Abstract
More attention has been paid to the axillary management over the past 50 years, and clinical practice has been changed as results of the random controlled trials. The American College of Surgeons Oncology Group Z0011 and International Breast Cancer Study Group (IBCSG) 23-01 trials provided high-level evidence to support the omission of axillary lymph nodes dissection (ALND) in sentinel lymph node (SLN)-positive patients receiving breast-conserving surgery (BCS) and adjuvant systemic treatment. In patients treated with BCS, whole breast irradiation (WBI) with tangential fields could lead to substantial axillary irradiation and control the residual tumor burden in axilla, whereas (intraoperative) partial breast irradiation has no therapeutic effect on these residual axillary metastases. In the observation group of the IBCSG 23-01 trial, 425 patients received BCS and 80 (18.8%) of them just underwent intra-operative radiotherapy. While the 10-year axillary recurrence rate was acceptable low (1.7%, 8/467) in the no ALND group, it was 4.5% (6/134) in patients without axillary management, which was significantly higher than that of 0.6% (2/333) in patients with axillary management (P=0.0024). Should we accept an axillary recurrence rate as high as 4.5% in patients with only SLNs micrometastases? What is the best way to control the residual tumor burden in the axilla and decrease the recurrence rate if there is no ALND? The evidence showed that both WBI after BCS (Z0011, AATRM [Agència d’Avaluació de Tecnologia i Recerca Mèdiques]) and axillary regional nodal irradiation after mastectomy/BCS OTOASOR (Optimal Treatment Of the Axilla - Surgery Or Radiotherapy), AMAROS (After Mapping of the Axilla: Radiotherapy Or Surgery) could control the regional residual tumor burden when the SLN is positive and an ALND is omitted. In the modern era, systemic therapy could further decrease the risk of local/regional recurrences. After the subanalysis of the POSNOC (POsitive Sentinel NOde: adjuvant therapy alone versus adjuvant therapy plus Clearance or axillary radiotherapy), SERC (Sentinelle Envahiet Randomisation du Curage), and Dutch BOOG (BOrstkanker Onderzoek Groep) trials, a prediction model might be established to identify those patients who could beneft from no axillary management as a guide to clinical practice. At present, axillary management should still be required for patients with SLN micrometastases.
The 10-year results of American College of Surgeons Oncology Group Z0011 trial showed that cT1-2N0 breast cancer with one to two positive sentinel lymph nodes (SLNs) undergoing breast-conserving surgery (BCS) and whole breast irradiation (WBI) could omit axillary lymph nodes dissection (ALND), which provided evidence to change the clinical practice.Citation1 In the post-Z0011 era, Galimberti et al presented the 10-year outcomes of the International Breast Cancer Study Group (IBCSG) 23-01 trial, which provided additional evidence to support ALND omission in patients with one or more micrometastatic (≤2 mm) SLNs, tumor size ≤5 cm, and receiving BCS and adjuvant systemic therapy.Citation2 These two clinical trials provided high-level evidence to support changes of National Comprehensive Cancer Network Guidelines since 2017Citation3 and resulted in the “standard of care” practice in the surgical management of the axillary lymph nodes by breast surgeon.Citation4 An important difference in the study design and conclusion between Z0011 and IBCSG 23-01 trials is the application of radiotherapy, in which Z0011 required that WBI should be followed by BCS but IBCSG 23-01 did not. WBI has an important effect on the axillary control in patients with positive SLNs who underwent BCS without ALND.
Although 27.3% of patients had metastatic non-SLNs in the Z0011 trial, which means a similar percentage of patients had metastatic nodes that were not surgically excided in the SNL biopsy (SLNB) alone group, the port design of WBI with tangential fields could led to substantial axillary irradiation and control the residual tumor burden in axilla.Citation1 The radiation field of Z0011 trial showed that some patients received high tangential irradiation fields, which means more prescribed dose delivered to lymph nodes ().Citation5,Citation6 However, (intraoperative) partial breast irradiation alone used in 27% of patients in the IBCSG 23-01 trial could not have made any therapeutic effect on the residual axillary metastases.Citation7 In the observation group (ie, those with ALND omission) of IBCSG 23-01, 425 patients received BCS in which 80 (18.8%) just underwent intraoperative radiotherapy (ie, single-dose intraoperative radiotherapy with electrons in breast).Citation2 After a 10-year follow-up, 5 of these 80 patients (6.3%) with intraoperative partial breast irradiation alone had an ipsilateral axillary recurrence,Citation2,Citation7 which is totally different from that of the Z0011 trial, which had only five (0.9%) axillary relapse in the SLNB + WBI group with 10-year follow-up. In the group of ALND omission, there were 12 cases without radiotherapy in patients with BCS, 42 cases without ALND in patients with mastectomy, but 333 cases receiving axillary treatment (WBI). The total axillary recurrence rate was 1.7% (8/467), which is still acceptable low, but the axillary recurrence rate was 4.5% (6/134) in patients without axillary management, which was significantly higher than that of 0.6% (2/333) in patients with axillary management (P=0.0024). Should we accept an axillary recurrence rate as high as 4.5% in patients with only SLNs micrometastases?
Table 1 Comparison of the average dose delivered to levels I–III in the standard and the high tangential irradiation fields
The residual tumor burden in the axilla is a serious risk factor to lead axillary failure, and more attention should be paid. Patients with SLN micrometastases might have a low axillary disease burden, but it does not mean there is no additional axillary node involvement. In Z0011 trial, 10% of patients with SLN micrometastases were found to have macrometastases in the non-SLNs after ALND.Citation1 In the AATRM (Agència d’Avaluació de Tecnologia i Recerca Mèdiques) 048/13/2000 trial, 13% (15/112) of patients with SLN micrometastases identified additional positive node after ALND.Citation8 Also, 13% of patients identified additional involved axillary lymph nodes after ALND in this IBCSG 23-01 study.Citation2 What is the best way to control the residual tumor burden in the axilla if there is no ALND? The evidence from clinical trials showed that both WBI after BCS (Z0011Citation1, AATRMCitation8) and axillary regional nodal irradiation (RNI) after mastectomy/BCS OTOASOR (Optimal Treatment Of the Axilla - Surgery Or Radiotherapy),Citation9 AMAROS (After Mapping of the Axilla: Radiotherapy Or Surgery)Citation10 could control the regional residual tumor burden when the SLN is positive and an ALND is omitted.
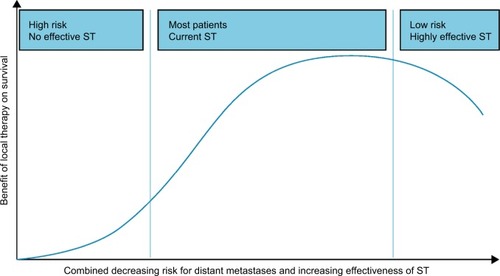
Systemic therapy will decrease the risk of local/regional recurrences and distant metastasis in the era of molecular subtype-guided adjuvant system therapy ().Citation11 However, with optimized systemic therapy guided by molecular subtypes, all patients with SLN micrometastases may not need ALND or axilla RNI. Currently, there are three ongoing clinical trials aiming to evaluate whether axilla management could be omitted in patients receiving modern-era therapy. The POSNOC (POsitive Sentinel NOde: adjuvant therapy alone versus adjuvant therapy plus Clearance or axillary radiotherapy) trial (NCT 02401685) will assess whether systemic therapy alone is noninferiority to systemic therapy plus axillary treatment (dissection or irradiation) to control the residual tumor burden in early stage breast cancer with one or two SLN macrometastases.Citation12 The SERC (Sentinelle Envahiet Randomisation du Curage) trial will randomly assign to observation only or ALND with positive SLN and demonstrate the noninferiority of ALND omission vs ALND.Citation13 The Dutch BOOG (BOrstkanker Onderzoek Groep) 2013-07 trial (NCT 02112682) will investigate whether completion axillary treatment can be safely omitted in SLN-positive breast cancer patients treated with mastectomy.Citation14 After the subanalysis of these trials, a prediction model might be established to identify the patients who can benefit from no axilla management as a guide to clinical practice. In our opinion, axillary management should still be required at the present time for patients with SLN micrometastases, ie, either WBI after BCS and axillary RNI or surgical dissection after mastectomy.
Figure 1 Combined hypothetical benefit of local tumor control on survival with increasing effectiveness of systemic therapy (ST) and decreasing risk of distant metastases of the primary tumor.
Notes: Patients in the left part of the slope have high-risk disease without effective systemic therapy and are not expected to benefit from improving locoregional treatments. For patients in the right part of the slope, treatment deintensification (surgery, radiation, or systemic therapy) might be appropriate. The middle group will represent most past and current patients with breast cancer, for whom an optimum multidisciplinary approach results in the greatest benefit.
Author contributions
All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Acknowledgments
We thank Xiao-Shan Cao, Chun-Jian Wang, Tong Zhao, Yan-Bing Liu, Peng Chen, Zhao-Peng Zhang, Xiao Sun, and Peng-Fei Qiu from our Breast Cancer Center. All eight of these individuals contributed to manuscript review; none received compensation for their contributions. We thank Charles M Balch from MD Anderson Cancer Center and the emeritus Editor-in-Chief of the Annals of Surgical Oncology, who contributed to revise the language of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
- GiulianoAEBallmanKVMcCallLEffect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trialJAMA20173181091892628898379
- GalimbertiVColeBFVialeGAxillary dissection versus no axillary dissection in patients with breast cancer and sentinel-node micrometastases (IBCSG 23-01): 10-year follow-up of a randomised, controlled phase 3 trialLancet Oncol201819101385139330196031
- GradisharWJAndersonBOBalassanianRNCCN guidelines insights: breast cancer, version 1.2017J Natl Compr Canc Netw201715443345128404755
- MorrowMManagement of the node-positive axilla in breast cancer in 2017: selecting the right optionJAMA Oncol20184225025129242929
- JagsiRChadhaMMoniJRadiation field design in the ACOSOG Z0011 (Alliance) trialJ Clin Oncol201432323600360625135994
- ReznikJCicchettiMGDegaspeBFitzgeraldTJAnalysis of axillary coverage during tangential radiation therapy to the breastInt J Radiat Oncol Biol Phys200561116316815629607
- GalimbertiVColeBFZurridaSAxillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trialLancet Oncol201314429730523491275
- SoláMAlberroJAFraileMComplete axillary lymph node dissection versus clinical follow-up in breast cancer patients with sentinel node micrometastasis: final results from the multicenter clinical trial AATRM 048/13/2000Ann Surg Oncol201320112012722956062
- SávoltÁPéleyGPolgárCEight-year follow up result of the OTOASOR trial: the optimal treatment of the axilla – surgery or radiotherapy after positive sentinel lymph node biopsy in early-stage breast cancer: a randomized, single centre, phase III, non-inferiority trialEur J Surg Oncol201743467267928139362
- RutgersERadiotherapy or surgery of the axilla after a positive sentinel node in breast cancer patients: 10-year results of the EORTC AMA-ROS trialProceedings from the 2018 San Antonio Breast Cancer SymposiumDecember 4–8San Antonio, Texas
- PoortmansPPostmastectomy radiation in breast cancer with one to three involved lymph nodes: ending the debateLancet201438399352104210624656686
- GoyalADodwellDPOSNOC: a randomised trial looking at axillary treatment in women with one or two sentinel nodes with macrometastasesClin Oncol20152712692695
- HouvenaeghelGResbeutMBoherJMGanglion sentinelle envahi: fautil faire le curage ou pas? Essai randomisé SERC [Sentinel node invasion: is it necessary to perform axillary lymph node dissection? Randomized trial SERC]Bull Canc2014101358363 French
- van RoozendaalLMde WiltJHvan DalenTThe value of completion axillary treatment in sentinel node positive breast cancer patients undergoing a mastectomy: a Dutch randomized controlled multicentre trial (BOOG 2013-07)BMC Canc201515610
