Abstract
Background
Some patients with low rectal cancer experience anorectal and urogenital dysfunctions after surgery, which can influence the long-term quality of life. In this study, we aimed to protect nerve function in such scenarios by performing intraoperative monitoring of pelvic autonomic nerves (IMPAN).
Patients and methods
We retrospectively investigated a series of 87 patients undergoing laparoscopic low anterior resection of rectal cancer. Nerve-sparing was evaluated both visually and electrophysiologically. IMPAN was performed by stimulating the pelvic autonomic nerves under processed electromyography of the internal anal sphincter. Urination, defecation, sexual function, and the quality of life were evaluated using validated and standardized questionnaires preoperatively and at follow-up, 12 months after surgery.
Results
Among a total of 87 patients (53 male and 34 female patients), IMPAN with simultaneous electromyography of the internal anal sphincter was performed in 58 (66.7%) patients. Bilateral positive IMPAN results for both measurements, indicating successfully confirmed pelvic autonomic nerve preservation, were obtained in 45 (51.7%) patients. No significant difference was found in terms of urogenital and anorectal functions between preoperative and postoperative patients with bilateral positive IMPAN (P>0.05). Compared to preoperative patients with IMPAN (unilateral) or without IMPAN, these patients exhibited higher International Prostate Symptom Score, a lower International Index of Erectile Function-5, and a lower Female Sexual Function Index score at 12 months postoperatively (P<0.05).
Conclusion
IMPAN is an appropriate method with which to laparoscopically protect nerve function.
Introduction
The surgical procedure used for total mesorectal excision and the implementation of multimodal treatment strategies have considerably improved the prognosis of patients with low rectal cancer. However, following low anterior resection (LAR), some patients are known to experience anorectal and urogenital dysfunctions, which can exert significant impact upon the long-term quality of life,Citation1–Citation3 regardless of whether open or laparoscopic LAR procedure was performed.Citation4 The dominant cause of such dysfunction appears to be injuries incurred by the pelvic autonomic nerves during the surgical procedure.Citation5 Therefore, it is very important to identify methods with which to protect the pelvic autonomic nerves during such procedures.
Poor nerve visualization and a lack of neuroanatomical knowledge will inevitably result in inadvertent nerve damage. Furthermore, the intraoperative identification of nerve structures can be difficult due to the complex neuroanatomy involved, as well as the involvement of numerous surgical and patient-related factors, such as a narrow or deep pelvic cavity, severe obesity, a history of pelvic surgery, and neoadjuvant chemoradiotherapy.Citation2–Citation4 In order to reduce the rate of dysfunction following this form of surgery, Kneist et al introduced nerve-sparing surgery via the intraoperative neuromonitoring of pelvic autonomic nerves.Citation6–Citation8 Throughout this new technique, intraoperative neuromonitoring was performed via the electrical stimulation of pelvic autonomic nerves with concomitant electromyography of the internal anal sphincter and cystomanometry. Notably, better outcomes of anorectal and urogenital functions were evident in patients undergoing surgery with intraoperative neuromonitoring compared to patients who did not experience this method.Citation9
Kneist et al were the first to demonstrate that laparoscopic intraoperative neuromonitoring is technically feasible.Citation10 Laparoscopy may allow optimal visualization of neural structures in the narrow and deep pelvic cavity due to a number of specialist characteristics, including angled view, illumination, and magnification. Nerve preservation was usually evaluated visually. Few surgeons protected nerve through electrophysiological technique. The aim of the present study was to assess the effect of intraoperative monitoring of pelvic autonomic nerves (IMPAN) on accurate evaluation of nerve-sparing during laparoscopic LAR of rectal cancer.
Patients and methods
Patients
We retrospectively investigated 87 patients (53 male and 34 female patients) who underwent laparoscopic LAR for primary rectal cancer in Huashan Hospital, Fudan University between January 2012 and May 2016. Of these 87 patients, 58 underwent surgery with IMPAN; the rest did not. Written informed consent was obtained from all patients. This study was approved by the Ethics Committee of Huashan Hospital affiliated to Fudan University, and was conducted in accordance with the Declaration of Helsinki. Total mesorectal excision was carried out by the same team of surgeons using a standardized procedure. In cases of poor anastomosis, we fitted a diverting stoma.
Outcome assessment
Urinary function, anorectal function, sexual function, and quality of life were assessed in rectal cancer patients who underwent laparoscopic LAR over a 12-month follow-up period (following stoma closure, patients were followed up for 6–9 months; and patients without a diverting stoma were followed up for 12 months). At the 12-month follow-up, stoma closure had failed in three patients with IMPAN (unilateral), five patients with IMPAN (bilateral), and six patients without IMPAN. These patients were eliminated from our analysis of anorectal function.
Urinary function
We ascertained the International Prostate Symptom Score ([IPSS], in which the total score ranges from 0 to 35 points) and the quality of life for urinary function (in which the total score ranges from 0 to 6 points) to assess urinary function for both male and female patients.Citation11 A higher score indicated more severe urinary dysfunction.
Sexual function
Assessment of sexual function differs according to gender. Male sexual function was evaluated using the International Index of Erectile Function-5 (IIEF-5) score (a five-item questionnaire in which total score ranges from 1 to 25 points).Citation12 A lower score indicated more severe erectile dysfunction. The Female Sexual Function Index (FSFI) has become a multidimensional self-reporting instrument for assessing sexual function in women and covers six domains: desire, subjective arousal, lubrication, orgasm, satisfaction, and pain. This is a 19-item questionnaire with a total score ranging from 2 to 36 points,Citation13 with a higher score indicating better sexual function.
Anorectal function
Anorectal function was determined by the Wexner score, the total score of which ranges from 0 to 20 points, with a score of >9 indicating anorectal dysfunction resulting in a diminished quality of life.Citation14
Electrophysiological assessment
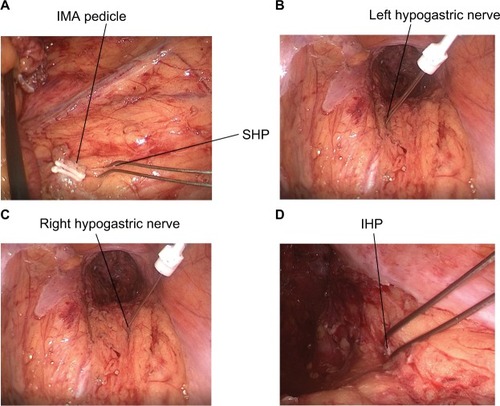
Neuromonitoring was performed with an electromyograph (DK-2740; Medtronic, Minneapolis, MN, USA). For electromyography, the needle electrode was placed into the internal anal sphincter, and a reference electrode was placed on the left thigh. As shown in , we developed a bipolar probe as the stimulating electrode. The stimulating electrode was placed into the abdominal cavity through the trocar. Any visualized pelvic autonomic nerves were directly stimulated after dissection of the lateral ligament of the rectum and Denonvilliers’ fascia (). The currents applied ranged from 5 to 10 mA, the frequency was 2 Hz, and stimulation lasted 5–20 seconds.
Figure 2 Pelvic autonomic nerves stimulated by a bipolar probe during surgery.
Note: (A) Intraoperative monitoring of SHP; (B) intraoperative monitoring of left hypogastric nerve; (C) intraoperative monitoring of right hypogastric nerve; and (D) intraoperative monitoring of right IHP.
Abbreviations: IHP, inferior hypogastric plexus; IMA, inferior mesenteric artery; SHP, superior hypogastric plexus.
Statistical analysis
For statistical evaluation, P-values <0.05 were considered statistically significant. The Wilcoxon’s signed-rank test was used to analyze paired random samples. All analyses were performed using SPSS 21.0 software (IBM Corporation, Armonk, NY, USA).
Results
Patient data
Out of the 87 patients (53 male and 34 female patients) included in this study, IMPAN with simultaneous electromyography of the internal anal sphincter was performed in 36 male patients and 22 female patients. Bilateral positive IMPAN results for both measurements indicating successfully confirmed pelvic autonomic nerve preservation were achieved in 45 patients (28 male and 17 female patients). In patients with IMPAN, if one side of the pelvic autonomic nerve can be successfully monitored and the other side failed, these patients belong to unilateral IMPAN group.
No significant differences were found in terms of the baseline characteristics of our patients. There were no major intraoperative or postoperative complications. None of the patients died as a result of the operation. Demographics, histopathological characteristics, and surgical data are sum-marized in .
Table 1 Characteristics of rectal cancer patients undergoing laparoscopic LAR with or without IMPAN
Urinary function
In 45 patients with bilateral positive stimulation responses, the mean IPSS total score was 6.58±3.19 preoperatively, and 6.76±3.11 at the 12-month follow-up. The mean preoperative IPSS score was 6.08±1.66 in 13 patients with a unilateral positive stimulation response, while the mean preoperative IPSS score was 6.28±2.53 in 29 patients without IMPAN. At the time of the 12-month follow-up, the IPSS score had increased significantly to 10.23±3.09 in patients with IMPAN (unilateral) and to 9.10±4.08 in patients without IMPAN (P<0.05). Assessment of the quality of life due to urinary symptoms in the 87 patients yielded a similar result for IPSS scores ().
Table 2 IPSS and quality of life due to urinary symptoms in patients with rectal cancer before surgery and at follow-up after LAR
Sexual function
Out of the 53 male patients, preoperative mean total IIEF-5 score was 18.29±4.27, 18.68±5.38, and 18.88±3.69 in the unilateral IMPAN group, bilateral IMPAN group, and none-IMPAN group, respectively. At the 12-month follow-up, 2 out of 28 patients with IMPAN (bilateral), three out of seven patients with IMPAN (unilateral), and five out of 18 patients without IMPAN had postoperative erectile dysfunction. The differences in the IIEF-5 scores between patients with IMPAN (unilateral) and without IMPAN were highly significant compared to patients with IMPAN (bilateral) (P<0.05). Similar results were observed in terms of FSFI scores among the three groups of female patients after surgery (six patients in the unilateral IMPAN group, 17 patients in the bilateral IMPAN group, and eleven patients in the none-IMPAN group). Impairment of female sexual function was significantly worse in patients with IMPAN (unilateral) and without IMPAN rather than in patients with IMPAN (bilateral) ( and ).
Table 3 IIEF-5 scores in male patients before and at follow-up after LAR from rectal cancer
Table 4 FSFI scores in female patients with rectal cancer prior to surgery and at follow-up after LAR
Anorectal function
Wexner score was evaluated in patients preoperatively and at the 12-month follow-up after LAR procedures. Three patients with IMPAN (unilateral), five patients with IMPAN (bilateral), and six patients without IMPAN failed to achieve stoma closure by the 12-month follow-up appointment. These patients were not evaluated for Wexner score. No significant difference was found in Wexner score when compared between preoperative and 12-month follow-up assessments, regardless of IMPAN (P>0.05) ().
Table 5 Wexner score in patients with rectal cancer before and at follow-up after LAR
Discussion
Total mesorectal excision is a standard technique for the treatment of rectal cancer and was first described in 1982 by Heald et al.Citation15 During this procedure, sharp dissection, a negative circumferential resection margin, and pelvic autonomic nerve preservation are required to ensure radical resection and reduce postoperative anorectal and urogenital dysfunctions.
Over the past decade, various intraoperative pelvic neuromonitoring methods, aimed at identifying and preserving pelvic autonomic nerves, have been developed and introduced to exenterative pelvic surgery.Citation16 The anatomy of the pelvis is highly complex, particularly with respect to the autonomic nervous system and its interindividual variations.Citation17–Citation20 It is anticipated that pelvic nerve injury may occur at different sites, with different functional consequences.Citation21,Citation22 First, during ligation of the inferior mesenteric artery pedicle, unsuitable lymph node dissection at the root of the inferior mesenteric artery may increase the possibility of superior hypogastric plexus injury. Second, during initial posterior rectal dissection, when separating the parietal (presacral) and the visceral (perirectal) pelvic fascia at the level of the sacral promontory, it is possible to injure the hypogastric nerves due to working in the wrong anatomic plane; the magnification of laparoscopy, and vaporization from the ultrasonic knife, can help us to identify the posterior plane. Third, during anterolateral rectal dissection close to the lateral ligaments, inferior hypogastric plexus should be protected. Finally, during anterior rectal dissection at the lateral edge of Denonvilliers’ fascia, the three-dimensional structural integrity of the prerenal presacral fascia and Denonvilliers’ fascia need be maintained in order to maintain the integrity of the mesorectum. Urogenital neurovascular bundles which are close to Denonvilliers’ fascia are vulnerable to injury.
Due to its angled view and magnification, the surgical field in laparoscopic operations is clearer than in open surgeries. Laparoscopic procedures could, therefore, provide improved views and enable a more selective approach for repetitive electric stimulations of different sites compared to open surgery. In this study, we demonstrated that IMPAN was a more appropriate method for the reliable quality assurance of laparoscopic nerve-sparing during LAR for rectal cancer.
When compared preoperatively and at 12-month follow-up, the differences in IPSS score, quality of life, IIEF-5 score, and FSFI score among patients with IMPAN (bilateral), with IMPAN (unilateral), and without IMPAN, respectively, were highly significant. These results suggested that IMPAN could become a predictor of urinary and sexual dysfunctions in patients undergoing laparoscopic LAR surgery. In patients without IMPAN, pelvic autonomic nerve preservation was assessed visually by the surgeon. Since the pelvic autonomic nerve was not damaged in some patients without IMPAN, the advantages of IMPAN may be greater than this result shows. Kneist et al reported similar improvements in urogenital and anorectal functions in patients undergoing surgery with monitoring of the autonomic pelvic nerves during laparoscopic LAR compared to patients who did not.Citation10
In our study, three out of seven patients with IMPAN (unilateral) had positive erectile dysfunction compared to five out of 18 patients without IMPAN. Erectile dysfunction in the two patients with bilateral nerve-sparing may have been associated with adjuvant radiochemotherapy and severe reactive depression subsequent to surgery. Our findings suggested that bilateral nerve-sparing is an essential prerequisite for maintaining male erectile function, which is in accordance with previous studies of erectile function following nerve-sparing radical surgery for rectal cancer.Citation23,Citation24 We should also acknowledge study limitations, including possible selection bias. IMPAN can be performed in selected patients with no radiotherapy, no edema, female patients with large pelvis, thin patients, tumor size is small, no invasion of serosa, etc. On the contrary, IMPAN will not be performed in selected patients with pelvic autonomic nerves that are not easily exposed. Owing to the difficulty of nerve exposure, nerve is very easily damaged. Even performing IMPAN can lead to unilateral or bilateral nerve monitoring failure.
It is remarkable that no significant difference was found in Wexner score between the preoperative and 12-month follow-up assessments in patients receiving IMPAN and those who did not. As the P-values in unilateral IMPAN group and without IMPAN group are quite low, type I error may be smaller and type II error may be greater in Wexner scores. But if we increase the sample size, we can reduce type I and type II errors at the same time. The sample size of our study, however, was small; our next step will be to recruit more patients to participate in our research. Most patients came to our hospital because of bloody stools and anorectal disorders, while others were preoperative patients with locally advanced stages who already had anorectal dysfunction. We plan to use anorectal manometry as an objective indicator with which to evaluate anorectal function. We also aim to increase the frequency and duration of postoperative follow-up.
In addition, neoadjuvant chemoradiotherapy may affect the anorectal and urogenital functions of patients for a long time. In a recent retrospective study of 263 rectal cancer patients, it was demonstrated, after a median follow-up of 51 months, that fecal incontinence occurs more frequently in irradiated patients with a trend toward worse sexual function.Citation25 A further study reported the negative long-term effect of preoperative radiation on anorectal function with a mean follow-up of 14 years.Citation26 Similar results were found in the Dutch Total Mesorectal Excision Trial in which Lange et al evaluated anorectal and sexual functions preoperatively and at several time points up to 5 years after surgery; results showed that anorectal and sexual functions worsened significantly over time in the irradiated patients.Citation5,Citation27
Conclusion
IMPAN may be of substantial value, because it provides the surgeon with direct feedback as to whether the plane of dissection is close to the pelvic autonomic nerves. Our retrospective study demonstrated that IMPAN is an appropriate and reliable method with which to assure laparoscopic nerve-sparing. However, up until now, there have been no published data from prospective randomized studies which compare the functional outcome after LAR for rectal cancer with and without IMPAN. Prospective randomized multicenter trials remain important for better demonstration of the efficacy, accuracy, and safety of IMPAN.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
This study was supported by a grant from the Medical Guidance Program of Shanghai Science and Technology Committee (No. 134119a1400).
Disclosure
The authors report no conflicts of interest in this work.
References
- WallnerCLangeMMBonsingBACauses of fecal and urinary incontinence after total mesorectal excision for rectal cancer based on cadaveric surgery: a study from the Cooperative Clinical Investigators of the Dutch total mesorectal excision trialJ Clin Oncol200826274466447218802159
- LangeMMvan de VeldeCJUrinary and sexual dysfunction after rectal cancer treatmentNat Rev Urol201181515721135876
- EmmertsenKJLaurbergSRectal Cancer Function Study GroupImpact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancerBr J Surg2013100101377138723939851
- AnderssonJAbisGGellerstedtMPatient-reported genitourinary dysfunction after laparoscopic and open rectal cancer surgery in a randomized trial (COLOR II)Br J Surg2014101101272127924924798
- LangeMMden DulkMBossemaERRisk factors for faecal incontinence after rectal cancer treatmentBr J Surg200794101278128417579345
- KauffDWKochKPSomerlikKHHoffmannKPLangHKneistWEvaluation of two-dimensional intraoperative neuromonitoring for predicting urinary and anorectal function after rectal cancer surgeryInt J Colorectal Dis201328565966423440364
- KneistWKauffDWJuhreVHoffmannKPLangHIs intraoperative neuromonitoring associated with better functional outcome in patients undergoing open TME? Results of a case-control studyEur J Surg Oncol201339999499923810330
- KneistWKauffDWRubenwolfPThomasCHampelCLangHIntraoperative monitoring of bladder and internal anal sphincter innervation: a predictor of erectile function following low anterior rectal resection for rectal cancer? Results of a prospective clinical studyDig Surg2013304–645946524481247
- FangJFWeiBZhengZHEffect of intra-operative autonomic nerve stimulation on pelvic nerve preservation during radical laparoscopic proctectomyColorectal Dis20151712O268O27626362914
- KneistWKauffDWLangHLaparoscopic neuromapping in pelvic surgery: scopes of applicationSurg Innov201421221322023892318
- MadersbacherSPychaAKlinglerCHSchatzlGMarbergerMThe international prostate symptom score in both sexes: a urodynamics-based comparisonNeurourol Urodyn199918317318210338437
- RosenRCCappelleriJCSmithMDLipskyJPeñaBMDevelopment and evaluation of an abridged, 5-item version of the International Index of Erectile Function (IIEF-5) as a diagnostic tool for erectile dysfunctionInt J Impot Res199911631932610637462
- RosenRBrownCHeimanJThe Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual functionJ Sex Marital Ther200026219120810782451
- RothbarthJBemelmanWAMeijerinkWJHJWhat is the impact of fecal incontinence on quality of life?Dis Colon Rectum2001441677111805565
- HealdRJHusbandEMRyallRDThe mesorectum in rectal cancer surgery–the clue to pelvic recurrence?Br J Surg198269106136166751457
- SkinnerSAPelvic autonomic neuromonitoring: present reality, future prospectsJ Clin Neurophysiol201431430231225083841
- HavengaKDeRuiterMCEnkerWEWelvaartKAnatomical basis of autonomic nerve-preserving total mesorectal excision for rectal cancerBr J Surg19968333843888665201
- LindseyIGuyRJWarrenBFMortensenNJAnatomy of Denonvilliers’ fascia and pelvic nerves, impotence, and implications for the colorectal surgeonBr J Surg200087101288129911044153
- ClausenNWolloscheckTKonerdingMAHow to optimize autonomic nerve preservation in total mesorectal excision: clinical topography and morphology of pelvic nerves and fasciaeWorld J Surg20083281768177518521663
- MoszkowiczDAlsaidBBessedeTWhere does pelvic nerve injury occur during rectal surgery for cancer?Colorectal Dis201113121326133420718836
- KneistWRinkADKauffDWKonerdingMALangHTopography of the extrinsic internal anal sphincter nerve supply during laparoscopic-assisted TAMIS TME: five key zones of risk from the surgeons’ viewInt J Colorectal Dis2015301717825310925
- ScheerASO’ConnorAMChanBPThe myth of informed consent in rectal cancer surgery: what do patients retain?Dis Colon Rectum201255997097522874604
- CelentanoVFabbrocileGLuglioGAntonelliGTarquiniRBucciLProspective study of sexual dysfunction in men with rectal cancer: feasibility and results of nerve sparing surgeryInt J Colorectal Dis201025121441144520582547
- KyoKSameshimaSTakahashiMFurugoriTSawadaTImpact of autonomic nerve preservation and lateral node dissection on male urogenital function after total mesorectal excision for lower rectal cancerWorld J Surg20063061014101916736330
- ContinPKuluYBrucknerTComparative analysis of late functional outcome following preoperative radiation therapy or chemoradiotherapy and surgery or surgery alone in rectal cancerInt J Colorectal Dis201429216517524136155
- PollackJHolmTCedermarkBHolmströmBMellgrenALong-term effect of preoperative radiation therapy on anorectal functionDis Colon Rectum200649334535216532369
- LangeMMMarijnenCAMaasCPRisk factors for sexual dysfunction after rectal cancer treatmentEur J Cancer20094591578158819147343