Abstract
Background
The association between occupational exposure and COPD reported previously has mostly been derived from studies relying on self-reported exposure to vapors, gases, dust, or fumes (VGDF), which could be subjective and prone to biases. The aim of this study was to assess the strength of association between exposure and COPD from studies that derived exposure by job exposure matrices (JEMs).
Methods
A systematic search of JEM-based occupational COPD studies published between 1980 and 2015 was conducted in PubMed and EMBASE, followed by meta-analysis. Meta-analysis was performed using a random-effects model, with results presented as a pooled effect estimate with 95% confidence intervals (CIs). The quality of study (risk of bias and confounding) was assessed by 13 RTI questionnaires. Heterogeneity between studies and its possible sources were assessed by Egger test and meta-regression, respectively.
Results
In all, 61 studies were identified and 29 were included in the meta-analysis. Based on JEM-based studies, there was 22% (pooled odds ratio =1.22; 95% CI 1.18–1.27) increased risk of COPD among those exposed to airborne pollutants arising from occupation. Comparatively, higher risk estimates were obtained for general populations JEMs (based on expert consensus) than workplace-based JEM were derived using measured exposure data (1.26; 1.20–1.33 vs 1.14; 1.10–1.19). Higher risk estimates were also obtained for self-reported exposure to VGDF than JEMs-based exposure to VGDF (1.91; 1.72–2.13 vs 1.10; 1.06–1.24). Dusts, particularly biological dusts (1.33; 1.17–1.51), had the highest risk estimates for COPD. Although the majority of occupational COPD studies focus on dusty environments, no difference in risk estimates was found for the common forms of occupational airborne pollutants.
Conclusion
Our findings highlight the need to interpret previous studies with caution as self-reported exposure to VGDF may have overestimated the risk of occupational COPD.
Introduction
The importance of occupational exposure as a cause of COPD has been recognized for decades.Citation1–Citation3 A recent systematic review concluded that there is strong and consistent evidence to support a causal association between occupational exposure(s) and COPD.Citation4 Recent reviews have identified associations between a few specific occupational pollutants, mainly dusts (silica, wood, coal, cotton, and grain) and fumes (rubber, welding, and cadmium), and the development of COPD.Citation4,Citation5 However, there is still an ongoing debate on the relative importance of the different occupational pollutants forms (vapors, gases, dusts, fumes, fibers, and mists) to which individuals may be exposed at work; this information would be valuable when identifying suitable workplace interventions and when planning adjustments at work for individuals either at risk of developing work-related COPD or when improving work ability in individuals with COPD.
The assessment of occupational exposure requires collection of personal exposure data, which are often not available and, where present, are usually limited to a few industries and substances. In the absence of measured exposure data, epidemiological studies have relied on self-reported exposure (questionnaires) to either specific substancesCitation6–Citation8 or a combination of airborne substances, typically vapors, gases, dusts, or fumes (VGDF),Citation9–Citation11 which could be prone to recall bias.
Over the past two decades, job exposure matrices (JEMs) have been increasingly used to estimate occupational exposures, particularly in large-scale epidemiological studies, as they are relatively easy to use and are economic. The majority of JEMs are based on general populationCitation12,Citation13 and rely on expert knowledge of industries, work environments, and determinants of occupational exposure to assign exposures to a standard job classification coding system. A few work-based JEMs have also been developed, which make use of actual measured data (current or historical) from particular work sites for the population of interest.Citation14,Citation15 Regardless of JEM types their use has allowed the assignation of exposure to specific substances as well as the full range of individual pollutant forms (vapors, gases, dusts, fumes, fibers, and mists) found in occupational settings.
This systematic review of JEM-based studies on occupational COPD aims to address the following questions:
Do different JEM types (based on general population and workplace) provide similar risk estimates for different pollutant forms including the common aggregate VGDF?
Are pollutant forms such as gases, vapors, fumes, and fibers as important as dusts in the development of occupational COPD?
Is the strength of association between different COPD phenotypes and occupational airborne pollutants consistent in JEM-based studies?
Methods
Study eligibility criteria, search strategy, and terms
We carried out a systematic review and meta-analysis of peer-reviewed articles that used JEMs to assign exposures to jobs for investigating the association between occupational exposure and COPD phenotypes. The systematic review was conducted adhering to the Preferred Reporting Items of Systematic reviews and Meta-Analysis guidelines.Citation16
Papers published from January 1, 1980, to December 13, 2015, were identified through a systematic literature search in PubMed and EMBASE. Search terms used for the initial search are shown in Table S1. Bibliographies of peer-reviewed publications on the subject were also screened to ensure that no relevant papers have been missed during our original searches.
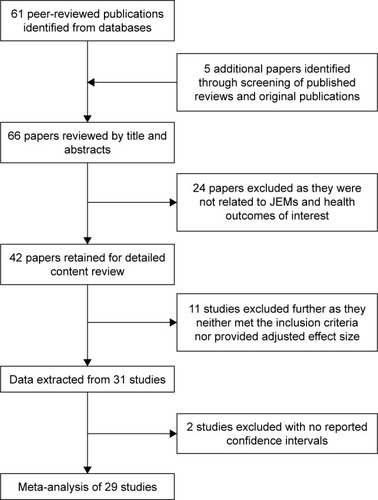
We used a multistage iterative process to reduce the initial search pool of citations down to a final selection as shown in . OPK and SS initially screened the titles and abstracts of all publications identified. The search was limited to human studies and English language. We included studies on adults that used a JEM to assign exposure to jobs with respiratory outcomes (COPD, chronic bronchitis, and breathlessness) only. We applied a broad definition of COPD (diagnosed by either a physician or on the basis of spirometry) and chronic bronchitis (those diagnosed by physician or those who completed Medical Research Council questionnaires on chronic bronchitis). The definitions used are shown in Table S2 for each study. Studies on environmental (outdoor or domestic) exposure were excluded unless the exposure occurred as part of an occupation, such as in traffic wardens or car park attendants. Following studies were excluded: 1) studies on respiratory health effects due to smoking unless they are related to the workplace, for example bar staff, and 2) studies on respiratory health effects from household air pollution, for example burning of solid fuel. Case reports and articles not related to occupation and the prespecified respiratory outcomes were also excluded.
Data extraction and quality assessment
Information from selected publications were extracted independently by two reviewers SS and SSS using a predefined template on the following: gender, study population (general population or workplace based), study design, types of occupational airborne pollutants (specific substances), formulations (paints and adhesives) and the six broader forms of pollutants (vapors, gases, dusts, fumes, fibers, and mists), JEM type (whether based on general population or workplace), level of exposures assigned by the JEM (low, medium, or high), confounder(s) adjusted for, respiratory outcomes, and risk estimates. Publication(s) with any disagreement in data extraction was further reviewed by OPK. Data on effect size and 95% confidence intervals (CIs) both before and after adjustment for confounders were extracted, but only those data sets that adjusted for confounders including smoking were used in the meta-analysis.
For studies conducted in the workplace, it was noted whether workplace-measured exposure data were used to inform the development of the JEM. All exposure estimates derived using a specified expert JEM were labeled as JEM based. Risk estimates for self-reported exposures were also recorded (where available) in the selected JEM-based studies.
The majority of JEMs provided respiratory risk estimates for one of the six broad forms of pollutants: vapors, gases, dusts, fumes, fibers, or mists, or the aggregate VGDF (exposed to one of the four pollutant forms). In cases where JEMs provided risk estimates for specific airborne chemical/materials, those were allocated by SS and OPK to one of the six broad forms of pollutants. For example, JEM-based risk estimates for paints, cement, and asbestos were classified as exposed to vapors, dusts, and fibers, respectively.
For each of the exposure estimates, information was also collated on whether the assigned exposure was for the current job, longest-held job, or an estimate of cumulative lifetime exposure, and where specified the level of exposure (low, medium, high) was also recorded. Of the different JEM types, the ALOHA JEM has been commonly used to investigate occupational COPD in particular for exposures to mineral dusts, biological dusts, and gases/fume.Citation13
The quality of each selected study was assessed independently by two authors (KBHL and OPK) using the RTI Item Bank for Assessing Risk of Bias and Confounding for Observational Studies of Interventions or Exposures,Citation17 with 13 questions covering 6 domains (selection bias, detection bias, performance bias, attrition bias, selective outcome reporting, and confounding) and an overall assessment. Responses to these RTI items consist of “yes” and “no”, plus a combination of “partially”, “cannot determine”, and “not applicable”. We recategorized those responses that reflected high quality as conveying a low-risk bias, low quality as high-risk bias, and “cannot determine” and “partially” as “unclear risk of bias”, similar to that reported by Margulis et al.Citation18
Statistical analysis
All eligible studies were pooled, and sensitivity analysis was conducted to assess the impact of methodological approaches (study design, study population, JEM types, exposure to VGDF [self-reported and JEM based], exposure to different individual pollutant forms, and exposure duration estimates [current job and cumulative]) by grouping them into different subgroups.Citation19 We used natural logarithms of odds ratio (OR) and the associated standard errors to estimate the pooled effect size of all studies and the subgroups. Within-group heterogeneity was assessed using Q-tests and/or I2 statistics.Citation20 As there was huge heterogeneity among studies, we used random-effects model to calculate the pooled effect estimates. We assessed publication bias by funnel plots and Egger regression.Citation21 Meta-regression was used to explore the sources of heterogeneity, including gender, study design, JEM types, exposure period, and pollutant forms. All analyses were performed using STATA (version 13; STATA, College Station, TX, USA).
Results
Study selection
A total of 61 articles were identified from the initial search and an additional 5 articles identified from screening the reference lists of previously published studies. Of them, 24 were excluded from further review as they were either not related to respiratory outcomes of interest or did not use a JEM to assign occupational exposures (). Detailed data for the 42 studies were extracted (Table S2).
Study characteristics
Of the 42 studies reviewed, 14 used JEMs that were developed using measured exposure data and applied to a specific occupational group or industry particularly of silica carbide workers,Citation15,Citation22 cement production plant workers,Citation23 smelters,Citation24–Citation26 woodworkers,Citation14,Citation27 and construction workers.Citation7,Citation28,Citation29 Most of these JEMs were based on personal measured data and each current/former employee was assigned an exposure level by the study authors. The remaining 28 studies used general population–based expert JEMs to assign exposures to recorded jobs, the most commonly used JEM being the ALOHA JEM that was applied in 12 of the 42 studies. The other general population JEMs used by researchers were the Blanc JEM,Citation10,Citation11,Citation30,Citation31 the NIOSH JEM,Citation9,Citation32 and the MRC JEM.Citation33–Citation35
We included 29 studies for meta-analysis; 13 were excluded which either did not meet the inclusion criteria or did not provide adjusted effect size estimates for meta-analysis. Most of the studies had low risk of bias across the domains (), although high risk of bias was noted in confounding studies, particularly in studies without adjustment for environmental tobacco smoke, and an unclear risk of detection bias was noted in the studies that did not clearly state if assessment of exposure was blinded where possible.
Table 1 Results of quality assessment of the 29 studies included in the meta-analysis
A range of outcomes were reported in these 29 studies, including shortness of breath (n=5), chronic bronchitis (n=15), COPD diagnosed by physician (n=10), and spirometry-defined COPD (n=17). Altogether these papers provided 575 individual risk estimates for one of the following pollutant forms: vapors, gases, dusts, fumes, fibers, and VGDF. Dust was the most commonly reported form of pollutant (n=312), followed by fumes (n=133), with fibers and fumes being least common (n<20). In addition, nine studies included risk estimates for self-reported exposures to VGDF.
Meta-analysis, risk estimates, and heterogeneity
The main results are shown in . Overall, there was little but significant heterogeneity among the studies (I2=46.8%, P<0.001), reducing only slightly (to 39.6%) when restricted to studies that defined COPD by spirometry. The pooled risk estimate was significantly higher (P<0.001) among the studies that used self-reported physician diagnosis (1.36; 95% CI 1.26–1.47) compared to those that defined COPD by spirometry (1.16; 1.12–1.20), giving an overall 22% increase in odds (95% CI 18%–27%) across all studies. Females tended to have higher COPD risk than males, and likewise for general population–based studies (vs workplace) and case–control studies (vs other designs). We also observed a 28% higher risk for occupational exposures based on current/longest-held job compared to cumulative historical exposure (19%). Higher risk estimates were reported in studies that used expert general population JEMs (1.26; 1.20–1.33) compared to work-based JEMs (1.14; 1.10–1.19) derived using measured exposure data.
Table 2 Occupational exposure and COPD from JEM-based studies
JEM-based studies provided more modest risk estimate (1.10; 1.06–1.24) compared to those with self-reported VGDF exposure (1.91; 1.72–2.13). Exposure levels among JEM-based studies showed a dose–response effect. As for the individual pollutants forms, no material difference was found for VGDF. Biological dusts (1.33; 1.17–1.51) produced higher risk estimates than mineral dusts (1.07; 1.05–1.09; ).
Substantial heterogeneity was observed in studies reporting chronic bronchitis as an outcome, but not for breathlessness (). Similar to COPD, the pooled effect size for breathlessness and chronic bronchitis was higher among those with current/longest-held job compared to cumulative historical exposure. Risk estimates from JEM-based studies were also attenuated compared to those using self-reported exposures. Similarly, there was no significant difference in terms of the magnitude of association across different forms of pollutants. However, studies using workplace-based JEMs gave a higher pooled effect estimate (1.73; 1.37–2.19) for chronic bronchitis compared to those that used JEMs for the community (1.29; 1.23–1.35).
Table 3 Occupational exposure and respiratory symptoms and chronic bronchitis from JEM-based studies
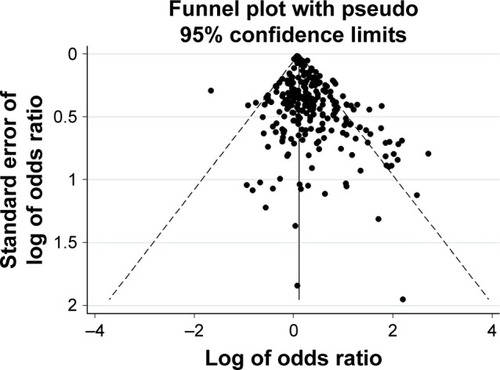
Funnel plots and Egger tests showed some evidence of publication bias for studies with self-reported physician-diagnosed COPD (bias =0.64, P<0.001), chronic bronchitis (bias =0.36, P=0.022), spirometry-diagnosed COPD (bias =0.50, P<0.001; ), and combined COPD (bias =0.63, P<0.001; ) as outcomes. However, the plots suggested no publication bias for breathlessness (bias =0.37, P=0.135).
Figure 2 Funnel plot of studies reporting COPD (diagnosed by spirometry) associated with exposure to occupational airborne pollutants.
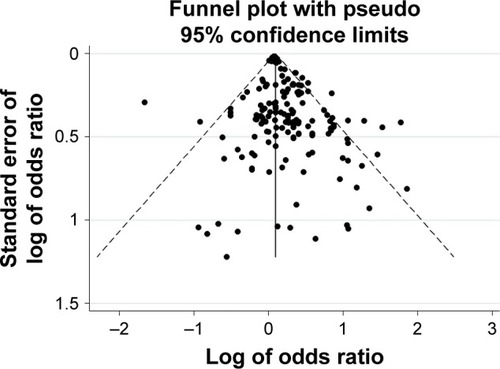
Figure 3 Funnel plot of studies reporting COPD (diagnosed by spirometry or physician) associated with exposure to occupational airborne pollutants.
We further assessed the contribution of various factors () toward heterogeneity by meta-regression. For studies reporting self-reported physician diagnosis of COPD, the factors contributing to heterogeneity were gender (coefficient =−0.102, P=0.046), publication year (−0.040, P<0.001), and JEM types (0.093, P=0.053) as was study population (0.256, P=0.002) and JEM types (0.256, P=0.002) for chronic bronchitis. None of the examined factors significantly contributed toward the heterogeneity for COPD defined by spirometry criteria or for shortness of breath.
Discussion
To our knowledge, this is the first systematic review and meta-analysis of peer-reviewed studies that have used different population JEMs to assess the association between the types of occupational airborne pollutants and COPD phenotypes. Overall occupational exposure to airborne pollutants as assessed by JEMs showed a 22% increased risk of COPD (diagnosed by physician or based on spirometry), which was lower compared to the risk estimate obtained by self-reported exposures. Although there was no significant difference in COPD risk estimates for individual forms of pollutants such as vapors, gases, dusts, and fumes, exposure to biological dusts appeared to confer a higher risk than that to mineral dusts.
Occupational exposure has been shown to be associated with COPD,Citation1–Citation4 but information on the role of different airborne pollutants is limited to few specific substances and industries. This may be partly due to the absence of reliable measured personal exposure data and has been addressed (over the past two decades) by the development and application of JEMs to assign occupational exposures in COPD epidemiological studies. Nevertheless, the majority of studies on occupational COPD to date have focused mainly on exposure to dusts and fumes with little information on other forms of airborne pollutants such as gases, vapors, fibers, and mists to which individuals may be exposed either alone or more commonly in combination with other pollutant forms.
General population–based studies often include the following question: In this job, are you exposed to VGDF?; similarly, general population–based JEMs developed by experts assign exposure to VGDF to different job types or standardized international job codes. In this pooled analysis, the risk for self-reported exposure to VGDF was 80% higher compared to that estimated by expert general population–based JEMs. This overestimation in self-reported exposures to VGDF may be due to misinterpretation by study respondents as being exposed to any chemical substance at work, by all routes such as by dermal and inhalation routes. The analysis of the JEM types also shows that JEMs derived using measured exposure data produced more modest estimates (1.14; 1.10–1.19) for occupational COPD compared with the general population–based JEMs (1.26; 1.20–1.33), which are based on expert knowledge, experience, and consensus. A recent review and meta-analysis of population-based studies which was limited to studies using the ALOHA JEM reported that low exposure to mineral dust had 17% increased risk of lung function defined COPD but surprisingly no association with high exposure to mineral dust.Citation36 Although measured exposure data are only available in a limited number of COPD epidemiological studies, this finding further supports the need for reliable industry-based exposure estimates and the need to validate expert-derived JEMs against measured data.
Although majority of substances reported in the literature to be associated with occupational COPD are mainly dusts (silica, metals, wood, and coal) and fumes (diesel), such as particulates, surprisingly we found no major difference when comparing risk estimates for different pollutant forms. This may be because of a lack of power, reflected by the fact that the majority (71%) of risk estimates for COPD from JEM studies were for dust or fumes, 26% of estimates were for gases and vapors, and only a few for fibers and mists. It is also important to note that the majority of individuals in industrial workplaces are exposed to a combination of pollutants rather than a single substance. For instance, a welder is exposed to metal fumes as well as inorganic gases (eg, ozone) and a carpenter may be exposed to organic solvents (adhesives and paints) as well as wood dust. It is thus important that future COPD JEM studies report and investigate the range and combination of pollutants to which individuals may be exposed over their typical work shift as well as common pollutants associated with their job. Little is known about the importance of the interaction of different forms of pollutants in occupational COPD, which was not possible to be investigated in this study.
Of the different pollutants, dusts appeared to be the most important. A number of JEM studies in particular those that used the ALOHA JEM have provided risk estimates for both mineral and biological dusts. Overall (for all population JEMs), biological dusts produced higher risk estimates for COPD compared with mineral dusts (metals, silica, and cement). This finding is contrast to the findings of Alif et al,Citation36 which did not find any association for the ALOHA JEM-based studies. JEM studies other than those using the ALOH JEM tend to provide risk estimates for all dusts ie do not differentiate between dust types or include organic dusts within the definition of biological dusts. The role and mechanism of biological dusts in COPD warrants further investigation.
For chronic occupational diseases such as COPD, estimation of cumulative occupational exposures would seem logical, but most of the JEMs assessed exposure for the current or longest-held job and few studies provided estimates for cumulative exposures. Nevertheless, cumulative exposure estimates are only possible where historical measurements of exposure is available for defined occupational groups or where JEMs take account of different exposures over decades. This presents a challenge for future studies on occupational COPD.
Although this review attempts to capture all relevant information on occupational exposures and COPD from reported JEM studies, there is considerable variability between studies as demonstrated by the heterogeneity for both exposure and different definitions of COPD. This variability is expected as all studies included in the meta-analysis are observational by design due to the chronic nature of COPD and the fact that majority of the studies attempt to estimate past occupational exposures and investigate associations between exposures and chronic effect. In the absence of randomized controlled trials for meta-analysis, it is important to assess and understand possible sources of heterogeneity. The exposure heterogeneity may be explained by different definitions and guidelines used by experts when developing general population JEMs that are often not explained in detail. For instance, only limited information is often available on how exposed groups are defined and factors used in assigning the levels of exposure (low, medium, high). It is also important to note that when risk of exposure is assessed to a particular pollutant, for example dusts, the reference category is usually defined as nonexposed to dusts but these individuals may be exposed to other different combination of airborne pollutants such as gases, vapors, and mists. In the case of workplace-based JEMs, exposed and nonexposed, are usually well defined, but the reference group may vary between studies which may affect the risk estimates. For COPD outcomes, large variation exists depending on the definition (diagnosed by doctor, symptoms, based on spirometry and mortality); however, in case of spirometry, majority (70%) of studies stated use of post-bronchodilators or followed the American Thoracic Society or European Respiratory Society spirometry guidelines. A further source of heterogeneity that is to be introduced in this review is the use of ORs rather than true relative risk, that is, the size of the effect may be overestimated when prevalence is high. However, majority of studies cited in this review were case–control or cross-sectional studies for which the common measure of effect size was OR. A further limitation of this review is that the COPD risk estimates for self-reported exposures were limited to those reported only in JEM-based studies, that is, occupational COPD studies that did not use JEMs but provided risk estimates based on self-reported occupational exposures were not included in this review. Majority of the above limitations are a consequence of meta-analysis of observational studies, that is combining diverse study designs and populations and calculating of single summary estimates of exposure which needs to be interpreted cautiously.
In summary, this review shows that while the majority of studies on occupational COPD focus on dusty environments, no difference in risk estimates was found for the common forms of occupational airborne pollutants such as vapors, gases, dusts, and fumes. However, biological dusts were associated with higher risks of occupational COPD than mineral dusts. The review also shows that self-reported exposure to VGDF provides higher risk estimates for occupational COPD compared to exposure assigned using JEMs.
Author contributions
Conception: SS, OPK, JGA; study design: all authors; data collection: SS, OPK, SSS; analysis and interpretation: all authors; writing of manuscript, revisions, and approval: all authors.
Acknowledgments
The authors thank Dr Nuredin Mohamed for updating the literature searches. This study was funded by the University of Birmingham, UK.
Disclosure
None of the authors has a financial relationship with a commercial entity that has interest in the subject of this manuscript. The authors report no conflicts of interest in this work.
References
- BecklakeMRChronic airflow limitation: its relationship to work in dusty occupationsChest19858846086173899533
- BalmesJBecklakeMBlancPAmerican Thoracic Society Statement: occupational contribution to the burden of airway diseaseAm J Respir Crit Care Med2003167578779712598220
- EisnerMDAnthonisenNCoultasDAn official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2010182569371820802169
- OmlandOWurtzETAasenTBOccupational chronic obstructive pulmonary disease: a systematic literature reviewScand J Work Environ Health2014401193524220056
- CullinanPOccupation and chronic obstructive pulmonary disease (COPD)Br Med Bull201210414316123080418
- HansellAGhoshREPooleSOccupational risk factors for chronic respiratory disease in a New Zealand population using lifetime occupational historyJ Occup Environ Med201456327028024327054
- AlbinMEngholmGHallinNHaqmarLImpact of exposure to insulation wool on lung function and cough in Swedish construction workersOccup Environ Med199855106616679930086
- PostWKHeederikDKromhoutHKromhoutDOccupational exposures estimated by a population specific job exposure matrix and 25 year incidence rate of chronic nonspecific lung disease (CNSLD): the Zutphen StudyEur Respir J199476104810557925872
- DoneyBHnizdoEGrazianiMOccupational risk factors for COPD phenotypes in the Multi-Ethnic Study of Atherosclerosis (MESA) Lung StudyCOPD201411436838024568208
- DarbyACWaterhouseJCStevensVChronic obstructive pulmonary disease among residents of an historically industrialised areaThorax2012671090190722744883
- TrupinLEarnestGSan PedroMThe occupational burden of chronic obstructive pulmonary diseaseEur Respir J200322346246914516136
- PannettBCoggonDAchesonEDA job-exposure matrix for use in population based studies in England and WalesBr J Ind Med198542117777834063222
- SunyerJKogevinasMKromhoutHPulmonary ventilatory defects and occupational exposures in a population-based study in Spain. Spanish Group of the European Community Respiratory Health SurveyAm J Respir Crit Care Med199815725125179476866
- JacobsenGSchlunssenVSchaumburgISiqsqaardTIncreased incidence of respiratory symptoms among female woodworkers exposed to dry woodEur Respir J20093361268127619483046
- JohnsenHLBuggeMDForelandSKjuusHKongerudJSøysethVDust exposure is associated with increased lung function loss among workers in the Norwegian silicon carbide industryOccup Environ Med2013701180380923852098
- LiberatiAAltmanDGTetzlaffJThe PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaborationJ Clin Epidemiol20096210e1e3419631507
- ViswanathanMBerkmanNDDrydenDMHartlingLAHRQ Methods for Effective Health Care Assessing Risk of Bias and Confounding in Observational Studies of Interventions or Exposures: Further Development of the RTI Item BankRockville, MDAgency for Healthcare Research and Quality (US)2013
- MargulisAVPladevallMRiera-GuardiaNQuality assessment of observational studies in a drug-safety systematic review, comparison of two tools: the Newcastle-Ottawa Scale and the RTI item bankClin Epidemiol2014635936825336990
- KurmiOPSempleSSimkhadaPSmithWCAyresJGCOPD and chronic bronchitis risk of indoor air pollution from solid fuel: a systematic review and meta-analysisThorax201065322122820335290
- HigginsJPThompsonSGDeeksJJAltmanDGMeasuring inconsistency in meta-analysesBMJ2003327741455756012958120
- BorensteinMHedgesLVHigginsJPTRothsteinHRIntroduction to Meta-AnalysisChichester, UKWiley2009
- BuggeMDForelandSKjaerheimKEduardWMartinsenJIKjuusHMortality from non-malignant respiratory diseases among workers in the Norwegian silicon carbide industry: associations with dust exposureOccup Environ Med2011681286386921364203
- NordbyKCFellAKNotoHExposure to thoracic dust, airway symptoms and lung function in cement production workersEur Respir J20113861278128621659410
- SoysethVJohnsenHLBuggeMDHetlandSMKongerudJPrevalence of airflow limitation among employees in Norwegian smelters: a longitudinal studyOccup Environ Med2011681242920798007
- FritschiLSimMRForbesARespiratory symptoms and lung-function changes with exposure to five substances in aluminium smeltersInt Arch Occup Environ Health200376210311012733082
- JohnsenHLHetlandSMBenthJSKongerudJSøysethVDust exposure assessed by a job exposure matrix is associated with increased annual decline in FEV1: a 5-year prospective study of employees in Norwegian smeltersAm J Respir Crit Care Med2010181111234124020203247
- JacobsenGSchlunssenVSchaumburgITaudorfESigsgaardTLongitudinal lung function decline and wood dust exposure in the furniture industryEur Respir J200831233434217989115
- BergdahlIATorenKErikssonKIncreased mortality in COPD among construction workers exposed to inorganic dustEur Respir J200423340240615065829
- BurkhartGSchultePARobinsonCSieberWKVossenasPRingenKJob tasks, potential exposures, and health risks of laborers employed in the construction industryAm J Ind Med19932444134258250061
- BlancPDEisnerMDEarnestGFurther exploration of the links between occupational exposure and chronic obstructive pulmonary diseaseJ Occup Environ Med200951780481019528835
- BlancPDIribarrenCTrupinLOccupational exposures and the risk of COPD: dusty trades revisitedThorax200964161218678700
- WeinmannSVollmerWMBreenVCOPD and occupational exposures: a case–control studyJ Occup Environ Med200850556156918469625
- HsairiMKauffmannFChavanceMBrochardPPersonal factors related to the perception of occupational exposure: an application of a job exposure matrixInt J Epidemiol19922159729801468862
- HeederikDPouwelsHKromhoutHKromhoutDChronic non-specific lung disease and occupational exposures estimated by means of a job exposure matrix: the Zutphen StudyInt J Epidemiol19891823823892767852
- HeederikDKromhoutHBuremaJKromhoutDOccupational exposure and 25-year incidence rate of non-specific lung disease: the Zutphen StudyInt J Epidemiol19901949459522084026
- AlifSMDharmageSCBowatteGOccupational exposure and risk of chronic obstructive pulmonary disease: a systematic review and meta-analysisExpert Rev Respir Med201610886187227187563
- PaulinLMDietteGBBlancPDOccupational exposures are associated with worse morbidity in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2015191555756525562375
- TorenKJarvholmBEffect of occupational exposure to vapors, gases, dusts, and fumes on COPD mortality risk among Swedish construction workers: a longitudinal cohort studyChest2014145599299724264472
- DijkstraAEde JongKBoezenHMRisk factors for chronic mucus hypersecretion in individuals with and without COPD: influence of smoking and job exposure on CMHOccup Environ Med201471534635224642640
- RodriguezEFerrerJZockJPLifetime occupational exposure to dusts, gases and fumes is associated with bronchitis symptoms and higher diffusion capacity in COPD patientsPLoS One201492e8842624516659
- PallasahoPKainuASovijarviALindqvistAPiiriläPLCombined effect of smoking and occupational exposure to dusts, gases or fumes on the incidence of COPDCOPD2014111889524111617
- MehtaAJMiedingerDKeidelDOccupational exposure to dusts, gases, and fumes and incidence of chronic obstructive pulmonary disease in the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in AdultsAm J Respir Crit Care Med2012185121292130022492989
- GovenderNLallooUGNaidooRNOccupational exposures and chronic obstructive pulmonary disease: a hospital based case–control studyThorax201166759760121502099
- SkorgeTDEaganTMEideGEGulsvikABakkePSOccupational exposure and incidence of respiratory disorders in a general populationScand J Work Environ Health200935645446119806271
- RodriguezEFerrerJMartiSZockJ-PPlanaEMorellFImpact of occupational exposure on severity of COPDChest200813461237124318689596
- MathesonMCBenkeGRavenJBiological dust exposure in the workplace is a risk factor for chronic obstructive pulmonary diseaseThorax200560864565116061705
- SunyerJZockJPKromhoutHLung function decline, chronic bronchitis, and occupational exposures in young adultsAm J Respir Crit Care Med200517291139114516040784
- de MeerGKerkhofMKromhoutHSchoutenJPHeederikDInteraction of atopy and smoking on respiratory effects of occupational dust exposure: a general population-based studyEnviron Health200431615175108
- MastrangeloGTartariMFedeliUFaddaESaiaBAscertaining the risk of chronic obstructive pulmonary disease in relation to occupation using a case–control designOccup Med (Lond)200353316517212724550
- ZockJPSunyerJKogevinasMKromhoutHBurneyPAntóJMOccupation, chronic bronchitis, and lung function in young adults. An international studyAm J Respir Crit Care Med200116371572157711401876
- BakkePSBasteVHanoaRGulsvikAPrevalence of obstructive lung disease in a general population: relation to occupational title and exposure to some airborne agentsThorax199146128638701792631