung cancerInt J Mol Sci2016179 pii:E1474
- WanGGaoFChenJNomogram prediction of individual prognosis of patients with hepatocellular carcinomaBMC Cancer20171719128143427
- KamimotoYHoriuchiSTanaseSMorinoYPlasma clearance of intravenously injected aspartate aminotransferase isozymes: evidence for preferential uptake by sinusoidal liver cellsHepatology1985533673753997068
- KumadaTToyodaHKiriyamaSPredictive value of tumor markers for hepatocarcinogenesis in patients with hepatitis C virusJ Gastroenterol2011464e44
- KimHCNamCMJeeSHNormal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort studyBr Med J2004328744698315028636
- ToghillPJGreenSFergusonFPlatelet dynamics in chronic liver disease with special reference to the role of the spleenJ Clin Pathol1977304367371853132
- MccormickPAMurphyKMSplenomegaly, hypersplenism and coagulation abnormalities in liver diseaseBaillieres Best Pract Res Clin Gastroenterol20001461009103111139352
- TomimaruYEguchiHGotohKPlatelet count is more useful for predicting posthepatectomy liver failure at surgery for hepatocel-lular carcinoma than indocyanine green clearance testJ Surg Oncol2016113556556926751258
- MaithelSKKneuertzPJKoobyDAImportance of low preoperative platelet count in selecting patients for resection of hepa-tocellular carcinoma: a multi-institutional analysisJ Am Coll Surg20112124638648 discussion 648–65021463803