Abstract
Background
Commonly, the thyroid gland is regarded as an organ with fewer metastatic diseases, and colorectal metastasis to the thyroid (CMT) is rarely reported, especially, with that the clinical sign of thyroid metastasis nidus is the chief complaint. The CMT occurs in advanced colorectal cancer and is associated with poor prognosis and short survival.
Case Report
In this case, we reported a patient with the sign of neck mass as the first manifestation of CMT. The patient underwent a partial thyroidectomy in June 2019, immunohistochemical findings of thyroid carcinoma suggested the possibility of adenocarcinoma of gastrointestinal tract. The patient underwent a colonoscopy in July 2019 and a colonic mass was found. Pathological examination diagnosed rectal adenocarcinoma. The patient underwent neoadjuvant chemotherapy, surgical treatment, postoperative adjuvant chemotherapy and targeted therapy. The patient died in June 2022.
Conclusion
The metastasis disease would not be ignored at all, when a patient complains at signs of neck mass. Further, the possibility of metastasis cancer should be considered once thyroid nodules occur in patients with colorectal cancer. Even though the biological characteristics and stage of the primary tumor have an important impact on the prognosis, positive standardized treatments can also be helpful.
Introduction
More than 1.9 million new colorectal cancer (including anus) cases and 935,000 deaths were estimated to occur in 2020, representing about one in 10 cancer cases and deaths.Citation1 The common metastatic sites of colorectal cancer include the liver and lung, but metastasis to the thyroid is rare. The thyroid metastatic carcinoma accounts for 1.4–3% of all thyroid carcinomas,Citation2 which is much less than the ratio of 1.9–9.5% detected during autopsies.Citation3
Several theories have been developed to explain the mechanisms that contribute to the rarity of thyroid gland metastatic deposits, including failure of cellular adhesion due to rapid arterial blood flow and inhibition of tumor cell growth by high iodine concentrations.Citation4
In the literature review, CMTs were all found during follow-up after colorectal cancer surgery. We report here a special case in which CMT was detected earlier than colorectal cancer, as well as a literature review of reported cases of colorectal metastasis to the thyroid.
Case Presentation
A 46-year-old woman initially presented with a 4-month history of a right anterior cervical mass without voice hoarse, dyspnea, pain, or bucking in June 2019. Physical examinations revealed a palpable 1.5 cm right thyroid nodule moving with deglutition, and without obviously enlarged lymph nodes. Ultrasonography showed a hypoechoic nodule in the right thyroid (TI-RADS 4A), and papillary thyroid carcinoma was diagnosed based on a needle aspiration cytology examination.
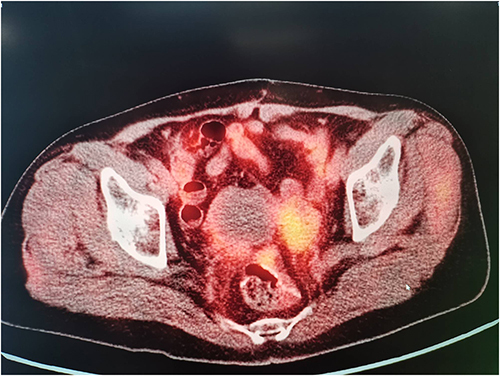
The patient then underwent a resection of the right thyroid and isthmus on June 15, 2019. The thyroid adenocarcinoma was shown by a histological analysis of the specimen (). Positive CDX2 and cytokeratin 20, and negative thyroid transcription factor 1 (TTF1) and thyroglobulin (TG) () were revealed by immunohistochemistry examinations, which indicated that the primary tumor originated was from the gastrointestinal tract. Then, colonoscopy revealed a tumor 10 cm from the anal margin. Histological analysis of the specimen confirmed moderately differentiated adenocarcinoma (). Positron Emission Tomography-Computed Tomography (PET-CT) showed colorectal carcinoma accompanied by multiple lymph nodes metastases (). And the carcinoembryonic antigen (CEA) was 7ng/mL. Chemotherapy, which included 2 cycles of intravenous raltitrexed combined with oxaliplatin and oral capecitabine, showed an excellent response, resulting in a decrease of CEA to 2.71ng/mL.
Figure 1 There were more adulterants in the thyroid gland, with disordered arrangement, some glands fused, and obvious cell atypia. The arrow indicates the heterocyst.
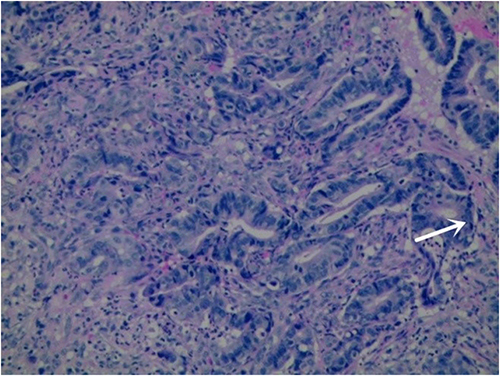
Figure 2 Immunohistochemistry revealed adenoid arrangement of heteromorphic cells with interstitial fibrosis. Immunohistochemistry revealed positive expression of CDX-2 (an intestinal specific transcription factor) and Villin, while negative expression of TG (thyroglobulin), suggesting a high possibility of intestinal metastatic adenocarcinoma. (A) The tumor cells (blue arrows) are adenoid and distributed in the thyroid tissue. And the thyroid follicles can be seen (red arrows); (B) The tumor cells were positive for CDX-2; (C) The tumor cells Villin were positive; (D) TG in thyroid follicles was positive and TG in tumor cells was negative.
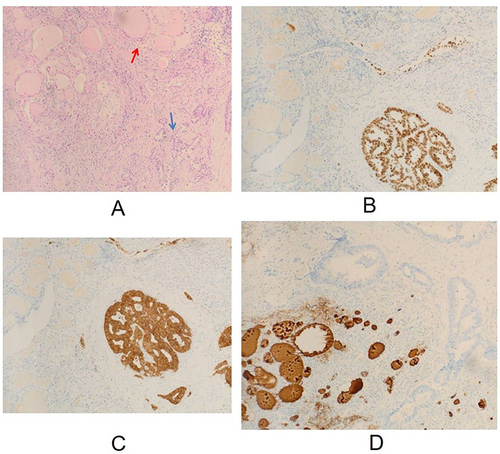
Figure 3 Heterotypic glands fused, partially ethmoidal, with marked interstitial fibrosis. The arrow indicates Cribriform heteromorphic cell fusion.
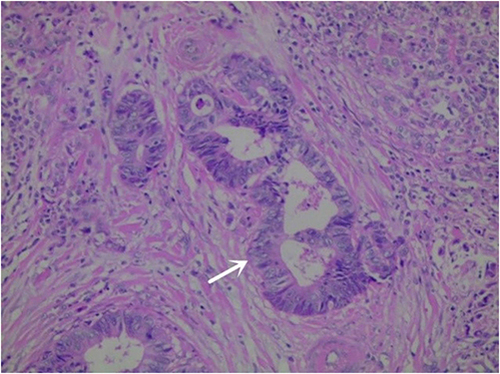
Figure 4 The 18F-FDG PET/CT scan images showing increased focal FDG uptake in the rectal mass and pelvic lymph nodes.
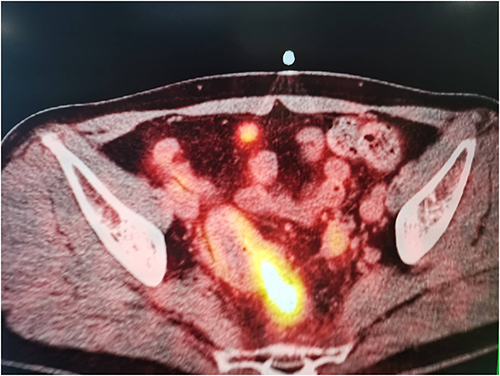
An anterior resection of the rectal cancer was performed on August 23, 2019, after a treatment with diabetes in the endocrinology department. A moderately differentiated adenocarcinoma with penetration of the intestinal wall into the submucosal adipose tissue was reported by the histological analysis of the specimen. Two of 16 dissected lymph nodes showed carcinoma metastasis. The postoperative TNM stage was pT3N1M1. Four courses of intravenous oxaliplatin combined with oral capecitabine were given after surgery. Until August 2020, a progressive increase in CEA was detected. Oral capecitabine was not satisfactory and CEA levels fluctuated repeatedly. From March 2021 to September 2021, four courses of targeted therapy (bevacizumab 400 mg) combined with chemotherapies (intravenous irinotecan combined with oral capecitabine) were given, with good tolerance. Then, on October 18, 2021, a second PET-CT examination suggested multiple metastases of the abdominal omentum and pelvic cavity (). Sequentially, the patient received another targeted therapy with a combination of chemotherapies (pembrolizumab, cetuximab, irinotecan, and raltitrexed) for 6 months. The patient died on June 2, 2022, with an overall survival of 35 months following diagnosis of colorectal cancer thyroid metastases.
Discussion
We reported a patient who complained about the neck mass without other symptoms but was finally diagnosed with colorectal cancer with thyroid metastasis. The colorectal cancer metastatic thyroid cancer is rarely reported, and sign of CMT as the initial symptom is much rarer.
We searched the literature on colorectal cancer metastasis to the thyroid and identified 13 cases between 2000 and 2020 (). Of these 13 patients, 10 underwent FNAB. Five cases were confirmed as having metastatic adenocarcinoma, three cases were diagnosed as papillary thyroid carcinoma, and one case was considered a benign tumor or hyperplastic change. Of the 13 cases reviewed, the mean interval from diagnosis of colorectal cancer to confirmation of thyroid metastasis carcinoma was 43.15 months (0–95 months). Thyroid gland metastases can present decades after the initial diagnosis and treatment of colorectum cancer.
Table 1 Thirteen Cases of Thyroid Metastases from Colorectum, the Previously Reported Cases in the Literature
Two hypotheses can explain the rarity of metastatic thyroid cancer. One of them is that the abundant blood flow in the thyroid makes malignant tumor cells hard to colonize. Another is that the high-iodine and high-oxygen environment of thyroid tissue may inhibit the growth of tumor cells.Citation4,Citation13 Studies have shown that thyroid nodules are more likely to develop thyroid metastases. Multinodular goiters and adenomas with altered structures may also alter the thyroid environment, resulting in them being more favorable for the colonization and growth of metastatic colorectal cancer cells.Citation5 CMTs are found after the treatment of primary colorectal cancer, most of them previously diagnosed of liver and/or lung metastases, while the latter are more common obviously.Citation4 Thyroid metastasis of colorectal cancer occurs mainly through the blood-type route, and colorectal cancer spreads to the thyroid through the portal vein, vena cava, and pulmonary vein.Citation6,Citation14 Also, BatsonCitation15 proposed another blood-borne metastasis route, the vertebral venous system, which allows carcinoma to transfer to the thyroid without passing through the portal vein, pulmonary vein, or vena cava. And cancer cells do not enter the thoracic or abdominal cavities. The ability of the colorectum cancer to transfer directly to the thyroid explains the isolated thyroid metastasis in this case, in which the CMT was the first and the sole metastatic site of the primary tumor.
Actually, that metastasis of the thyroid may not be as rare as the accounting ratio, but with a missed diagnosis, which suggested by the data of autopsy. The kidney, particularly renal clear cell carcinoma, are the most common origins of thyroid metastasis. Metastases from colorectal cancer to the thyroid are rare, accounting for only 0.1% of all colorectal cancer cases.Citation16 Similar to primary malignant thyroid tumors, thyroid gland metastases can manifest as goiter, neck lumps, dysphagia, dyspnea, pain, and hoarseness. In other cases, thyroid gland metastases can also show a clinically silent course without specific symptoms, and are occasionally discovered after imaging procedures. However, routine follow-up examinations of colorectal carcinoma incl thoracic, abdominal, and pelvic examinations, but not neck evaluation,may lead to more cases being reported during autopsies. In the 13 reviewed cases, seven patients (53.85%) were diagnosed on detailed routine follow-up examinations, higher than that reported in the past.Citation4 More cases of thyroid gland metastases prior to the diagnosis of rectal cancer occurring may relate to improvements in follow-up techniques and more attention to thyroid gland metastases. Early detection and treatment of malignant tumors have a positive effect on the prognosis of patients, and the early detection of metastatic lesions will commonly change the treatment strategy, which may improve the efficacy and prognosis.
The application of PET-CT increases the number of patients accidentally discovered with thyroid gland metastases in clinical practice.Citation17,Citation18 In a retrospective study in which patients with a history of non-thyroid malignancies underwent PET-CT examination, 71 cases (3.7%) had increased thyroid uptake, 20 patients underwent fine-needle aspiration biopsy (FNAB), and 8 cases were finally diagnosed with malignant tumors (including primary thyroid tumors).Citation19 In another retrospective study, 24 patients with secondary thyroid carcinoma diagnosed by cytology and PET-CT were included, while 16 patients showed no clinical symptoms. The original treatment plan has changed because of the discovery of metastatic thyroid cancer.Citation20 The two retrospective studies emphasized the importance of PET-CT examination for detecting potential metastases, especially non-symptom thyroid metastases. For patients with a history of malignant tumors, PET-CT seems to be essential for patient management (follow-up and treatment plans). However, in view of the higher possibility of malignancy of the goiter with increasedCitation21 F-FDG uptake, the benefit-risk balance must be considered, and further investigations should be conducted.
Fine-needle aspiration (FNA) has a high accuracy and specificity for the diagnosis of thyroid metastases. The sensitivity for detecting thyroid cancer metastasis is 94%, and the specificity is 100%.Citation22 With the improvement and the increase using frequency of FNA technology, the detection rate of thyroid gland metastases is increasing.Citation23 FNAB avoids unnecessary surgical treatment. Some surgeons believe that surgical intervention is unnecessary without proven survival benefits,Citation13 and the source of the tumor and whether it is a sole metastatic site are all necessary factors for surgical treatment.Citation21,Citation24 But it is difficult to identify primary and secondary thyroid cancers. Metastatic colorectal adenocarcinoma and thyroid papillary carcinoma have highly similar cell or columnar cell variants.Citation25,Citation26 Considering the differentiation of thyroid gland metastases from primary tumors and the diversity of primary tumors, physicians’ experience in suspecting thyroid cancer metastasis and extensive immunohistochemistry is necessary.
Immunohistochemistry (IHC) can distinguish most primary thyroid cancers from thyroid gland metastases. TTF1(-) and TG(-) levels of thyroid tumors can be used to exclude primary tumors.
Immunohistochemistry provides an important clue for the diagnosis of primary tumors. And a clear history of colorectal cancer is an important clue for accurate diagnosis, which is extremely important for selecting an appropriate immunohistochemistry panel according reviewing literature. Some oncologic cases are difficult to diagnose because of the severe degree of de-differentiation of tumor cells. Thyroid transcription factor-1 (TTF-1) is expressed in both thyroid cancer and lung adenocarcinoma.Citation27 Molecular pathological analysis is required in complicated and poorly differentiated cases.
The stage of the primary tumor and the rate of spread of the primary tumor dissemination are key factors influencing diagnosis,Citation13 and identifying the origin of metastasis is important because the biological behavior of the primary tumor is believed to be more affected on survival compared with the surgery. According to the autopsy results, breast cancer, lung cancer, and malignant melanoma are the most common malignant tumors that metastasize to the thyroid with poor prognosis.Citation26 These metastases are clinically insidious and do not cause any symptoms. However, patients with primary renal cell tumors have the longest interval between the diagnosis of the primary tumor and thyroid metastasis, and they are more likely to undergo surgery for the primary tumor and thyroid metastasisCitation3 Patients with nodular thyroid lesions also have a better prognosis than those with thyroid infiltration.Citation24 MD Anderson Cancer Center’sCitation28 retrospective study on thyroid gland metastases showed that selective thyroidectomy for patients with metastatic thyroid cancer is safe and prolongs survival. In this case, the patients received excision of primary and metastases, pre-operation and post-operation chemotherapies, and targeted therapies, has a longer OS than mOS. Therefore, we believe that the significance of surgical treatment for prolonging survival of patients with thyroid gland metastases is based on multiple factors. It mainly depends on the isolation of thyroid metastasis and type of primary tumor.
The evaluation of microscopic histopathological samples is still the gold standard for tumor diagnosis, and accurate pathological reports are essential for selecting the best treatment plan and directly affect the survival time of patients. However, histopathological examination is a time-consuming process, thus leading to treatment delays. In addition, the process is subjective in nature, and the level of pathology experts is uneven, which directly affects the accuracy of pathology reports. In the past few years, artificial intelligence (AI) has steadily entered the fields of medicine and pathology. For faster and more accurate diagnosis, deep learning can assist in the pathological identification of tumors in a variety of ways. According to the literature, further investigation has been conducted into the potential clinical practice implementation of deep learning algorithms for the classification and diagnosis of CRC histopathology images. The advancement made possible by deep learning algorithms has the potential to improve CRC detection’s accuracy and efficacy.Citation29,Citation30
In the last few years, technological developments in the surgical field have been rapid and are continuously evolving. One of the most revolutionizing breakthroughs was the introduction of the “Internet of Things” (IoT) concept within surgical practice. IoT describes a network of Internet-based connected things equipped with sensing and actuating devices, with data production, processing, and consumption abilities. The application of IoT has been studied for remote guidance of surgery, remote monitoring of patients and visualization of surgery. Then this device can be used instead of colonoscopy for those who cannot undergo colonoscopy due to psychological and physical problems. The device can enter the intestine and transmit a series of information about the results, including images.Citation31 In this way, screening for colon cancer will be more convenient and acceptable
Conclusion
Due to regular follow-ups and improvement of diagnostic technology, more thyroid gland metastases can be diagnosed. Positron emission tomography (CT), FNAB, and IHC play important roles in diagnosis, especially in patients with a previous oncologic history. The thyroid is an important organ for colorectal cancer follow-up, and a sole thyroid mass may be a potential metastasis. Within the background of unchangeable biological characteristics and stage of the primary tumor, the early positive standardized treatment may prolong survival.
Abbreviations
CMT, colorectal metastasis to the thyroid; TTF1, thyroid transcription factor 1; TG, thyroglobulin; PET-CT, Positron Emission Tomography-Computed Tomography; CEA, carcinoembryonic antigen; IHC, Immunohistochemistry; IoT, Internet of Things.
Ethics Approval and Informed Consent
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study was approved by the Institutional Research Ethics Committee of the First Affiliated Hospital of the Anhui Medical University (Quick-PJ 2020-15-29). Written informed consent was obtained from all the patients.
Consent for Publication
Written informed consent for publication was obtained from the patient.
Author Contributions
Zhaorui Wang, Jingjing Wang, Jing Pei, Yubo Pan, Rui Ding made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas, and took part in drafting, revising or critically reviewing the article. All authors gave final approval of the version to be published, have agreed on the journal to which the article has been submitted, and agree to be accountable for all aspects of the work.
Disclosure
Dr Yubo Pan is now affiliated with Department of Gastrointestinal Surgery, Yixing People’s Hospital, Yixing, Jiangsu, China. The authors declare that they have no conflicts of interest in this work.
Data Sharing Statement
All data generated or analyzed during this study are included in this article.
Additional information
Funding
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. 2021;71(3):209–249. doi:10.3322/caac.21660
- Ciriano Hernandez P, Martinez Pinedo C, Calcerrada Alises E, et al. Colorectal cancer metastases to the thyroid gland: a case report. World J Gastrointest Surg. 2020;12(3):116–122. doi:10.4240/wjgs.v12.i3.116
- Wood K, Vini L, Harmer C. Metastases to the thyroid gland: the Royal Marsden experience. Eur J Surg Oncol. 2004;30(6):583–588. doi:10.1016/j.ejso.2004.03.012
- Keranmu A, Zheng H, Wu Y, et al. Comparative study of single-center patients with thyroid metastases from colorectal cancer and previously reported cases in the literature. World J Surg Oncol. 2017;15(1):88. doi:10.1186/s12957-017-1140-5
- Luo M, Huang Y, Li Y, Zhang Y. Metastatic rectal cancer to papillary thyroid carcinoma: a case report and review of literature. BMC Gastroenterol. 2020;20(1):136. doi:10.1186/s12876-020-01286-z
- Fujita T, Ogasawara Y, Doihara H, Shimizu N. Rectal adenocarcinoma metastatic to the thyroid gland. Int J Clin Oncol. 2004;9(6):515–519. doi:10.1007/s10147-004-0428-y
- Malani AK, Gupta C, Rangineni S, Gupta V. Thyroid metastasis from colorectal cancer: role of [18F]-fluoro-2-deoxy-D-glucose positron emission tomography. Clin Colorectal Cancer. 2005;5(4):287–291. doi:10.3816/CCC.2005.n.042
- Amante MA, Real IO, Bermudez G. Thyroid metastasis from rectal adenocarcinoma. BMJ Case Rep. 2018;2018:bcr–2018.
- Jin Y, Jiang Q, Li L, Zhao R, Xin T. Rectal cancer only metastasis to the thyroid which has a primary papillary thyroid cancer. Int J Colorectal Dis. 2014;29(6):769–770. doi:10.1007/s00384-014-1865-3
- Cheung WY, Brierley J, Mackay HJ. Treatment of rectal cancer metastases to the thyroid gland: report of two cases. Clin Colorectal Cancer. 2008;7(4):280–282. doi:10.3816/CCC.2008.n.036
- Cozzolino I, Malapelle U, Carlomagno C, Palombini L, Troncone G. Metastasis of colon cancer to the thyroid gland: a case diagnosed on fine-needle aspirate by a combined cytological, immunocytochemical, and molecular approach. Diagn Cytopathol. 2010;38(12):932–935. doi:10.1002/dc.21346
- Mori K, Koinuma K, Nishino H, Horie H, Lefor AK, Sata N. Rectal cancer with a metastasis to the thyroid gland: a case report. Int J Surg Case Rep. 2020;66:39–42. doi:10.1016/j.ijscr.2019.11.013
- Papi G, Fadda G, Corsello SM, et al. Metastases to the thyroid gland: prevalence, clinicopathological aspects and prognosis: a 10-year experience. Clin Endocrinol. 2007;66(4):565–571. doi:10.1111/j.1365-2265.2007.02773.x
- Goatman C, Goldsmith PJ, Antonopoulos V, Ali B. Metastasis of colorectal adenocarcinoma to the thyroid: a case report and review of the literature. Case Rep Surg. 2012;2012:1–3. doi:10.1155/2012/179407
- Onuigbo WIBJO. Batson’s theory of vertebral venous metastasis. Oncology. 1975;32(3–4):145–150.
- Lièvre A, Leboulleux S, Boige V, et al. Thyroid metastases from colorectal cancer: the Institut Gustave Roussy experience. Eur J Cancer. 2006;42(12):1756–1759. doi:10.1016/j.ejca.2005.11.042
- Durmo R, Albano D, Giubbini R. Thyroid metastasis from breast cancer detected by 18F-FDG PET/CT. Endocrine. 2019;64(2):424–425. doi:10.1007/s12020-019-01916-x
- Agrawal K, Weaver J, Mohan HK. Metastasis to the thyroid from non-small cell carcinoma of the lung: findings in (18)F-FDG PET/CT study. Endocrine. 2015;48(2):720–721. doi:10.1007/s12020-014-0297-8
- Czepczyński R, Stangierski A, Oleksa R, et al. Incidental F-FDG uptake in the thyroid in patients diagnosed with PET/CT for other malignancies. Nuclear Medicine Review. Central & Eastern Europe. 2011;14(2):68–72. doi:10.5603/nmr.2011.00018
- Millare GG, Kwon M, Edeiken-Monroe BS, Debnam JM. (18)F-PET/CT imaging of metastasis to the thyroid gland: imaging findings and effect on patient management. J Solid Tumors. 2017;7(2):7–13. doi:10.5430/jst.v7n2p7
- Medas F, Calò PG, Lai ML, Tuveri M, Nicolosi AMCR. Renal cell carcinoma metastasis to thyroid tumor: a case report and review of the literature. J Med Case Rep. 2013;7(1):1–5.
- Hegerova L, Griebeler ML, Reynolds JP, Henry MR, Gharib H. Metastasis to the thyroid gland: report of a large series from the Mayo Clinic. Am J Clin Oncol. 2015;38(4):338–342. doi:10.1097/COC.0b013e31829d1d09
- Kim TY, Kim WB, Gong G, Hong SJ, Shong YK. Metastasis to the thyroid diagnosed by fine-needle aspiration biopsy. Clin Endocrinol. 2005;62(2):236–241. doi:10.1111/j.1365-2265.2005.02206.x
- Mirallié E, Rigaud J, Mathonnet M, et al. Management and prognosis of metastases to the thyroid gland. J Am Coll Surg. 2005;200(2):203–207. doi:10.1016/j.jamcollsurg.2004.10.009
- Rottuntikarn W, Wangsiricharoen S, Rangdaeng S. Cytomorphology and immunocytochemistry of columnar cell variant of papillary thyroid carcinoma. Cytopathology. 2017;28(4):338–341. doi:10.1111/cyt.12429
- Guan H, Vandenbussche CJ, Erozan YS, et al. Can the tall cell variant of papillary thyroid carcinoma be distinguished from the conventional type in fine needle aspirates? A cytomorphologic study with assessment of diagnostic accuracy. Acta Cytol. 2013;57(5):534–542. doi:10.1159/000353823
- Matrone A, Torregrossa L, Sensi E, et al. The molecular signature more than the site of localization defines the origin of the malignancy. Front Oncol. 2019;9:1390. doi:10.3389/fonc.2019.01390
- Romero Arenas MA, Ryu H, Lee S, et al. The role of thyroidectomy in metastatic disease to the thyroid gland. Ann Surg Oncol. 2014;21(2):434–439. doi:10.1245/s10434-013-3282-1
- Bousis D, Verras GI, Bouchagier K, et al. The role of deep learning in diagnosing colorectal cancer. Prz Gastroenterol. 2023;18(3):266–273. doi:10.5114/pg.2023.129494
- Chlorogiannis DD, Verras GI, Tzelepi V, et al. Tissue classification and diagnosis of colorectal cancer histopathology images using deep learning algorithms. Is the time ripe for clinical practice implementation? Prz Gastroenterol. 2023;18(4):353–367. doi:10.5114/pg.2023.130337
- Mulita F, Verras GI, Anagnostopoulos CN, Kotis K. A smarter health through the internet of surgical things. Sensors. 2022;22(12):4577. doi:10.3390/s22124577