Abstract
Background
Many patients have a higher risk of thyroid cancer if they have both papillary thyroid carcinoma (PTC) and Type 2 diabetes mellitus (T2DM). Meanwhile, the primary reason for local PTC recurrence is cervical lymph node metastasis. Therefore, the prognosis of patients affects how cervical lymph nodes are managed during surgery. Due to surgical complications such as laryngeal nerve palsy and hypocalcemia, it is still debatable whether to prevent central lymph node dissection (CLND). Predicting central lymph node metastasis (CLNM) is crucial to direct CLND. It is unclear how important the fibrinogen-to-neutrophil ratio (FNR) is in thyroid cancer, so we looked into how it might help patients with PTC and T2DM predict CLNM.
Patients and methods
Wenzhou Medical University’s First Affiliated Hospital provided us with 413 patients with PTC and T2DM, randomly divided into a training set (N = 292) and a validation set (N = 121). Univariate and multivariate logistic regression analyses were used to identify independent risk factors. After constructing a nomogram, the validity of the model was evaluated.
Results
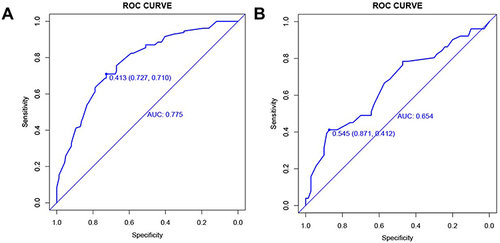
The maximum tumor diameter, high-density lipoprotein, thyroxine, triglyceride, lymphocyte, and FNR were all identified as independent risk factors by multivariate logistic regression analysis. The C index of the training set was 0.775, and the validation set was 0.654.
Conclusion
In patients with PTC and T2DM, preoperative FNR was an independent risk factor for CLNM.
Introduction
Thyroid cancer is a common endocrine malignancy.Citation1 According to cancer statistics, thyroid cancer is now the ninth most common cancer globally, with 586,000 new cases reported yearly. Women are three times more likely than men to experience the condition globally.Citation2 The high incidence of thyroid cancer may be primarily attributed to improved papillary thyroid carcinoma (PTC) detection and diagnosis.Citation3,Citation4 Worldwide, diabetes mellitus (DM) incidence and mortality are rising.Citation5 Both thyroid cancer and diabetes affect a large number of patients. Therefore, we cannot disregard the substantial number of such patients. This justifies the target population of this study is patients with PTC and T2DM.
PTC is the most important type of thyroid cancer.Citation1,Citation6 Cervical lymph node metastasis occurs in 40–90% of the cases.Citation7 Although PTC lymph node metastasis most commonly occurs in the central region, it is also possible to skip metastasis.Citation8 LNM is an important indicator of the prognosis, scope, and surgical method of PTC, as well as an important risk factor for both a high recurrence rate and a low patient survival rate.Citation9 However, prophylactic central lymph node dissection (CLND) is still debatable because it can lead to surgical complications such as laryngeal nerve palsy and hypocalcemia caused by resection of CLND.Citation10 Therefore, it is crucial to accurately predict the likelihood of preoperative central lymph node metastasis (CLNM) so that some patients with PTC can avoid preventive CLND.
Cancer occurrence, development, and metastasis are closely linked to inflammation.Citation11,Citation12 Numerous inflammatory indicators, such as neutrophil,Citation13 lymphocyte,Citation14 C-reactive protein,Citation15 fibrinogen,Citation16 the neutrophil-to-lymphocyte ratio,Citation17 the platelet-to-lymphocyte ratio,Citation18 etc., are linked to cancer. Fibrinogen, a glycoprotein, is an essential clotting factor in the inflammatory response.Citation19 Increased fibrinogen has recently been associated with the progression and poor prognosis of some malignancies, such as gastric cancer,Citation20 gallbladder cancer,Citation21 and bladder cancer.Citation22
The fibrinogen to the neutrophil ratio (FNR), a new predictive marker, was identified in our study, and its predictive value for CLNM in patients with PTC and T2DM was evaluated.
Methods
Patients
We enrolled 413 patients with PTC and T2DM who underwent thyroid lobectomy and lymph node dissection at the First Affiliated Hospital of Wenzhou Medical University from 2018 to 2021. The following were our exclusion criteria:
Insufficient clinical data.
Non-thyroid papillary carcinoma was suggested by intraoperative rapid freezing and postoperative paraffin specimens or pathologically confirmed by PTC without CLND.
History of hyperthyroidism, thyroid radiation, and thyroid surgery.
History of other malignant tumors.
Patients with hemoglobin A1c >7% or who had poor preoperative blood glucose control were not eligible for surgery.
Preoperative imaging tests revealed evidence of enlargement of central or lateral lymph nodes or distant tumor metastasis.
Information Collection
All enrolled patients received complete information. Basic information including name, hospitalization number, age, sex, history of diabetes, medication use, etc. Prior to surgery, all patients underwent a thorough evaluation that included a preoperative thyroid ultrasound, computed tomography (CT) scan, blood routine, blood biochemistry, blood glucose monitoring, and thyroid function examination. Additionally, surgical records, intraoperative rapid freezing, and postoperative paraffin pathology were collected.
Data Analysis
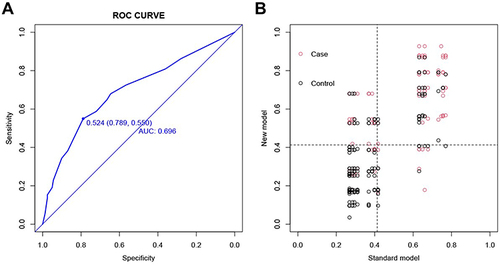
Receiver operating characteristic (ROC) curve analysis, which converts continuous variables into dichotomous variables for straightforward analysis, helps us determine the optimal cut-off values. By entering a random seed number, the 413 cases were randomly divided into a training set (N = 292) and a validation set (N = 121). The two cohorts were then compared using the chi-square test to determine whether they were comparable. To further assess the independent risk factors for CLNM in the training set, factors with P < 0.1 were included in multivariate logistic regression analysis based on the binary logistic regression analysis results. Then, to create nomogram plots, factors with P < 0.05 in the multiple regression analysis were selected. The prediction performance of the training and validation sets was measured using the area under the curve (AUC) under the ROC curve. We used a calibration plot to show the consistency between predictions and results. The calibration plot’s p-value was also evaluated using the Hosmer-Lemeshow test (a score of p > 0.05 indicated a good model fit). The clinical result of the model was assessed using decision curve analysis (DCA). To determine whether the new model’s predictive ability had increased, we compared it to the original model and used the integrated discrimination improvement (IDI) and net reclassification index (NRI) measures; if IDI >0, the new model’s predictive power was considered to have increased compared to the original model. If IDI <0, it had decreased predictive power; if IDI = 0, there had been no improvement. NRI and IDI had similar significance. R 4.0.2 and statistical package for social sciences 25.0 were used.
Result
Clinical Characteristics of Patients
The First Affiliated Hospital of Wenzhou Medical University from 2018 to 2021 included 413 patients with PTC and T2DM. In the R package, 413 cases were randomly divided into a training set (N = 292) and a validation set (N = 121) in a 7:3 ratio. The data were processed if the ROC curve identified the ideal cut-off value for a continuous variable. shows the chi-square analysis of the two data groups; the results suggested that the two data groups were consistent and comparable.
Table 1 Baseline Characteristics of the Training Dataset and the External Validation Dataset
Correlation of FNR with Clinicopathological Features in the Two Cohorts
Using the ideal FNR cut-off value, data were divided into high FNR group (N = 259) and low FNR group (N = 154). Age (P = 0.007), maximum tumor diameter (P = 0.048), neutrophils (P < 0.001), monocytes (P < 0.001), percentage of lymphocytes (P < 0.001), T3 (P = 0.005), and fibrinogen (P < 0.001) were all significantly correlated with FNR ().
Table 2 Correlations Between FNR and Clinical Characteristics in All Cohorts
Univariate and Multivariate Logistic Regression Analyses of Preoperative CLNM
Metformin (P = 0.087), maximum tumor diameter (P < 0.001), triglyceride (TG) (P = 0.001), high-density lipoprotein (HDL) (P = 0.009), lymphocyte (P = 0.032), thyroxine (T4) (P = 0.099), and FNR (P = 0.028) were all associated with CLNM in univariate regression analysis. Multivariate regression analysis was used to identify further the independent risk factors associated with CLNM. The larger the tumor, the lower the TG, HDL, lymphocytes, T4, and FNR, and the more likely CLNM occurred ().
Table 3 Univariate and Multivariate Analysis of Logistic Regression in the Training Data Set
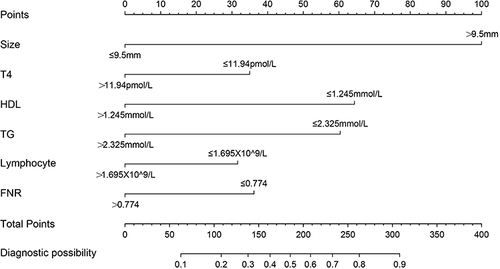
Build the Predicted Nomogram
A nomogram was created to predict the risk of CLNM using the independent factors screened by multivariate analysis that was included in the analysis (). We plotted the scores of each independent predictor and continuously added them to obtain the total score to confirm the likelihood of preoperative CLNM.
Evaluate the Effectiveness of the Nomogram
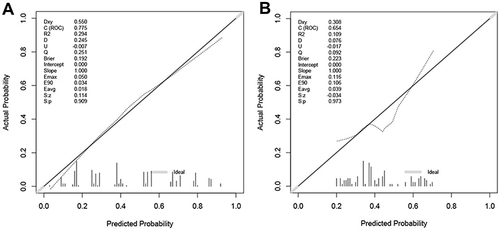
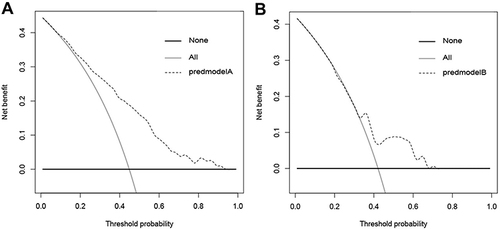
ROC curves were created using R packages to evaluate the ability of our nomogram to predict CLNM. The AUC of the training set () and validation set () were 0.775 and 0.654, respectively, as shown in the figure. It was demonstrated that the method accurately predicts CLNM. Additionally, according to the Hosmer-Lemeshow test, the calibration diagrams of our recently developed model ( and ) were well-fit between the actual and estimated probabilities of CLNM (internal training set, p = 0.677826 > 0.05 and external validation set p = 0.6933441 > 0.05). We used DCA to assess whether the benefits of using our predictive model in the clinic outweigh the risks ( and ). The ordinate is threshold probability, and the ordinate is a net return. All patients did not receive net benefits from CLND, as indicated by the gray line. The gray dotted line represents the patient’s net clinical benefit. The threshold probability range for this rosette was approximately 10–90% in the training set and 30–70% in the validation set, with a higher net clinical benefit when compared with all or none of the patients receiving CLND treatment.
Comparison with the Original Model
We compared our new model with the original one to determine whether it had better test performance. The model constructed by Thompson et al included age, gender, maximum tumor diameter, and multifocality.Citation23 Inputting our data yielded an AUC of 0.696, which was lower than the new one’s AUC of 0.775 (). It demonstrated the new model’s improved accuracy. The problem of comparing the diagnostic efficacy of the two models can be resolved by applying NRI and IDI, which quantifies the degree of improvement in the diagnostic efficacy of one index over another. shows NRI = 0.1283 and IDI = 0.0929. Both NRI and IDI showed that the new model’s testing efficiency is higher than the original model.
Discussion
To the best of our knowledge, this study is the first to focus on the relationship between preoperative FNR and CLNM in patients with PTC and T2DM, as well as the relationship between preoperative FNR and cancer FNR and cancer. FNR-related research has not yet been published. Our research remains significant and valuable.
Currently, surgeons typically perform preventive lymph node dissection in patients with PTC’s central region of the neck. Still, this practice can raise the danger of postoperative hypocalcemia, which is controversial in CLND research.Citation10 Ultrasound is still the primary imaging technique for detecting CLNM in PTC among the commonly used clinical diagnosis and treatment approaches. When assessing CLNM of PTC, CT, magnetic resonance imaging, and other imaging techniques are not more effective than ultrasound.Citation24,Citation25 However, there are high false negatives and poor diagnostic accuracy with ultrasound diagnosis of CLNM in PTC. An important factor in surgical selection is the ability to accurately identify patients who do not require preventive dissection of lymph nodes in the central region of the neck prior to surgery. This issue has become an urgent clinical problem that needs to be resolved.
There is growing evidence that inflammation is a crucial factor inextricably linked to cancer, with neutrophils, monocytes, and other inflammatory cells promoting tumor cell proliferation, survival, and migration.Citation26 Numerous studies have linked elevated fibrinogen to some malignant tumors’ progression and poor prognosis.Citation20–22 However, studies on the role of FNR in cancer are lacking. According to two large studies, thyroid cancer may be influenced by a history of diabetes.Citation27,Citation28 Thyroid cancer is more common in people with diabetes than those without,Citation29 with a 20% increase in incidence compared to those without DM.Citation30 What’s more, according to a study by Xu et al, who used data from a cohort of 36,379 patients with Type 2 DM (T2DM), the crude incidence of thyroid cancer and T2DM in men was 5.01 per 105 person-years. The crude incidence of cancer subtypes for women was 34.97 per 105 person-years, placing women in the top 10.Citation31 Therefore, we boldly hypothesized that in patients with PTC and T2DM, preoperative FNR was significantly associated with CLNM.
Statistics were used to screen out the independent risk factors for CLNM in 413 patients with PTC and T2DM. These risk factors included maximum tumor diameter >9.5mm, low TG, low lymphocyte, low HDL, low T4, and low FNR. A low FNR value indicated low fibrinogen or high neutrophils. Fibrinogen and neutrophils were known to be associated with poor prognosis of tumors. In our previous data analysis, it was found that there was no significant correlation between CLNM of PTC and T2DM and fibrinogen alone, and the AUC value of the ROC curve for the analysis results of neutrophil number alone was lower than that of FNR. These results indicated that in patients with PTC and T2DM, FNR was a novel and more significant indicator for predicting preoperative CLNM. Tumor size is an independent risk factor for CLNM, supporting earlier studies. Liu et al concluded that the tumor measured 1.0 cm in diameter.Citation32 The ideal tumor truncation measured was 1.1 cm by Wu et al.Citation33 In the study by Zhou et al, the ideal truncation value of the tumor was 0.7 cm.Citation34 In our study, the ideal truncation value was 0.95 cm. TG had various effects on various cancers.Citation35–39 Studies conducted in Austria showed a positive correlation between TG and thyroid cancer.Citation37 In our study, patients with PTC and T2DM may have increased CLNM metastasis due to low TG levels. Further studies are needed to verify the mechanism of TG in tumor development, most likely because the Austrian study was prospective, and ours was a case-control study with some selection bias. The lymphocyte’s primary component of anti-tumor immunity can activate the release of cytokines such as interferon and tumor necrosis factor-α to play a protective role.Citation26,Citation40 Low lymphocyte count, which has been regarded as a poor prognostic biomarker,Citation14,Citation41 was associated with CLNM in this study. Low lymphocyte count may also be associated with activating reactive oxygen species-mediated apoptosis pathways.Citation42 Recent studies have found a negative correlation between HDL and cancer. HDL may exert anti-inflammatory and antioxidant properties by regulating cytokine production.Citation43 Further research must be done to determine the specific mechanism of action. In our study, low HDL levels in patients with PTC and T2DM may be associated with CLNM. Li et al found that low T4 levels were only related to capsule infiltration, and routine preoperative serum T4 determination helped identify which patients should undergo surgery.Citation44 Lower T4 levels were found to be correlated with an increased risk of thyroid cancer.Citation45
We constructed relevant programs further to explore the clinical value of this new indicator after it was established that low FNR was an independent risk factor for CLNM in patients with PTC and T2DM. Our nomogram exhibits good discrimination and calibration. Additionally, the ROC curve shows that the rotors are more accurate predictors than the original model.Citation23 Both NRI and IDI suggest that our model’s predictive ability has increased compared to the original model. Because routine tests like blood indicators, blood glucose, and B-ultrasound are performed before each patient is admitted to the hospital for surgery, our model is a simple to use the clinical tool. The model is universal and can facilitate patient consultation and personalized treatment.
This study has some limitations. First, this analysis uses a small sample size. To confirm this, multicenter studies are needed. Second, since this is a retrospective study, data biases such as selection bias are unavoidable. We anticipate developing more accurate indicators and tools to predict CLNM in the future.
In conclusion, FNR is a new predictor and an independent risk factor for CLNM in patients with PTC and T2DM.
Ethical Approval and Informed Consent
The approval of the clinical ethics committee was obtained from the ethics committee of the First Affiliated Hospital of Wenzhou Medical University. This study design was in accordance with the Declaration of Helsinki. All individual participants were aware and signed the informed consent for participation in this study.
Disclosure
All authors declare no potential conflicts of interest in this work.
Additional information
Funding
References
- Wiltshire J, Drake T, Uttley L, Balasubramanian SJ. Systematic review of trends in the incidence rates of thyroid cancer. Thyroid. 2016;26(11):1541–1552. doi:10.1089/thy.2016.0100
- Sung H, Ferlay J, Siegel R, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
- Li N, Du X, Reitzel L, Xu L, Sturgis EM. Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance, epidemiology, and end results registry, 1980–2008. Thyroid. 2013;23(1):103–110. doi:10.1089/thy.2012.0392
- Hajeer M, Awad H, Abdullah N, Almuhaisen G, Abudalu LE. The rising trend in papillary thyroid carcinoma. True increase or over diagnosis? Saudi Med J. 2018;39(2):147–153. doi:10.15537/smj.2018.2.21211
- Cho N, Shaw J, Karuranga S, et al. IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi:10.1016/j.diabres.2018.02.023
- Al-Brahim N, Asa S. Papillary thyroid carcinoma: an overview. Arch Pathol Lab Med. 2006;130(7):1057–1062. doi:10.5858/2006-130-1057-PTCAO
- Lundgren C, Hall P, Dickman P, Zedenius J. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006;106(3):524–531. doi:10.1002/cncr.21653
- Lim Y, Koo BS. Predictive factors of skip metastases to lateral neck compartment leaping central neck compartment in papillary thyroid carcinoma. Oral Oncol. 2012;48(3):262–265. doi:10.1016/j.oraloncology.2011.10.006
- Zhao Q, Ming J, Liu C, Shi L, Xu X, Nie X. Multifocality and total tumor diameter predict central neck lymph node metastases in papillary thyroid microcarcinoma. Ann Surg Oncol. 2013;20(3):746–752. doi:10.1245/s10434-012-2654-2
- Calò P, Medas F, Conzo G, et al. Intraoperative neuromonitoring in thyroid surgery: is the two-staged thyroidectomy justified? Int J Surg. 2017;41(Suppl 1):S13–S20. doi:10.1016/j.ijsu.2017.02.001
- Greten F, Grivennikov S. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51(1):27–41. doi:10.1016/j.immuni.2019.06.025
- McMillan DC. The systemic inflammation-based Glasgow prognostic score: a decade of experience in patients with cancer. Cancer Treat Rev. 2013;39(5):534–540. doi:10.1016/j.ctrv.2012.08.003
- Brostjan C, Oehler R. The role of neutrophil death in chronic inflammation and cancer. Cell Death Discov. 2020;6:26. doi:10.1038/s41420-020-0255-6
- Feng F, Zheng G, Wang Q, et al. Low lymphocyte count and high monocyte count predicts poor prognosis of gastric cancer. BMC Gastroenterol. 2018;18(1):148. doi:10.1186/s12876-018-0877-9
- Hart P, Rajab I, Alebraheem M, Potempa LA. C-reactive protein and cancer-diagnostic and therapeutic insights. Front Immunol. 2020;11:595835. doi:10.3389/fimmu.2020.595835
- Li X, Shu K, Zhou J, et al. Preoperative plasma fibrinogen and D-dimer as prognostic biomarkers for non-muscle-invasive bladder cancer. Clin Genitourin Cancer. 2020;18(1):11–19.e11. doi:10.1016/j.clgc.2019.10.025
- Hasegawa T, Iga T, Takeda D, et al. Neutrophil-lymphocyte ratio associated with poor prognosis in oral cancer: a retrospective study. BMC Cancer. 2020;20(1):568. doi:10.1186/s12885-020-07063-1
- Zhang X, Zhao W, Yu Y, et al. Clinicopathological and prognostic significance of platelet-lymphocyte ratio (PLR) in gastric cancer: an updated meta-analysis. World J Surg Oncol. 2020;18(1):191. doi:10.1186/s12957-020-01952-2
- Luyendyk J, Schoenecker J, Flick M. The multifaceted role of fibrinogen in tissue injury and inflammation. Blood. 2019;133(6):511–520. doi:10.1182/blood-2018-07-818211
- Cheng F, Zeng C, Zeng L, Chen YJM. Clinicopathological and prognostic value of preoperative plasma fibrinogen in gastric cancer patients: a meta-analysis. Medicine. 2019;98(40):e17310. doi:10.1097/MD.0000000000017310
- Xu W, Zhang H, Yang X, et al. Prognostic significance of combined preoperative fibrinogen and CA199 in gallbladder cancer patients. World J Gastroenterol. 2018;24(13):1451–1463. doi:10.3748/wjg.v24.i13.1451
- Yang S, Guan H, Wang S, Wu H, Sun W, Chen Z. Plasma fibrinogen predicts the prognosis of bladder cancer patients after radical cystectomy. Cancer Manag Res. 2020;12:9303–9314. doi:10.2147/CMAR.S269244
- Thompson A, Turner R, Hayen A, et al. A preoperative nomogram for the prediction of ipsilateral central compartment lymph node metastases in papillary thyroid cancer. Thyroid. 2014;24(4):675–682. doi:10.1089/thy.2013.0224
- Suh C, Baek J, Choi Y, Lee JH. Performance of CT in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid cancer: a systematic review and meta-analysis. Am J Neuroradiol. 2017;38(1):154–161. doi:10.3174/ajnr.A4967
- Chen Q, Raghavan P, Mukherjee S, et al. Accuracy of MRI for the diagnosis of metastatic cervical lymphadenopathy in patients with thyroid cancer. Radiol Med. 2015;120(10):959–966. doi:10.1007/s11547-014-0474-0
- Coussens L, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860–867. doi:10.1038/nature01322
- Aschebrook-Kilfoy B, Sabra M, Brenner A, et al. Diabetes and thyroid cancer risk in the national institutes of Health-AARP diet and health study. Thyroid. 2011;21(9):957–963. doi:10.1089/thy.2010.0396
- Meinhold C, Ron E, Schonfeld S, Alexander B, Freedman D, Linet M. Nonradiation risk factors for thyroid cancer in the US radiologic technologists study. Am J Epidemiol. 2010;171(2):242–252. doi:10.1093/aje/kwp354
- Schmid D, Behrens G, Jochem C, Keimling M, Leitzmann M. Physical activity, diabetes, and risk of thyroid cancer: a systematic review and meta-analysis. Eur J Epidemiol. 2013;28(12):945–958. doi:10.1007/s10654-013-9865-0
- Li H, Qian J. Association of diabetes mellitus with thyroid cancer risk: a meta-analysis of cohort studies. Medicine. 2017;96(47):e8230. doi:10.1097/MD.0000000000008230
- Xu H, Fang H, Xu W, et al. Cancer incidence in patients with type 2 diabetes mellitus: a population-based cohort study in Shanghai. BMC Cancer. 2015;15:852. doi:10.1186/s12885-015-1887-4
- Liu C, Xiao C, Chen J, Li X, Feng Z, Gao Q. Risk factor analysis for predicting cervical lymph node metastasis in papillary thyroid carcinoma: a study of 966 patients. BMC Cancer. 2019;19(1):622. doi:10.1186/s12885-019-5835-6
- Wu Y, Rao K, Liu J, et al. Machine learning algorithms for the prediction of central lymph node metastasis in patients with papillary thyroid cancer. Front Endocrinol. 2020;11:577537. doi:10.3389/fendo.2020.577537
- Zhou Y, Gao E, Zhang W, Yang H, Guo G, Zhang X. Factors predictive of papillary thyroid micro-carcinoma with bilateral involvement and central lymph node metastasis: a retrospective study. World J Surg Oncol. 2012;10(1):67. doi:10.1186/1477-7819-10-67
- Wulaningsih W, Garmo H, Holmberg L, Hammar N, Jungner I, Walldius G. Serum Lipids and the risk of gastrointestinal malignancies in the Swedish AMORIS study. J Cancer Epidemiol. 2012;2012:792034. doi:10.1155/2012/792034
- Vatten L, Foss OP. Total serum cholesterol and triglycerides and risk of breast cancer: a prospective study of 24,329 Norwegian women. Cancer Res. 1990;50(8):2341–2346.
- Ulmer H, Borena W, Rapp K, et al. Serum triglyceride concentrations and cancer risk in a large cohort study in Austria. Br J Cancer. 2009;101(7):1202–1206. doi:10.1038/sj.bjc.6605264
- Wuermli L, Joerger M, Henz S, et al. Hypertriglyceridemia as a possible risk factor for prostate cancer. Prostate Cancer Prostatic Dis. 2005;8(4):316–320. doi:10.1038/sj.pcan.4500834
- Martin R, Vatten L, Gunnell D, Romundstad P, Nilsen T. Components of the metabolic syndrome and risk of prostate cancer: the HUNT 2 cohort, Norway. Cancer Causes Control. 2009;20(7):1181–1192.
- Grivennikov S, Greten F, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–899. doi:10.1016/j.cell.2010.01.025
- Quigley D, Kristensen V. Predicting prognosis and therapeutic response from interactions between lymphocytes and tumor cells. Mol Oncol. 2015;9(10):2054–2062. doi:10.1016/j.molonc.2015.10.003
- Kim B, Chung H. Hypoxia/reoxygenation induces apoptosis through a ROS-mediated caspase-8/Bid/Bax pathway in human lymphocytes. Biochem Biophys Res Commun. 2007;363(3):745–750. doi:10.1016/j.bbrc.2007.09.024
- Barter P, Nicholls S, Rye K, Anantharamaiah G, Navab M, Fogelman AM. Antiinflammatory properties of HDL. Circ Res. 2004;95(8):764–772. doi:10.1161/01.RES.0000146094.59640.13
- Li C, Yu W, Fan J, et al. Thyroid functional parameters and correlative autoantibodies as prognostic factors for differentiated thyroid cancers. Oncotarget. 2016;7(31):49930–49938. doi:10.18632/oncotarget.10236
- Gul K, Ozdemir D, Dirikoc A, et al. Are endogenously lower serum thyroid hormones new predictors for thyroid malignancy in addition to higher serum thyrotropin? Endocrine. 2010;37(2):253–260. doi:10.1007/s12020-010-9316-6