Abstract
Background
There have been no reliable scientific studies examining whether the interval between induction chemotherapy (IC) and initiating radiotherapy is associated with poor outcomes of nasopharyngeal carcinoma (NPC).
Patients and methods
In this retrospective study, we included a total of 239 local advanced NPC patients who underwent concurrent chemoradiotherapy and IC. Based on the interval between IC and intensity-modulated radiation therapy (IMRT), the patients were classified into three groups as follows: Group A (≤7 vs >7 days), Group B (≤14 vs >14 days), and Group C (≤ 21 vs >21 days). Univariate and multivariate regression analyses were performed to determine the prognostic factors of survival outcomes. The differences between the two groups were compared by the log-rank test.
Results
The median IC-IMRT interval was 9 days (range, 1–76 days). The median follow-up time was 40 months (range, 4–58 months). The IC-IMRT interval including Group A, Group B, and Group C was not significantly associated with overall survival (OS), distant metastasis-free survival (DMFS), locoregional relapse-free survival (LRFS), or disease-free survival (DFS). Multivariate analysis showed that the tumor stage was the independent significant predictor for OS, DMFS, LRFS, and DFS. But it appears that there was a trend toward improvement in the outcome of ≤7 days group in OS from the Kaplan–Meier curves.
Conclusion
It is also feasible to postpone radiotherapy for 1–3 weeks if patients were unable to receive treatment immediately due to chemotherapy complications such as bone marrow suppression. However, we suggest that patients should start IMRT as soon as possible after IC.
Introduction
Nasopharyngeal carcinoma (NPC) is the most common head and neck cancer in Southeast Asia. Citation1 Radiotherapy is the main treatment modality for NPC. With the advancement of imaging technology, the emergence of intensity-modulated radiation therapy (IMRT), and the application of concurrent chemotherapy in patients with advanced diseases, the survival rate of NPC patients has been significantly improved. Citation2
Numerous research studies have revealed that induction chemotherapy (IC) followed by concurrent chemoradiotherapy was relatively safe and could achieve a better survival than concurrent chemoradiotherapy in NPC patients by reducing the risk of death, tumor progression, and distant metastasis. Citation3–Citation5 The study of Phase III trial by Sun et al showed that the combination of radiotherapy and chemotherapy with IC in locally advanced NPC with high-risk T3-4N1/TxN2-3M0 can significantly improve the overall survival (OS), failure-free survival, and distant failure-free survival rate. Citation6
Some oncologists try to give radiation therapy as soon as clinically possible after the IC, whereas others delay the use of radiation with an interval of 3 weeks after chemotherapy. However, patients occasionally face a delay in starting their radiotherapy due to many factors including comorbid medical diseases, chemotherapy complications, and availability of radiation facilities. In less developed areas such as Hainan Province with a rather high incidence of NPC and limited resources in many settings (such as a shortage of radiation oncologists and/or equipment), a delay in starting radiotherapy is a major public health problem.
Various studies have proposed that the interval time (IT) from surgery to adjuvant therapy (radiation or chemotherapy) can have an impact in many types of cancers such as breast, colorectal, endometrial, head and neck cancers, and glioblastoma. Citation7–Citation11
To date, there have been no reliable scientific studies examining whether the IT from IC to radiotherapy can be associated with poor survival outcomes of NPC. Neither has the optimal time from IC to initiating radiotherapy been examined. Thus, to address these research gaps, we performed a retrospective analysis to evaluate the effect of IT from IC to radiotherapy on oncological outcomes in patients with NPC. In this study, we define “interval time” as the time between the end of chemotherapy and the beginning of radiotherapy.
Patients and methods
Patients
We retrospectively analyzed the medical data of patients with NPC who underwent IMRT and IC between December 2013 and November 2015 at the Hainan General Hospital, Haikou, China. Patients were eligible for inclusion in this study if:
the patients had stage III–IVb NPC;
the patients had not received radiotherapy or chemotherapy before;
IMRT was administered to the nasopharynx at a prescription dose of 68–72 Gy in 30–33 fractions;
they finished radiotherapy on time;
they underwent no adjuvant chemotherapy followed by IMRT;
they had complete clinicopathological and follow-up data.
We ensured that all patients’ information is anonymous before starting analysis. Two-hundred thirty-nine NPC patients were included in this study. All patients were staged according to the seventh edition of the International Union against Cancer Control/American Joint Committee on Cancer staging system. All patients provided informed consent before treatment. All patients underwent a complete pre-treatment evaluation, including medical history, physical examination, hematology and biochemistry, fiber optic nasopharyngeal biopsy, nasopharyngeal and cervical magnetic resonance imaging, chest X-ray, abdominal ultrasound, and Technetium-99m-methylene diphosphonate whole body bone scan.
Treatment
All patients were treated by definitive IMRT plus concurrent chemotherapy with IC. All patients were treated with IMRT and fixed with a custom head-to-neck thermoplastic cast, with the neck resting on the stent. High-resolution CT scan was performed at 2 cm (slicing thickness 3 mm) below the sternoclavicular joint. Target volume was delineated slice-by-slice on CT scan of treatment plan.
The prescribed doses were 68–72 Gy in 30–33 fractions to planning target volume (PTV) of primary gross tumor volume (GTV), 60–62 Gy to PTV of high-risk clinical target volume (CTV1), 64–70 Gy to PTV of GTV of involved lymph nodes (GTVnd), and 54–56 Gy to PTV of low-risk clinical target volume (CTV2).
All patients were delivered with the concurrent chemoradiation regimen every 3 weeks during radiotherapy. IC consisted of docetaxel plus cisplatin (or nedaplatin) or cisplatin (or nedaplatin) plus fluorouracil and concurrent chemoradiation consisted of platinum-based single or two drugs given every 3 weeks for one to three cycles during radiotherapy. The patients received IC plus concurrent chemotherapy for at least three cycles.
Follow-up
All patients were followed at regular intervals by our department after radiotherapy. These follow-ups were every 3 months during the first 2 years, every 6 months for the next 3 years, and annually thereafter. The primary end points were OS, locoregional relapse-free survival (LRFS), disease-free survival (DFS), and distant metastasis-free survival (DMFS). All intervals were calculated from the date of the beginning of therapy.
Statistical analyses
χ2 test was used to assess the distribution and clinical characteristics of selected demographic variables. The survival curves of OS and DFS were calculated by the Kaplan–Meier method, and the differences between the two groups were compared by the log-rank test. Univariate Cox regression analysis was used to explore the risk factors of survival outcome. Using the Cox proportional hazard model, multivariate analysis of each prognostic variable was analyzed by the backward stepwise (likelihood ratio) procedure. The statistical significance was P<0.05. All analyses were conducted in the 22.0 edition of IBM SPSS statistics.
Ethics statement
This retrospective study was approved by the ethics committee of the Hainan General Hospital, Haikou, China. Patient consent to review their medical records was not required by the ethics committee of the Hainan General Hospital as this is a retrospective study. No interventional therapy was implemented to the patients and will not affect the outcome of the patients. Data were deidentifed to protect patient information confidentiality and privacy. We declare that this study was conducted in accordance with the Declaration of Helsinki.
Results
Patient demographics and baseline characteristics according to interval category
The baseline characteristics of patients are provided in . Their average age was 47 years, and the median age was 48 years (range, 19–70 years). One-hundred ninety-four (81.2%) patients were male. All the pathological types were type II/III. There were 129 (54.0%) and 110 (46.0%) patients with stage III and IV diseases, respectively. There were 151 (63.2%) and 88 (36.8%) patients with 3 and 4–5 cycles of chemotherapy, respectively.
Table 1 Baseline characteristics of all 239 patients grouped the data by day on the interval between induction chemotherapy and initiating radiotherapy
The median IC-IMRT interval was 9 days (range, 1–76 days). One patient had an interval of 76 days between rounds of treatment. At this point, his clinical stage was T1N2M0, but due to financial difficulties he could not afford radiotherapy after having two cycles of IC. This meant that by the time he and his family had raised enough money for the radiotherapy it was the Spring Festival (Chinese New Year) holiday, which resulted in the delay of 76 days mentioned earlier. However, with this patient it was found during subsequent checkups that 43 months after finishing his treatment there had been no recurrence or metastasis. Overall, the number of cases whose IT was >3 weeks was relatively small, and so the patient was not ruled out by us. A total of 25%, 50%, and 75% of the patients were distributed within 6, 9, and 16 days, respectively. Based on the interval between IC and IMRT, the patients were classified into three groups as follows: Group A (≤7 vs >7 days), Group B (≤14 vs >14 days), and Group C (≤21 vs >21 days). Patient’s characteristics by IC-IMRT interval are listed in . There were more patients receiving three cycles of chemotherapy in the patients with an IC-IMRT interval of ≤7 days in Group A (≤7 vs >7 days) and an IC-IMRT interval of ≤14 days in Group B (≤14 vs >14 days). There were no significant differences in patient characteristics in Group C (≤21 vs >21 days).
The median follow-up time was 40 months (range, 4–58 months). The 3-year OS, DMFS, LRFS, and DFS were 82.7%, 87.5%, 92.5%, and 80.6%, respectively. Thirty patients with details on treatment failure are listed in . There were less patients with LRFS in the patients with an IC-IMRT interval of ≤7 days in Group A.
Table 2 Patterns of failure in 239 patients in different groups
shows the univariate analyses of survival outcomes. The IC-IMRT interval including Group A, Group B, and Group C was not significantly associated with OS, DMFS, LRFS, or DFS. The multivariate analysis shows that the tumor stage was the independent significant predictor for OS, DMFS, LRFS, and DFS in . The survival curves of OS and DFS in Group A, Group B, and Group C are shown in . There was no significant difference in OS and DFS among Group A, Group B, and Group C. But, it appears that there was a trend toward improvement in the outcome of ≤7 days group in OS from the Kaplan–Meier curves.
Figure 1 Kaplan–Meier OS (A–C) and DFS (D–F) curves for the 239 patients grouped the data by interval.
Note: P-values were calculated by the unadjusted log-rank test.
Abbreviations: DFS, disease-free survival; DMFS, distant metastasis-free survival; OS, overall survival.
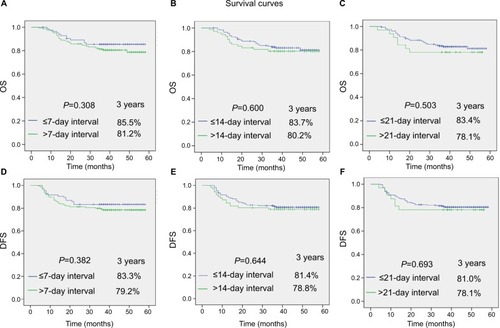
Table 3 Univariate Cox regression analysis of prognostic factors
Discussion
Recently, induced chemotherapy has attracted much attention because in recent successful trials it has been found that it can reduce tumor volume and eliminate micrometastasis before radiotherapy. Following these positive results, IC has become a more promising treatment. Citation6,Citation12–Citation14 However, no published scientific or clinical data to support an exact time frame between IC and concurrent chemoradiation are available yet. This is the first research to explore the impact of timing between IC and radiotherapy on outcomes in patients with NPC.
Comparison of the results of IT in previous research
Positive results
The IT of adjuvant therapy after surgery has been extensively reported by previous studies. Several retrospective cohort studies have found that a longer IT is associated with poor oncological outcomes for patients with breast, endometrial, head, and neck cancers. Citation9–Citation11,Citation15 In some studies,Citation16,Citation17 distant metastasis rates also appeared to increase in women who received radiotherapy for >8 weeks postoperative. In patients with unresected head and neck cancers, delays of 1 month in the initiation of radiotherapy tended to increase the risk of local recurrence at 5 years. Citation18–Citation20 For head and neck cancers, patients who started radiotherapy >6 weeks after the operation had a higher chance of local recurrence. Citation21–Citation24 In one study,Citation25 the 5-year survival rates of patients with non-small-cell lung cancer receiving radiotherapy at 1–6 weeks, 7–8 weeks, and >8 weeks after surgery were 61%, 46%, and 30%, respectively. Recently, a study on 308 endometrial cancer patients found that delay (≥9 weeks) in beginning adjuvant RT after hysterectomy was associated with poor survival outcomes. Citation26
Negative results
Interval timing of postoperative radiotherapy after breast-conserving surgery was not significantly associated with time to local recurrence, FFS, or OS in patients receiving adjuvant endocrine therapy for radiotherapy who had a delay of up to about 20 weeks between treatments as found in the study by Clarke et al. Citation27 In the trial of the International Breast Cancer Research Group, there was no significant correlation with LRFS, DFS, and OS between the timing of radiotherapy after breast-conserving surgery in patients receiving initial or endocrine therapy. Citation28,Citation29 Two population-based cohort studies also found that starting radiotherapy soon after breast-conserving surgery did not improve long-term survival in patients with or without chemotherapy. The study of He et alCitation30 showed that the delay in the beginning of IMRT in locally advanced breast cancer did not increase the likelihood of locoregional recurrence, distant metastasis, and death.
Our result
In our current analysis, characteristics in ≤7 and >7 days groups are relatively balanced (). Although there were more patients receiving three cycles of chemotherapy in the patients with an IC-IMRT interval of ≤7 days in Group A (≤7 vs >7 days), the multivariate analysis shows that the cycles of chemotherapy were not the independent significant predictor for OS, DMFS, LRFS, and DFS (). Although time interval between IC and definitive RT was not significantly associated with OS, DMFS, LRFS, and DFS, shorter time interval patient groups showed better oncological outcomes. In , shorter time interval patient groups showed higher survival curves (OS and DFS) during all time of follow-up duration compared with longer time interval patient groups. Moreover, the survival curves did not cross each other. This phenomenon was particularly evident in Group A (≤7 vs >7 days). It appears that there is a trend toward improvement in the outcome of ≤7 days group in OS and DFS from the Kaplan–Meier curves. In addition, patient group with a time interval of <7 days showed no locoregional recurrences ().
Table 4 Multivariate Cox regression analysis of prognostic factors
Thus, we suggested that patients should start IMRT as soon as possible after IC. It is also feasible to postpone radiotherapy for 1–3 weeks if patients were unable to receive radiotherapy immediately due to chemotherapy complications such as bone marrow suppression.
Limitations
The weakness in this study should be acknowledged. First, the data were collected from a single institution. Furthermore, plasma Epstein–Barr virus (EBV) DNACitation31–Citation33 was not given consideration since the data of plasma EBV DNA were incomplete. Moreover, median follow-up time was 40 months in this study. The long-term outcome needs a followup of >40 months in order to document it in more detail. It is impossible to analyze the impact of an IT of >4 weeks or longer on survival because there were few cases in these patients who had a longer interval.
Conclusion
It is feasible to postpone radiotherapy for 1–3 weeks if patients were unable to receive radiotherapy immediately due to chemotherapy complications such as bone marrow suppression. However, we suggest that patients should start IMRT as soon as possible after IC.
Acknowledgments
We are very grateful to Dean Moody for helping us improve our English writing.
Disclosure
The authors report no conflicts of interest in this work.
References
- LiuLTTangLQChenQYThe prognostic value of plasma Epstein-Barr viral DNA and tumor response to neoadjuvant chemotherapy in advanced-stage nasopharyngeal carcinomaInt J Radiat Oncol Biol Phys201593486286926530755
- ZhangBMoZDuWWangYLiuLWeiYIntensity-modulated radiation therapy versus 2D-RT or 3D-CRT for the treatment of nasopharyngeal carcinoma: a systematic review and meta-analysisOral Oncol201551111041104626296274
- LanMChenCHuangYNeoadjuvant chemotherapy followed by concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in nasopharyngeal carcinoma patients with cervical nodal necrosisSci Rep2017714262428211482
- DuXJTangLLChenLNeoadjuvant chemotherapy in locally advanced nasopharyngeal carcinoma: defining high-risk patients who may benefit before concurrent chemotherapy combined with intensity-modulated radiotherapySci Rep201551666426564805
- PengHChenLZhangJInduction chemotherapy improved long-term outcomes of patients with locoregionally advanced nasopharyngeal carcinoma: a propensity matched analysis of 5-year survival outcomes in the era of intensity-modulated radiotherapyJ Cancer20178337137728261337
- SunYLiWFChenNYInduction chemotherapy plus concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase 3, multicentre, randomised controlled trialLancet Oncol201617111509152027686945
- ValduviecoIVergerEBrunaJImpact of radiotherapy delay on survival in glioblastomaClin Transl Oncol201315427828222855197
- BiagiJJRaphaelMJMackillopWJKongWKingWDBoothCMAssociation between time to initiation of adjuvant chemotherapy and survival in colorectal cancer: a systematic review and meta-analysisJAMA2011305222335234221642686
- BenkVJosephLFortinPEffect of delay in initiating radiotherapy for patients with early stage breast cancerClin Oncol (R Coll Radiol)200416161114768749
- TribiusSDonnerJPazdykaHSurvival and overall treatment time after postoperative radio(chemo)therapy in patients with head and neck cancerHead Neck20163871058106526873810
- AhmadNRLancianoRMCornBWSchultheissTPostoperative radiation therapy for surgically staged endometrial cancer: impact of time factors (overall treatment time and surgery-to-radiation interval) on outcomeInt J Radiat Oncol Biol Phys19953348378427591891
- HongMHNeoadjuvant chemotherapy followed by concurrent chemoradiotherapy versus concurrent chemoradiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: a phase III multicenter randomised controlled trialEur J Canc20177514e23
- PengHChenLLiWFTumor response to neoadjuvant chemotherapy predicts long-term survival outcomes in patients with locoregionally advanced nasopharyngeal carcinoma: a secondary analysis of a randomized phase 3 clinical trialCancer201712391643165228001301
- FangzhengWQuanquanSChunerJGemcitabine/cisplatin induction chemotherapy before concurrent chemotherapy and intensity-modulated radiotherapy improves outcomes for locoregionally advanced nasopharyngeal carcinomaOncotarget2017857967989680829228572
- KimKChieEKHanWNohDYHaSWImpact of delayed radiotherapy on local control in node-negative breast cancer patients treated with breast-conserving surgery and adjuvant radiotherapy without chemotherapyTumori201197334134421789013
- FroudPJMatesDJacksonJSEffect of time interval between breast-conserving surgery and radiation therapy on ipsilateral breast recurrenceInt J Radiat Oncol Biol Phys200046236337210661343
- AmpilFLBurtonGVLiBDMillsGMRadiotherapy with and without chemotherapy after breast conservation surgery for early stage breast cancer: a review of timingEur J Gynaecol Oncol199920425425710475116
- BrouhaXDOp De CoulBTerhaardCHHordijkGJDoes waiting time for radiotherapy affect local control of T1N0M0 glottic laryngeal carcinoma?Clin Otolaryngol200025321521810944052
- BartonMBMorganGSmeeRTiverKWHamiltonCGebskiVDoes waiting time affect the outcome of larynx cancer treated by radiotherapy?Radiother Oncol19974421371419288841
- O’SullivanBMackillopWGriceBThe influence of delay in the initiation of definitive radiotherapy in carcinoma of the tonsillar regionInt J Radiat Oncol Biol Phys199842S97
- DixitSVyasRKToparaniRBBabooHAPatelDDSurgery versus surgery and postoperative radiotherapy in squamous cell carcinoma of the buccal mucosa: a comparative studyAnn Surg Oncol1998565025109754758
- KajantiMHolstiLRHolstiPRadical surgery and postoperative split-course radiotherapy in squamous cell carcinoma of the mobile tongue: factors influencing local control and the time to recurrenceRadiother Oncol19912231741791771258
- AmpilFLBuechterKJBairnsfatherLEShockleyWWTiming and dosage of postoperative radiotherapy for squamous cell carcinoma of the upper aerodigestive tractJ Oral Maxillofac Surg19935111119411978229390
- BastitLBlotEDebourdeauPMenardJBastitPLe FurRInfluence of the delay of adjuvant postoperative radiation therapy on relapse and survival in oropharyngeal and hypopharyngeal cancersInt J Radiat Oncol Biol Phys200149113914611163507
- ChoiNBaumannMFlentjieMPredictive factors in radiotherapy for non-small cell lung cancer: present statusLung Cancer2001311435611162866
- CattaneoRHannaRKJacobsenGElshaikhMAInterval between hysterectomy and start of radiation treatment is predictive of recurrence in patients with endometrial carcinomaInt J Radiat Oncol Biol Phys201488486687124444758
- ClarkeMCollinsRDarbySEffects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trialsLancet200536695032087210616360786
- KarlssonPColeBFColleoniMTiming of radiotherapy and outcome in patients receiving adjuvant endocrine therapyInt J Radiat Oncol Biol Phys201180239840220729007
- KarlssonPColeBFPriceKNTiming of radiation therapy and chemotherapy after breast-conserving surgery for node-positive breast cancer: long-term results from international Breast cancer Study Group trials VI and VIIInt J Radiat Oncol Biol Phys201696227327927598802
- ZhangWWWuSGSunJYLiFYHeZYLong-term survival effect of the interval between mastectomy and radiotherapy in locally advanced breast cancerCancer Manag Res2018102047205430038520
- PengHGuoRChenLPrognostic impact of plasma Epstein-Barr virus DNA in patients with nasopharyngeal carcinoma treated using intensity-modulated radiation therapySci Rep2016612200026924234
- LinJCWangWYLiangWMLong-term prognostic effects of plasma Epstein-Barr virus DNA by minor groove binder-probe real-time quantitative PCR on nasopharyngeal carcinoma patients receiving concurrent chemoradiotherapyInt J Radiat Oncol Biol Phys20076851342134817449194
- ChanATLoYMZeeBPlasma Epstein-Barr virus DNA and residual disease after radiotherapy for undifferentiated nasopharyngeal carcinomaJ Natl Cancer Inst200294211614161912419787
