Abstract
The recommended standard treatment for giant bullae is surgical bullectomy. However, with a relatively high risk for perioperative morbidity and mortality, it is unsuitable for some patients. Recently, bronchoscopic bullectomy with one-way valves has shown efficacy and safety in some cases. Locating the giant bulla and confirming the negative collateral ventilation are essential for the bronchoscopic bullectomy with valves. Here, we report a case with a giant bulla using the Chartis System to correct the previous mislocation by the high-resolution computed tomography (HRCT), thus helping to achieve a great efficacy in the bronchoscopic bullectomy with valves. Our case suggests that bronchoscopic bullectomy with valves could be an effective and safe choice. Chartis system can be helpful in determining the location of a bulla when difficulty is encountered using HRCT.
Keywords:
Introduction
In recent years, bronchoscopic lung volume reduction (BLVR) with one-way valves has been shown to improve lung function and exercise capacity in carefully selected patients with severe heterogeneous emphysema.Citation1–Citation4 The one-way valves implanted in the target bronchi can permit airflow out of the target lobe during exhalation and prevent it from flowing back in through the valves, thus causing the target lobe volume reduction. However, patients with giant bullae (greater than 5cm diameters) have been excluded from previous randomized controlled trials (RCTs) of valves.
Bullae frequently appear in the lung of emphysematous patients. Giant bullae, precipitating a total loss of lung function, will occupy a relatively larger space of the thorax than pure emphysema and cause more lung tissue compression around the affected area. Therefore, it can be recognized as extremely heterogeneous emphysema from lung mechanics, restricting the pulmonary function of patients more significantly. Although the recommended standard therapy is surgical bullectomy,Citation5 it is rational that giant bullae can be deflated by implanting valves in the bronchi connected to it. Another advantage of bronchoscopic bullectomy with valves over bullectomy is less invasiveness which can reduce the risks for perioperative morbidity and mortality that are much higher after thoracic surgical procedures in patients with severe emphysema.Citation6 The largest obstacle challenging interventional pulmonologists is how to locate a giant bulla, as the airway might be compressed and the tension of a giant bulla may transpose itself to a different location. Therefore, the lobe where a giant bulla originates from might be misjudged using high-resolution computed tomography (HRCT), which is the standard screening method before the BLVR. If the valves are placed into the wrong lobe bronchi, it may lead to treatment failure or even the enlargement of the bulla. The latter change may further deteriorate pulmonary function and cause very severe complications. Here we reported a case with a giant bulla, for the first time to our knowledge, using Chartis system to redress the previously mislocation by HRCT and acquired the successful therapy of bronchoscopic bullectomy with endobronchial valve (EBV).
Case Presentation
A 70-year-old male, diagnosed with chronic obstructive pulmonary disease (COPD) for 3 years, was admitted to the hospital in July 2019. He presented with exertional dyspnea, a mild chronic cough with reduced sputum production. He had a history of cigarette smoking (10 pack-years) and had quit when COPD was diagnosed. He was on budesonide/formoterol (160/4.5ug) for two years with a mild symptomatic improvement. This year, he experienced acute exacerbations that required hospitalization twice. The last one was in June. Five days before hospitalization, he experienced a deterioration of symptoms including worsening dyspnea and sweating. X-ray and chest CT in the local hospital showed a large right pneumothorax and consequently, thoracic drainage was conducted.
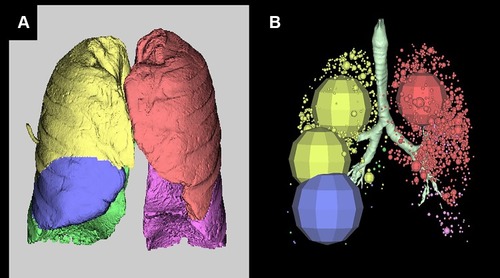
After 1 week of recovery from the pneumothorax, HRCT was performed. It revealed severe bilateral centrilobular emphysema with a giant bulla, which might be located in the right middle lobe (RML) (see in ). Both the upper lobe and the middle lobe in the right lung were compressed. The maximum dimension of the giant bulla in the axial view was 15.2×6.9 cm. Automatic HRCT analysis software (SYNAPSE VINCENT; Fuji Film, Tokyo, Japan) was used to analyze the emphysematous lung volume (see in and ). The percentage of emphysematous lung volume in the RML was 82.9% which confirmed that the giant bulla originated from the RML. The 6-min walk distance (6MWD) was 163m. The modified Medical Research Council (mMRC) dyspnea scale was 3 and the COPD Assessment Test (CAT) score was 18. Arterial blood gas analysis (on 2.0L/min oxygen therapy) showed that pH was 7.413, PaCO2 40.0 mmHg, and PaO2 92.2 mmHg. The pulmonary function test (PFT) was not performed for the recent pneumothorax.
Table 1 Changes in Volume and Emphysematous Volume After Bronchoscopic Bullectomy with Endobronchial Valves
Figure 1 (A–C) High resolution computed tomography (HRCT) taken before the procedure (Horizontal axis, coronal, sagittal, respectively) indicates severe emphysema and a giant bulla in the right middle lobe. (D–F) HRCT taken at 1st day after the procedure showing the decrease of the bulla and the re-expansion of the adjacent lobe.
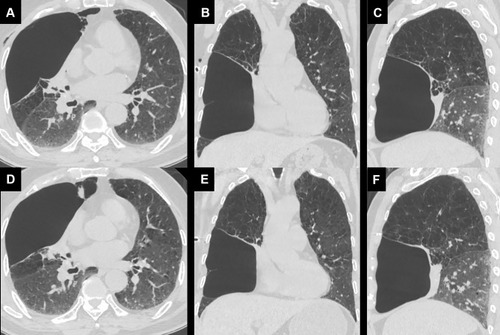
Figure 2 (A) 3-D analysis by SYNAPSE shows the lung lobes with a different color: yellow, right upper lobe; blue, right middle lobe; green, right lower lobe; red, left upper lobe; purple, left lower lobe. (B) 3-D analysis by the SYNAPSE shows the emphysematous area. The larger the area, the more severe the emphysema.
After a discussion with a thoracic surgeon, the patient refused surgical bullectomy because of the high risk associated with the surgical procedure. Thus, we decided to perform bronchoscopic bullectomy with valves.
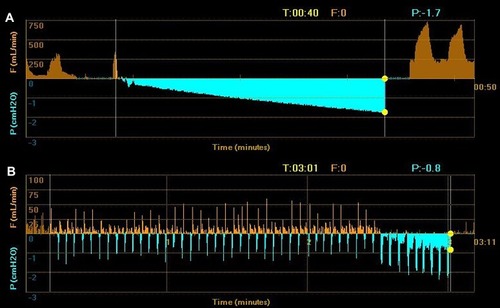
The procedure was performed under general anesthesia with intubation. The Chartis System (Pulmonx International SARL, Switzerland) was used to test bilateral ventilation. We blocked the right middle bronchus with the balloon catheter and observed the expiratory airflow and the airway pressure (). Before blocking, the peak airflow of RML was about 300–400 mL/min, and then the flow stopped immediately and a progressive negative pressure was observed. Such a change indicated that the right middle bronchus may collapse or the RML was completely atelectatic. It showed that the location of the giant bulla was probably not in the RML, which did not match the previous analysis by HRCT. Then we placed the catheter in the entrance of the right upper bronchus, a peak airflow less than 50 mL/min was measured before blocking and then a gradual decrease in flow (total of 22.4mL) and an increase in pressure were observed (). The airflow reached zero in 3min and 1s, which indicated the collateral ventilation was negative. Then we confirmed the target lobe to be the right upper lobe (RUL). After the measurements of the apical segmental bronchus, the posterior segmental bronchus, and the anterior segmental bronchus, we selected three Zephyr EBV 4.0 (PulmonX Corp, Redwood City, CA, USA) and implanted them in each segmental bronchus of the right upper lobe.
Figure 3 The output in the Chartis system. (A) Right middle lobe: Higher leak airflow before blocking in the right middle bronchus. The airflow stops immediately and a progressive negative pressure is observed. (B) Right upper lobe: Small leak airflow (less than 50mL/min) before blocking in the right upper bronchus. And the airflow gradually decreases and reaches zero in 3min and 1s.
A bedside X-ray was performed immediately after the bronchoscopy. It showed that the right lung volume decreased mildly compared to that before the procedure (). HRCT conducted on the 1st day illustrated mild shrinking of the giant bulla and re-expansion of the adjacent lobe (see in ). The volumes before and after bronchoscopic bullectomy were also measured using SYNAPSE VINCENT (see in ).
Figure 4 (A) Posterior-anterior chest X-ray taken before the procedure indicating severe emphysema and a huge bulla in the right lung. (B) Supine chest X-ray taken after the procedure, showing a mild volume decrease in the right upper lobe.

The patient got a significant improvement in symptoms and 6MWD, which increased to 276m. He completed PFT successfully and the outcome measures were the following: forced expiratory volume in 1 s (FEV1), 0.97L (percentage of predicted the FEV1, 39.7%); forced vital capacity (FVC), 2.17L (percentage of predicted the FVC, 68.7%); FEV1/FVC ratio, 43.29%; residual volume (RV), 4.14L (percentage of predicted RV, 170.5%); total lung capacity (TLC), 6.21 L (percentage of predicted TLC, 106.2%); and percentage of predicted diffusing capacity of carbon monoxide (DLCO), 53.9%.
Eight days after the procedure, the patient suffered right pneumothorax again and was cured by closed thoracic drainage in the local hospital. The second bronchoscopy showed no EBV migration or dysfunction, indicating that the pneumothorax probably originated from RML or right lower lobe (RLL). The patient could not complete the examination of HRCT or PFT for personal reasons. After 5 months, through a follow-up performed over telephone, he indicated that he felt well with an mMRC scale score of 1 and a CAT score of 6.
Discussion
We performed bronchoscopic bullectomy with one-way EBVs to treat a patient with a giant bulla which was originally mislocated and achieved great efficacy with our intervention.
The management of giant bullae depends on the severity of symptoms. Most of the patients seek bullectomy therapy because of severe dyspnea or other complications including pneumothorax.Citation6,Citation7 There are several papers including case reports that showed the efficacy and safety of bronchoscopic bullectomy with one-way valves in the treatment of giant bullae.Citation8–Citation11
Determining the location of a giant bulla and confirming the bulla is supplied by the bronchus is essential for valve treatment. Nevertheless, in some patients, it is difficult for the transposition of giant bullae caused by its high tension. HRCT can provide detailed information from the 3-D analysis. However, it may be misleading or futile when the airways feeding a bulla are collapsed by the compression of the giant bulla or adjacent lung tissues. The Chartis System can measure the airflow and intra-luminal pressure signals of airways. Primarily, it is used to measure the presence of collateral ventilation between adjacent lobes, which is a contraindication of bronchial volume reduction. Therefore, the Chartis System can predict the radiological and clinical response to bronchial valve volume reduction.Citation12 However, the patterns of giant bullae in the Chartis system remain uncertain. The mechanism of evolution of a giant bulla is essential. The traditional view indicates a valvular mechanism in an emphysematous area which only allows gas to enter but not leave. Under tension, the inflated area blows up. However, MorganCitation13 measured the oxygen and carbon dioxide tension and pressure in the giant bullae, and found that the pressure in the bullae mirrored the pleural pressure and was not “under tension”. Besides, they found that although gas could flow into and out of the giant bulla, the ventilation is smaller and slower than the surrounding lung. These results, to some extent, could indicate the flow signal of a lobe with giant bullae in the Chartis System - a relatively low leak airflow first, and a subsequent gradual decrease in flow after blocking the bronchus.
In the present case, the giant bulla was identified in the right middle lobe first from the HRCT analysis. In addition, the automatic software SYNAPSE VINCENTconfirmed the highest emphysema rate in the RML (82.9%). To clarify it, we used the Chartis System during the procedure. The performance of the RML in the Chartis System did not match the characters of a giant bulla while the RUL did. One day after the procedure, the giant bulla was deflated mildly which indicated the bronchus feeding it had been closed. To our knowledge, this was the first case reported where the Chartis System helped to correct and confirm the location of a giant bulla which was originally misjudged by HRCT analysis.
The patient in our institution underwent a memorable experience. He encountered spontaneous pneumothoraces twice, one before and one after the procedure. In the second pneumothorax, there was no evidence of valve dysfunction or bulla re-expansion. The compressed adjacent lung tissue will expand to occupy the newly created space.Citation1,Citation14 The shifting of volume on one side of the lung can result in the tearing of lung tissue, which partly explains the reason for the pneumothorax. It was reported that more than 90% of pneumothoraces developed within 3 days after the procedure in severe emphysema;Citation4 however, the present patient experienced pneumothorax on day 8. The untreated ipsilateral lobes were also emphysematous, and a rupture of blebs or bullae in these lobes could also cause the second pneumothorax.
During follow up, the patient showed significant improvements in symptoms and exercise capacity. This successful implantation suggests that in selected patients, whose definite bullae location is known and those who have negative collateral ventilation, a bronchoscopic bullectomy with EBV could be an effective and safe choice. Chartis System can be helpful for determining the location when it is difficult using HRCT.
Ethics and Consent Statement
The authors confirm that the patient provides written informed consent and gives his consent for images and all other clinical information to be published.
The ethic approval is not required to publish these case report details according to the institutional ethic committee.
Disclosure
The authors report no conflicts of interest in this work.
References
- SciurbaFC, ErnstA, HerthFJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363(13):1233–1244. doi:10.1056/NEJMoa090092820860505
- DaveyC, ZoumotZ, JordanS, et al. Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (the BeLieVeR-HIFi study): a randomised controlled trial. Lancet (London, England). 2015;386(9998):1066–1073. doi:10.1016/S0140-6736(15)60001-0
- KloosterK, Ten HackenNH, HartmanJE, KerstjensHA, van RikxoortEM, SlebosDJ. Endobronchial valves for emphysema without interlobar collateral ventilation. N Engl J Med. 2015;373(24):2325–2335. doi:10.1056/NEJMoa150780726650153
- SkowaschD, FertlA, SchwickB, SchaferH, HellmannA, HerthFJ. A long-term follow-up investigation of endobronchial valves in emphysema (the LIVE study): study protocol and six-month interim analysis results of a prospective five-year observational study. Respiration Int Rev Thoracic Diseases. 2016;92(2):118–126. doi:10.1159/000448119
- SinghD, AgustiA, AnzuetoA, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53(5):1900164.30846476
- KrishnamohanP, ShenKR, WigleDA, et al. Bullectomy for symptomatic or complicated giant lung bullae. Ann Thorac Surg. 2014;97(2):425–431. doi:10.1016/j.athoracsur.2013.10.04924365212
- SniderGL. Reduction pneumoplasty for giant bullous emphysema. Implications for surgical treatment of nonbullous emphysema. Chest. 1996;109(2):540–548.8620733
- SantiniM, FiorelliA, VicidominiG, Di CrescenzoVG, MessinaG, LaperutaP. Endobronchial treatment of giant emphysematous bullae with one-way valves: a new approach for surgically unfit patients. Eur J Cardiothorac Surg. 2011;40(6):1425–1431. doi:10.1016/j.ejcts.2011.03.04621764325
- TianQ, AnY, XiaoBB, ChenLA. Treatment of giant emphysamous bulla with endobronchial valves in patients with chronic obstructive pulmonary disease: a case series. J Thorac Dis. 2014;6(12):1674–1680. doi:10.3978/j.issn.2072-1439.2014.11.0725589959
- HouG, WangW, WangQY, KangJ. Bronchoscopic bullectomy with a one-way endobronchial valve to treat a giant bulla in an emphysematic lung: a case report. Clin Respir J. 2016;10(5):657–660. doi:10.1111/crj.1225725516237
- LeeEG, RheeCK. Bronchoscopic lung volume reduction using an endobronchial valve to treat a huge emphysematous bullae: a case report. BMC Pulm Med. 2019;19(1):92. doi:10.1186/s12890-019-0849-z31088437
- HerthFJ, EberhardtR, GompelmannD, et al. Radiological and clinical outcomes of using Chartis to plan endobronchial valve treatment. Eur Respir J. 2013;41(2):302–308. doi:10.1183/09031936.0001531222556025
- MorganMD, EdwardsCW, MorrisJ, MatthewsHR. Origin and behaviour of emphysematous bullae. Thorax. 1989;44(7):533–538. doi:10.1136/thx.44.7.5332505400
- CoxsonHO, Nasute FauerbachPV, Storness-BlissC, et al. Computed tomography assessment of lung volume changes after bronchial valve treatment. Eur Respir J. 2008;32(6):1443–1450. doi:10.1183/09031936.0005600818684848
