Abstract
Background
Exacerbation history is used to grade the risk of COPD exacerbation, but its reliability and relationship to other risk factors and prior therapy is unclear. To examine these interrelationships, we conducted a post hoc analysis of patients in the TIOSPIR trial with ≥2 years’ follow-up or who died on treatment.
Patients and methods
Patients were grouped by their annual exacerbation rate on treatment into nonexacerbators, infrequent, and frequent exacerbators (annual exacerbation rates 0, ≤1, and >1, respectively), and baseline characteristics discriminating among the groups were determined. We used univariate and multivariate analyses to explore the effect of baseline characteristics on risk of exacerbation, hospitalization (severe exacerbation), and death (all causes).
Results
Of 13,591 patients, 6,559 (48.3%) were nonexacerbators, 4,568 (33.6%) were infrequent exacerbators, and 2,464 (18.1%) were frequent exacerbators; 45% of patients without exacerbations in the previous year exacerbated on treatment. Multivariate analysis identified baseline pulmonary maintenance medication as a predictive factor of increased exacerbation risk, with inhaled corticosteroid treatment associated with increased exacerbation risk irrespective of exacerbation history.
Conclusion
Our data confirm established risk factors for exacerbation, but highlight the limitations of exacerbation history when categorizing patients and the importance of prior treatment when identifying exacerbation risk.
Keywords:
Plain-language summary
Patients with COPD may experience times when symptoms suddenly get worse, known as exacerbations. These events contribute to progression of the disease, and make patients feel worse. People who have had a lot of exacerbations in the past are most at risk of having more exacerbations. In this study, researchers looked at what factors other than the number of past exacerbations might predict which patients are most likely to have an exacerbation. The researchers used results from a clinical trial that included more than 17,000 patients with COPD who were followed for 2–3 years. The results showed that in addition to history of exacerbation, the medications that patients were prescribed before they entered the trial also predicted how likely they were to have an exacerbation. This is probably because patients who are not doing well and most at risk of having an exacerbation are more likely to be prescribed certain medications. Overall, this study confirms that patients who have had more exacerbations in the past are at greater risk of exacerbations in the future, and shows that patients who require more medications for their COPD are at higher risk of exacerbations.
Introduction
Exacerbations of symptoms sufficient to warrant treatment with antibiotics and/or systemic corticosteroids (CSs) and/or hospitalization contribute to health-status impairment and disease progression in patients with COPD.Citation1,Citation2 Multiple reports in different COPD populations have found that exacerbations are more likely if the patient reports previous events, is more breathless, and has poor lung function,Citation3–Citation5 although the importance of a history of chronic bronchitis as a predictor of exacerbations is less clear.Citation5,Citation6 The data identifying these risk factors for exacerbations derive largely from observational cohorts or database studies where treatment choices reflect routine clinical practice.
To date, relatively little attention has been paid to the relationship of baseline treatment to the risk of subsequent exacerbation of COPD. Extensive randomized controlled trial data show that inhaled long-acting muscarinic antagonists (LAMAs), long-acting β2-agonists (LABAs), and LABA–inhaled CS (ICS) combinations reduce the risk of exacerbations.Citation7–Citation9 Further studies have shown that LAMAs are more likely to be effective than LABAs in preventing exacerbation, irrespective of whether LABA is administered once dailyCitation10 or twice daily.Citation11 Whether the same risk factors operate when all patients are treated with these drugs is not yet clear. Moreover, it is not known whether treatment intensity, which is often used as a surrogate for disease severity in patients with asthma,Citation12 is a marker of disease severity in COPD.
To address these problems, we examined data from the TIOSPIR trial,Citation13,Citation14 the largest long-term, randomized, double-blind, double-dummy, parallel-group trial in patients with COPD performed to date. We wished to establish whether use of LABAs and ICSs could be used as a surrogate marker for increased exacerbation risk in patients with COPD treated with tiotropium. We also sought to examine whether clinical and demographic variables that have been shown to be risk factors for exacerbations would pertain to a large international COPD population using tiotropium maintenance therapy.
Patients and methods
Study design
In TIOSPIR, 17,135 patients with COPD were randomized and treated in a double-blind, parallel-group, event-driven trial with follow-up of 2–3 years. Patients were randomized to once-daily tiotropium Respimat 5 or 2.5 μg, or once-daily tiotropium HandiHaler 18 μg (both Boehringer Ingelheim, Ingelheim am Rhein, Germany). The trial design and methodology have been published previously.Citation13 TIOSPIR was performed in accordance with the provisions of the Declaration of Helsinki, and the study protocol and procedures were approved by relevant institutional review boards and ethics committees (independent ethics committee Johns Hopkins Medicine Institutional Review Board, Baltimore, MD, USA). All the patients provided written informed consent.
Study population
All participants had a diagnosis of COPD with a postbronchodilator forced expiratory volume in 1 second (FEV1) ≤70% predicted, an FEV1:forced vital capacity (FVC) ratio ≤0.7, were aged ≥40 years, had been clinically stable for at least 6 weeks, and had ≥10 pack-years of smoking history. Patients with concomitant cardiac disease were included, unless they had a recent history of myocardial infarction, cardiac arrhythmia, or hospitalization for heart failure. Patients were excluded if they had a history of significant respiratory diseases other than COPD, including asthma.
Assessments
The study period was dependent on the number of fatal events observed (event-driven trial). Visits occurred at weeks 0, 6, and 12, and then every 12 weeks for the duration of the trial. At the first visit, concomitant medication use and medical history were noted, as was exacerbation history. Hospitalization due to COPD in the year prior to enrolment was not collected. At all visits, information about exacerbations and their treatment, including the need for hospitalization, were recorded. Vital status during the trial period was obtained in 99.7% of participants. Causes of death were adjudicated by an independent mortality adjudication committee.
COPD exacerbations were defined as a worsening of two or more major respiratory symptoms (dyspnea, cough, sputum, chest tightness, or wheezing) lasting ≥3 days and requiring specified treatment changes. Moderate exacerbations required a prescription for antibiotics, systemic CSs, or both (with no hospitalization); severe exacerbations required hospitalization. Fatal COPD exacerbations were those with fatal outcome. The onset of exacerbation was defined as the onset of the first reported symptom; the end of exacerbation was decided by the investigator, based on clinical judgment (GOLD grouping was determined according to 2011 guidelines, which classified patients’ risk by airflow limitation, symptoms, and exacerbations).Citation15
Statistical analysis
The tiotropium-treatment arms were pooled for this post hoc analysis, as there were no differences between treatments for the primary outcomes (exacerbations and mortality).Citation14 Patients were categorized by their annual exacerbation rate on treatment into the following frequency groups: nonexacerbators, infrequent exacerbators (annual exacerbation rate >0 and ≤1), and frequent exacerbators (annual exacerbation rate >1). Patients were also categorized by the number of reported prestudy exacerbations (exacerbation history 0, 1, and >1 in the year before the study). In addition, we analyzed patients with severe exacerbations (exacerbations associated with hospitalization) and those with a fatal exacerbation.
Baseline characteristics discriminating between patients in the exacerbation groups (either prestudy or on treatment) were identified using descriptive statistics (differences between groups were signified by nominal P-values established using the Kruskal–Wallis test and the χ2 test). Furthermore, prognostic characteristics of exacerbation, hospitalization due to COPD exacerbation, and death (all-cause) were identified by univariate and multivariate Cox regression analyses, with results shown as forest plots.
The importance of factors added to the models was assessed by means of likelihood ratio tests. The effect of exacerbation history, LABA, and ICS use at baseline on exacerbations and death was investigated by Cox regression models with covariates for postbronchodilator FEV1 and smoking status at baseline. Time to event according to exacerbation history and ICS use at baseline are shown as Kaplan–Meier plots. To ensure that there was sufficient time for recurrent events to occur, we restricted the analysis to individuals with ≥2 years of clinical observation (follow-up) or who had died within that period.
Results
Study population
Of the 17,135 patients who received tiotropium, 13,591 were followed for ≥2 years or died during the study. In this group, 6,559 (48.3%) had no exacerbations during the trial, 4,568 (33.6%) were infrequent exacerbators (annual exacerbation rate >0 and ≤1), and 2,464 (18.1%) were frequent exacerbators (annual exacerbation rate >1). A severe exacerbation requiring hospitalization was reported in 2,002 (14.7%) of these patients, and 120 (0.9%) patients experienced a fatal exacerbation (, continued in Table S1). In the year before randomization, 7,022 (51.7%) patients had no exacerbations, 3,902 (28.7%) had one exacerbation, and 2,667 (19.6%) had more than one exacerbation (Table S2).
Table 1 Patient baseline characteristics according to exacerbation rate, and severe and fatal exacerbation during trial
Risk factors by exacerbation frequency and severity (hospitalized and fatal exacerbation)
Baseline demographics
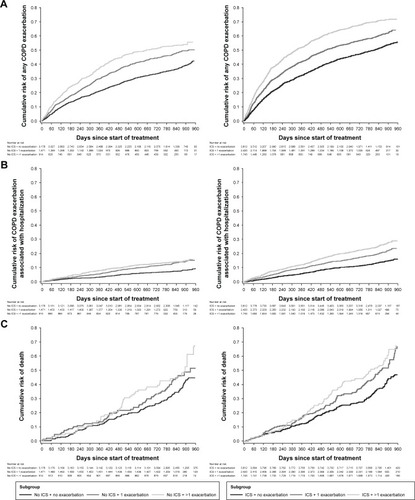
Baseline characteristics, including smoking history and body-mass index (BMI), were similar among the different groups whether defined by exacerbation rate on treatment () or pretreatment (number of exacerbations reported in the preceding year; Table S2). The proportion of female patients was highest in the frequent-exacerbator group compared with the other exacerbation groups. Patients aged ≥60 years had more exacerbations on treatment than patients <60 years of age (), although patients aged ≥60 years were more likely to report no exacerbation in the year prior to the trial compared with younger (<60 years) patients (Table S2). Patients most likely to have a fatal exacerbation were male and ≥70 years old (, ).
Figure 1 Multivariate Cox regression of time to (A) first exacerbation, (B) first hospitalization due to COPD exacerbation, and (C) death (treated set).
Abbreviations: Aus, Australia; BMI, body-mass index; Euro, Europe; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; mMRC, modified Medical Research Council; NZ, New Zealand.
Baseline lung function, exacerbation history, and COPD symptoms
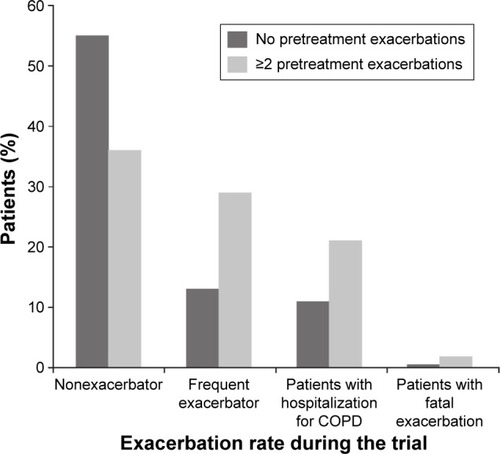
Baseline spirometry and exacerbation history showed a gradation across the on-treatment exacerbation-frequency group (being worst in frequent exacerbators), as did GOLD staging (I–IV), GOLD grouping (A–D), and breathlessness (Table S1). However, 13% of patients without a pretreatment exacerbation in the year before the study became frequent exacerbators during the trial (). The presence of sputum-producing cough (chronic bronchitis for >3 months over 2 years) was consistent across these groups. When patients were classified according to their history of exacerbations before study entry, a similar demographic pattern was seen (Table S2); however, those reporting previous exacerbations were more likely to have a history of sputum-producing cough. Patients who experienced severe exacerbations showed poorer lung function, were more likely to be GOLD stage IV and group D, and had more breathlessness than frequent on-treatment exacerbators. In patients with fatal exacerbations, this pattern was even more pronounced (, Table S1).
Figure 2 Exacerbation rate during the trial by pretreatment exacerbation history.
Baseline cardiovascular history and medication
In general, there were no differences between the on-treatment and prestudy frequency groups in either their history of cardiovascular events or their use of cardiovascular medications (, Table S3). However, heart failure was present at study entry more often among those dying from an exacerbation.
Baseline risk factors for exacerbation, hospitalization (due to COPD), and death (all-cause)
Risk of exacerbation
Overall, univariate analysis identified the same baseline characteristics associated with differences in risk for exacerbation as the descriptive analysis (Figure S1A). Multivariate analysis adjusted for all other relevant covariates indicated that modified Medical Research Council scale breathlessness score, exacerbation history, airflow limitation (FEV1% predicted), and LABA or ICS use at baseline (the surrogate marker for maintenance therapy) are the most important risk factors ().
Even after adjustment for all other important risk factors, baseline maintenance therapy with LABAs and ICSs remained relevant factors improving the model fit (P<0.0001) (). The surrogate marker LAMA use could not be evaluated, as patients on LAMAs at baseline did not add an additional treatment during the study compared with those receiving LABAs or ICSs at baseline.
Table 2 Likelihood-ratio test for baseline maintenance therapies
Risk of hospitalization due to COPD
Similar risk predictors as those for exacerbations were observed for hospitalization due to COPD, with the addition of poor FVC (Figure S1B). Multivariate analysis identified breathlessness score, exacerbation history, FEV1% predicted, ICS use at baseline (surrogate marker), and cardiac history as the most important factors; however, the analysis did not confirm the independent risk-modifying effect of FVC (). After adjustment for other risk factors, baseline maintenance therapy with LABAs and ICSs remained relevant factors for time to hospitalization due to COPD, improving the model fit (P<0.0001) ().
Risk of death (all-cause)
With respect to mortality, significant predictors included sex, age, BMI, breathlessness score, exacerbation history, lung function (FEV1% predicted and FVC), and history of cardiac events (Figure S1C). With the exception of FVC, these factors were confirmed by multivariate analysis, indicating that underweight male patients were at increased risk of dying, and this risk increased with age, reduced lung function, and exacerbation frequency.
Effect of exacerbation history and baseline pulmonary therapy on exacerbation, hospitalization, and death
Risk of exacerbation
When analyzing the risk-modifying effect of exacerbation history and baseline LABA/ICS use on exacerbation (analysis adjusted for smoking status and postbronchodilator FEV1 at baseline), patients with a history of frequent exacerbations (annual exacerbation rate >1) were at significantly higher risk of exacerbations during the trial. This higher risk of exacerbations for frequent exacerbators was irrespective of their LABA or ICS use at baseline (P<0.0001) versus nonexacerbators (). Nevertheless, use of ICSs at baseline was a marker for increased risk of further exacerbations in patients with and without exacerbation history. Overall, patients receiving ICS or LABA therapy did not show a lower exacerbation risk than patients without ICS or LABA use at baseline (). Kaplan–Meier analysis of time to first exacerbation showed that patients without an exacerbation history who used ICSs at baseline had a similar risk of exacerbation as patients with previous exacerbations without ICS use ().
Table 3 Moderate–severe COPD exacerbations (A) and death by exacerbation history (B), LABA, and ICS use at baseline, adjusted for postbronchodilator FEV1 and smoking status at baseline
Risk of hospitalization due to COPD
Kaplan–Meier analysis of time to hospitalization showed that the ICS-use marker and a history of more than one exacerbation were associated with increased risk of hospitalization ().
Risk of death (all-cause)
Patients receiving ICSs/LABAs at baseline were not at an increased risk of mortality during the trial compared with patients not receiving the combination, irrespective of exacerbation history (). Similarly, patients receiving ICSs or LABAs did not have a lower risk of mortality compared with patients not receiving ICSs or LABAs, respectively (). Patients with an exacerbation history receiving ICSs plus LABAs were, however, at an increased risk of mortality compared with those without a history of exacerbations. Therefore, past exacerbations warranting ICS/LABA use are an indicator for increased risk of death (). Kaplan–Meier analysis of time to death showed that ICS use and a history of more than one exacerbation were associated with increased risk of death ().
Stability of exacerbation phenotype
In the first year, 11,885 patients were infrequent exacerbators (0–1 exacerbation). Of these, 10,953 (92.2%) were also infrequent exacerbators in the second year. However, of the 1,706 patients with two or more exacerbations in the first year (frequent exacerbators), 1,023 (60%) were infrequent exacerbators in the second year.
Discussion
Identifying patients at greatest risk of exacerbation should facilitate the clinical management of COPD. In this large population of patients who were initially clinically stable and whose therapy always included the LAMA tiotropium, we found a similar risk profile to that reported in other groups where therapy was less standardized. Important factors included history of prior exacerbations, more dyspnea, poor lung function, and female sex. Medication use at baseline represented an independent risk of future exacerbation, but was not as important as exacerbation history in identifying those at risk of hospitalization or death. These data have implications for how we evaluate COPD patients already receiving treatment.
Unlike earlier studies, TIOSPIR participants all received a LAMA via either HandiHaler or Respimat, but in addition could continue with any non-LAMA therapy. The resulting population would be one that would occur if the health-care provider followed recommendations for treatment of current GOLD groups B–D.Citation16 Standardizing therapy in this way did not change the relative contribution of predictive factors associated with exacerbations.
There was no difference in age, smoking status, or BMI category between individuals with frequent events and those who never experienced an exacerbation over the ≥2 years of follow-up. As in the ECLIPSE study,Citation5 a history of sputum-producing cough in our patients did not predict those more likely to exacerbate. This difference from the data reported in COPDGene participantsCitation17 and other studiesCitation18 may reflect differences in the definition of chronic bronchitis that is used: studies that did not use the classic definition of chronic bronchitis were more likely to identify an association between chronic cough and exacerbation frequency.Citation19,Citation20 Neither a history of cardiac disease nor cardiac medication use distinguished the exacerbation groups (grouped by exacerbation frequency and severe and fatal exacerbation), suggesting that in this population most events were driven by respiratory rather than cardiac causes. As in earlier reports, both postbronchodilator FEV1 and dyspnea intensity were related to exacerbation frequency. However, there was considerable overlap between subgroups, with a third of frequent exacerbators having a modified Medical Research Council grade ≤1 at baseline.
When the effect of relevant covariates (postbronchodilator FEV1 and smoking status at baseline) was controlled for, the same relationships for exacerbation frequency and time to first exacerbation held true; this was also the case for time to hospitalization and death. Sex was an exception, where females were more likely to experience exacerbations, but less likely to die. This paradoxical finding has been noted previously, and no satisfactory explanation currently exists for this anomaly.Citation21 However, it has been suggested that women are more often underdiagnosed, show lower adherence to treatment than men, and present with fewer comorbidities.Citation22
A history of exacerbations (in the year before the study) was a powerful explanatory variable, with evidence of a dose–response effect for time to first exacerbation and time to hospitalization, although less evident for time to death. However, the use of exacerbation history as a categorical variable in individual patients as proposed by GOLD (“0 or 1 indicates low risk, while 2 or more exacerbations indicate high risk”) was rather disappointing.Citation16 Overall, 55% of patients remained exacerbation-free if they had no exacerbation in the year before the study, while 45% did not, despite all of them using at least a LAMA. Additionally, 13% of patients without exacerbation history became frequent exacerbators, and 36% of frequent exacerbators before the study had no exacerbations during the study.
ECLIPSE noted that patients did shift from high-risk to low-risk exacerbator groups over time, and the reasons for doing so were unclear.Citation23 Recently, Han et al made similar observations regarding the instability of the frequent-exacerbator phenotype in the SPIROMICS cohort.Citation24 However, adequate therapy seems to improve the ratio of infrequent to frequent exacerbators over time.Citation25–Citation27 Our data emphasize that patients with COPD have the propensity to exacerbate during the course of their disease, and that prior exacerbation history is only an approximate guide as to what will happen subsequently, not a precise predictor of exacerbation risk. As all our patients received the same COPD maintenance therapy on treatment, other factors may also be relevant for changes in risk over time.
The use of a maintenance respiratory therapy, such as a LABA, LAMA, or ICS, is usually considered in terms of the ability of that treatment to prevent exacerbations, rather than as a marker of the likelihood that they will occur. However, prior use of certain treatments, especially ICSs, which are almost exclusively prescribed as a way to prevent exacerbations, has been shown to identify patients more likely to exacerbate,Citation28 a finding supported by clinical trial data where prior ICS users had a higher exacerbation rate postrandomization.Citation29 Our data suggest that both LABA and ICS use predicts a higher rate of subsequent exacerbations, and that this is true irrespective of the previous exacerbation rate. Nevertheless, this only applied to the risk of a health-care utilization-defined exacerbation. This relationship might mean that therapy increased the risk of exacerbations, although this is unlikely given the wealth of randomized controlled data suggesting the opposite.Citation30,Citation31 A more likely explanation is that patients are given these drugs to prevent exacerbations and/or because they are believed to be progressing less well, and thus are more likely to relapse in future, irrespective of any positive effect of their therapy. Hospitalizations and death were related to exacerbation history, but not medication use.
Our study has strengths and limitations. Although not as large as the recent UK database study,Citation28 exacerbations were prospectively defined and collected. We considered data over a potential 2-year follow-up period in a substantial number of patients, and had a near-complete assessment of vital status. The universal use of LAMA therapy allowed us to not just assess how this treatment option related to exacerbation outcomes but also how the use of other treatments interacted with LAMA use. However, these treatments were not randomized and reflected the treatment choices of clinicians. We did not evaluate the surrogate marker LAMA use at baseline. Patients on LAMAs prior to the study simply remained on them, unlike patients receiving LABAs or ICSs at baseline, who had a LAMA added to their therapy. This analysis would thus show the benefit of adding a LAMA, rather than the risk of being on a LAMA. In addition, bio-marker data were not included, which some have suggested are associated with more events,Citation32 although these are not routinely recorded. Furthermore, when describing associations between current treatment and future risk, there is the limitation that the characteristics of patients at the time of prescription are not known, nor is the effect of the treatments on these characteristics.
Our data have some clinical implications. The similarity of the risk profile in our patients to those reported in groups where treatment was less rigidly controlled not only supports attempts to predict the inherent likelihood of exacerbation,Citation33 but also supports the idea of an “exacerbator phenotype” and its use as a way to stratify future risk. However, reliance on exacerbation history alone can be misleading, and factors other than those commonly assessed, and specifically prior and/or current therapy, should be considered when assessing the likelihood of the individual patient experiencing future exacerbations. The additional role of treatment as a marker of the propensity to exacerbate resembles the situation in asthma, where treatment steps are commonly linked to the therapy already prescribed. Whether a similar system can be developed for COPD patients will be for others to determine.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Acknowledgments
This study was funded by Boehringer Ingelheim. Writing assistance was provided by Sarah J Petit and Jennifer C Fuchs of Parexel and Kristina Standeven of MediTech Media, and was funded by Boehringer Ingelheim.
Supplementary materials
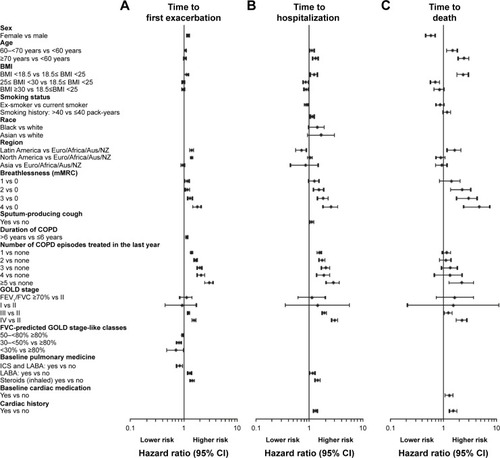
Figure S1 Univariate Cox regression of time to first (A) exacerbation, (B) first hospitalization due to COPD exacerbation and (C) death (treated set).
Notes: Breathlessness mMRC descriptions: 0, not troubled with breathlessness except with strenuous exercise; 1, troubled by shortness of breath when hurrying on the level or walking up a slight hill; 2, walks more slowly than people of the same age on the level because of breathlessness or has to stop for breath when walking at own pace on the level; 3, stops for breath after walking about 100 yards [91.44 m] or after a few minutes on the level; 4, too breathless to leave the house or breathless when dressing or undressing.
Abbreviations: Aus, Australia; BMI, body-mass index; Euro, Europe; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; mMRC, modified Medical Research Council; NZ, New Zealand.
![Figure S1 Univariate Cox regression of time to first (A) exacerbation, (B) first hospitalization due to COPD exacerbation and (C) death (treated set).Notes: Breathlessness mMRC descriptions: 0, not troubled with breathlessness except with strenuous exercise; 1, troubled by shortness of breath when hurrying on the level or walking up a slight hill; 2, walks more slowly than people of the same age on the level because of breathlessness or has to stop for breath when walking at own pace on the level; 3, stops for breath after walking about 100 yards [91.44 m] or after a few minutes on the level; 4, too breathless to leave the house or breathless when dressing or undressing.Abbreviations: Aus, Australia; BMI, body-mass index; Euro, Europe; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; ICS, inhaled corticosteroid; LABA, long-acting β2-agonist; mMRC, modified Medical Research Council; NZ, New Zealand.](/cms/asset/d65f1b96-b1b2-402d-a61d-ba40d10ea8cf/dcop_a_145814_sf0001_b.jpg)
Table S1 Patient baseline characteristics according to exacerbation rate and severe and fatal exacerbations during trial (continued from )
Table S2 Patient baseline characteristics according to the number of exacerbations in the year preceding the trial
Table S3 Pulmonary and cardiac medication at baseline, during treatment, and after discontinuation
Disclosure
PMAC reports receiving consulting fees, lecture fees, and travel support from Novartis, GlaxoSmithKline, Boehringer Ingelheim, and Takeda. DD reports receiving consulting fees, lecture fees, and payment for the development of educational activities from Boehringer Ingelheim, Pfizer, Novartis, Chiesi, Nycomed, and Dey Pharma. RAW reports receiving consulting fees from AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, ContraFect, GlaxoSmithKline, Janssen, Mylan, Novartis, Pfizer, Pulmonx, Roche, Spiration, Sunovion, Teva, Theravance, Verona, and Vertex, and grant support from Boehringer Ingelheim, Glaxo-SmithKline, and Pearl Therapeutics. KT, AM, and NM are employees of Boehringer Ingelheim, and ARA reports receiving consulting fees, lecture fees, and travel support from AstraZeneca, Boehringer Ingelheim, Forest Laboratories, GlaxoSmithKline, and Novartis and grant support from GlaxoSmithKline. The authors report no other conflicts of interest in this work.
References
- VestboJEdwardsLDScanlonPDChanges in forced expiratory volume in 1 second over time in COPDN Engl J Med2011365131184119221991892
- WilkeSJonesPWMüllerovaHOne-year change in health status and subsequent outcomes in COPDThorax201570542042525782757
- MüllerovaHMaselliDJLocantoreNHospitalized exacerbations of COPD: risk factors and outcomes in the ECLIPSE cohortChest20151474999100725356881
- BeehKMGlaabTStowasserSCharacterisation of exacerbation risk and exacerbator phenotypes in the POET-COPD trialRespir Res20131411624168767
- HurstJRVestboJAnzuetoASusceptibility to exacerbation in chronic obstructive pulmonary diseaseN Engl J Med2010363121128113820843247
- KimVCrinerGJChronic bronchitis and chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2013187322823723204254
- De SoyzaACalverleyPMLarge trials, new knowledge: the changing face of COPD managementEur Respir J20154561692170325792640
- VestboJAgustiAWoutersEFShould we view chronic obstructive pulmonary disease differently after ECLIPSE? A clinical perspective from the study teamAm J Respir Crit Care Med201418991022103024552242
- FarneHACatesCJLong-acting beta2-agonist in addition to tiotropium versus either tiotropium or long-acting beta2-agonist alone for chronic obstructive pulmonary diseaseCochrane Database Syst Rev201510CD00898926490945
- DecramerMLChapmanKRDahlROnce-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group studyLancet Respir Med20131752453324461613
- VogelmeierCHedererBGlaabTTiotropium versus salmeterol for the prevention of exacerbations of COPDN Engl J Med2011364121093110321428765
- Global Initiative for Asthma2016 GINA Report: Global Strategy for Asthma Management and PreventionBethesda (MD)GINA2016
- WiseRAAnzuetoACalverleyPThe Tiotropium Safety and Performance in Respimat Trial (TIOSPIR), a large scale, randomized, controlled, parallel-group trial-design and rationaleRespir Res2013144023547660
- WiseRAAnzuetoACottonDTiotropium Respimat inhaler and the risk of death in COPDN Engl J Med2013369161491150123992515
- VestboJHurdSSRodriguez-RoisinRThe 2011 revision of the global strategy for the diagnosis, management and prevention of COPD (GOLD): why and what?Clin Respir J20126420821422906068
- Global Initiative for Chronic Obstructive Lung DiseaseGlobal Strategy for Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary DiseaseBethesda (MD)GOLD2016
- BuschRHanMKBowlerRPRisk factors for COPD exacerbations in inhaled medication users: the COPDGene study biannual longitudinal follow-up prospective cohortBMC Pulm Med2016162826861867
- BurgelPRChronic cough and sputum production: a clinical COPD phenotype?Eur Respir J20124014622753831
- KimVSternbergALWashkoGSevere chronic bronchitis in advanced emphysema increases mortality and hospitalizationsCOPD201310666767823978192
- KimVCrapoJZhaoHComparison between an alternative and the classic definition of chronic bronchitis in COPDGeneAnn Am Thorac Soc201512333233925575351
- CelliBVestboJJenkinsCRSex differences in mortality and clinical expressions of patients with chronic obstructive pulmonary disease: the TORCH experienceAm J Respir Crit Care Med2011183331732220813884
- KilicHKokturkNSariGCakirMDo females behave differently in COPD exacerbation?Int J Chron Obstruct Pulmon Dis20151082383025977604
- DonaldsonGCMüllerovaHLocantoreNFactors associated with change in exacerbation frequency in COPDRespir Res2013147923899210
- HanMKQuibreraPMCarrettaEEFrequency of exacerbations in patients with chronic obstructive pulmonary disease: an analysis of the SPIROMICS cohortLancet Respir Med20175861962628668356
- CelliBRDecramerMAsijeeGMKupasKTashkinDPEffects of tiotropium on exacerbations in patients with COPD with low or high risk of exacerbations: a post-hoc analysis from the 4-year UPLIFT trialChronic Obstr Pulm Dis20152212213028848836
- VogelmeierCFAsijeeGMKupasKBeehKMTiotropium and salmeterol in COPD patients at risk of exacerbations: a post hoc analysis from POET-COPDAdv Ther201532653754726100349
- WedzichaJARabeKFMartinezFJEfficacy of roflumilast in the COPD frequent exacerbator phenotypeChest201314351302131123117188
- MüllerovaHShuklaAHawkinsAQuintJRisk factors for acute exacerbations of COPD in a primary care population: a retrospective observational cohort studyBMJ Open2014412e006171
- BatemanEDRabeKFCalverleyPMRoflumilast with long-acting β2-agonists for COPD: influence of exacerbation historyEur Respir J201138355356021737553
- CalverleyPMAndersonJACelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med2007356877578917314337
- CelliBDecramerMKestenSMortality in the 4-year trial of tiotropium (UPLIFT) in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20091801094895519729663
- ThomsenMIngebrigtsenTSMarottJLInflammatory biomarkers and exacerbations in chronic obstructive pulmonary diseaseJAMA2013309222353236123757083
- MakeBJErikssonGCalverleyPMA score to predict short-term risk of COPD exacerbations (SCOPEX)Int J Chron Obstruct Pulmon Dis20151020120925670896